Abstract
Although genome editing technologies have the potential to revolutionize the way we treat human diseases, barriers to successful clinical implementation remain. Increasingly, preclinical large animal models are being used to overcome these barriers. In particular, the immunogenicity and long-term safety of novel gene editing therapeutics must be evaluated rigorously. However, short-lived small animal models, such as mice and rats, cannot address secondary pathologies that may arise years after a gene editing treatment. Likewise, immunodeficient mouse models by definition lack the ability to quantify the host immune response to a novel transgene or gene-edited locus. Large animal models, including dogs, pigs, and non-human primates (NHPs), bear greater resemblance to human anatomy, immunology, and lifespan and can be studied over longer timescales with clinical dosing regimens that are more relevant to humans. These models allow for larger scale and repeated blood and tissue sampling, enabling greater depth of study and focus on rare cellular subsets. Here, we review current progress in the development and evaluation of novel genome editing therapies in large animal models, focusing on applications in human immunodeficiency virus 1 (HIV-1) infection, cancer, and genetic diseases including hemoglobinopathies, Duchenne muscular dystrophy (DMD), hypercholesterolemia, and inherited retinal diseases.
Keywords: genome editing, CRISPR, nuclease, ZFN, meganuclease, Base editor, large animal models, preclinical models, nanoparticle, Lipid nanoparticle, non-human primate, pig, dog, in vivo gene therapy, ex vivo gene therapy
Graphical abstract
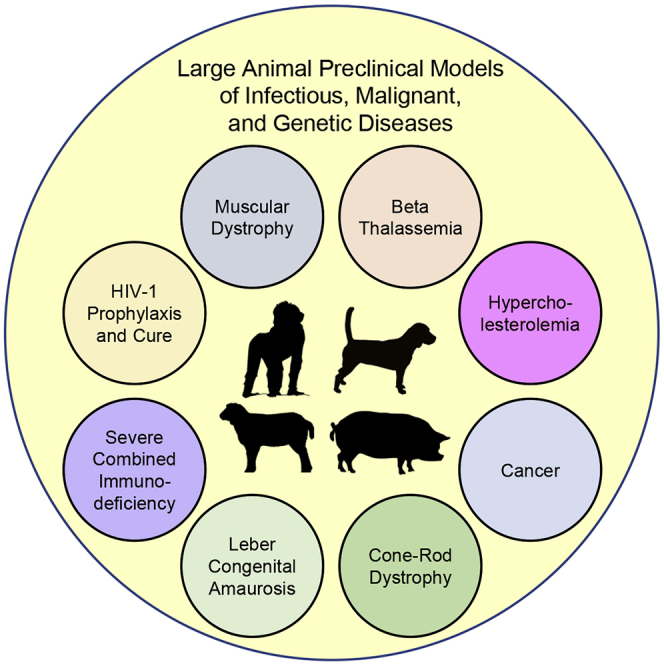
In this review, Maynard and colleagues outline how large animal models are being applied to optimize state-of-the-art gene editing therapies for the clinic. Specific focus is given to large animal models of HIV-1, cancer, and various heritable genetic diseases.
Introduction
Animal models are indispensable elements of translational research that have contributed enormously to our enhanced understanding of disease pathophysiology, transplantation biology, and gene therapy. For therapeutic development, animal models have been used to identify novel targets, evaluate dosing regimens, assess pharmacokinetic/pharmacodynamic (PK/PD) relationships, and, importantly, measure the therapeutic index of novel drugs. While small animal models (e.g., rodents) are generally more accessible and cost effective, they differ from humans in core biological processes such as hematopoiesis and immunological response1,2 and have demonstrated limitations in generating clinically relevant data for human diseases including cancer,3,4 neurodegenerative diseases,5,6 diabetes,7 and stroke.8 Large animals, including canines, non-human primates (NHPs), and pigs, may help to bridge the gap between rodent models and clinical studies since they are more similar to humans in anatomy, physiology, and metabolism (Table 1).9, 10, 11, 12, 13, 14 Compared to rodents, large animals have a considerably longer lifespan and thus enable multi-year studies to evaluate the long-term safety and efficacy of gene editing therapeutics, an especially critical aspect, for example, when assessing the impacts of off-target gene editing.15 Furthermore, given that large animals are closer in size to humans than rodents, the dosage and clinical feasibility of large-scale manufacturing can be assessed more directly. This is a critical and often overlooked aspect of translational research, and many manufacturing protocols for generating gene editing reagents or gene-modified cell products for small animals are often not readily scalable for applications in large mammals. The field of transplantation biology was pioneered in canine models,16 which also closely recapitulate many human malignancies, cardiovascular disease, and neuromuscular disorders.17, 18, 19 Early gene therapy and transplantation studies were conducted in dog and NHP models, since mouse models failed to identify important barriers to successful clinical implementation, such as human leukocyte antigen (HLA) matching and effective conditioning regimens.9,20 As a result, large animal studies helped develop clinically translatable protocols for generating gene-modified cells and achieving efficient in vivo engraftment. Here we review the development and preclinical evaluation of therapeutic genome editing strategies in large animal models, with a focus on applications in human immunodeficiency virus (HIV), cancer, blood disorders, muscular dystrophy, and retinal degenerations.
Table 1.
Benefits of a large animal model
| Small animals | Large animals | |
|---|---|---|
| Examples | rodents, zebrafish, insects, nematodes | NHPs, pigs, dogs, sheep |
| Sampling | limited blood volumes; difficult to isolate and characterize secondary organs | larger blood volumes and organs for studies of cancer, infectious diseases, and muscular dystrophies |
| Relevant cellular subsets | incomplete humanization in xenogeneic models (e.g., challenges in generating human myeloid and red blood cells in humanized mice)21 | often highly conserved versus human; availability of comparable mutations for modeling (e.g., SCID and DMD dogs) |
| Relevant anatomical structures | smaller and often not comparable to human (e.g., rodent retina lacks a macula)22 | close resemblance to human immune system (NHP), circulatory system (pigs)12, 13, 14 |
| Lifespan | short; limitation for long-term follow-up studies | longer lifespans enable tracking of edited cells for years/decades |
| Cost | low | high |
| Ease of manufacturing | labor-intensive process for humanized mice; limited availability of specific human stem cell sources; smaller size enables smaller-scale manufacturing of cell products | larger size facilitates test of manufacturing feasibility at scales closer to human |
| Route of administration | frequently not relevant to humans (e.g., intraperitoneal or tail vein in rodents) | intravenous and intramuscular dosing, central lines, and other routes highly comparable to humans |
| Infectious disease models | fewer human pathogens capable of infecting rodents and lower metazoans | broader susceptibility of large animals to human pathogens and closely related strains (e.g., HIV and SIV)23,24 |
| Musculoskeletal disease models | due to shortened lifespan, shorter time frame to study muscle wasting phenotypes, which are often less severe than human phenotypes25 | more clinically relevant progressive muscle wasting phenotypes, which can be studied over a longer lifespan |
NHP, nonhuman primate; SCID, severe combined immunodeficiency.
Overview of gene editing systems
There are four main families of engineered nucleases that have been used to insert, delete, or replace DNA in the genome: zinc finger nucleases (ZFNs),26 meganucleases,27,28 transcription activator-like effector nucleases (TALENs),29 and CRISPR-associated nuclease Cas9 (CRISPR-Cas9).30,31 While ZFNs, meganucleases, and TALENs recognize specific sequences in the genome through protein-DNA interactions, CRISPR-Cas9 nucleases are directed to a target site through simple base pairing to a complementary short guide RNA (gRNA) sequence. Once bound to a target site, these nucleases generate double-stranded breaks (DSBs) in the genome and enlist endogenous cellular pathways to repair the lesion. In the absence of a repair template, non-homologous end joining (NHEJ) pathways are activated to rapidly re-ligate the two ends of the DSB.32 NHEJ is error prone, and small insertions or deletions (indels) at the DSB cut site are frequently incorporated.33 These indels can create frameshift mutations or premature stop codons that result in gene knockout if the DSB occurs within the coding region of a gene. If a repair template with homology to the flanking regions of the DSB is provided, homologous recombination (HR) pathways can facilitate targeted integration of the repair template at the DSB.34 Researchers have relied on NHEJ and HDR pathways to engineer specific DNA manipulations to knock out aberrant genes, excise foreign DNA, correct disease-causing mutations, and integrate therapeutic genes.
Gene editing approaches for HIV-1
Since the discovery of HIV 40 years ago, 77.5 million people have been infected with HIV and almost 35 million people have died following progression to acquired immunodeficiency syndrome (AIDS) (Joint United Nations Programme on HIV/AIDS [UNAIDS]; https://www.unaids.org/). While suppressive antiretroviral therapy (ART) can efficiently block HIV replication and substantially improve the life expectancy of HIV+ individuals,35 ART is not curative, and latent viral reservoirs persist.36 These viral reservoirs can be reactivated if ART is interrupted, and thus ART is only effective at mitigating viral replication if strict adherence is maintained.37, 38, 39 To date, there have only been two documented cases of functional cure, defined here as sustained virus remission in the absence of ART. Both individuals, termed the Berlin and London patients, received myeloablative conditioning and transfusion of allogeneic hematopoietic stem cells (HSCs) to treat hematological malignancies.40, 41, 42 The transplanted HSCs harbored a homozygous loss-of-function deletion in the CCR5 gene (CCR5Δ32), the primary coreceptor used by most strains of HIV to gain entry into CD4+ cells.43 Reconstitution of the hematopoietic system with CCR5 null HIV-resistant HSCs led to durable HIV clearance in the absence of ART.
These case studies have inspired a new functional HIV cure approach that focuses on genetic engineering of CCR5 in a patient’s own (autologous) cells to confer resistance to HIV infection. Although highly complementary to large animal models of HIV persistence and cure, studies in humanized mouse models of HIV are more challenging, since humanization protocols are labor intensive and often result in incomplete development of all hematopoietic lineages (Table 1).21 Furthermore, due to their small size, adequate amounts of blood and tissue samples from rodents are more difficult to obtain. NHPs are widely regarded as the gold standard animal model for HIV. Although HIV-1 does not efficiently infect macaque cells (reviewed in Thippeshappa et al.44), NHPs are susceptible to closely related simian immunodeficiency virus (SIV) and simian/human immunodeficiency virus (SHIV), displaying hallmark features of HIV infection including CD4+ T cell depletion, progression to AIDS-like disease, and establishment of reactivatable latent reservoirs.23,24 A key consideration for NHP models of HIV cure and other diseases, including COVID-19,45 is the NHP species to apply, usually either rhesus macaques (Macaca mulatta), pigtail macaques (Macaca nemestrina), or cynomolgus macaques (Macaca fascicularis). Due to species-specific differences in the activity of lentiviral restriction factors, including TRIM5α, for example, pigtail macaque cells can be modified by the identical HIV-based lentiviral vectors that are used in patients, whereas rhesus macaque cells require specially engineered SIV-based lentiviral vectors.46, 47, 48, 49, 50 Cynomolgus macaques are slightly smaller than rhesus or pigtail macaques; the Mauritian subspecies further possesses limited MHC diversity due to a geographical bottleneck event, which is advantageous for MHC-centric studies of the control of numerous pathogens, including HIV.51 We have developed an autologous transplantation model to evaluate the function and engraftment potential of CCR5-edited HSCs that is applicable in multiple NHP species.52 Using ZFNs we achieved up to 64% CCR5 editing in pigtail macaque hematopoietic stem and progenitor cells (HSPCs) and demonstrated low but durable engraftment and multilineage repopulation of CCR5-edited progeny following myeloablative conditioning and transplantation (Table 2). Translating this approach to a model of latent HIV infection using SHIV-infected pigtail macaques suppressed with ART yielded comparable CCR5 editing efficiencies in HSCs and engraftment of CCR5-edited cells, notably in secondary lymphoid tissues known to harbor viral reservoirs.53 While transplanted animals ultimately exhibited viral rebound after ART cessation, the time to viral rebound trended later in CCR5-edited HSC transplants relative to unedited HSC transplanted controls. This approach was also investigated in SIV-infected ART-suppressed rhesus macaques by Yu and colleagues.54 Ex vivo CRISPR-Cas9 editing in HSPCs was suboptimal (<16%), and engraftment in busulfan-conditioned animals was low (∼1%). While all but one animal exhibited viral rebound after ART withdrawal, a small increase in CCR5 editing was detected in all hematopoietic subsets analyzed. Together, these data suggest that a selective advantage is conferred in CCR5 null cells in the context of active viremia but highlight that more efficient means will be needed to achieve a therapeutic threshold of engraftment of CCR5-edited cells.72
Table 2.
Overview of gene editing in large animal models
| Disease | Animal/disease model | Strategy | In vivo or ex vivo | Target | Gene editing system | Delivery | Conditioning | Results | Reference |
|---|---|---|---|---|---|---|---|---|---|
| HIV | NHP (pigtail macaque) | inactivate CCR5 in HSCs to enable HIV-resistant hematopoiesis | ex vivo | CCR5 in HSPCs | ZFN | electroporation of ZFN mRNA | myeloablative (TBI) | 64% CCR5 editing in infusion product, 3%–5% long-term engraftment | 52 |
| HIV | SHIV+ NHP (pigtail macaque) | inactivate CCR5 in HSCs to enable HIV-resistant hematopoiesis | ex vivo | CCR5 in HSCs | ZFN | electroporation of ZFN mRNA | myeloablative (TBI) | ∼50% CCR5 editing in infusion product, 3%–4% long-term engraftment, trafficking to secondary lymphoid tissue, trends toward delayed viral rebound after ART removal | 53 |
| HIV | SIV+ NHP (rhesus macaque) | inactivate CCR5 in HSCs to enable HIV-resistant hematopoiesis | ex vivo | CCR5 in HSPCs | CRISPR (SpCas9) | SIV-based LV | non-myeloablative (busulfan) | <16% CCR5 editing in infusion product, ∼1% long-term engraftment, all but one animal rebounded after ART removal | 54 |
| HIV | SHIV+ NHP (rhesus macaque) | inactivate CCR5 in anti-HIV CAR T cells to confer HIV resistance and enable virus-specific effector function | ex vivo | CCR5 in anti-HIV CAR T cells | CRISPR (SpCas9) | electroporation of CRISPR RNPs | none | <36% CCR5 editing in infusion product | 55 |
| HIV | SIV+ NHP (rhesus macaque) | excise integrated proviral DNA in SIV-infected cells | in vivo | SIV proviral DNA in SIV-infected cells | CRISPR (SaCas9) | AAV9 | none | up to 92% and 95% decrease in proviral DNA in blood and peripheral lymph nodes | 56 |
| SCD | NHP (rhesus macaque) | POC: correct point mutation in HBB that causes SCD via single base pair HDR conversion | ex vivo | HBB in HSCs | CRISPR | electroporation of CRISPR RNP + ssDNA donor template to recreate SCD point mutation via HDR | myeloablative (TBI) | 17%–26% recapitulation of SCD mutation in infusion product, ∼1% long-term engraftment | 57 |
| SCD/β-thalassemia | NHP (pigtail macaque) | disrupt BCL11A in HSCs to reactivate fetal hemoglobin | ex vivo | BCL11A in HSCs | TALEN | electroporation of TALEN mRNA | myeloablative (TBI) | 1.5% BCL11A editing in infusion product, 0.3%–0.4% long-term engraftment | 58 |
| SCD/β-thalassemia | NHP (rhesus macaque) | prevent BCL11A repression of fetal hemoglobin by disrupting BCL11A binding site in γ-globin promoter | ex vivo | HBG promoter in HSCs | CRISPR | electroporation of CRISPR RNPs | myeloablative (TBI) | 75% editing and 39% recapitulation of HPFH mutation in infusion product, 8%–27% editing and 6%–18% HbF expression in PB cells >1 year after treatment | 59 |
| SCD/β-thalassemia | NHP (rhesus macaque) | disrupt the erythroid-specific BCL11A enhancer region to disable BCL11A in erythroid lineages and reactivate fetal hemoglobin | ex vivo | erythroid-specific BCL11A enhancer region in HSCs | CRISPR (SpCas9) | electroporation of CRISPR RNPs | myeloablative (TBI) | up to 85% editing in enhancer region in infusion product, but engraftment and γ-globin expression highly dependent on number of infused cells | 60 |
| AML | NHP (rhesus macaque) | POC: inactivate CD33 in HSPCs to establish CD33-deficient hematopoiesis and enable CD33-directed immunotherapy | ex vivo | CD33 in HSPCs | CRISPR (SpCas9) | electroporation of CRISPR RNPs | myeloablative (TBI) | <15% CD33 editing in infusion product, 2%–4% long-term engraftment | 61 |
| DMD | DeltaE50-MD dogs62 | disrupt DMD exon 51 splice acceptor site to enable exon 51 skipping and restoration of dystrophin reading frame | in vivo | DMD exon 51 splice acceptor site in peripheral and cardiac muscle | CRISPR (SpCas9) | dual AAV9 to co-deliver Cas9 and gRNA | none | restoration of up to 70% and 92% of normal dystrophin in peripheral and cardiac muscles 8 weeks post-treatment | 63 |
| DMD | DMD exon 52-deficient pigs64 | excise DMD exon 51 to restore dystrophin reading frame | in vivo | DMD exon 51 in peripheral and cardiac muscle | CRISPR (SpCas9) | dual AAV9 to deliver split intein Cas9 + gRNA | none | widespread expression of truncated dystrophin in cardiac and skeletal muscle, decreased fibrosis, improved cardiac function and survival | 65 |
| Hypercholesterolemia | NHP (rhesus macaque) | knock out PCSK9 to prevent degradation of LDLR and increase uptake of blood LDL-c | in vivo | PCSK9 in hepatocytes | meganuclease | AAV8 | none | up to 84% reduction in serum PCSK9 and 60% LDL-c 11 months after treatment | 66 |
| Hypercholesterolemia | NHP (rhesus macaque) | knock out PCSK9 to prevent degradation of LDLR and increase uptake of blood LDL-c | in vivo | PCSK9 in hepatocytes | meganuclease | AAV8 | none | sustained dose-dependent reductions in serum PCSK9 and LDL-c 3 years after treatment | 67 |
| Hypercholesterolemia | NHP (cynomolgus macaque) | introduce precise loss-of-function PCSK9 mutation to knock out PCSK9, prevent LDLR degradation, and increase uptake of blood LDL-c | in vivo | PCSK9 in hepatocytes | CRISPR adenine base editors | LNP delivery of ABE8.8 mRNA and PCSK9 gRNA | none | >60% PCSK9 editing in NHP liver, stable 90% reduction of PCSK9 and 60% reduction of LDL-c | 68 |
| Hypercholesterolemia | NHP (cynomolgus macaque) | introduce precise loss-of-function PCSK9 mutation to knock out PCSK9, prevent LDLR degradation, and increase uptake of blood LDL-c | in vivo | PCSK9 in hepatocytes | CRISPR adenine base editors | LNP delivery of ABEmax mRNA and PCSK9 gRNA | none | up to 34% PCSK9 editing in NHP liver, ∼32% reduction in PCSK9 and ∼14% reduction in LDL-c | 69 |
| Leber congenital amaurosis | NHP (cynomolgus macaque) | POC: correct aberrant splice donor created by mutation in CEP290 to restore reading frame and normal CEP290 expression | in vivo | CEP290 mutation in retinal cells | CRISPR (SaCas9) | AAV5 delivery of SaCas9 and pair of gRNA | none | up to 30% reading frame-restoring editing | 70 |
| Cone-rod dystrophy (CORD6) | NHP (cynomolgus macaque) | POC: knockout of mutant GUCY2D followed by complementation with wt GUCY2D | in vivo | GUCY2D in retinal cells | CRISPR (SaCas9) | dual AAV5 delivery of SaCas9 and gRNA | none | 10%–20% editing in photoreceptor cells, up to 80% decrease in GUCY2D protein product | 71 |
Data from our group and others in the NHP model suggest that the successful cure of the Berlin and London patients was largely due to the near-complete hematopoietic reconstitution with donor-derived, HIV-resistant cells.73, 74, 75 Since both patients were primarily treated for their hematological cancers, lymphodepletion via myeloablative conditioning was a justifiable risk, whereas for otherwise healthy ART-suppressed HIV+ patients, the toxicities associated with myeloablative conditioning are generally not reasonable. While several clinical trials have attempted to recreate the success of the Berlin and London patients through transplantation of autologous CCR5-edited HSCs in non-conditioned patients, these studies have ultimately failed to eliminate HIV after ART withdrawal, since HIV-vulnerable CCR5+ lymphocytes and latent viral reservoirs persist.76, 77, 78, 79 In order to enable ART-free remission of HIV, more active means of targeting these reservoirs will likely be necessary. Rather than replacing the entire immune system with CCR5-edited cells, for example, a smaller number of enhanced virus-specific immune effectors, like chimeric antigen receptor (CAR) T cells, could be applied. We recently provided proof of principle for this strategy by transplanting SHIV-infected rhesus macaques with T cells that were electroporated with CCR5-targeted CRISPR-Cas9 ribonucleoprotein (RNP) complexes and transduced with lentiviral vectors expressing a virus-specific CAR.55 More elegant “2-for-1” gene editing strategies in which a virus-specific CAR is targeted to the CCR5 locus to enable simultaneous CAR integration and CCR5 knockout have also been developed. While these approaches showed promise in ex vivo studies and in small animal models, they remain to be tested in large animal models or in clinical studies.80,81
Gene editing to excise integrated proviral DNA has also shown promise in SIV-infected ART-suppressed rhesus macaque models. Through systemic delivery of adeno-associated virus serotype 9 (AAV9) vectors expressing Staphylococcus aureus Cas9 (SaCas9) and a pair of gRNAs targeting the SIV genome, Mancuso et al.56 demonstrated efficient excision of integrated proviral DNA in blood and relevant secondary lymphoid tissue. Following a single infusion, intact SIV DNA was markedly reduced, with up to 95% decrease in SIV DNA in lymph nodes. Given that multiplexed genome editing and DSB generation can result in chromosomal translocations,82,83 further studies evaluating the safety of this approach are required, particularly since AAV9 delivery of CRISPR machinery will lead to prolonged expression in broad tissue types and potential integration of the transgene at the cut site.84 Additionally, whether this approach is capable of accessing every latently infected cell in the body and inactivating replication-competent provirus, which will be required in order to prevent viral rebound in the absence of ART, remains to be determined.
Gene editing for hemoglobinopathies
Hemoglobinopathies are the most common genetic diseases, with around 1.1% of all couples at risk for having a child with a hemoglobin disorder.85 Sickle cell disease (SCD) and β-thalassemia are the most prevalent hemoglobinopathies and are caused by mutations in the β-globin gene (HBB), which together with α-globin forms adult hemoglobin (HbA). In SCD, a point mutation in HBB results in structural abnormalities in hemoglobin and the formation of sickle hemoglobin (HbS).86 Patients homozygous for HbS develop fragile, sickle-shaped red blood cells that cause vaso-occlusion, pain crises, irreversible organ damage, and early mortality.87 In β-thalassemia, mutations in HBB result in reduced or absent HBB synthesis, which leads to ineffective erythropoiesis and anemia.88 Currently, allogeneic bone marrow transplantation to replace defective HSCs is the only cure for SCD and β-thalassemia, although this approach is hampered by scarcities in HLA-matched donors. While vector-based gene therapy approaches to supplement autologous HSCs with a corrected HBB gene prior to transplantation have shown success in clinical trials,89,90 gene editing strategies offer the potential for endogenous gene correction without the risks associated with genomic integration of a viral vector.91 NHP models are uniquely suited for evaluating gene-edited HSC therapeutics since, unlike mouse HSCs, NHP and human HSCs can be identified by characteristic CD34 expression,92,93 enabling analogous and clinically relevant HSC isolation methods.20 Furthermore, for recently developed HSC-targeted in vivo gene therapy technologies,94,95 NHP models are useful for assessing genotoxicity, off-target transduction, and long-term efficacy.
For SCD, many groups have explored gene editing strategies that directly target and correct the causative mutation in the HBB coding sequence.96, 97, 98, 99 Similar to preclinical models of cancer, however, no large animal model of SCD currently exists. To demonstrate proof-of-principle correction of the SCD point mutation in HBB, Uchida et al.57 used CRISPR-Cas9 to generate the SCD mutation via HDR in CD34+ HSCs isolated from healthy rhesus macaques. HDR efficiency in infusion products was moderate (17%–26% gene conversion) and decreased to ∼1% in peripheral lymphocytes and granulocytes 16 weeks after transplantation into conditioned NHPs. HbS production similarly declined over time, from 8%–17% at early time points to 3%–10% 12 months post-transplant.
An alternative approach that has shown promise in large animal studies focuses on restoring functional hemoglobin through the reactivation of fetal hemoglobin (HbF), a tetramer composed of two α-globin and two γ-globin chains. While HbF is usually silenced after birth, post-natal HbF can be maintained or reactivated, as observed in individuals with a benign condition known as hereditary persistence of fetal hemoglobin (HPFH).100 Importantly, increased levels of HbF are correlated with decreased morbidity and mortality in SCD and β-thalassemia patients.101 HbF expression can be induced by inactivating BCL11A, a transcriptional repressor of HbF.102 To test this strategy, we established an NHP transplantation model to evaluate HbF reactivation in autologous BCL11A-edited CD34+ HSCs.58 We subsequently used CRISPR-Cas9 to recapitulate a naturally occurring 13-nucleotide deletion in HPFH individuals that disrupts the BCL11A binding site found in the γ-globin promoter regions.103,59 We achieved an average of 75% on-target editing and up to 39% recapitulation of the HPFH deletion either in CD34+ cells or in the refined CD90+ HSC enriched subpopulation. After myeloablative conditioning and transplantation, edited HSCs displayed stable, multilineage engraftment in rhesus macaques for over 1 year. Editing at the γ-globin locus was detected in 8% to 27% of peripheral blood (PB)-nucleated cells, and HbF-expressing cells stably reconstituted 6% to 18% of PB (Table 2).
Given that BCL11A plays critical roles in HSC self-renewal,104 lymphoid development,105 and dendritic cell fate,106 inactivation of BCL11A in HSCs may impair normal hematopoiesis. In 2013, Bauer et al.107 used genome-wide association studies to uncover an erythroid-specific BCL11A enhancer region that could be mutated in HSCs to inactivate BCL11A and induce HbF expression in erythroid cells.108 This strategy was tested in an NHP model of autologous HSC editing and transplantation, using CRISPR-Cas9 to disrupt the erythroid-specific enhancer and restore HbF expression in rhesus macaques.60 Infused HSCs demonstrated high (80%–85%) on-target editing, although engraftment and γ-globin expression were highly dependent on the number of cells infused. Targeting of the BCL11A enhancer region is also being explored in two clinical trials (NCT03655678, NCT03745287). Early reports from two patients—one with β-thalassemia and one with SCD—demonstrated ∼80% ex vivo editing in HSCs and >60% editing in nucleated PB cells more than 1 year after myeloablative conditioning and infusion.109 HbF expression increased rapidly in both patients, with HbF accounting for >91% of total hemoglobin in the β-thalassemia patient and 43.2% in the SCD patient. Importantly, neither patient experienced any further vaso-occlusive episodes or required transfusion of packed red cells by 30 days post-infusion. While these data are preliminary and longer-term studies in more patients are required, these extremely promising early reports are likely to change the landscape of β-thalassemia and SCD treatment and serve as the flagship example of the potential of gene editing to cure human disease.
Modeling gene editing therapies for cancer in large animals
CAR T cell therapies have shown remarkable responses in patients with B cell malignancies, as evidenced by recent US Food and Drug Administration (FDA) approvals.110, 111, 112, 113, 114 However, the success of this approach is highly dependent on the availability of cancer-restricted surface markers that can be targeted by CAR T cells. Although validated models of tumorigenesis are not readily available, proof-of-principle experiments in healthy NHPs provide a useful model to quantify depletion in cellular subsets that normally express such markers. For example, CD20 CAR T cells designed to target B cell malignancies have been shown to efficiently induce CD20+ B cell aplasia in healthy rhesus macaques.115 In acute myeloid leukemia (AML), up to 90% of leukemic blasts express CD33, a sialic acid receptor, although shared CD33 expression on normal hematopoietic and myeloid progenitors poses challenges for AML-specific targeting.116,117 While the role of CD33 in myeloid cells is not fully understood, CD33 knockout in mice showed no apparent consequence on survival, fertility, or hematopoiesis, suggesting CD33 may be dispensable for normal hematological function.118 This finding opens the door to CD33 gene editing/immunotherapeutic strategies in HSCs, where reconstitution of CD33 null hematopoiesis may enable CD33-dependent selection in AML patients. While this concept has been successfully demonstrated in mouse AML xenograft models,61,119 validation in an NHP model is critical, since long-term safety and engraftment cannot be assessed in a short-lived immunocompromised mouse model. In a proof-of-concept (POC) study, Kim et al.61 demonstrated that CRISPR-Cas9 inactivation of CD33 in HSPCs had no impact on myeloid development or function after autologous transplantation into conditioned rhesus macaques. While on-target editing in the infusion product was low (<15%), the CD33-edited CD34+ HSPCs engrafted and CD33 editing in myeloid cells and bone marrow HSPCs was stably detected for over 1 year. Follow-up studies assessing the efficacy of subsequent CD33-directed immunotherapy are required, although the lack of suitable NHP models of AML and other cancers may pose challenges.
Gene editing for Duchenne muscular dystrophy
Duchenne muscular dystrophy (DMD) is a severe X-linked recessive disease that affects roughly 1 in 5,000 newborn males and is characterized by progressive muscle degeneration and atrophy.120,121 DMD is caused by loss-of-function mutations in the gene that encodes dystrophin (DMD), a critical cytoskeletal protein.122 Despite improvements in standard of care, most DMD patients die from respiratory and cardiac failure between 20 and 40 years of age.123 While thousands of DMD mutations have been identified,124 frameshifting mutational “hotspots” are commonly found across exons 45 to 53.125 Dystrophin-deficient DMD animal models have been generated in mice,126, 127, 128, 129, 130, 131, 132 rats,133,134 and rabbits,135 although DMD models in larger animals, including dogs,62 pigs,64,136 and rhesus macaques,137 display phenotypes that more closely resemble human DMD pathophysiology.25 As such, large animal DMD models are particularly useful for functional evaluation of novel therapeutics. Targeted exon skipping to restore the DMD reading frame and generate a truncated but functional dystrophin protein is an area of active research, particularly given that more than 90% of DMD-causing mutations are predicted to be suitable for exon-skipping strategies.138 Moreover, a restoration of just 15% of the normal dystrophin levels is estimated to provide significant therapeutic improvement for DMD patients.139,140
Gene editing approaches to restore the DMD open reading frame and rescue functional dystrophin expression have recently been demonstrated in large animal models of DMD. Using CRISPR-Cas9 to target the DMD exon 51 splice acceptor site, Amoasii et al.63 co-delivered AAV9-Cas9 and AAV9-gRNA to deltaE50-MD dogs. Dystrophin rescue varied by administration route, with systemic delivery achieving up to 70% and 92% of wild-type (wt) dystrophin levels 8 weeks post-treatment in the peripheral and cardiac muscles, respectively. More recently, Moretti et al.65 demonstrated that dual AAV9s could be used to co-deliver a split-intein Cas9 and a pair of gRNAs to excise exon 51 and restore the reading frame in DMD exon 52-deficient pigs.64,141 Intravenous delivery of AAV9 vectors coated in polyamidoamine nanoparticles resulted in efficient exon 51 targeting and robust expression of a shortened form of dystrophin in skeletal muscle, heart tissue, and the diaphragm. While the truncated dystrophin was only partially functional, treated pigs showed significant reductions in fibrosis, improvements in cardiac function, and prolonged survival. This work represents an important step toward functional validation of gene editing therapeutics for DMD, but further studies are needed to fine-tune vector dosing, cardiac targeting, and toxicity.
Gene editing for hypercholesterolemia
Genome editing has also shown promise for the treatment of elevated levels of cholesterol in the blood (hypercholesterolemia). Proprotein convertase subtilisin/kexin type 9 (PCSK9), a protein encoded by the PCSK9 gene, binds to the hepatic low-density lipoprotein receptor (LDLR) and inhibits the uptake of LDL cholesterol (LDL-c) from the bloodstream by catalyzing the degradation of LDLR.142,143 Gain-of-function mutations in PCSK9 have been identified in individuals with familial hypercholesterolemia, an autosomal dominant condition that is characterized by increased serum LDL-c and an elevated risk of coronary heart disease (CHD).144 Conversely, loss-of-function PCSK9 mutations, which are found in 2%–3% of some populations, are associated with decreased levels of LDL-c and a significant (up to 88%) reduction in the risk of CHD.145, 146, 147 While several antibody-based PCSK9 inhibitors have gained FDA approval for the treatment of hypercholesterolemia,148,149 gene editing approaches offer the potential for durable PCSK9 inactivation from a single-dose treatment.
In 2018, Wang et al.66 published the first report of PCSK9 inhibition in rhesus macaques following a single infusion of AAV vectors expressing a PCSK9-targeted meganuclease. Serum PCSK9 and LDL-c decreased in a dose-dependent manner, with up to 84% PCSK9 and 60% LDL-c reduction 11 months after treatment. A 3-year follow-up report demonstrated durable PCSK9 and LDL-c reductions, with no significant changes in levels measured at year 2.67 Off-target editing was low but detectable at up to 80 sites by inverted terminal repeat sequencing (ITR-seq),150 and large (>15 bp) insertions at the PCSK9 locus were identified, the majority of which contained portions of the vector transgene. While vector-associated immunotoxicity was only evident at early time points, the presence of integrated transgene at the PCSK9 locus will likely raise safety concerns. A PCSK9 inhibition approach that avoids generating DSBs may help address these safety issues. Recently, Musunuru et al.68 demonstrated that CRISPR-derived adenine base editors (ABEs) could be used to introduce precise PCSK9 loss-of-function mutations in cynomolgus macaques. Following treatment with a single intravenous infusion of lipid nanoparticles (LNPs) containing ABE8.8 mRNA and PCSK9 gRNA,151 NHPs showed a durable 90% reduction in blood PCSK9 and 60% reduction in serum LDL-c for up to 8 months. Of the 48 off-target sites interrogated by ONE-seq,152 editing was only evident at one site. A similar approach using ABEmax69 (in place of ABE8.8) and the same LNP formulation was also recently demonstrated in a cynomolgus macaque model, although on-target editing, PCSK9 knockout, and serum LDL-c reduction were less efficient.153 While further studies are needed to assess the long-term safety and efficacy of ABE-mediated PCSK9 inhibition, the reduction in off-target editing, as well as the absence of DSB generation, vector integration, and prolonged meganuclease expression may offer significant safety advantages.
Gene editing for inherited retinal degenerations
Inherited retinal degenerations (IRDs) are a group of heterogeneous disorders characterized by degeneration of photoreceptors and retinal pigment epithelium.154 IRDs are a leading cause of blindness, with a global incidence of ∼1 in 2,000.155 IRD-causing mutations in more than 250 genes have been identified, and while some recessive IRD mutations can be treated with gene supplementation therapies,156 many autosomal dominant IRD mutations are not amenable to these approaches, since gene supplementation cannot overcome the dominant effect of the mutated gene product. As such, gene editing therapies that correct the underlying IRD mutations are actively being explored. Notably, the eye is an ideal target for developing novel gene editing therapies: therapeutics can be easily administered at this site, and because the eye is an immunoprivileged organ, anti-transgene and anti-vector immune responses are less likely to occur. Major anatomical differences between the mouse and human eye have been characterized, including the lack of a macula in the mouse retina (Table 1). NHP retinal anatomy is highly comparable to humans, making NHPs the optimal animal model for evaluating novel IRD therapies.22,157
One IRD being targeted with gene editing is Leber congenital amaurosis (LCA), an autosomal recessive disorder that affects ∼1 in 40,000 newborns158,159 and results in blindness or significant visual impairment in early infancy.160 LCA is caused by deleterious mutations in genes involved in diverse aspects of retinal function, such as photoreceptor development and transduction, vitamin A cycling, and guanine synthesis.161 While up to 18 genes have been implicated in LCA,162 CEP290, GUCY2D, and CRB1 are the most commonly mutated genes, occurring in 15%, 12%, and 10% of LCA patients, respectively.161 In a proof-of-principle study, Maeder et al.70 demonstrated that CRISPR-Cas9 could be used to correct the most prevalent loss-of-function mutation in CEP290 that impairs photoreceptor function.163 Healthy cynomolgus macaques were treated with AAV5 vectors expressing SaCas9 and a pair of gRNAs targeting the flanking regions of the CEP290 mutation site to excise the site or invert the intervening sequence within the CEP290 reading frame. Importantly, only ∼10% of functional photoreceptors are required for near-normal visual acuity.164 Up to 30% productive editing (i.e., predicted to restore the reading frame) was achieved at the highest dose, exceeding the therapeutic threshold that is hypothesized to restore vision. This promising therapeutic is now being investigated in a clinical trial (NCT03872479), highlighting the direct translatability of findings from large animal models to the clinic.
GUCY2D is another gene that is frequently implicated in IRDs. While loss-of-function mutations in GUCY2D are common in LCA patients, gain-of-function mutations in GUCY2D are identified in 35% of patients with cone-rod dystrophy 6 (CORD6),165,166 a rare autosomal dominant eye disorder. CORD6 pathology progresses more slowly than LCA, and patients typically present with macular degeneration, photophobia, and loss of visual and color acuity by age 10.167 GUCY2D encodes retGC1, an enzyme that facilitates the recovery phase of phototransduction. In CORD6, GUCY2D mutations lead to increased retGC1 activity, aberrant calcium signaling, and photoreceptor apoptosis. Inactivation of mutant GUCY2D followed by rescue with wt GUCY2D is one treatment strategy for CORD6 that is actively being investigated. In a proof-of-concept study, McCullough et al.71 co-injected dual AAV5 vectors expressing SaCas9 and GUCY2D gRNA into the retina of healthy cynomolgus macaques and detected up to 20% editing in photoreceptor cells and ∼80% reduction in retGC1 expression. This study represents an important step toward correcting GUCY2D-mediated CORD6, though future studies evaluating the success of subsequent rescue with wt GUCY2D are needed.
Conclusions and future directions
Compared to studies in small animals, therapeutic validation in large animals is more likely to be predictive of clinical success.168 As such, use of large animal disease models will be critical as the gene editing field continues to flourish. Moving forward, large animal models will continue to provide a key resource, for example, to optimize cell manufacturing at a scale that is most relevant to a patient. This involves not only an increase of several orders of magnitude in cell number and associated gene editing reagents (e.g., CRISPR RNP), but also the maintenance of an optimal ratio of gene editing efficiency to toxicity. Associated instrumentation (e.g., electroporation devices) must be capable of adjusting over this scale and should ideally transition seamlessly from the handling of millions to hundreds of millions or billions of cells. Previously, we observed a sharp decrease in editing efficiency when increasing to NHP scale for delivery of BCL11A-specific TALEN mRNA electroporation, despite no impact on delivery of a control GFP mRNA.58 We have recently found that in addition to limitations associated with electroporation hardware platforms, mRNA stability may also become an increasingly relevant factor as larger numbers of cells are handled in a given experiment (C.W.P. and R. Venkataraman, unpublished data). Stabilized mRNA formulations, transitioning to pre-formed, enzymatically active complexes like CRISPR RNPs, and use of electroporation devices featuring microfluidic and flowthrough capabilities169 are the most likely paths forward to overcome barriers related to scale-up for gene editing experiments in large animal models and in early-phase clinical studies. More importantly, so-called in vivo delivery approaches that prioritize global health endpoints by increasing portability and scalability should be a key focus moving forward. These strategies are needed in resource-limited settings where expensive gene therapy infrastructure is not available. For some of the indications described in this review, in vivo delivery systems are already at the forefront—for example, AAV vectors to treat DMD, hypercholesterolemia, and IRDs. For the treatment of other diseases, including HIV-1,170 rapidly emerging pathogens such as SARS-CoV-2,171 SCD,172 and cancer,173 bringing effective treatments to the patient without the need for costly cell manufacturing facilities will be more challenging. While AAV vectors are a major platform for in vivo gene delivery, adenoviral vectors and nanoparticle-based approaches have emerged as particularly promising alternatives. Gutless adenoviral vectors feature large genetic packaging capacities, which can be used to deliver both CRISPR-Cas9 machinery and homology donor templates to a cell type of interest.174 Nanoparticle formulations, namely mRNA-loaded LNPs, are leading global SARS-CoV-2 vaccination efforts and are exquisitely programmable and targetable for other indications, including cancer and metabolic diseases.175,176 Looking forward, these in vivo delivery platforms hold great promise in targeting a broadly neutralizing antibody to the inactivated CCR5 locus for HIV cure, or precise repair of sickle cell mutations without the need for ex vivo HSPC therapy, all via a single intravenous injection in an outpatient setting. While large animal studies are more costly and require specialized veterinary staff, the benefits of testing therapeutics and novel in vivo delivery systems in animal models that bear greater resemblance to human physiology, anatomy, and immunology should not be understated. Identifying critical issues in long-term safety, feasibility, and efficacy before novel genome editing therapies enter the clinic will help to de-risk these approaches, optimize formulations and dosing, and potentially increase the chance of clinical success.
Acknowledgments
We thank Helen Crawford for help in preparing this review and acknowledge the work of numerous colleagues whose published studies could not be cited due to space constraints. The authors are supported by grants from the NIH National Institute of Allergy and Infectious Diseases (UM1 AI126623, R01 AI135953, U01 AI138329, U19 AI149680, and U19 AI149505) and National Heart, Lung, and Blood Institute (R01 HL136135, U19 HL156247, and R01 HL151765).
Declaration of interests
H.P.K. has received support as the inaugural recipient of the José Carreras/E. Donnall Thomas Endowed Chair for Cancer Research and the Stephanus Family Endowed Chair for Cell and Gene Therapy, and is or was a consultant to and has or had ownership interests with Rocket Pharmaceuticals, Homology Medicines, VOR Biopharma and Ensoma Inc. H.P.K. has also been a consultant to CSL Behring and Magenta Therapeutics. Other authors have no competing interests.
References
- 1.Seok J., Warren H.S., Cuenca A.G., Mindrinos M.N., Baker H.V., Xu W., Richards D.R., McDonald-Smith G.P., Gao H., Hennessy L., Inflammation and Host Response to Injury, Large Scale Collaborative Research Program Genomic responses in mouse models poorly mimic human inflammatory diseases. Proc. Natl. Acad. Sci. USA. 2013;110:3507–3512. doi: 10.1073/pnas.1222878110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parekh C., Crooks G.M. Critical differences in hematopoiesis and lymphoid development between humans and mice. J. Clin. Immunol. 2013;33:711–715. doi: 10.1007/s10875-012-9844-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Voskoglou-Nomikos T., Pater J.L., Seymour L. Clinical predictive value of the in vitro cell line, human xenograft, and mouse allograft preclinical cancer models. Clin. Cancer Res. 2003;9:4227–4239. [PubMed] [Google Scholar]
- 4.Begley C.G., Ellis L.M. Drug development: Raise standards for preclinical cancer research. Nature. 2012;483:531–533. doi: 10.1038/483531a. [DOI] [PubMed] [Google Scholar]
- 5.Cavanaugh S.E., Pippin J.J., Barnard N.D. Animal models of Alzheimer disease: historical pitfalls and a path forward. ALTEX. 2014;31:279–302. doi: 10.14573/altex.1310071. [DOI] [PubMed] [Google Scholar]
- 6.Benatar M. Lost in translation: treatment trials in the SOD1 mouse and in human ALS. Neurobiol. Dis. 2007;26:1–13. doi: 10.1016/j.nbd.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 7.Roep B.O., Atkinson M., von Herrath M. Satisfaction (not) guaranteed: re-evaluating the use of animal models of type 1 diabetes. Nat. Rev. Immunol. 2004;4:989–997. doi: 10.1038/nri1502. [DOI] [PubMed] [Google Scholar]
- 8.van der Worp H.B., Howells D.W., Sena E.S., Porritt M.J., Rewell S., O’Collins V., Macleod M.R. Can animal models of disease reliably inform human studies? PLoS Med. 2010;7:e1000245. doi: 10.1371/journal.pmed.1000245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dehoux J.P., Gianello P. The importance of large animal models in transplantation. Front. Biosci. 2007;12:4864–4880. doi: 10.2741/2434. [DOI] [PubMed] [Google Scholar]
- 10.Meurens F., Summerfield A., Nauwynck H., Saif L., Gerdts V. The pig: a model for human infectious diseases. Trends Microbiol. 2012;20:50–57. doi: 10.1016/j.tim.2011.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Swindle M.M., Makin A., Herron A.J., Clubb F.J., Jr., Frazier K.S. Swine as models in biomedical research and toxicology testing. Vet. Pathol. 2012;49:344–356. doi: 10.1177/0300985811402846. [DOI] [PubMed] [Google Scholar]
- 12.Phillips K.A., Bales K.L., Capitanio J.P., Conley A., Czoty P.W., ’t Hart B.A., Hopkins W.D., Hu S.L., Miller L.A., Nader M.A. Why primate models matter. Am. J. Primatol. 2014;76:801–827. doi: 10.1002/ajp.22281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsang H.G., Rashdan N.A., Whitelaw C.B., Corcoran B.M., Summers K.M., MacRae V.E. Large animal models of cardiovascular disease. Cell Biochem. Funct. 2016;34:113–132. doi: 10.1002/cbf.3173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Skaggs H., Chellman G.J., Collinge M., Enright B., Fuller C.L., Krayer J., Sivaraman L., Weinbauer G.F. Comparison of immune system development in nonclinical species and humans: Closing information gaps for immunotoxicity testing and human translatability. Reprod. Toxicol. 2019;89:178–188. doi: 10.1016/j.reprotox.2019.06.005. [DOI] [PubMed] [Google Scholar]
- 15.AlJanahi A.A., Lazzarotto C.R., Chen S., Shin T.H., Cordes S., Fan X., Jabara I., Zhou Y., Young D.J., Lee B.C. Prediction and validation of hematopoietic stem and progenitor cell off-target editing in transplanted rhesus macaques. Mol. Ther. 2021 doi: 10.1016/j.ymthe.2021.06.016. Published online June 24, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ladiges W.C., Storb R., Thomas E.D. Canine models of bone marrow transplantation. Lab. Anim. Sci. 1990;40:11–15. [PubMed] [Google Scholar]
- 17.Sargan D.R. IDID: inherited diseases in dogs: web-based information for canine inherited disease genetics. Mamm. Genome. 2004;15:503–506. doi: 10.1007/s00335-004-3047-z. [DOI] [PubMed] [Google Scholar]
- 18.Rowell J.L., McCarthy D.O., Alvarez C.E. Dog models of naturally occurring cancer. Trends Mol. Med. 2011;17:380–388. doi: 10.1016/j.molmed.2011.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Camacho P., Fan H., Liu Z., He J.Q. Large mammalian animal models of heart disease. J. Cardiovasc. Dev. Dis. 2016;3:E30. doi: 10.3390/jcdd3040030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trobridge G.D., Kiem H.P. Large animal models of hematopoietic stem cell gene therapy. Gene Ther. 2010;17:939–948. doi: 10.1038/gt.2010.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marsden M.D. Benefits and limitations of humanized mice in HIV persistence studies. Retrovirology. 2020;17:7. doi: 10.1186/s12977-020-00516-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marmorstein A.D., Marmorstein L.Y. The challenge of modeling macular degeneration in mice. Trends Genet. 2007;23:225–231. doi: 10.1016/j.tig.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 23.Hatziioannou T., Evans D.T. Animal models for HIV/AIDS research. Nat. Rev. Microbiol. 2012;10:852–867. doi: 10.1038/nrmicro2911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Evans D.T., Silvestri G. Nonhuman primate models in AIDS research. Curr. Opin. HIV AIDS. 2013;8:255–261. doi: 10.1097/COH.0b013e328361cee8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McGreevy J.W., Hakim C.H., McIntosh M.A., Duan D. Animal models of Duchenne muscular dystrophy: from basic mechanisms to gene therapy. Dis. Model. Mech. 2015;8:195–213. doi: 10.1242/dmm.018424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim Y.G., Cha J., Chandrasegaran S. Hybrid restriction enzymes: zinc finger fusions to Fok I cleavage domain. Proc. Natl. Acad. Sci. USA. 1996;93:1156–1160. doi: 10.1073/pnas.93.3.1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Silva G., Poirot L., Galetto R., Smith J., Montoya G., Duchateau P., Pâques F. Meganucleases and other tools for targeted genome engineering: perspectives and challenges for gene therapy. Curr. Gene Ther. 2011;11:11–27. doi: 10.2174/156652311794520111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arnould S., Delenda C., Grizot S., Desseaux C., Pâques F., Silva G.H., Smith J. The I-CreI meganuclease and its engineered derivatives: applications from cell modification to gene therapy. Protein Eng. Des. Sel. 2011;24:27–31. doi: 10.1093/protein/gzq083. [DOI] [PubMed] [Google Scholar]
- 29.Joung J.K., Sander J.D. TALENs: a widely applicable technology for targeted genome editing. Nat. Rev. Mol. Cell Biol. 2013;14:49–55. doi: 10.1038/nrm3486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jinek M., Chylinski K., Fonfara I., Hauer M., Doudna J.A., Charpentier E. A programmable dual-RNA-guided DNA endonuclease in adaptive bacterial immunity. Science. 2012;337:816–821. doi: 10.1126/science.1225829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ran F.A., Hsu P.D., Wright J., Agarwala V., Scott D.A., Zhang F. Genome engineering using the CRISPR-Cas9 system. Nat. Protoc. 2013;8:2281–2308. doi: 10.1038/nprot.2013.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jackson S.P., Bartek J. The DNA-damage response in human biology and disease. Nature. 2009;461:1071–1078. doi: 10.1038/nature08467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lieber M.R. The mechanism of double-strand DNA break repair by the nonhomologous DNA end-joining pathway. Annu. Rev. Biochem. 2010;79:181–211. doi: 10.1146/annurev.biochem.052308.093131. 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bibikova M., Beumer K., Trautman J.K., Carroll D. Enhancing gene targeting with designed zinc finger nucleases. Science. 2003;300:764. doi: 10.1126/science.1079512. [DOI] [PubMed] [Google Scholar]
- 35.Teeraananchai S., Kerr S.J., Amin J., Ruxrungtham K., Law M.G. Life expectancy of HIV-positive people after starting combination antiretroviral therapy: a meta-analysis. HIV Med. 2017;18:256–266. doi: 10.1111/hiv.12421. [DOI] [PubMed] [Google Scholar]
- 36.Finzi D., Hermankova M., Pierson T., Carruth L.M., Buck C., Chaisson R.E., Quinn T.C., Chadwick K., Margolick J., Brookmeyer R. Identification of a reservoir for HIV-1 in patients on highly active antiretroviral therapy. Science. 1997;278:1295–1300. doi: 10.1126/science.278.5341.1295. [DOI] [PubMed] [Google Scholar]
- 37.Chun T.W., Davey R.T., Jr., Engel D., Lane H.C., Fauci A.S. Re-emergence of HIV after stopping therapy. Nature. 1999;401:874–875. doi: 10.1038/44755. [DOI] [PubMed] [Google Scholar]
- 38.Davey R.T., Jr., Bhat N., Yoder C., Chun T.W., Metcalf J.A., Dewar R., Natarajan V., Lempicki R.A., Adelsberger J.W., Miller K.D. HIV-1 and T cell dynamics after interruption of highly active antiretroviral therapy (HAART) in patients with a history of sustained viral suppression. Proc. Natl. Acad. Sci. USA. 1999;96:15109–15114. doi: 10.1073/pnas.96.26.15109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Deeks S.G., Lewin S.R., Ross A.L., Ananworanich J., Benkirane M., Cannon P., Chomont N., Douek D., Lifson J.D., Lo Y.R., International AIDS Society Towards a Cure Working Group International AIDS Society global scientific strategy: towards an HIV cure 2016. Nat. Med. 2016;22:839–850. doi: 10.1038/nm.4108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hütter G., Nowak D., Mossner M., Ganepola S., Müssig A., Allers K., Schneider T., Hofmann J., Kücherer C., Blau O. Long-term control of HIV by CCR5 Delta32/Delta32 stem-cell transplantation. N. Engl. J. Med. 2009;360:692–698. doi: 10.1056/NEJMoa0802905. [DOI] [PubMed] [Google Scholar]
- 41.Allers K., Hütter G., Hofmann J., Loddenkemper C., Rieger K., Thiel E., Schneider T. Evidence for the cure of HIV infection by CCR5Δ32/Δ32 stem cell transplantation. Blood. 2011;117:2791–2799. doi: 10.1182/blood-2010-09-309591. [DOI] [PubMed] [Google Scholar]
- 42.Gupta R.K., Peppa D., Hill A.L., Gálvez C., Salgado M., Pace M., McCoy L.E., Griffith S.A., Thornhill J., Alrubayyi A. Evidence for HIV-1 cure after CCR5Δ32/Δ32 allogeneic haemopoietic stem-cell transplantation 30 months post analytical treatment interruption: a case report. Lancet HIV. 2020;7:e340–e347. doi: 10.1016/S2352-3018(20)30069-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Farzan M., Mirzabekov T., Kolchinsky P., Wyatt R., Cayabyab M., Gerard N.P., Gerard C., Sodroski J., Choe H. Tyrosine sulfation of the amino terminus of CCR5 facilitates HIV-1 entry. Cell. 1999;96:667–676. doi: 10.1016/s0092-8674(00)80577-2. [DOI] [PubMed] [Google Scholar]
- 44.Thippeshappa R., Kimata J.T., Kaushal D. Toward a macaque model of HIV-1 infection: Roadblocks, progress, and future strategies. Front. Microbiol. 2020;11:882. doi: 10.3389/fmicb.2020.00882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Salguero F.J., White A.D., Slack G.S., Fotheringham S.A., Bewley K.R., Gooch K.E., Longet S., Humphries H.E., Watson R.J., Hunter L. Comparison of rhesus and cynomolgus macaques as an infection model for COVID-19. Nat. Commun. 2021;12:1260. doi: 10.1038/s41467-021-21389-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dietrich E.A., Jones-Engel L., Hu S.L. Evolution of the antiretroviral restriction factor TRIMCyp in Old World primates. PLoS ONE. 2010;5:e14019. doi: 10.1371/journal.pone.0014019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brennan G., Kozyrev Y., Kodama T., Hu S.L. Novel TRIM5 isoforms expressed by Macaca nemestrina. J. Virol. 2007;81:12210–12217. doi: 10.1128/JVI.02499-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Uchida N., Hsieh M.M., Washington K.N., Tisdale J.F. Efficient transduction of human hematopoietic repopulating cells with a chimeric HIV1-based vector including SIV capsid. Exp. Hematol. 2013;41:779–788.e1. doi: 10.1016/j.exphem.2013.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Evans M.E., Kumkhaek C., Hsieh M.M., Donahue R.E., Tisdale J.F., Uchida N. TRIM5α variations influence transduction efficiency with lentiviral vectors in both human and rhesus CD34(+) cells in vitro and in vivo. Mol. Ther. 2014;22:348–358. doi: 10.1038/mt.2013.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hanawa H., Hematti P., Keyvanfar K., Metzger M.E., Krouse A., Donahue R.E., Kepes S., Gray J., Dunbar C.E., Persons D.A., Nienhuis A.W. Efficient gene transfer into rhesus repopulating hematopoietic stem cells using a simian immunodeficiency virus-based lentiviral vector system. Blood. 2004;103:4062–4069. doi: 10.1182/blood-2004-01-0045. [DOI] [PubMed] [Google Scholar]
- 51.Wiseman R.W., Karl J.A., Bohn P.S., Nimityongskul F.A., Starrett G.J., O’Connor D.H. Haplessly hoping: macaque major histocompatibility complex made easy. ILAR J. 2013;54:196–210. doi: 10.1093/ilar/ilt036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Peterson C.W., Wang J., Norman K.K., Norgaard Z.K., Humbert O., Tse C.K., Yan J.J., Trimble R.G., Shivak D.A., Rebar E.J. Long-term multilineage engraftment of autologous genome-edited hematopoietic stem cells in nonhuman primates. Blood. 2016;127:2416–2426. doi: 10.1182/blood-2015-09-672337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Peterson C.W., Wang J., Deleage C., Reddy S., Kaur J., Polacino P., Reik A., Huang M.L., Jerome K.R., Hu S.L. Differential impact of transplantation on peripheral and tissue-associated viral reservoirs: Implications for HIV gene therapy. PLoS Pathog. 2018;14:e1006956. doi: 10.1371/journal.ppat.1006956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yu S., Ou Y., Xiao H., Li J., Adah D., Liu S., Zhao S., Qin L., Yao Y., Chen X. Experimental treatment of SIV-infected macaques via autograft of CCR5-disrupted hematopoietic stem and progenitor cells. Mol. Ther. Methods Clin. Dev. 2020;17:520–531. doi: 10.1016/j.omtm.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rust B.J., Kean L.S., Colonna L., Brandenstein K.E., Poole N.H., Obenza W., Enstrom M.R., Maldini C.R., Ellis G.I., Fennessey C.M. Robust expansion of HIV CAR T cells following antigen boosting in ART-suppressed nonhuman primates. Blood. 2020;136:1722–1734. doi: 10.1182/blood.2020006372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mancuso P., Chen C., Kaminski R., Gordon J., Liao S., Robinson J.A., Smith M.D., Liu H., Sariyer I.K., Sariyer R. CRISPR based editing of SIV proviral DNA in ART treated non-human primates. Nat. Commun. 2020;11:6065. doi: 10.1038/s41467-020-19821-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Uchida N., Li L., Nassehi T., Drysdale C.M., Yapundich M., Gamer J., Haro-Mora J.J., Demirci S., Leonard A., Bonifacino A.C. Preclinical evaluation for engraftment of CD34+ cells gene-edited at the sickle cell disease locus in xenograft mouse and non-human primate models. Cell Rep. Med. 2021;2:100247. doi: 10.1016/j.xcrm.2021.100247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Humbert O., Peterson C.W., Norgaard Z.K., Radtke S., Kiem H.P. A Nonhuman Primate Transplantation Model to Evaluate Hematopoietic Stem Cell Gene Editing Strategies for β-Hemoglobinopathies. Mol. Ther. Methods Clin. Dev. 2017;8:75–86. doi: 10.1016/j.omtm.2017.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Humbert O., Radtke S., Samuelson C., Carrillo R.R., Perez A.M., Reddy S.S., Lux C., Pattabhi S., Schefter L.E., Negre O. Therapeutically relevant engraftment of a CRISPR-Cas9-edited HSC-enriched population with HbF reactivation in nonhuman primates. Sci. Transl. Med. 2019;11:eaaw3768. doi: 10.1126/scitranslmed.aaw3768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Demirci S., Zeng J., Wu Y., Uchida N., Shen A.H., Pellin D., Gamer J., Yapundich M., Drysdale C., Bonanno J. BCL11A enhancer-edited hematopoietic stem cells persist in rhesus monkeys without toxicity. J. Clin. Invest. 2020;130:6677–6687. doi: 10.1172/JCI140189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim M.Y., Yu K.R., Kenderian S.S., Ruella M., Chen S., Shin T.H., Aljanahi A.A., Schreeder D., Klichinsky M., Shestova O. Genetic inactivation of CD33 in hematopoietic stem cells to enable CAR T cell immunotherapy for acute myeloid leukemia. Cell. 2018;173:1439–1453.e19. doi: 10.1016/j.cell.2018.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Walmsley G.L., Arechavala-Gomeza V., Fernandez-Fuente M., Burke M.M., Nagel N., Holder A., Stanley R., Chandler K., Marks S.L., Muntoni F. A duchenne muscular dystrophy gene hot spot mutation in dystrophin-deficient cavalier king charles spaniels is amenable to exon 51 skipping. PLoS ONE. 2010;5:e8647. doi: 10.1371/journal.pone.0008647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Amoasii L., Hildyard J.C.W., Li H., Sanchez-Ortiz E., Mireault A., Caballero D., Harron R., Stathopoulou T.R., Massey C., Shelton J.M. Gene editing restores dystrophin expression in a canine model of Duchenne muscular dystrophy. Science. 2018;362:86–91. doi: 10.1126/science.aau1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Klymiuk N., Blutke A., Graf A., Krause S., Burkhardt K., Wuensch A., Krebs S., Kessler B., Zakhartchenko V., Kurome M. Dystrophin-deficient pigs provide new insights into the hierarchy of physiological derangements of dystrophic muscle. Hum. Mol. Genet. 2013;22:4368–4382. doi: 10.1093/hmg/ddt287. [DOI] [PubMed] [Google Scholar]
- 65.Moretti A., Fonteyne L., Giesert F., Hoppmann P., Meier A.B., Bozoglu T., Baehr A., Schneider C.M., Sinnecker D., Klett K. Somatic gene editing ameliorates skeletal and cardiac muscle failure in pig and human models of Duchenne muscular dystrophy. Nat. Med. 2020;26:207–214. doi: 10.1038/s41591-019-0738-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang L., Smith J., Breton C., Clark P., Zhang J., Ying L., Che Y., Lape J., Bell P., Calcedo R. Meganuclease targeting of PCSK9 in macaque liver leads to stable reduction in serum cholesterol. Nat. Biotechnol. 2018;36:717–725. doi: 10.1038/nbt.4182. [DOI] [PubMed] [Google Scholar]
- 67.Wang L., Breton C., Warzecha C.C., Bell P., Yan H., He Z., White J., Zhu Y., Li M., Buza E.L. Long-term stable reduction of low-density lipoprotein in nonhuman primates following in vivo genome editing of PCSK9. Mol. Ther. 2021;29:2019–2029. doi: 10.1016/j.ymthe.2021.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Musunuru K., Chadwick A.C., Mizoguchi T., Garcia S.P., DeNizio J.E., Reiss C.W., Wang K., Iyer S., Dutta C., Clendaniel V. In vivo CRISPR base editing of PCSK9 durably lowers cholesterol in primates. Nature. 2021;593:429–434. doi: 10.1038/s41586-021-03534-y. [DOI] [PubMed] [Google Scholar]
- 69.Rothgangl T., Dennis M.K., Lin P.J.C., Oka R., Witzigmann D., Villiger L., Qi W., Hruzova M., Kissling L., Lenggenhager D. In vivo adenine base editing of PCSK9 in macaques reduces LDL cholesterol levels. Nat. Biotechnol. 2021;39:949–957. doi: 10.1038/s41587-021-00933-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Maeder M.L., Stefanidakis M., Wilson C.J., Baral R., Barrera L.A., Bounoutas G.S., Bumcrot D., Chao H., Ciulla D.M., DaSilva J.A. Development of a gene-editing approach to restore vision loss in Leber congenital amaurosis type 10. Nat. Med. 2019;25:229–233. doi: 10.1038/s41591-018-0327-9. [DOI] [PubMed] [Google Scholar]
- 71.McCullough K.T., Boye S.L., Fajardo D., Calabro K., Peterson J.J., Strang C.E., Chakraborty D., Gloskowski S., Haskett S., Samuelsson S. Somatic gene editing of GUCY2D by AAV-CRISPR/Cas9 alters retinal structure and function in mouse and macaque. Hum. Gene Ther. 2019;30:571–589. doi: 10.1089/hum.2018.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cardozo-Ojeda E.F., Duke E.R., Peterson C.W., Reeves D.B., Mayer B.T., Kiem H.P., Schiffer J.T. Thresholds for post-rebound SHIV control after CCR5 gene-edited autologous hematopoietic cell transplantation. eLife. 2021;10:e57646. doi: 10.7554/eLife.57646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mavigner M., Watkins B., Lawson B., Lee S.T., Chahroudi A., Kean L., Silvestri G. Persistence of virus reservoirs in ART-treated SHIV-infected rhesus macaques after autologous hematopoietic stem cell transplant. PLoS Pathog. 2014;10:e1004406. doi: 10.1371/journal.ppat.1004406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Peterson C.W., Benne C., Polacino P., Kaur J., McAllister C.E., Filali-Mouhim A., Obenza W., Pecor T.A., Huang M.L., Baldessari A. Loss of immune homeostasis dictates SHIV rebound after stem-cell transplantation. JCI Insight. 2017;2:e91230. doi: 10.1172/jci.insight.91230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Colonna L., Peterson C.W., Schell J.B., Carlson J.M., Tkachev V., Brown M., Yu A., Reddy S., Obenza W.M., Nelson V. Evidence for persistence of the SHIV reservoir early after MHC haploidentical hematopoietic stem cell transplantation. Nat. Commun. 2018;9:4438. doi: 10.1038/s41467-018-06736-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tebas P., Stein D., Tang W.W., Frank I., Wang S.Q., Lee G., Spratt S.K., Surosky R.T., Giedlin M.A., Nichol G. Gene editing of CCR5 in autologous CD4 T cells of persons infected with HIV. N. Engl. J. Med. 2014;370:901–910. doi: 10.1056/NEJMoa1300662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Xu L., Wang J., Liu Y., Xie L., Su B., Mou D., Wang L., Liu T., Wang X., Zhang B. CRISPR-edited stem cells in a patient with HIV and acute lymphocytic leukemia. N. Engl. J. Med. 2019;381:1240–1247. doi: 10.1056/NEJMoa1817426. [DOI] [PubMed] [Google Scholar]
- 78.Tebas P., Jadlowsky J.K., Shaw P.A., Tian L., Esparza E., Brennan A.L., Kim S., Naing S.Y., Richardson M.W., Vogel A.N. CCR5-edited CD4+ T cells augment HIV-specific immunity to enable post-rebound control of HIV replication. J. Clin. Invest. 2021;131:144486. doi: 10.1172/JCI144486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zeidan J., Sharma A.A., Lee G., Raad A., Fromentin R., Fourati S., Ghneim K., Sanchez G.P., Benne C., Canderan G. Infusion of CCR5 gene-edited T cells allows immune reconstitution, HIV reservoir decay, and long-term virological control. bioRxiv. 2021 doi: 10.1101/2021.1102.1128.433290. [DOI] [Google Scholar]
- 80.Sather B.D., Romano Ibarra G.S., Sommer K., Curinga G., Hale M., Khan I.F., Singh S., Song Y., Gwiazda K., Sahni J. Efficient modification of CCR5 in primary human hematopoietic cells using a megaTAL nuclease and AAV donor template. Sci. Transl. Med. 2015;7:307ra156. doi: 10.1126/scitranslmed.aac5530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hale M., Mesojednik T., Romano Ibarra G.S., Sahni J., Bernard A., Sommer K., Scharenberg A.M., Rawlings D.J., Wagner T.A. Engineering HIV-resistant, anti-HIV chimeric antigen receptor T cells. Mol. Ther. 2017;25:570–579. doi: 10.1016/j.ymthe.2016.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shin H.Y., Wang C., Lee H.K., Yoo K.H., Zeng X., Kuhns T., Yang C.M., Mohr T., Liu C., Hennighausen L. CRISPR/Cas9 targeting events cause complex deletions and insertions at 17 sites in the mouse genome. Nat. Commun. 2017;8:15464. doi: 10.1038/ncomms15464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Webber B.R., Lonetree C.L., Kluesner M.G., Johnson M.J., Pomeroy E.J., Diers M.D., Lahr W.S., Draper G.M., Slipek N.J., Smeester B.A. Highly efficient multiplex human T cell engineering without double-strand breaks using Cas9 base editors. Nat. Commun. 2019;10:5222. doi: 10.1038/s41467-019-13007-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hanlon K.S., Kleinstiver B.P., Garcia S.P., Zaborowski M.P., Volak A., Spirig S.E., Muller A., Sousa A.A., Tsai S.Q., Bengtsson N.E. High levels of AAV vector integration into CRISPR-induced DNA breaks. Nat. Commun. 2019;10:4439. doi: 10.1038/s41467-019-12449-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Modell B., Darlison M. Global epidemiology of haemoglobin disorders and derived service indicators. Bull. World Health Organ. 2008;86:480–487. doi: 10.2471/BLT.06.036673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rees D.C., Williams T.N., Gladwin M.T. Sickle-cell disease. Lancet. 2010;376:2018–2031. doi: 10.1016/S0140-6736(10)61029-X. [DOI] [PubMed] [Google Scholar]
- 87.Steinberg M.H. Management of sickle cell disease. N. Engl. J. Med. 1999;340:1021–1030. doi: 10.1056/NEJM199904013401307. [DOI] [PubMed] [Google Scholar]
- 88.Cao A., Galanello R. Beta-thalassemia. Genet. Med. 2010;12:61–76. doi: 10.1097/GIM.0b013e3181cd68ed. [DOI] [PubMed] [Google Scholar]
- 89.Ribeil J.A., Hacein-Bey-Abina S., Payen E., Magnani A., Semeraro M., Magrin E., Caccavelli L., Neven B., Bourget P., El Nemer W. Gene therapy in a patient with sickle cell disease. N. Engl. J. Med. 2017;376:848–855. doi: 10.1056/NEJMoa1609677. [DOI] [PubMed] [Google Scholar]
- 90.Thompson A.A., Walters M.C., Kwiatkowski J., Rasko J.E.J., Ribeil J.A., Hongeng S., Magrin E., Schiller G.J., Payen E., Semeraro M. Gene Therapy in Patients with Transfusion-Dependent β-Thalassemia. N. Engl. J. Med. 2018;378:1479–1493. doi: 10.1056/NEJMoa1705342. [DOI] [PubMed] [Google Scholar]
- 91.Cavazzana-Calvo M., Payen E., Negre O., Wang G., Hehir K., Fusil F., Down J., Denaro M., Brady T., Westerman K. Transfusion independence and HMGA2 activation after gene therapy of human β-thalassaemia. Nature. 2010;467:318–322. doi: 10.1038/nature09328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Okuno Y., Iwasaki H., Huettner C.S., Radomska H.S., Gonzalez D.A., Tenen D.G., Akashi K. Differential regulation of the human and murine CD34 genes in hematopoietic stem cells. Proc. Natl. Acad. Sci. USA. 2002;99:6246–6251. doi: 10.1073/pnas.092027799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Brehm M.A., Shultz L.D., Luban J., Greiner D.L. Overcoming current limitations in humanized mouse research. J. Infect. Dis. 2013;208(Suppl 2):S125–S130. doi: 10.1093/infdis/jit319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Li C., Wang H., Gil S., Georgakopoulou A., Radtke S., Yannaki E., Papayannopoulou T., Kiem H.P., Lieber A. In vivo HSC gene therapy for hemoglobinopathies: A proof of concept evaluation in rhesus macaques. Blood. 2020;136:46–47. [Google Scholar]
- 95.Cannon P., Asokan A., Czechowicz A., Hammond P., Kohn D.B., Lieber A., Malik P., Marks P., Porteus M., Verhoeyen E. Safe and effective in vivo targeting and gene editing in hematopoietic stem cells: strategies for accelerating development. Hum. Gene Ther. 2021;32:31–42. doi: 10.1089/hum.2020.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hoban M.D., Cost G.J., Mendel M.C., Romero Z., Kaufman M.L., Joglekar A.V., Ho M., Lumaquin D., Gray D., Lill G.R. Correction of the sickle cell disease mutation in human hematopoietic stem/progenitor cells. Blood. 2015;125:2597–2604. doi: 10.1182/blood-2014-12-615948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hoban M.D., Lumaquin D., Kuo C.Y., Romero Z., Long J., Ho M., Young C.S., Mojadidi M., Fitz-Gibbon S., Cooper A.R. CRISPR/Cas9-Mediated Correction of the Sickle Mutation in Human CD34+ cells. Mol. Ther. 2016;24:1561–1569. doi: 10.1038/mt.2016.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lomova A., Clark D.N., Campo-Fernandez B., Flores-Bjurström C., Kaufman M.L., Fitz-Gibbon S., Wang X., Miyahira E.Y., Brown D., DeWitt M.A. Improving gene editing outcomes in human hematopoietic stem and progenitor cells by temporal control of DNA repair. Stem Cells. 2019;37:284–294. doi: 10.1002/stem.2935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Park S.H., Lee C.M., Dever D.P., Davis T.H., Camarena J., Srifa W., Zhang Y., Paikari A., Chang A.K., Porteus M.H. Highly efficient editing of the β-globin gene in patient-derived hematopoietic stem and progenitor cells to treat sickle cell disease. Nucleic Acids Res. 2019;47:7955–7972. doi: 10.1093/nar/gkz475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Forget B.G. Molecular basis of hereditary persistence of fetal hemoglobin. Ann. N Y Acad. Sci. 1998;850:38–44. doi: 10.1111/j.1749-6632.1998.tb10460.x. [DOI] [PubMed] [Google Scholar]
- 101.Musallam K.M., Sankaran V.G., Cappellini M.D., Duca L., Nathan D.G., Taher A.T. Fetal hemoglobin levels and morbidity in untransfused patients with β-thalassemia intermedia. Blood. 2012;119:364–367. doi: 10.1182/blood-2011-09-382408. [DOI] [PubMed] [Google Scholar]
- 102.Sankaran V.G., Menne T.F., Xu J., Akie T.E., Lettre G., Van Handel B., Mikkola H.K., Hirschhorn J.N., Cantor A.B., Orkin S.H. Human fetal hemoglobin expression is regulated by the developmental stage-specific repressor BCL11A. Science. 2008;322:1839–1842. doi: 10.1126/science.1165409. [DOI] [PubMed] [Google Scholar]
- 103.Gilman J.G., Mishima N., Wen X.J., Stoming T.A., Lobel J., Huisman T.H. Distal CCAAT box deletion in the A gamma globin gene of two black adolescents with elevated fetal A gamma globin. Nucleic Acids Res. 1988;16:10635–10642. doi: 10.1093/nar/16.22.10635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Luc S., Huang J., McEldoon J.L., Somuncular E., Li D., Rhodes C., Mamoor S., Hou S., Xu J., Orkin S.H. Bcl11a deficiency leads to hematopoietic stem cell defects with an aging-like phenotype. Cell Rep. 2016;16:3181–3194. doi: 10.1016/j.celrep.2016.08.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Liu P., Keller J.R., Ortiz M., Tessarollo L., Rachel R.A., Nakamura T., Jenkins N.A., Copeland N.G. Bcl11a is essential for normal lymphoid development. Nat. Immunol. 2003;4:525–532. doi: 10.1038/ni925. [DOI] [PubMed] [Google Scholar]
- 106.Ippolito G.C., Dekker J.D., Wang Y.H., Lee B.K., Shaffer A.L., 3rd, Lin J., Wall J.K., Lee B.S., Staudt L.M., Liu Y.J. Dendritic cell fate is determined by BCL11A. Proc. Natl. Acad. Sci. USA. 2014;111:E998–E1006. doi: 10.1073/pnas.1319228111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bauer D.E., Kamran S.C., Lessard S., Xu J., Fujiwara Y., Lin C., Shao Z., Canver M.C., Smith E.C., Pinello L. An erythroid enhancer of BCL11A subject to genetic variation determines fetal hemoglobin level. Science. 2013;342:253–257. doi: 10.1126/science.1242088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wu Y., Zeng J., Roscoe B.P., Liu P., Yao Q., Lazzarotto C.R., Clement K., Cole M.A., Luk K., Baricordi C. Highly efficient therapeutic gene editing of human hematopoietic stem cells. Nat. Med. 2019;25:776–783. doi: 10.1038/s41591-019-0401-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Frangoul H., Altshuler D., Cappellini M.D., Chen Y.S., Domm J., Eustace B.K., Foell J., de la Fuente J., Grupp S., Handgretinger R. CRISPR-Cas9 Gene Editing for Sickle Cell Disease and β-Thalassemia. N. Engl. J. Med. 2021;384:252–260. doi: 10.1056/NEJMoa2031054. [DOI] [PubMed] [Google Scholar]
- 110.Neelapu S.S., Locke F.L., Bartlett N.L., Lekakis L.J., Miklos D.B., Jacobson C.A., Braunschweig I., Oluwole O.O., Siddiqi T., Lin Y. Axicabtagene ciloleucel CAR T-cell therapy in refractory large B-cell lymphoma. N. Engl. J. Med. 2017;377:2531–2544. doi: 10.1056/NEJMoa1707447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Schuster S.J., Bishop M.R., Tam C.S., Waller E.K., Borchmann P., McGuirk J.P., Jäger U., Jaglowski S., Andreadis C., Westin J.R., JULIET Investigators Tisagenlecleucel in adult relapsed or refractory diffuse large B-cell lymphoma. N. Engl. J. Med. 2019;380:45–56. doi: 10.1056/NEJMoa1804980. [DOI] [PubMed] [Google Scholar]
- 112.Abramson J.S., Palomba M.L., Gordon L.I., Lunning M.A., Wang M., Arnason J., Mehta A., Purev E., Maloney D.G., Andreadis C. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): a multicentre seamless design study. Lancet. 2020;396:839–852. doi: 10.1016/S0140-6736(20)31366-0. [DOI] [PubMed] [Google Scholar]
- 113.Wang M., Munoz J., Goy A., Locke F.L., Jacobson C.A., Hill B.T., Timmerman J.M., Holmes H., Jaglowski S., Flinn I.W. KTE-X19 CAR T-cell therapy in relapsed or refractory mantle-cell lymphoma. N. Engl. J. Med. 2020;382:1331–1342. doi: 10.1056/NEJMoa1914347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Munshi N.C., Anderson L.D., Jr., Shah N., Madduri D., Berdeja J., Lonial S., Raje N., Lin Y., Siegel D., Oriol A. Idecabtagene vicleucel in relapsed and refractory multiple myeloma. N. Engl. J. Med. 2021;384:705–716. doi: 10.1056/NEJMoa2024850. [DOI] [PubMed] [Google Scholar]
- 115.Taraseviciute A., Tkachev V., Ponce R., Turtle C.J., Snyder J.M., Liggitt H.D., Myerson D., Gonzalez-Cuyar L., Baldessari A., English C. Chimeric antigen receptor T cell-mediated neurotoxicity in nonhuman primates. Cancer Discov. 2018;8:750–763. doi: 10.1158/2159-8290.CD-17-1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ehninger A., Kramer M., Röllig C., Thiede C., Bornhäuser M., von Bonin M., Wermke M., Feldmann A., Bachmann M., Ehninger G., Oelschlägel U. Distribution and levels of cell surface expression of CD33 and CD123 in acute myeloid leukemia. Blood Cancer J. 2014;4:e218. doi: 10.1038/bcj.2014.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Taussig D.C., Pearce D.J., Simpson C., Rohatiner A.Z., Lister T.A., Kelly G., Luongo J.L., Danet-Desnoyers G.A., Bonnet D. Hematopoietic stem cells express multiple myeloid markers: implications for the origin and targeted therapy of acute myeloid leukemia. Blood. 2005;106:4086–4092. doi: 10.1182/blood-2005-03-1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Brinkman-Van der Linden E.C., Angata T., Reynolds S.A., Powell L.D., Hedrick S.M., Varki A. CD33/Siglec-3 binding specificity, expression pattern, and consequences of gene deletion in mice. Mol. Cell. Biol. 2003;23:4199–4206. doi: 10.1128/MCB.23.12.4199-4206.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Borot F., Wang H., Ma Y., Jafarov T., Raza A., Ali A.M., Mukherjee S. Gene-edited stem cells enable CD33-directed immune therapy for myeloid malignancies. Proc. Natl. Acad. Sci. USA. 2019;116:11978–11987. doi: 10.1073/pnas.1819992116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Mendell J.R., Shilling C., Leslie N.D., Flanigan K.M., al-Dahhak R., Gastier-Foster J., Kneile K., Dunn D.M., Duval B., Aoyagi A. Evidence-based path to newborn screening for Duchenne muscular dystrophy. Ann. Neurol. 2012;71:304–313. doi: 10.1002/ana.23528. [DOI] [PubMed] [Google Scholar]
- 121.Mah J.K., Korngut L., Dykeman J., Day L., Pringsheim T., Jette N. A systematic review and meta-analysis on the epidemiology of Duchenne and Becker muscular dystrophy. Neuromuscul. Disord. 2014;24:482–491. doi: 10.1016/j.nmd.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 122.Hoffman E.P., Brown R.H., Jr., Kunkel L.M. Dystrophin: the protein product of the Duchenne muscular dystrophy locus. Cell. 1987;51:919–928. doi: 10.1016/0092-8674(87)90579-4. [DOI] [PubMed] [Google Scholar]
- 123.Duan D., Goemans N., Takeda S., Mercuri E., Aartsma-Rus A. Duchenne muscular dystrophy. Nat. Rev. Dis. Primers. 2021;7:13. doi: 10.1038/s41572-021-00248-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bladen C.L., Salgado D., Monges S., Foncuberta M.E., Kekou K., Kosma K., Dawkins H., Lamont L., Roy A.J., Chamova T. The TREAT-NMD DMD Global Database: analysis of more than 7,000 Duchenne muscular dystrophy mutations. Hum. Mutat. 2015;36:395–402. doi: 10.1002/humu.22758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Aartsma-Rus A., Ginjaar I.B., Bushby K. The importance of genetic diagnosis for Duchenne muscular dystrophy. J. Med. Genet. 2016;53:145–151. doi: 10.1136/jmedgenet-2015-103387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Amoasii L., Long C., Li H., Mireault A.A., Shelton J.M., Sanchez-Ortiz E., McAnally J.R., Bhattacharyya S., Schmidt F., Grimm D. Single-cut genome editing restores dystrophin expression in a new mouse model of muscular dystrophy. Sci. Transl. Med. 2017;9:eaan8081. doi: 10.1126/scitranslmed.aan8081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kim K., Ryu S.M., Kim S.T., Baek G., Kim D., Lim K., Chung E., Kim S., Kim J.S. Highly efficient RNA-guided base editing in mouse embryos. Nat. Biotechnol. 2017;35:435–437. doi: 10.1038/nbt.3816. [DOI] [PubMed] [Google Scholar]
- 128.Koo T., Lu-Nguyen N.B., Malerba A., Kim E., Kim D., Cappellari O., Cho H.Y., Dickson G., Popplewell L., Kim J.S. Functional rescue of dystrophin deficiency in mice caused by frameshift mutations using Campylobacter jejuni Cas9. Mol. Ther. 2018;26:1529–1538. doi: 10.1016/j.ymthe.2018.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Amoasii L., Li H., Zhang Y., Min Y.L., Sanchez-Ortiz E., Shelton J.M., Long C., Mireault A.A., Bhattacharyya S., McAnally J.R. In vivo non-invasive monitoring of dystrophin correction in a new Duchenne muscular dystrophy reporter mouse. Nat. Commun. 2019;10:4537. doi: 10.1038/s41467-019-12335-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Egorova T.V., Zotova E.D., Reshetov D.A., Polikarpova A.V., Vassilieva S.G., Vlodavets D.V., Gavrilov A.A., Ulianov S.V., Buchman V.L., Deykin A.V. CRISPR/Cas9-generated mouse model of Duchenne muscular dystrophy recapitulating a newly identified large 430 kb deletion in the human DMD gene. Dis. Model. Mech. 2019;12:dmm037655. doi: 10.1242/dmm.037655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Min Y.L., Li H., Rodriguez-Caycedo C., Mireault A.A., Huang J., Shelton J.M., McAnally J.R., Amoasii L., Mammen P.P.A., Bassel-Duby R., Olson E.N. CRISPR-Cas9 corrects Duchenne muscular dystrophy exon 44 deletion mutations in mice and human cells. Sci. Adv. 2019;5:eaav4324. doi: 10.1126/sciadv.aav4324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Min Y.L., Chemello F., Li H., Rodriguez-Caycedo C., Sanchez-Ortiz E., Mireault A.A., McAnally J.R., Shelton J.M., Zhang Y., Bassel-Duby R., Olson E.N. Correction of three prominent mutations in mouse and human models of Duchenne muscular dystrophy by single-cut genome editing. Mol. Ther. 2020;28:2044–2055. doi: 10.1016/j.ymthe.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Larcher T., Lafoux A., Tesson L., Remy S., Thepenier V., François V., Le Guiner C., Goubin H., Dutilleul M., Guigand L. Characterization of dystrophin deficient rats: a new model for Duchenne muscular dystrophy. PLoS ONE. 2014;9:e110371. doi: 10.1371/journal.pone.0110371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Nakamura K., Fujii W., Tsuboi M., Tanihata J., Teramoto N., Takeuchi S., Naito K., Yamanouchi K., Nishihara M. Generation of muscular dystrophy model rats with a CRISPR/Cas system. Sci. Rep. 2014;4:5635. doi: 10.1038/srep05635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sui T., Lau Y.S., Liu D., Liu T., Xu L., Gao Y., Lai L., Li Z., Han R. A novel rabbit model of Duchenne muscular dystrophy generated by CRISPR/Cas9. Dis. Model. Mech. 2018;11:dmm032201. doi: 10.1242/dmm.032201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Xie J., Ge W., Li N., Liu Q., Chen F., Yang X., Huang X., Ouyang Z., Zhang Q., Zhao Y. Efficient base editing for multiple genes and loci in pigs using base editors. Nat. Commun. 2019;10:2852. doi: 10.1038/s41467-019-10421-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Chen Y., Zheng Y., Kang Y., Yang W., Niu Y., Guo X., Tu Z., Si C., Wang H., Xing R. Functional disruption of the dystrophin gene in rhesus monkey using CRISPR/Cas9. Hum. Mol. Genet. 2015;24:3764–3774. doi: 10.1093/hmg/ddv120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Yokota T., Duddy W., Partridge T. Optimizing exon skipping therapies for DMD. Acta Myol. 2007;26:179–184. [PMC free article] [PubMed] [Google Scholar]
- 139.Godfrey C., Muses S., McClorey G., Wells K.E., Coursindel T., Terry R.L., Betts C., Hammond S., O’Donovan L., Hildyard J. How much dystrophin is enough: the physiological consequences of different levels of dystrophin in the mdx mouse. Hum. Mol. Genet. 2015;24:4225–4237. doi: 10.1093/hmg/ddv155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.van Putten M., van der Pijl E.M., Hulsker M., Verhaart I.E., Nadarajah V.D., van der Weerd L., Aartsma-Rus A. Low dystrophin levels in heart can delay heart failure in mdx mice. J. Mol. Cell. Cardiol. 2014;69:17–23. doi: 10.1016/j.yjmcc.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 141.Truong D.J., Kühner K., Kühn R., Werfel S., Engelhardt S., Wurst W., Ortiz O. Development of an intein-mediated split-Cas9 system for gene therapy. Nucleic Acids Res. 2015;43:6450–6458. doi: 10.1093/nar/gkv601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Lagace T.A., Curtis D.E., Garuti R., McNutt M.C., Park S.W., Prather H.B., Anderson N.N., Ho Y.K., Hammer R.E., Horton J.D. Secreted PCSK9 decreases the number of LDL receptors in hepatocytes and in livers of parabiotic mice. J. Clin. Invest. 2006;116:2995–3005. doi: 10.1172/JCI29383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Maxwell K.N., Fisher E.A., Breslow J.L. Overexpression of PCSK9 accelerates the degradation of the LDLR in a post-endoplasmic reticulum compartment. Proc. Natl. Acad. Sci. USA. 2005;102:2069–2074. doi: 10.1073/pnas.0409736102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Abifadel M., Varret M., Rabès J.P., Allard D., Ouguerram K., Devillers M., Cruaud C., Benjannet S., Wickham L., Erlich D. Mutations in PCSK9 cause autosomal dominant hypercholesterolemia. Nat. Genet. 2003;34:154–156. doi: 10.1038/ng1161. [DOI] [PubMed] [Google Scholar]
- 145.Cohen J.C., Boerwinkle E., Mosley T.H., Jr., Hobbs H.H. Sequence variations in PCSK9, low LDL, and protection against coronary heart disease. N. Engl. J. Med. 2006;354:1264–1272. doi: 10.1056/NEJMoa054013. [DOI] [PubMed] [Google Scholar]
- 146.Cohen J., Pertsemlidis A., Kotowski I.K., Graham R., Garcia C.K., Hobbs H.H. Low LDL cholesterol in individuals of African descent resulting from frequent nonsense mutations in PCSK9. Nat. Genet. 2005;37:161–165. doi: 10.1038/ng1509. [DOI] [PubMed] [Google Scholar]
- 147.Kent S.T., Rosenson R.S., Avery C.L., Chen Y.I., Correa A., Cummings S.R., Cupples L.A., Cushman M., Evans D.S., Gudnason V. PCSK9 Loss-of-Function Variants, Low-Density Lipoprotein Cholesterol, and Risk of Coronary Heart Disease and Stroke: Data From 9 Studies of Blacks and Whites. Circ. Cardiovasc. Genet. 2017;10:e001632. doi: 10.1161/CIRCGENETICS.116.001632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Sabatine M.S., Giugliano R.P., Keech A.C., Honarpour N., Wiviott S.D., Murphy S.A., Kuder J.F., Wang H., Liu T., Wasserman S.M., FOURIER Steering Committee and Investigators Evolocumab and clinical outcomes in patients with cardiovascular disease. N. Engl. J. Med. 2017;376:1713–1722. doi: 10.1056/NEJMoa1615664. [DOI] [PubMed] [Google Scholar]
- 149.Robinson J.G., Farnier M., Krempf M., Bergeron J., Luc G., Averna M., Stroes E.S., Langslet G., Raal F.J., El Shahawy M., ODYSSEY LONG TERM Investigators Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. N. Engl. J. Med. 2015;372:1489–1499. doi: 10.1056/NEJMoa1501031. [DOI] [PubMed] [Google Scholar]
- 150.Breton C., Clark P.M., Wang L., Greig J.A., Wilson J.M. ITR-Seq, a next-generation sequencing assay, identifies genome-wide DNA editing sites in vivo following adeno-associated viral vector-mediated genome editing. BMC Genomics. 2020;21:239. doi: 10.1186/s12864-020-6655-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Gaudelli N.M., Lam D.K., Rees H.A., Solá-Esteves N.M., Barrera L.A., Born D.A., Edwards A., Gehrke J.M., Lee S.J., Liquori A.J. Directed evolution of adenine base editors with increased activity and therapeutic application. Nat. Biotechnol. 2020;38:892–900. doi: 10.1038/s41587-020-0491-6. [DOI] [PubMed] [Google Scholar]
- 152.Petri K., Kim D.Y., Sasaki K.E., Canver M.C., Wang X., Shah H., Lee H., Horng J.E., Clement K., Iyer S. Global-scale CRISPR gene editor specificity profiling by ONE-seq identifies population-specific, variant off-target effects. bioRxiv. 2021 doi: 10.1101/2021.04.05.438458. [DOI] [Google Scholar]
- 153.Koblan L.W., Doman J.L., Wilson C., Levy J.M., Tay T., Newby G.A., Maianti J.P., Raguram A., Liu D.R. Improving cytidine and adenine base editors by expression optimization and ancestral reconstruction. Nat. Biotechnol. 2018;36:843–846. doi: 10.1038/nbt.4172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Quinn J., Musa A., Kantor A., McClements M.E., Cehajic-Kapetanovic J., MacLaren R.E., Xue K. Genome-editing strategies for treating human retinal degenerations. Hum. Gene Ther. 2021;32:247–259. doi: 10.1089/hum.2020.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Berger W., Kloeckener-Gruissem B., Neidhardt J. The molecular basis of human retinal and vitreoretinal diseases. Prog. Retin. Eye Res. 2010;29:335–375. doi: 10.1016/j.preteyeres.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 156.Russell S., Bennett J., Wellman J.A., Chung D.C., Yu Z.F., Tillman A., Wittes J., Pappas J., Elci O., McCague S. Efficacy and safety of voretigene neparvovec (AAV2-hRPE65v2) in patients with RPE65-mediated inherited retinal dystrophy: a randomised, controlled, open-label, phase 3 trial. Lancet. 2017;390:849–860. doi: 10.1016/S0140-6736(17)31868-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Moshiri A., Chen R., Kim S., Harris R.A., Li Y., Raveendran M., Davis S., Liang Q., Pomerantz O., Wang J. A nonhuman primate model of inherited retinal disease. J. Clin. Invest. 2019;129:863–874. doi: 10.1172/JCI123980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Koenekoop R.K. An overview of Leber congenital amaurosis: a model to understand human retinal development. Surv. Ophthalmol. 2004;49:379–398. doi: 10.1016/j.survophthal.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 159.Stone E.M. Leber congenital amaurosis - a model for efficient genetic testing of heterogeneous disorders: LXIV Edward Jackson Memorial Lecture. Am. J. Ophthalmol. 2007;144:791–811. doi: 10.1016/j.ajo.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 160.Perrault I., Rozet J.M., Gerber S., Ghazi I., Leowski C., Ducroq D., Souied E., Dufier J.L., Munnich A., Kaplan J. Leber congenital amaurosis. Mol. Genet. Metab. 1999;68:200–208. doi: 10.1006/mgme.1999.2906. [DOI] [PubMed] [Google Scholar]
- 161.den Hollander A.I., Roepman R., Koenekoop R.K., Cremers F.P. Leber congenital amaurosis: genes, proteins and disease mechanisms. Prog. Retin. Eye Res. 2008;27:391–419. doi: 10.1016/j.preteyeres.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 162.Chacon-Camacho O.F., Zenteno J.C. Review and update on the molecular basis of Leber congenital amaurosis. World J. Clin. Cases. 2015;3:112–124. doi: 10.12998/wjcc.v3.i2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.den Hollander A.I., Koenekoop R.K., Yzer S., Lopez I., Arends M.L., Voesenek K.E., Zonneveld M.N., Strom T.M., Meitinger T., Brunner H.G. Mutations in the CEP290 (NPHP6) gene are a frequent cause of Leber congenital amaurosis. Am. J. Hum. Genet. 2006;79:556–561. doi: 10.1086/507318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Geller A.M., Sieving P.A. Assessment of foveal cone photoreceptors in Stargardt’s macular dystrophy using a small dot detection task. Vision Res. 1993;33:1509–1524. doi: 10.1016/0042-6989(93)90144-l. [DOI] [PubMed] [Google Scholar]
- 165.Payne A.M., Morris A.G., Downes S.M., Johnson S., Bird A.C., Moore A.T., Bhattacharya S.S., Hunt D.M. Clustering and frequency of mutations in the retinal guanylate cyclase (GUCY2D) gene in patients with dominant cone-rod dystrophies. J. Med. Genet. 2001;38:611–614. doi: 10.1136/jmg.38.9.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Kitiratschky V.B., Wilke R., Renner A.B., Kellner U., Vadalà M., Birch D.G., Wissinger B., Zrenner E., Kohl S. Mutation analysis identifies GUCY2D as the major gene responsible for autosomal dominant progressive cone degeneration. Invest. Ophthalmol. Vis. Sci. 2008;49:5015–5023. doi: 10.1167/iovs.08-1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Gregory-Evans K., Kelsell R.E., Gregory-Evans C.Y., Downes S.M., Fitzke F.W., Holder G.E., Simunovic M., Mollon J.D., Taylor R., Hunt D.M. Autosomal dominant cone-rod retinal dystrophy (CORD6) from heterozygous mutation of GUCY2D, which encodes retinal guanylate cyclase. Ophthalmology. 2000;107:55–61. doi: 10.1016/s0161-6420(99)00038-x. [DOI] [PubMed] [Google Scholar]
- 168.Harding J., Roberts R.M., Mirochnitchenko O. Large animal models for stem cell therapy. Stem Cell Res. Ther. 2013;4:23. doi: 10.1186/scrt171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Lee W.G., Demirci U., Khademhosseini A. Microscale electroporation: challenges and perspectives for clinical applications. Integr. Biol. 2009;1:242–251. doi: 10.1039/b819201d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Peterson C.W., Kiem H.P. Lessons from London and Berlin: Designing a scalable gene therapy approach for HIV cure. Cell Stem Cell. 2019;24:685–687. doi: 10.1016/j.stem.2019.04.010. [DOI] [PubMed] [Google Scholar]
- 171.Wang H., Gil S., Li G., Doering C., Ng P., Roffler S., Kiem H.P., Lieber A.L. In vivo HSC gene therapy with high-level, erythroid-specific expression of a secreted SARS-CoV-2 decoy receptor (abstract) Mol. Ther. 2021;29(Suppl 1):91–92. [Google Scholar]
- 172.Li C., Wang H., Georgakopoulou A., Gil S., Yannaki E., Lieber A. In Vivo HSC Gene Therapy Using a Bi-modular HDAd5/35++ Vector Cures Sickle Cell Disease in a Mouse Model. Mol. Ther. 2021;29:822–837. doi: 10.1016/j.ymthe.2020.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Liu S., Cheng Q., Wei T., Yu X., Johnson L.T., Farbiak L., Siegwart D.J. Membrane-destabilizing ionizable phospholipids for organ-selective mRNA delivery and CRISPR-Cas gene editing. Nat. Mater. 2021;20:701–710. doi: 10.1038/s41563-020-00886-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Li C., Lieber A. Adenovirus vectors in hematopoietic stem cell genome editing. FEBS Lett. 2019;593:3623–3648. doi: 10.1002/1873-3468.13668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Rosenblum D., Gutkin A., Kedmi R., Ramishetti S., Veiga N., Jacobi A.M., Schubert M.S., Friedmann-Morvinski D., Cohen Z.R., Behlke M.A. CRISPR-Cas9 genome editing using targeted lipid nanoparticles for cancer therapy. Sci. Adv. 2020;6:eabc9450. doi: 10.1126/sciadv.abc9450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Song C.Q., Jiang T., Richter M., Rhym L.H., Koblan L.W., Zafra M.P., Schatoff E.M., Doman J.L., Cao Y., Dow L.E. Adenine base editing in an adult mouse model of tyrosinaemia. Nat. Biomed. Eng. 2020;4:125–130. doi: 10.1038/s41551-019-0357-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


