Abstract
Background
Immunotherapy is the first‐line treatment for melanoma and lung cancer and brings new risks of immune‐related adverse events. We aimed to describe patients’ knowledge about risks, benefits, and goals of immunotherapy.
Materials and Methods
We conducted a cross‐sectional study of patients with advanced melanoma or non‐small cell lung cancer that used a 9‐item knowledge survey and questions from the Prognosis and Treatment Perceptions Questionnaire.
Results
We surveyed 105 participants (57 with melanoma, 48 with lung cancer) with median age 69 years (range 36–89). Participants’ responses revealed knowledge deficits about immunotherapy mechanism of action and lack of awareness about the timing and severity of side effects. One third (34%; 36/105) of participants reported that the primary goal of their treatment is to cure their cancer.
Conclusion
Given the widespread use of immunotherapy, patients would benefit from educational tools so that they know what to expect regarding side effects and prognosis.
Short abstract
Individual experiences with immunotherapy are varied. This article describes patients’ knowledge about the risks, benefits, and goals of immunotherapy treatment.
Introduction
Immunotherapy is the standard first‐line treatment for most patients with advanced melanoma and lung cancer [1, 2]. Immunotherapy extends survival and leads to durable responses in some patients, yet individual experiences are varied [3]. Prior studies have found that patients with incurable cancer commonly misperceive that the goal of their treatment with chemotherapy is to cure, yet how patients perceive the curative potential of immunotherapy in the setting of advanced cancer has not yet been studied [4]. In addition, immunotherapy poses new risks of immune‐related adverse events that require prompt recognition in order to limit morbidity and mortality [5]. In this cross‐sectional study, we aimed to describe patients’ knowledge about the risks, benefits, and goals of immunotherapy treatment.
Materials and Methods
We conducted a survey of patients at a single institution who had initiated therapy with an immune checkpoint inhibitor within the past 12 weeks for advanced (stage IV or unresectable stage III) melanoma or non‐small cell lung cancer (including patients receiving chemoimmunotherapy for lung cancer). The Dana‐Farber/Harvard Cancer Center Institutional Review Board approved this study. We identified potentially eligible patients by electronic health record screen and approached them in person during infusion or by telephone to obtain informed consent. Study participants completed the survey on paper, verbally, or remotely using an electronic data capture tool (REDCap) based on their preferences. The survey included a 9‐item knowledge questionnaire comprising true/false questions about immunotherapy designed by a multidisciplinary team of clinicians (including oncology, palliative care, and psychology) and piloted with five patients with exit interviews to obtain feedback and make refinements prior to enrolling the remainder of the cohort. The survey also included questions about treatment goals from the Prognosis and Treatment Perceptions Questionnaire (PTPQ) [6]. We summarized responses using descriptive statistics. The knowledge questionnaire was scored using a 0–100 scale, with higher scores indicating better knowledge. We used PTPQ items to ask participants about the primary goal of their treatment and we dichotomized responses into “to cure my cancer” versus all other options as in prior studies [6]. For a question that asked about the likelihood that immunotherapy is curative using a Likert scale of responses that ranged from “Extremely likely (>90% chance)” to “Not at all likely” (≤10% chance),” we dichotomized responses into “Likely (>25% chance)” or “Unlikely (≤25% chance)” [7]. We compared knowledge and prognostic understanding between patients with melanoma versus lung cancer using two‐sample t test and Chi‐square tests, respectively.
Results
We approached 156 patients to participate between May 2019 and January 2021, and 115 patients enrolled. A total of 105 participants (57 with melanoma, 48 with lung cancer) completed the survey; 10 patients deferred the survey after providing consent and were lost to follow‐up. Participants had a median age of 69 years (range 36–89) and 33% (35/105) were female. Most had completed at least a year of college (76.7%) and 73.3% felt “very” or “extremely” confident filling out medical forms. Most participants received pembrolizumab (79/105 [75.0%]; 34/105 [32.4%] in combination with chemotherapy), 20.0% received ipilimumab and nivolumab, 2.9% received nivolumab, and 1.9% received atezolizumab. All received immunotherapy as standard treatment (i.e., were not in a clinical trial). The mean knowledge score was 69.0 (SD = 23.3). Participants with melanoma had higher mean knowledge scores than patients with lung cancer (74.7 vs. 62.3, p = .003). Participants’ responses to knowledge questions are shown in Figure 1. With respect to immunotherapy side effects, 68% (71/105) of patients reported that side effects can affect any organ in the body and 65% (68/105) endorsed that side effects can occur at any time, even after the treatment ends. Figure 2 depicts participants’ perceptions of their treatment goal. Overall, 40% (41/103) of participants responded that there was at least a 25% chance that immunotherapy could cure stage IV cancer and 34% (36/105) of participants endorsed that the primary goal of their treatment is to cure their cancer. Participants with melanoma were more likely than those with lung cancer to report that their treatment goal is to cure (58% [33/57] vs. 6% [3/48], p < .001), and that their oncologist had said that immunotherapy would cure their cancer (19% [11/57] vs. 0% [0/48], p = .005).
Figure 1.
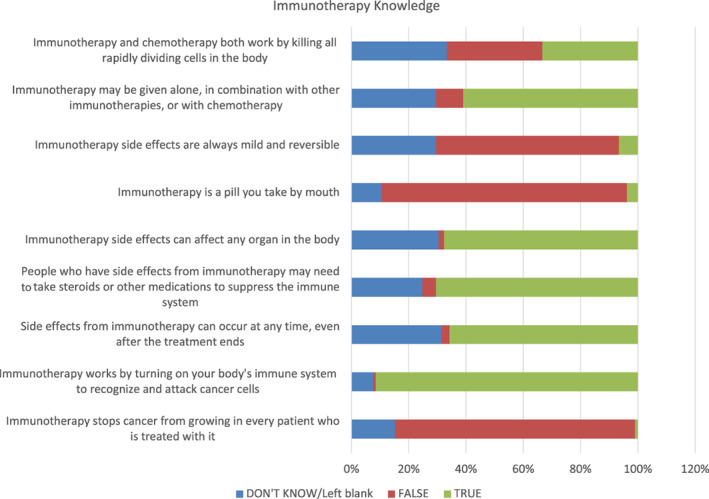
Participant knowledge about immunotherapy. Bars are percentage of participants who provided each response.
Figure 2.
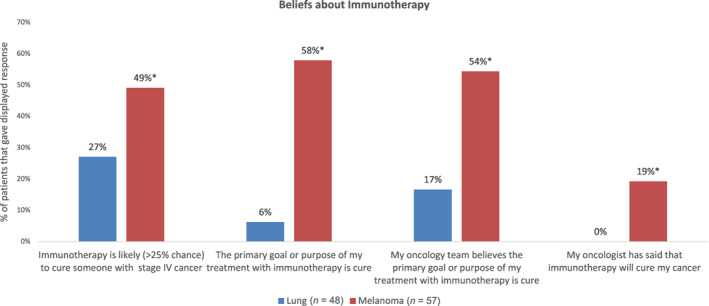
Participant responses regarding their beliefs about the curative intent of immunotherapy. Results are shown by participants’ cancer type (non‐small cell lung cancer vs. melanoma). Bars are proportion of participants that provided the responses shown. Asterisks indicate a statistically significant difference between groups.
Discussion
In this cross‐sectional sample of patients with a confirmed diagnosis of melanoma or lung cancer, we observed substantial knowledge deficits about immunotherapy and prevalent expectations that immunotherapy is curative in the metastatic setting, particularly among patients with melanoma. Although individual preferences vary, most patients prefer to receive as much information as possible in order to be active participants in their cancer care. Treatment‐related information (information about side effects, treatment options, and alternatives) is the most frequently named information need among patients with cancer [8]. Oncology teams thoroughly counsel patients about risks and benefits of treatment as part of the informed consent process and in preparation for the first infusion of a new treatment. However, patients commonly struggle to recall the information their oncologists provide, and these results demonstrate that patients receiving immunotherapy are no exception [9]. Participants in this study lacked awareness about the timing, severity, reversibility, and presentation of side effects, knowledge deficits that might affect their behavior with regard to recognizing and seeking care for potential immune‐related adverse events.
In addition, understanding of the goal of therapy is an important component of prognostic awareness. Patients with accurate understanding of the goal of their cancer treatment are more likely to receive care that is consistent with their preferences at the end of life [10]. Prior studies have found that 69% of patients with incurable lung cancer perceived that the chemotherapy they received was intended to cure; a much smaller percentage of patients with lung cancer in this study (6%) perceived that immunotherapy was curative [4]. The finding that most patients with melanoma (58%) perceived immunotherapy as curative likely reflects oncologists’ warranted optimism regarding the long‐term durable responses that a significant minority of patients experience [11]. Given the heterogeneity of possible treatment outcomes, however, future research should investigate how best to communicate uncertainty to patients.
This study is limited by its sample size and recruitment from a single academic medical center, although the knowledge deficiencies we observed in this sample with high self‐reported health literacy likely underestimate those of the general population of patients receiving immunotherapy.
Conclusion
These findings highlight the need for educational tools for patients initiating treatment with immunotherapy to supplement the communication of information by oncology teams.
Disclosures
Ryan Sullivan: Asana Biosciences, AstraZeneca, Bristol‐Myers Squibb, Eisai, Iovance, Merck, Novartis, OncoSec, Pfizer, Replimmune (C/A), Merck, Amgen (RF); Angelo Volandes: ACP Decisions (E [spouse]); Joseph A. Greer: Blue Note Therapeutics (C/A), Blue Note Therapeutics, Gaido Health/BCG Digital Ventures (RF), Springer/Humana Press (royalties). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
Supporting information
See http://www.TheOncologist.com for supplemental material available online.
Appendix S1: Supporting information
Acknowledgments
We thank the patients who participated in this study, as well as Dr. Karen Donelan for her advice in creating the immunotherapy knowledge survey and Robert Sommer for his study administration support. We also acknowledge the REDCap electronic data capture instrument (Harris PA, Taylor R, Thielke R et al. J Biomed Inform 2009;42:377–381). This work was supported by an American Society of Clinical Oncology Conquer Cancer Career Development Award (Petrillo).
No part of this article may be reproduced, stored, or transmitted in any form or for any means without the prior permission in writing from the copyright holder. For information on purchasing reprints contact commercialreprints@wiley.com. For permission information contact permissions@wiley.com.
Disclosures of potential conflicts of interest may be found at the end of this article.
References
- 1. Gandhi L, Rodríguez‐Abreu D, Gadgeel S et al. Pembrolizumab plus chemotherapy in metastatic non–small‐cell lung cancer. N Engl J Med 2018;378:2078–2092. [DOI] [PubMed] [Google Scholar]
- 2. Larkin J, Chiarion‐Sileni V, Gonzalez R et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med 2015;373:23–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Betof Warner A, Palmer JS, Shoushtari AN et al. Long‐term outcomes and responses to retreatment in patients with melanoma treated with PD‐1 blockade. J Clin Oncol 2020;38:1655–1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Weeks JC, Catalano PJ, Cronin A et al. Patients’ expectations about effects of chemotherapy for advanced cancer. N Engl J Med 2012;367:1616–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brahmer JR, Lacchetti C, Schneider BJ et al. Management of immune‐related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 2018;36:1714–1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. El‐Jawahri A, Traeger L, Park ER et al. Associations among prognostic understanding, quality of life, and mood in patients with advanced cancer. Cancer 2014;120278–285. [DOI] [PubMed] [Google Scholar]
- 7. Winner M, Wilson A, Yahanda A et al. A cross‐sectional study of patient and provider perception of “cure” as a goal of cancer surgery. J Surg Oncol 2016;114:677–683. [DOI] [PubMed] [Google Scholar]
- 8. Rutten LJF, Arora NK, Bakos AD, Aziz N, Rowland J. Information needs and sources of information among cancer patients: a systematic review of research (1980–2003). Patient Educ Couns 2005;57:250–261. [DOI] [PubMed] [Google Scholar]
- 9. Jansen J, Butow PN, van Weert JCM et al. Does age really matter? Recall of information presented to newly referred patients with cancer. J Clin Oncol 2008;26:5450–5457. [DOI] [PubMed] [Google Scholar]
- 10. Mack JW, Walling A, Dy S et al. Patient beliefs that chemotherapy may be curative and care received at the end of life among patients with metastatic lung and colorectal cancer. Cancer 2015;121:1891–1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wolchok JD, Chiarion‐Sileni V, Gonzalez R et al. CheckMate 067: 6.5‐year outcomes in patients (pts) with advanced melanoma. J Clin Oncol 2021;39(suppl 15):9506–9506. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
See http://www.TheOncologist.com for supplemental material available online.
Appendix S1: Supporting information


