Abstract
The ubiquitously present gram-negative bacteria Pantoea agglomerans is not a commonly known human pathogen. Recently, increasing recognition of the species as a human pathogen has led to controversy as limited documented cases of P. agglomerans bacteremia and infections have been reported in the literature, with most cases reported among immunocompromised patients or the pediatric population. Here, we present the case of a 54-year-old female with P. agglomerans and Enterococcus faecium bacteremia along with chronic obstructive pulmonary disease.
Keywords: chronic obstructive pulmonary disease, copd, pantoea agglomerans, bacteremia, copd exacerbation, gram-negative bacteria
Introduction
The genus Pantoea, gram-negative rods with yellow pigmentation belonging to the Erwiniaceae family, has been reported to cause opportunistic infections in immunocompromised patients. Only a few cases of spontaneous Pantoea agglomerans bacteremia have been reported, mostly among pediatric, hospitalized, immunocompromised, or cancer patients [1-3]. Although it is present in the soil, plant surfaces, human excreta, vegetables, and fruits, it is known to jump kingdoms and cause a clinical spectrum of diseases ranging from diarrhea, sepsis, arthritis, osteomyelitis, synovitis, urinary tract infections, pneumonia, to septic shock in humans [3-5]. The impact of P. agglomerans bacteremia remains largely unknown in chronic respiratory disorders such as chronic obstructive pulmonary disease (COPD).
Case presentation
A 54-year-old female with a history of (Global Initiative for Chronic Obstructive Lung Disease stage 3 and group D) multiple COPD exacerbations and one with endotracheal intubation, without home oxygen, 16 pack-year cigarette smoking, and marijuana abuse came to the emergency department for worsening shortness of breath with nonproductive cough, myalgia, and watery diarrhea for three days. Other systems were normal.
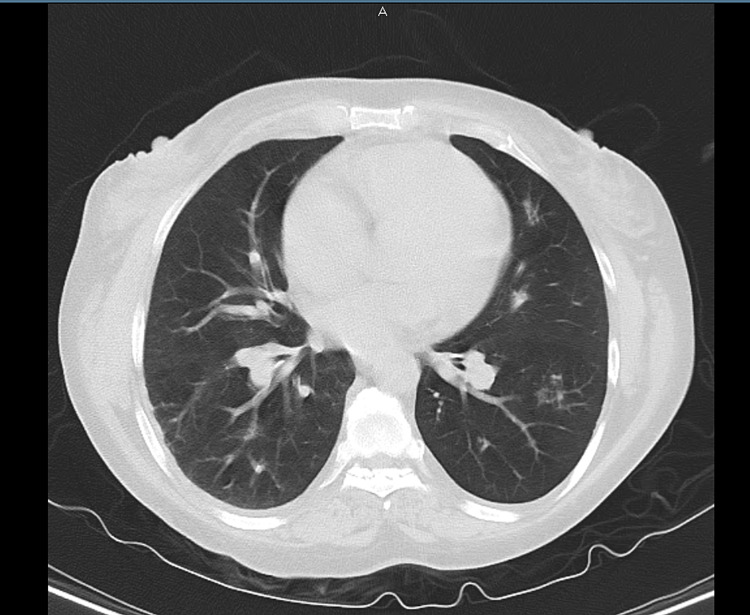
At presentation, she was afebrile, with a heart rate of 112 beats per minute, respiratory rate of 30 breaths per minute, and saturation of 95-98% on 3 L of oxygen on nasal cannula. Bilateral wheezing with few crepitations was noted on the bilateral bases of the lungs. The rest of the examination was unremarkable. Labs at the time of admission showed leukocytosis of 15.6 × 109/L (reference range: 4.5-11 × 109/L) with a left shift of neutrophils at 88.3% and relative lymphopenia at 4.5% (0.7 × 109/L). The chemistry panel was near-normal with the following findings: Na+/K+ of 139/3.9 mmol/L, Cl- of 97 mmol/L, elevated HCO3 of 32 mEeq/L, and normal anion gap of 10. Blood urea nitrogen (BUN)/creatinine ratio was 13.0/0.66 mg/dL, with a slightly elevated glucose level of 173 mg/dL. Furthermore, calcium, phosphorus, and magnesium levels were 8.9 mg/dL, 5.3 mg/dL, and 1.9 mg/dL, respectively. Liver function tests showed total bilirubin of 0.5 mg/dL, aspartate transaminase of 14 U/L, alanine transaminase of 13 U/L, alkaline phosphatase of 119 U/L, total protein of 5.9 g/dL, albumin of 3.7 m/dL, and elevated bicarbonate of 35.7 mEq/L. Moreover, urine toxicology was positive for cannabinoids. Polymerase chain reaction (PCR) test for coronavirus disease 2019 (COVID-19) was negative, and influenza, mycoplasma, and Legionella antigen tests were also negative. Lactate dehydrogenase was elevated at 322 U/L (reference range: 125-220 U/L), and total creatine kinase was 43 U/L. D-dimer was 414 ng/mL with a normal coagulation profile with prothrombin time (PT) of 12.8 seconds and activated partial thromboplastin time of 31.3 seconds. PT/international normalized ratio was 1.09. Chest X-ray showed hyperinflation with mild perihilar congestion without any evidence of consolidation and no significant changes compared with the prior study. Computed tomography (CT) without contrast revealed mildly hyperinflated lungs with mild emphysematous changes predominating in the apices, along with scattered small areas of fibrotic changes. No convincing lung consolidation or acute infiltrate pleural effusion was noted, with normal mediastinum, heart size, and unremarkable hila with pericardial effusion (Figure 1).
Figure 1. CT chest showing no consolidation and emphysematous changes due to COPD. Incidental finding of small GGO in the left lower lobe.
CT: computed tomography; COPD: chronic obstructive pulmonary disease; GGO: ground-glass opacities
Arterial blood gas (ABG) on 2 L of oxygen via nasal cannula showed pH of 7.299, pCO2 of 75 mmHg, pO2 of 72.9 mmHg, HCO3- of 35 mmol/L, and oxygen saturation of 96%. Sequential Organ Failure Assessment (SOFA) score was less than 2 (less than 9 implies <33.3% mortality), and PaO2/FiO2 ratio was 260. She was admitted to the hospital for acute hypoxic and hypercapnic respiratory failure secondary to COPD exacerbation and was started on methylprednisolone along with albuterol and ipratropium nebulization and intravenous ceftriaxone and azithromycin. Her clinical course worsened on days two and three of admission with tachypnea, fatigue, as well as occasional and multiple episodes of desaturation of up to 86% on 2 L of oxygen via a nasal cannula. She was switched to bilevel positive airway pressure (BiPAP) with inspiratory positive airway pressure/expiratory positive airway pressure of 15/5 mmHg, with a respiratory rate of 15 breaths per minute and FiO2 of 40% due to worsening respiratory status. Two repeat PCR tests for COVID-19 were negative. Blood culture sent at the time of admission grew two organisms later identified as E. faecium and P. agglomerans.
She was fairly compliant with BiPAP, and on day four of admission, she started improving clinically and reported feeling comfortable on 2-3 L of oxygen via a nasal cannula with on and off BiPAP (approximately six to seven hours) during the night. Her ABG on BiPAP with FiO2 of 40% oxygen also showed improvement with pH of 7.339, pCO2 of 63.7 mmHg, pO2 of 87.2 mmHg, HCO3- of 33 mmol/L, and oxygen saturation of 97%. Antibiotic sensitivity analysis of E. faecium and P. agglomerans revealed that both were sensitive to ceftriaxone. Therefore, ceftriaxone and azithromycin were continued for five days, with a continued tapering dose of steroids.
Of note, another set of blood cultures sent on the day of admission and on days two and three during deterioration showed no growth in the subsequent follow-up. On day six of admission, the patient improved significantly and was discharged home with home oxygen therapy with proper instructions regarding the medication and oxygen therapy. On the two-week follow-up at the medical clinic, she reported remarkable improvement in respiratory symptoms and was using oxygen during nights with the occasional need for inhaler use.
Discussion
Pantoea species are yellow-pigmented, Gram-negative, rod-shaped, aerobic bacteria belonging to the Erwiniaceae family. Based on shared protein homologs, it was previously classified in the Enterobacteriaceae family along with Klebsiella, Escherichia, Salmonella, and Enterobacter [6-8]. It is commonly isolated from plant surfaces, seeds, fruits, and animal/human feces. Humans get exposed by ingestion of infected plants or thorn pricks. However, It can also cause opportunistic infections in humans, especially when the immune system is impaired. This case report aims to investigate the clinical features, pathogenesis, and treatment course of P. agglomerans bacteremia in a patient with COPD and bring attention to the association of this rare bacterium with COPD. P. agglomerans is a rare cause of blood, wound, and respiratory and urinary infections which usually present as fever, chills, and disseminated diseases such as septic arthritis, endophthalmitis, endocarditis, and osteomyelitis in the setting of bacteremia. Spontaneous infection can occur in an immunocompromised host. Typically, the bacteria have low virulence and a mild clinical course, with timely antibiotic initiation resulting in a favorable outcome.
Ubiquitous in the environment, P. agglomerans is found naturally in cotton and has been speculated as a possible pathological contribution in byssinosis and hypersensitivity pneumonitis (HP) [9,10]. In Eastern Poland, it has been identified as the most important cause of HP [11]. It is also postulated that inhaled P. agglomerans endotoxins elicit pathologic processes similar to cotton dust, resulting in the activation of alveolar macrophages and secretion of mediators such as interleukin-1, tumor necrosis factor (TNF), and prostaglandins. These mediators lead to the accumulation of platelets in pulmonary capillaries triggering acute and chronic inflammation associated with byssinosis. These changes subsequently result in bronchoconstriction, reduced forced expiratory volume in the first second, reduced diffusing capacity of the lung for carbon monoxide, and increased airway reactivity, which leads to significant respiratory symptoms [10]. The dominant presence of P. agglomerans (as high as 31.25%) has been reported in respiratory samples of immunocompromised patients presenting with respiratory symptoms, raising the possibility of its effect among patients with poorly controlled COPD with chronic exposure to steroids similar to our patient [12].
Spontaneous bacteremia with P. agglomerans has been associated with gastroesophageal reflux disease, active malignancy, and end-stage renal disease patients [13]. In our case, the patient had multiple hospitalizations due to COPD exacerbations leading to multiple and prolonged doses of steroids. Hence, therapeutic use of steroids in COPD can act as a double-edged sword; on one hand, helping acute exacerbation, while, on the other hand, leading to opportunistic infections such as P. agglomerans. Most previously documented cases of P. agglomerans bacteremia have been reported in clinical settings associated with central venous line, osteomyelitis, urinary tract infection, or isolated from abscess cavities. It should be noted that only about 20% of reported case reports and case series were able to isolate Pantoea species in two sets of blood cultures. It is our understanding that while Pantoea bacteremia may be transient, its potential for clinical deterioration could not be ignored, as seen in our case of clinical deterioration after days two to three of admission. In concordance with previous literature findings of transient bacteremia and significant clinical improvement after antibiotics, our case proves that early diagnosis and proper antibiotic use can prevent potential complications [14]. Of note, most reported Pantoea species infections are sensitive to broad-spectrum antibiotics. Other clinically relevant species of Pantoea have been reported such as P. brenneri in the urethra, P. dispersa in central line infections, P. gavinae and P. calida among formula feeding infants, and P. conspicua occasionally isolated in blood [15-17]. All of the species have been documented to infect both immunocompetent and immunocompromised individuals. Except for the occasional grave clinical course, most clinical entities described in regards to P. agglomerans are amenable to the treatment by appropriate antibiotics and supportive management, as seen in our case [18]. In addition to its association with many diseases, it is being evaluated for its potential role as immunopotentiators (IP-PA1) causing increased expression of cytokines such as TNF and causing macrophage activation and reversal of immunosuppression after chemotherapy. They are also being investigated for therapeutic use against cancers such as melanoma and allergic conditions [19].
According to a 2014 systematic review, 15.1-30% of the U.S. population suffers from GERD. Some of these patients can present with atypical symptoms such as cough, asthma, laryngitis, or chest pain. Although our patient did not report a history of underlying GERD, it is worth noting that COPD and GERD are commonly associated with P. agglomerans, possibly acting synergistically and worsening outcomes in COPD [20]. Of note, GERD is very prevalent and may contribute to lung pathologies such as COPD and interstitial lung disease [20-22]. Widespread occurrence and potential of inhalational transmission make P. agglomerans a possible cause of COPD exacerbations [23]. To our knowledge, this is the first case report speculating the possibility of P. agglomerans as a potential contributing factor for the pathology of COPD. In complex diseases with multifactorial pathophysiology such as COPD where a small trigger can have fatal consequences, the potential causes which could be easily treated should be further investigated. Bacteremia with P. agglomerans and E. faecium co-infection in colon cancer has been reported previously in the literature, but our case report describes spontaneous bacteremia with P. agglomerans and E. faecium in an individual presenting with COPD exacerbation without previously documented risk factors [24].
Conclusions
The epidemiology and clinical significance of P. agglomerans are still largely unknown in COPD. P. agglomerans can cause bacteremia in COPD patients which can be treated successfully with proper antibiotics. Further large-scale studies are needed to evaluate its potential role in exacerbation and its prognostic value in COPD.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
References
- 1.Pantoea agglomerans bacteremia: is it dangerous? Kaur IP, Inkollu S, Prakash A, Gandhi H, Mughal MS, Du D. http://PubMed PMID: 32313708; PMCID: PMCPMC7160720. Case Rep Infect Dis. 2020;2020:7890305. doi: 10.1155/2020/7890305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bloodstream infections in neutropenic patients with haematological malignancies. Carvalho AS, Lagana D, Catford J, Shaw D, Bak N. Infect Dis Health. 2020;25:22–29. doi: 10.1016/j.idh.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 3.Successful treatment of sepsis due to Pantoea agglomerans by polymyxin B-immobilized fiber column direct hemoperfusion therapy in a small cell lung carcinoma patient. Tsubouchi H, Matsumoto N, Yanagi S, Arimura Y, Nakazato M. Respir Med Case Rep. 2016;19:155–158. doi: 10.1016/j.rmcr.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Septic arthritis of the knee due to Pantoea agglomerans: look for the thorn. Koester T, Kusano T, Eijer H, Escher R, Waldegg G. J Bone Jt Infect. 2020;6:51–55. doi: 10.5194/jbji-6-51-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spondylodiscitis caused by Enterobacter agglomerans. Jayaweera JA, Kothalawala M, Devakanthan B, Arunan S, Galgamuwa D, Rathnayake M. Case Rep Infect Dis. 2016;2016:8491571. doi: 10.1155/2016/8491571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Emended description of the genus Pantoea, description of four species from human clinical samples, Pantoea septica sp. nov., Pantoea eucrina sp. nov., Pantoea brenneri sp. nov. and Pantoea conspicua sp. nov., and transfer of Pectobacterium cypripedii (Hori 1911) Brenner et al. 1973 emend. Hauben et al. 1998 to the genus as Pantoea cypripedii comb. nov. Brady CL, Cleenwerck I, Venter SN, Engelbeen K, De Vos P, Coutinho TA. Int J Syst Evol Microbiol. 2010;60:2430–2440. doi: 10.1099/ijs.0.017301-0. [DOI] [PubMed] [Google Scholar]
- 7.PATRIC, the bacterial bioinformatics database and analysis resource. Wattam AR, Abraham D, Dalay O, et al. Nucleic Acids Res. 2014;42:0–91. doi: 10.1093/nar/gkt1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Polyphasic study of plant- and clinic-associated Pantoea agglomerans strains reveals indistinguishable virulence potential. Völksch B, Thon S, Jacobsen ID, Gube M. Infect Genet Evol. 2009;9:1381–1391. doi: 10.1016/j.meegid.2009.09.016. [DOI] [PubMed] [Google Scholar]
- 9.Acute hypersensitivity pneumonitis in woodworkers caused by inhalation of birch dust contaminated with Pantoea agglomerans and Microbacterium barkeri. Mackiewicz B, Dutkiewicz J, Siwiec J, et al. Ann Agric Environ Med. 2019;26:644–655. doi: 10.26444/aaem/114931. [DOI] [PubMed] [Google Scholar]
- 10.Pantoea agglomerans: a marvelous bacterium of evil and good. Part I. Deleterious effects: dust-borne endotoxins and allergens - focus on cotton dust. Dutkiewicz J, Mackiewicz B, Lemieszek MK, Golec M, Milanowski J. Ann Agric Environ Med. 2015;22:576–588. doi: 10.5604/12321966.1185757. [DOI] [PubMed] [Google Scholar]
- 11.Pantoea agglomerans chronic exposure induces epithelial-mesenchymal transition in human lung epithelial cells and mice lungs. Lemieszek MK, Rzeski W, Golec M, Mackiewicz B, Zwoliński J, Dutkiewicz J, Milanowski J. Ecotoxicol Environ Saf. 2020;194:110416. doi: 10.1016/j.ecoenv.2020.110416. [DOI] [PubMed] [Google Scholar]
- 12.Pantoea agglomerans in immunodeficient patients with different respiratory symptoms. Flores Popoca EO, Miranda García M, Romero Figueroa S, Mendoza Medellín A, Sandoval Trujillo H, Silva Rojas HV, Ramírez Durán N. ScientificWorldJournal. 2012;2012:156827. doi: 10.1100/2012/156827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bacteremia caused by Pantoea agglomerans at a medical center in Taiwan, 2000-2010. Cheng A, Liu CY, Tsai HY, et al. J Microbiol Immunol Infect. 2013;46:187–194. doi: 10.1016/j.jmii.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 14.Pantoea agglomerans, a plant pathogen causing human disease. Cruz AT, Cazacu AC, Allen CH. J Clin Microbiol. 2007;45:1989–1992. doi: 10.1128/JCM.00632-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pantoea: insights into a highly versatile and diverse genus within the Enterobacteriaceae. Walterson AM, Stavrinides J. FEMS Microbiol Rev. 2015;39:968–984. doi: 10.1093/femsre/fuv027. [DOI] [PubMed] [Google Scholar]
- 16.[Seven cases of port-a-cath contamination caused by Pantoea agglomerans in the Oncological Service of Iseo Hospital, Brescia (Italy)] Izzo I, Lania D, Castro A, Lanzini F, Bella D, Pagani A, Colombini P. https://www.infezmed.it/index.php/article?Anno=2014&numero=2&ArticoloDaVisualizzare=Vol_22_2_2014_152. Infez Med. 2014;22:152–155. [PubMed] [Google Scholar]
- 17.Pantoea dispersa bacteremia caused by central line-associated bloodstream infection. Hagiya H, Otsuka F. Braz J Infect Dis. 2014;18:696–697. doi: 10.1016/j.bjid.2014.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pantoea agglomerans infections in children: report of two cases. Siwakoti S, Sah R, Rajbhandari RS, Khanal B. Case Rep Pediatr. 2018;2018:4158734. doi: 10.1155/2018/4158734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oral administration of immunopotentiator from Pantoea agglomerans 1 (IP-PA1) improves the survival of B16 melanoma-inoculated model mice. Hebishima T, Matsumoto Y, Watanabe G, et al. Exp Anim. 2011;60:101–109. doi: 10.1538/expanim.60.101. [DOI] [PubMed] [Google Scholar]
- 20.Meta-analysis of gastroesophageal reflux disease and idiopathic pulmonary fibrosis. Bédard Méthot D, Leblanc É, Lacasse Y. Chest. 2019;155:33–43. doi: 10.1016/j.chest.2018.07.038. [DOI] [PubMed] [Google Scholar]
- 21.Proton pump inhibitors use is associated with a lower risk of acute exacerbation and mortality in patients with coexistent COPD and GERD. Su VY, Liao HF, Perng DW, et al. Int J Chron Obstruct Pulmon Dis. 2018;13:2907–2915. doi: 10.2147/COPD.S157761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gastro-esophageal reflux disease and exacerbations in chronic obstructive pulmonary disease. Ingebrigtsen TS, Marott JL, Vestbo J, Nordestgaard BG, Hallas J, Lange P. Respirology. 2015;20:101–107. doi: 10.1111/resp.12420. [DOI] [PubMed] [Google Scholar]
- 23.Pantoea agglomerans pneumonia in a heart-lung transplant recipient: case report and a review of an emerging pathogen in immunocompromised hosts. Shubov A, Jagannathan P, Chin-Hong PV. Transpl Infect Dis. 2011;13:536–539. doi: 10.1111/j.1399-3062.2011.00630.x. [DOI] [PubMed] [Google Scholar]
- 24.Bacteremia caused by Pantoea agglomerans and Enterococcus faecalis in a patient with colon cancer. Christakis GB, Perlorentzou SP, Aslanidou M, Savva L, Zarkadis IK. https://pubmed.ncbi.nlm.nih.gov/17600887/ J BUON. 2007;12:287–290. [PubMed] [Google Scholar]