Abstract
Background:
Epidural dumbbell-shaped chordomas are localized slow growing, and malignant/aggressive neoplasms. Here, we present a 62-year-old male with a T3-T4 dumbbell-shaped chordoma and reviewed the appropriate literature.
Case Description:
A 62-year-old male presented with a three-month history of thoracic pain. When the thoracolumbar magnetic resonance (MR) showed a T3-T4 dumbbell-shaped intracanalicular/extradural tumor, he underwent tumor removal. After the histological examination proved the lesion was a spinal chordoma, he underwent a secondary radical transthoracic tumor resection. Postoperatively, the patient was able to walk without assistance, and at 6-month follow-up, was neurologically intact with only residual paresthesias.
Conclusion:
Malignant spinal chordomas may mimic benign neurinomas on MR scans. Here, biopsy of the lesion to confirm the diagnosis of chordoma was critical and directed subsequent definitive transthoracic tumor resection.
Keywords: Chordoma, Dumbbell, Schwannoma, Spine, Thoracic

INTRODUCTION
Chordomas are localized, slow growing, and malignant/aggressive neoplasms originating from notochordal remnants. Although they are typically found in the sacrococcygeal (50–60%) followed by the spheno-occipital (25–40%) regions, spinal chordomas (15%), and more often found in the cervical spine.[3,5] Here, we present a 62-year-old male with a dumbbell-shaped T3/ T4 chordoma who first underwent biopsy followed by definitive transthoracic resection of his tumor. The relevant literature was additionally reviewed.
CASE PRESENTATION
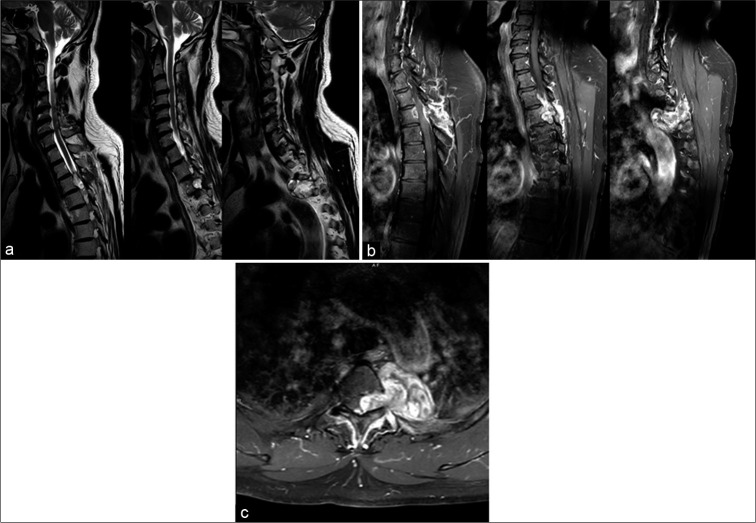
A 62-year-old male presented with 3-month history of thoracic pain, gait disturbance, bilateral lower extremity weakness, and paresthesias below the T2 level. The thoracolumbar magnetic resonance (MR) showed a combined intracanalicular and extradural left-sided T3/T4 dumbbell-shaped tumor that markedly compressed the spinal cord and left T3 root. Further, the lesion extended through the left T3-T4 intervertebral foramen into the subpleural space, abutting the posterior wall of the descending aorta. On MR, the lesion was hypointense on T1 studies, inhomogeneously hyperintense on T2 weighted images, and inhomogeneously enhanced with contrast (Type I according to Wang et al. classification) [Figure 1].
Figure 1:
(a) Thoracolumbar spine magnetic resonance imaging (MRI) T2-weighted sagittal images in series showed an extradural T3 dumbbell-shaped tumor, that severely compressed the spinal cord non-homogenously hyperintense. (b) Thoracolumbar spine MRI T1-weighted sagittal images in series with Gadolinium in series showed an extradural T3 dumbbell-shaped tumor in-homogeneously enhanced with enlarged neuroforamina. (c) Thoracolumbar spine MRI T1-weighted axial image showed a left extradural T3 dumbbell-shaped tumor.
Surgery, pathology, and immunological confirmation of spinal chordoma
As the lesion severely compressed the spinal cord, the patient underwent a T3-T4 laminectomy for intracanalicular/ extracanalicular extradural tumor removal [Figure 2]. The frozen section diagnosis suggested a spinal chordoma, while the permanent specimen confirmed this diagnosis.
Figure 2:
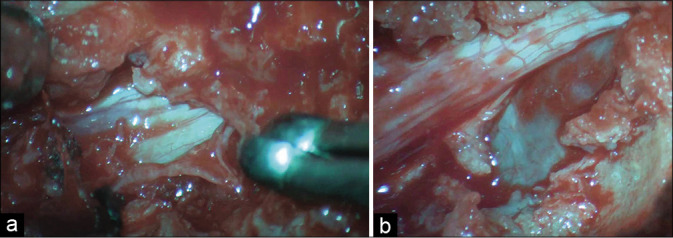
Intraoperative images showing epidural removal of the lesion (a) and extraforaminal component (b).
Pathology and immunohistochemistry
Pathologically the lesion was a chordoma and contained vacuolated “physaliphorous” cells with eosinophilic cytoplasm in a fibro-myxoid stroma. The Immunostaining confirmed the diagnosis of a chordoma and included: EMA, Vimentin, S-100, CK7 positivity, negativity for GFAP, HBM-45, synaptophysin, chromogranin, desmin, alfa-smooth muscle actin, p53with a low proliferation rate (Ki-67.5%).
Post-operative course
The patient then underwent aggressive transthoracic resection of tumor. The post-operative course was uneventful; the patient’s gait immediately improved, and the thoracic pain resolved. The 3-month post-operative MRI documented almost complete removal of the lesion except for the portion adherent to the posterior wall of the descending aorta. At 6 post-operative months, the patient’s motor deficit had resolved, and he exhibited only mild residual paresthesias.
DISCUSSION
Incidence
Chordomas are slow-growing tumors that originate from notochordal residuals. They are mostly localized to the sacral, clival, and spinal regions.[4,5] They have an overall incidence of 8.4 per 10 million people and typically carry a poor prognosis; the median survival is just 6.29 years due to the tumor’s high proclivity for local invasiveness and/or metastasizing early.[3]
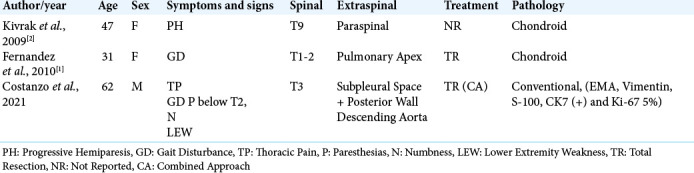
MR and computed tomography (CT) diagnosis of spinal chordomas
Spinal chordomas typically occur in the cervical (71.4%), followed by thoracic (14.3%), lumbar (7.1%), and sacral (7.1%) levels.[1,3] A review of 14 dumbbell-shaped spinal chordomas revealed that only two were located in the thoracic spine as in the case we presented [Table 1]. Typically on MR scans, spinal chordomas appear isointense on T1 weighted images, hyperintense on T2 studies (i.e. demonstrating fibrous septa), and uniformly heterogeneously enhance with contrast.[5] On CT scans, other common findings include: intratumoral calcified deposits, enlargement of the involve neural foramina, and potential extension/involvement of intervertebral disks.[2]
Table 1:
Patients’ demographics.
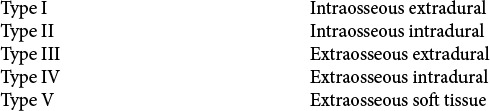
Classification of spinal chordomas
Wang et al. (2004) classified spinal chordomas into Types I-V.[6] [Table 2] Interestingly, spinal extraosseous chordomas have a better prognosis due to the greater feasibility of achieving an en-bloc resection of these lesions.[8] Notably, however, most lesions metastasize early in the clinical course to the lungs (58%), liver (22%), lymph nodes (33%), bone (17%), and skeletal muscles (9%).[8]
Table 2:
Classification of spinal chordomas according to Wang et al. (2004).
Histopathology
The major differential diagnoses for chordomas include schwannomas, meningiomas, neurofibromas, arachnoid cysts, and myxopapillary ependymomas.[8] It is, therefore, critical to obtain timely histological confirmation of these lesions (i.e. biopsy/open resection to determine chondroid, and/or cellular dedifferentiation) to determine whether and if they are amenable to gross total surgical resection which carries the best prognosis.[3,7]
CONCLUSION
Spinal chordomas are rare, malignant, and aggressive tumors that may radiographically mimic benign neurinomas. It is critical to obtain timely pathological confirmation of these chordomas as the best prognoses are attributed to early surgery (i.e. gross total resection if feasible), prior to the onset of further local invasiveness and metastases.
Footnotes
How to cite this article: Costanzo R, Scalia G, Marrone S, Umana GE, Graziano F, Furnari M, et al. Thoracic dumbbell spinal chordoma mimicking a schwannoma. Surg Neurol Int 2021;12:497.
Contributor Information
Roberta Costanzo, Email: robertacostanzo3@gmail.com.
Gianluca Scalia, Email: gianluca.scalia@outlook.it.
Salvatore Marrone, Email: salvo.mr89@gmail.com.
Giuseppe Emmanuele Umana, Email: umana.nch@gmail.com.
Francesca Graziano, Email: fragraziano9@gmail.com.
Massimo Furnari, Email: massimofurnari@alice.it.
Giancarlo Ponzo, Email: giancarlo.ponzo@gmail.com.
Massimiliano Giuffrida, Email: mass.giuffrida@tiscalinet.it.
Domenico Gerardo Iacopino, Email: gerardo.iacopino@gmail.com.
Giovanni Federico Nicoletti, Email: gfnicoletti@alice.it.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fernández Carballal C, González Rodrigalvarez R, de la Riva ML, Ares C. Dumbbell-shaped thoracic chondroid chordoma mimicking a neurinoma. Acta Neurochir (Wien) 2010;152:325–6. doi: 10.1007/s00701-009-0321-6. [DOI] [PubMed] [Google Scholar]
- 2.Kivrak AS, Koc O, Emlik D, Kiresi D, Odev K, Kalkan E. Differential diagnosis of dumbbell lesions associated with spinal neural foraminal widening: Imaging features. Eur J Radiol. 2009;71:29–41. doi: 10.1016/j.ejrad.2008.03.020. [DOI] [PubMed] [Google Scholar]
- 3.Lee SJ, Paeng SH, Kang MS, Jung SJ, Yoon SA, Park HY, et al. Retropharyngeal chordoma extending to the spinal cord, mimicking a neurogenic tumor: A case report and literature review. J Int Med Res. 2021;49:300060521999566. doi: 10.1177/0300060521999566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mukherjee D, Chaichana KL, Gokaslan ZL, Aaronson O, Cheng JS, McGirt MJ. Survival of patients with malignant primary osseous spinal neoplasms: Results from the surveillance, epidemiology, and end results (SEER) database from 1973 to 2003. J Neurosurg Spine. 2011;14:143–50. doi: 10.3171/2010.10.SPINE10189. [DOI] [PubMed] [Google Scholar]
- 5.Smolders D, Wang X, Drevelengas A, Vanhoenacker F, de Schepper AM. Value of MRI in the diagnosis of non-clival, non-sacral chordoma. Skeletal Radiol. 2003;32:343–50. doi: 10.1007/s00256-003-0633-1. [DOI] [PubMed] [Google Scholar]
- 6.Wang YP, Lee KS, Chen YJ, Huang JK. Extraosseous chordoma of the retropharyngeal space. Otolaryngol Head Neck Surg. 2004;130:383–5. doi: 10.1016/j.otohns.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Wasserman JK, Gravel D, Purgina B. Chordoma of the head and neck: A review. Head Neck Pathol. 2018;12:261–8. doi: 10.1007/s12105-017-0860-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang J, Yang X, Miao W, Jia Q, Wan W, Meng T, et al. Spine extra-osseous chordoma mimicking neurogenic tumors: Report of three cases and review of the literatures. World J Surg Oncol. 2016;14:206. doi: 10.1186/s12957-016-0951-0. [DOI] [PMC free article] [PubMed] [Google Scholar]