Abstract
Background
Major adverse cardiovascular events (MACE) are increasingly used as composite outcomes in randomized controlled trials (RCTs) and observational studies. However, it is unclear how observational studies most commonly define MACE in the literature when using administrative data.
Methods
We identified peer-reviewed articles published in MEDLINE and EMBASE between January 1, 2010 to October 9, 2020. Studies utilizing administrative data to assess the MACE composite outcome using International Classification of Diseases 9th or 10th Revision diagnosis codes were included. Reviews, abstracts, and studies not providing outcome code definitions were excluded. Data extracted included data source, timeframe, MACE components, code definitions, code positions, and outcome validation.
Results
A total of 920 articles were screened, 412 were retained for full-text review, and 58 were included. Only 8.6% (n = 5/58) matched the traditional three-point MACE RCT definition of acute myocardial infarction (AMI), stroke, or cardiovascular death. None matched four-point (+unstable angina) or five-point MACE (+unstable angina and heart failure). The most common MACE components were: AMI and stroke, 15.5% (n = 9/58); AMI, stroke, and all-cause death, 13.8% (n = 8/58); and AMI, stroke and cardiovascular death 8.6% (n = 5/58). Further, 67% (n = 39/58) did not validate outcomes or cite validation studies. Additionally, 70.7% (n = 41/58) did not report code positions of endpoints, 20.7% (n = 12/58) used the primary position, and 8.6% (n = 5/58) used any position.
Conclusions
Components of MACE endpoints and diagnostic codes used varied widely across observational studies. Variability in the MACE definitions used and information reported across observational studies prohibit the comparison, replication, and aggregation of findings. Studies should transparently report the administrative codes used and code positions, as well as utilize validated outcome definitions when possible.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12874-021-01440-5.
Keywords: Observational study, Reproducibility, Acute myocardial infarction, Stroke, Heart failure, Acute coronary syndrome, Cardiovascular disease
Background
Cardiovascular disease is the leading cause of death in the United States, making it a common target for interventional research [1, 2]. Due to this, the composite endpoint of “major adverse cardiovascular events” (MACE) is an increasingly common primary outcome of interest. In 2008, the United States Food and Drug Administration (FDA), followed by the European Medicines Agency (EMA) in 2012, provided guidance on utilizing a three-point MACE outcome, which includes acute myocardial infarction (AMI), stroke, and cardiovascular mortality in all trials evaluating the cardiovascular safety of diabetic agents [3]. Some trials have utilized a four-point MACE as well, by including hospitalization for unstable angina or revascularization procedures [3, 4]. Five-point MACE further expands on this with the inclusion of heart failure (HF). While MACE is now a better-defined and more ubiquitous outcome among RCTs, its use in observational studies to assess the safety and real-world effectiveness of therapies remains less clear.
Observational studies using large administrative databases can evaluate population-level use and outcomes of therapies in an efficient and cost-effective way [5]. However, several common issues with observational studies limit their reproducibility and comparability to RCTs, thus limiting the utility of MACE as a composite outcome. First, in comparison to RCTs, observational studies often do not consistently report their protocols, including outcome definitions [6]. To allow for useful comparisons between observational studies and RCTs, improved standardization and transparency is needed [7, 8]. Even when MACE components are well-defined, such as AMI or stroke, another challenge encountered in observational studies is how to define outcomes using diagnosis codes available from administrative data. For example, the International Classification of Diseases (ICD) is a commonly used coding system for medical reimbursement and is one of the most frequent sources of information available in administrative databases [9]. Unfortunately, ICD codes can be prone to errors and diagnosis misclassifications, as they are primarily collected for reimbursement purposes and rely on clinical documentation that can vary across settings and providers [5]. Though several studies have attempted to validate the diagnosis codes for commonly used MACE components (e.g., AMI, stroke, and HF), with positive predictive values of upwards of 80–90%, it is unclear how these codes have been taken up in MACE composite outcome definitions [10–12]. For these reasons, the current use of MACE in observational studies warrants further investigation.
Thus, the purpose of this review was to systematically determine the most common definitions of MACE employed in observational studies using administrative data. With that, our objectives were: i) assess each study’s definition of MACE components (e.g., AMI, stroke), ii) assess the diagnostic criteria used for outcome ascertainment such as codes used and position of codes, and iii) assess whether outcomes had been validated. We hypothesized that, across observational studies, there is great variability in the definitions of MACE used and minimal alignment with the classic three, four, or five-point MACE outcomes. Our hope is that this work will promote a standard approach to the definition of MACE in future studies, allowing for the improved transparency and reproducibility of observational studies.
Methods
Search strategy and selection criteria
The protocol for this systematic review is based on the 2015 Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P) statement [13]. The protocol was not registered in the International Prospective Register of Systematic Reviews (PROSPERO), but the original protocol and modifications are included in Supplementary Text 1 (see Additional file 1). The reporting of this review is based on the 2020 PRISMA statement and the checklist is provided in Supplementary Table 1 (see Additional file 2) [14]. We searched MEDLINE and EMBASE for literature published from January 1, 2010 to October 9, 2020 that defined composite MACE as a primary or secondary outcome in studies utilizing administrative databases. A 10-year lookback was used in order to restrict to the most recently published studies. The search strategy was developed by the authors using the search terms presented in Supplementary Text 2 (see Additional file 3) and was performed on October 9, 2020. A standardized protocol for study abstract screening and full-text review was developed and piloted using the same 20 studies among the reviewers (EB, ES, LH), and is further described in Supplementary Text 1 (see Additional file 1). The abstracts from each record were initially screened for relevance by three independent reviewers (EB, ES, LH) using Abstrackr (http://abstrackr.cebm.brown.edu/), a free semi-automated abstract screening tool [15]. Afterwards, we performed a full-length text review of the abstracts that were retained after screening (EB, ES, LH).
We included studies that identified MACE composite endpoints as the primary or secondary study outcome, used administrative data sources in the study, and defined MACE using International Classification of Diseases, Clinical Modification, Ninth Revision (ICD-9-CM) or Tenth Revision (ICD-10-CM) diagnosis codes. The included studies did not need to overtly name “major adverse cardiovascular events” as the primary or secondary outcome to be included into this study, as many definitions and terms are used across studies. For example, MACE may be referred to as “adverse” or “acute cardiovascular events”, “major adverse cardiovascular and cerebrovascular events” or simply “cardiovascular events”, among other terms. Thus, we included studies if the composite outcome that was studied utilized a combination of multiple MACE endpoints. We excluded reviews, meta-analyses, conference abstracts, editorials, papers whose primary or secondary outcome was not a composite of multiple MACE endpoints, and those that did not use or report ICD-9-CM or ICD-10-CM codes to define MACE endpoints. Any uncertainty with regards to inclusion or exclusion of an individual paper was resolved by consensus of the three reviewers.
Data extraction and synthesis
After each of the independent reviewers determined that a full-text met inclusion criteria for the study, definitions for composite MACE outcomes were extracted into a shared document using a standardized protocol by two reviewers (LH, EB). ICD-9-CM and ICD-10-CM codes were also extracted for each MACE endpoint, and were acquired either through full-length text review or through review of published supplements. The position of the diagnosis code required in the study outcome criteria was recorded as primary position, any position, or not reported. Further, information on whether the study outcomes had been previously validated was assessed in each individual study or review of supplements, and citations were extracted. Each study’s administrative data source and study years were also recorded.
Once data were extracted from included studies, we categorized the specific definitions of MACE based on the individual components referred to by the authors as opposed to the specific diagnosis codes used. We made this decision due to the lack of consistency in diagnosis codes used across studies and chose to categorize based on the MACE components that the authors reported. Component definitions of MACE included: AMI, acute coronary syndrome or ischemic heart disease (ACS/IHD), stroke (either ischemic or hemorrhagic stroke), revascularization procedures, cardiovascular (CV) death, and all-cause death. Of note, due to the variability of outcomes used across studies, the ACS/IHD component reflects the following definitions used by study authors: ACS, IHD, coronary artery disease (CAD), and unstable angina (UA). Overall, we performed a qualitative assessment of the evidence only, and did not perform a meta-analysis or strength of evidence assessment due to the nature of the research questions.
Results
Included studies
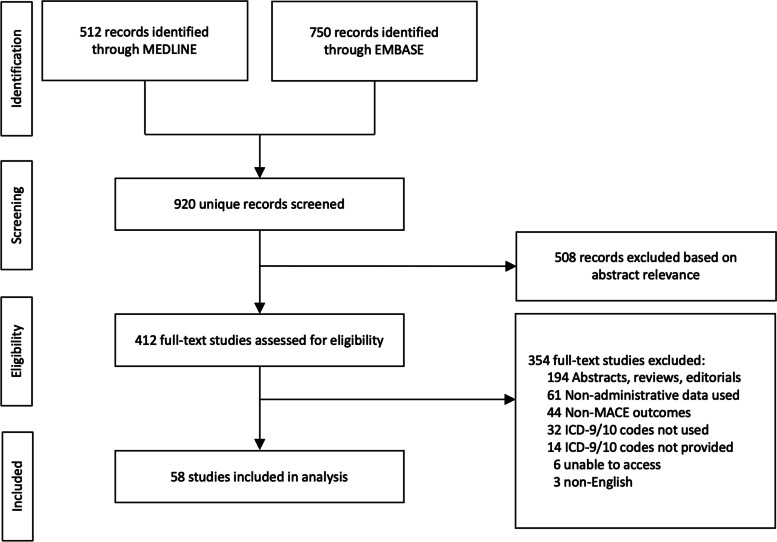
Our search of MEDLINE and EMBASE yielded 920 unique articles, 412 of which were retained for full-text review after abstract screening (Fig. 1). After excluding 354 studies during full-text review, 58 studies were included in the final analysis.
Fig. 1.
PRISMA flow diagram for included studies. Abbreviations: MACE, major adverse cardiovascular events; ICD, International Classification of Diseases
Overall studies
The included observational studies utilized a range of outcome components to define MACE (Table 1). The majority of the included studies utilized ICD-9-CM to define outcomes. There was poor concordance of MACE definitions used in the included studies when compared to the three-point, four-point, and five-point definitions of MACE commonly used in randomized controlled trials (RCTs). For instance, 8.6% (5/58) of observational studies used a MACE definition that matched the three-point definition of MACE (AMI, stroke, CV death) while no studies matched the four-point or five-point definitions (Table 2). Across all included studies, the most common MACE component definitions were: AMI, stroke, 15.5% (9/58); AMI, stroke, all-cause death, 13.8% (8/58); and AMI, stroke, CV death 8.6% (5/58) (Table 3). Overall, 67% of studies (39/58) did not perform a validation or provided no citations validating the outcome definitions used. Additionally, 70.7% (41/58) of studies did not report the position of diagnosis codes used in endpoints, while 20.7% (12/58) used the primary diagnosis position and 8.6% (5/58) used any position.
Table 1.
MACE definitions based on publication
| Study Citation and Publication Year | Data Source and Time Period | MACE Definition | ICD-9/10 Codes Diagnosis or Procedure Position |
Validation |
|---|---|---|---|---|
| Chapman et al. (2010) [16] | IMS LifeLink: US Health Plan Claims database from 2004 to 2005 | AMI, other non-AMI IHD, HF, stroke/TIA, PVD, cardiac revascularization procedure, carotid endarterectomy |
AMI: 410.xx, 412; other non-AMI IHD: 411.xx, 413.xx, 414.xx, 427.xx, V45.81, V45.82; stroke/TIA: 433.xx, 434.xx, 435.x, 436, 437.0, 437.1, 438; PVD: 440, 440.1, 443.xx (ICD-9). (Authors did not cite ICD codes for carotid endarterectomy or other revascularization procedures.) Primary position. |
NR |
| Gudbjornsson et al. (2010) [17] | Icelandic Medicines Registry from 2001 to 2003 | AMI, UA, stroke |
AMI: I21; UA: I20.0; stroke: I63 (ICD-10). NR |
NR |
| Charlot et al. (2011) [18] | Danish national patient registry from 1997 to 2006 | AMI, stroke, CV death |
AMI: I21, I22; Stroke: I60–I69, G45 (ICD-10). (No specific codes were listed for CV death). Any position. |
Validated through data linkage between the Danish national patient registry and patient level data collected through the Danish MONICA registry [19] and the Copenhagen City Heart Study [20] |
| Kociol et al. (2011) [21] | Medicare claims linked to the ADHERE-Core registry from 2001 to 2004 | AMI, stroke |
AMI: 410.× 1; stroke: 433.x, 434.x (ICD-9). Primary position. |
NR |
| Chen et al. (2012) [22] | Taiwan National Health Research Insurance database from 2000 | AMI, ischemic stroke |
AMI: 410.xx; ischemic stroke 433.xx, 434.xx, 436, 437.1 (ICD-9). NR |
Authors cite a study validating incident events utilizing these specific ICD codes when compared with direct patient chart review [23] |
| Degli Esposti et al. (2012) [24] | Multiple databases of the Local Health Unit of Florence from 2004 to 2007 | AMI, stroke, all cause death |
AMI: 410.x; stroke: 430–438.x (ICD-9). NR |
NR |
| Parker et al. (2012) [25] | Cardiovascular Research Network Hypertension Registry from 2000 to 2009 | IHD, stroke, PVD, HF |
IHD: 410.xx–414.xx; stroke: 430.xx–434.xx, 436.xx, 852.0, 852.2. 852.4, 853.0; PVD: 441.3–441.7, 443.9, 444.0, 444.2; HF: 428.xx, 402.xx, 398.91 (ICD-9). Primary position. |
NR |
| Karthikesalingam et al. (2013) [26] | Hospital Episode Statistics data from 2006 to 2011 | AMI, stroke, aortoiliac or peripheral arterial thrombosis or embolism, emergency amputation, open/endovascular lower limb revascularization |
AMI: I21, I22; stroke: I63, I64, I69.4, I69.8 (ICD-10). NR |
NR |
| Mortensen et al. (2014) [27] | VA Health Care System administrative and clinical databases from 2001 to 2012 | AMI, HF, cardiac arrhythmia |
AMI: 410, 410.0–410.9, 411, 411.1, 412, 414.2, 414.8, 429.71, 429.79; HF: 402, 402.1, 402.10, 402.11, 402.9, 402.90, 402.91, 404, 414.19, 425.4, 428, 428.0, 428.1, 428.2, 428.20–428.23, 428.3, 428.30–428.33, 428.4, 428.40–428.43, 428.9, 429.1, 429.4, 997.1; cardiac arrhythmia: 427, 427.0, 427.1–427.5, 427.31, 427.32, 427.41, 427.42, 427.8, 427.81, 427.89, 427.9, 429.4, 997.1, V12.53 (ICD-9). NR |
NR |
| Neumann et al. (2014) [28] | Système National d’Information Inter-Régimes de l’Assurance Maladie from 2008 to 2011 | IHD, ischemic stroke |
IHD: I21–24; ischemic stroke: I63, I65, I66. (ICD-10). Any position. |
NR |
| Vanasse et al. (2014) [29] | Régie de l’assurance maladie du Québec from 2006 to 2007 | CV disease, CV death |
CV disease: 410–414, 428, 430–438 (ICD-9). I20–I25, I50, I60-I69 (ICD-10). Any position. |
NR |
| Chou et al. (2015) [30] | National Health Insurance Research Database of Taiwan from 2001 to 2010 | AMI, stroke, HF, cardiac arrhythmia, cardiac shock, cardiac revascularization procedure |
AMI: 410–410.9; stroke: 430–437; HF: 428.0–428.10, cardiac arrhythmia: 26.0, 426.12–426.13, 426.51, 426.52, 426.54, 427.1, 427.4, 427.41, 427.42, 427.5; cardiac shock: 785.51; revascularization: 36.0–36.03, 36.05–36.09, 36.1–36.99, V45.8, 36.0–36.9 (ICD-9). NR |
NR |
| Desai et al. (2015) [31] | SUPREME-DM consortium database from 2005 to 2011 | ACS, stroke, HF |
ACS: 410.0–410.9, 411.1–411.8; stroke: 430–432.9, 433–434.9; HF: 428–428.9 (ICD-9). Primary position. |
Authors cited multiple studies that have shown good PPVs using these specific ICD codes [32–34] |
| Doll et al. (2015) [35] | Medicare claims linked to the ACTION Registry-GWTG registry from 2007 to 2010 | AMI, stroke, all cause death, cardiac revascularization procedure |
AMI: 410.× 1; stroke: 430.x, 431.x, 432.x, 433.× 1, 434.× 1, 436.x, 437.1, 437.9, 997.02; revascularization: 00.66, 36.0, 36.1, 36.2, 36.3 (ICD-9). Primary position. |
NR |
| Jernberg et al. (2015) [36] | Swedish National Inpatient Register, Swedish Prescribed Drug Register, and Swedish Cause of Death Register from 2006 to 2011 | AMI, stroke, CV death |
AMI: I21; stroke: I61-I64; CV death: I00-I99 (ICD-10). NR |
Authors cited a study which reported that > 95% of MI diagnoses were valid in the National Inpatient register [37]. No validation was reported for stroke or CV death. |
| Korsnes et al. (2015) [38] | MarketScan Commercial Claims and Encounters and Medicare Supplemental Database from 2006 to 2011 | AMI, ischemic stroke |
AMI: 410.xx; ischemic stroke: 433.xx, 434.xx, 436.xx (ICD-9). Primary position. |
NR |
| Roussel et al. (2015) [39] | French National Health Insurance Information System from 2008 to 2010 | AMI, ischemic stroke, all cause death, above the ankle amputations |
AMI: I21-I24; ischemic stroke: I63, I65, I66 (ICD-10). (Authors did not use ICD codes for above the ankle amputations.) NR |
NR |
| Sirois et al. (2015) [40] | Quebec health insurance board databases, Quebec registry of hospitalization databases from 1998 to 2004 | AMI, strokes |
AMI: 410; stroke: 430–431, 433.× 1, 434.× 1 and 435 (ICD-9). Any position |
Authors cite a study that validated the accuracy of coding hospital discharge data of AMI and found a PPV of 96% utilizing this specific ICD code for AMI [41]. No validation was reported for stroke. |
| Stochkendahl et al. (2015) [42] | Danish National Patient Register from 2006 to 2011 | ACS, stroke, CV death, cardiac revascularization procedure |
ACS: I21-I23, I24.0, I24.8, I24.9; stroke: I60-I69; CV death: I00-I99 (ICD-10). (Authors did not cite ICD codes for cardiac revascularization procedures.) NR |
NR |
| Blin et al. (2016) [43] | Echantillon Généraliste des Bénéficiaires database from 2007 to 2010 | AMI, stroke/TIA, all cause death |
AMI: I21.0-I21.9, I22.0–22.9; stroke/TIA: I60-I64, G45 (ICD-10). Primary position. |
NR |
| Cheng et al. (2016) [44] | Taiwan National Health Research Insurance database from 2004 to 2015 | AMI, ischemic stroke, hemorrhagic stroke, all cause death |
AMI: 410; ischemic stroke: 434–437; hemorrhagic stroke: 430–432 (ICD-9). NR |
NR |
| Chuang et al. (2016) [45] | Taiwan National Health Research Insurance database from 1996 to 2011 | ACS, ischemic stroke, hemorrhagic stroke |
ACS: 410, 411; ischemic stroke: 433–438; hemorrhagic stroke: 430–432 (ICD-9). NR |
NR |
| Fortuna et al. (2016) [46] | HealthPartners Medical Group electronic medical record (EPIC) from 2007 to 2009 | AMI. stroke, PCI |
AMI: 410.xx; stroke: 430.xx-434.xx, 436.xx, 852.0, 852.2, 852.4, 853.0 (ICD-9); PCI: 92980–92,996 (CPT). NR |
Authors cited a study validating the claims definitions using electronic medical records [47]. |
| Hsu et al. (2016) [48] | Taiwan National Health Research Insurance database from 1995 to 2010 | AMI, stroke |
AMI: 410.x; stroke: 433.x, 434.x, 436.x (ICD-9). Primary position. |
Authors cite two studies that previously validated the accuracy of these ICD codes [49, 50]. |
| Shih et al. (2016) [51] | Taiwan National Health Insurance Research Database from 1995 to 2012 | AMI, ischemic stroke, in-hospital cardiovascular mortality |
AMI: 410.x; ischemic stroke: 433.x, 434.x, 436.x (ICD-9); in-hospital cardiovascular mortality. Primary position. |
Authors cited two studies for ischemic stroke validation only [50, 52]. |
| Solomon et al. (2016) [53] | Medicare claims linked to Brigham and Women’s Hospital electronic medical record from 2006 to 2011 | AMI, stroke, TIA |
AMI: 410.x except 410.×2; stroke: 430.x, 431.x, 434.x, 436.x; TIA: 435.x (ICD-9). NR |
Authors cited multiple studies demonstrating that using these specific ICD codes, there’s a 94% PPV for AMI, 96% PPV for stroke and 72–96% PPV for TIA [33, 54, 55]. |
| Babazade et al. (2017) [56] | Inpatient databases from multiple U.S. states, HCUP database from 2009 to 2011 | AMI, Acute coronary occlusion without AMI, postoperative pulmonary edema, cardiac arrest |
AMI: 410; acute coronary occlusion without AMI: 411.81; pulmonary edema: 518.4; cardiac arrest: 997.1 (ICD-9). NR |
NR |
| de Miguel-Yanes et al. (2017) [57] | Spanish National Hospital Discharge Database from 2002, 2006, 2010 and 2014 | AMI, stroke, aortic aneurysm and dissection, acute limb ischemia |
AMI: 410.xx; stroke: 431, 432.9, 433.× 1, 434.01, 434.11, 434.91; aortic aneurysm and dissection: 441.xx; acute limb ischemia: 440.21–440.24, 440.4, 444.22, 444.81, 445.02 (ICD-9). Primary position. |
NR |
| Lindahl et al. (2017) [58] | SWEDEHEART from 2003 to 2013 | AMI, ischemic stroke, HF, all cause death |
AMI: I21, I22, I23; ischemic stroke: I63, I64; HF: I50, K761, I971, I110 (ICD-10). NR |
NR |
| Policardo et al. (2017) [59] | Tuscany regional health system from 2008 to 2012 | AMI, ischemic stroke, HF, lower extremity amputation |
AMI: 410.xx; ischemic stroke: 430.xx, 431.xx, 432.xx, 434.xx, 436.xx; HF: 401.91, 402.01, 402.11, 402.91, 404.01, 404.3, 404.13, 404.93, 428.0, 428.1, 428.9; lower extremity amputation: 84.1x (ICD-9). NR |
NR |
| Tung et al. (2017) [60] | Taiwan National Health Research Insurance database from 2009 to 2012 | AMI, UA, stroke, resuscitation after cardiac arrest, all cause death, cardiac revascularization procedure |
AMI: 410–410.9; UA: 411.1; stroke: 430–437; resuscitation after cardiac arrest: 427.5; revascularization: 36.0–36.03, 36.05–36.09, 36.1–36.99, V45.81 (ICD-9). NR |
NR |
| Arinze et al. (2018) [61] | OptumLabs Data Warehouse from 2004 to 2014 | AMI, stroke |
AMI: 410; stroke: 434, 434.0, 434.00, 434.01, 434.1, 434.10, 434.11, 434.9, 434.90, 434.91 (ICD-9). NR |
NR |
| Baviera et al. (2018) [62] | Administrative health databases of Lombardy from 2002 to 2014 | ACS, stroke, all cause death, major amputation |
ACS: 410.xx, 411; stroke: 430, 431, 434.xx, 436, 433.11; major amputation: 84.10, 84.13, 84.14, 84.15, 84.16, 84.17, 84.18, 84.19 (ICD-9). NR |
Authors state that diagnoses were retrieved from hospital discharge charts, which have been validated across all Italian hospitals for reimbursement purposes. |
| Chan et al. (2018) [63] | Taiwan National Health Research Insurance database from 2000 to 2011 | ACS, stroke, all cause death |
ACS: 410; stroke: 430–438 (ICD-9). NR |
NR |
| Wu et al. (2018) [64] | Taiwan National Health Research Insurance database from 2001 to 2013 | AMI, stroke, HF, all cause death |
AMI: 410.xx; stroke: 430.xx-437.xx; HF: 428.xx (ICD-9). NR |
Authors cite an 88% PPV for AMI [65]. Authors do not report validation data specifically for stroke or HF. |
| Degli Esposti et al. (2018) [66] | Health-Assisted Subjects’ Database, Outpatients and Inpatients Pharmaceutical Drugs Database, Hospital Discharge Database from 2010 to 2011 (administrative databases of six Italian local health units) | AMI, other IHD, angina, cerebral artery occlusion, TIA, acute but ill-defined cerebrovascular disease |
AMI: 410; IHD: 411; angina: 413; cerebral artery occlusion: 433, 434; TIA: 435; cerebrovascular disease: 436 (ICD-9). NR |
NR |
| Hussain et al. (2018) [67] | Ontario Drug Benefit program database from 2002 to 2015 | AMI, stroke, all cause death |
AMI: I21.x, I22.x; stroke: I60.x I61.x I62.x I63.x, I64.x, H34.1, excluding I63.6 (ICD-10) NR |
Authors cite studies validating ICD codes for AMI [68] and stroke [69]. |
| Jin et al. (2018) [70] | U.S. Nationwide Readmissions Database from 2013 | AMI, HF, cardiac revascularization procedure, aortic valve repair, cardiac ablation, cardioversion, cardiac catheterization, left atrial appendage closure, Implanted cardioverter defibrillator placement, pacemaker placement, ischemic stroke, hemorrhagic stroke, iatrogenic stroke |
AMI: 410.x; HF: 428.x, 491.8, 491.9, 492.0, 492.6, 496.0; revascularization: 0.66, 36.1x, 36.2x; aortic valve repair: 35.00x, 35.01x, 35.1x, 35.2x, 35.3x, 35.05, 35.06; Cardiac ablation: 37.33, 37.34; Cardioversion 99.61, 99.62, 99.69; Cardiac catheterization: 37.21, 37.22, 37.23; Left atrial appendage closure 379, 373.6; Implanted cardioverter defibrillator placement: 37.94, 37.95, 37.96, 37.97, 37.98; pacemaker placement: 0.50, 0.51, 0.52, 0.53, 0.54, 37.7, 37.71, 37.72, 37.73, 37.74, 37.76, 37.80, 37.81, 37.82, 37.83, 37.85, 37.86, 37.87; Ischemic stroke 433.× 1, 434.× 1, 436; Hemorrhagic stroke 430, 431; Iatrogenic stroke 997.02 (ICD-9). Primary position. |
Authors cite multiple studies that have demonstrated a PPV of 89–96% using these ICD codes [55, 71, 72]. |
| Kim et al. (2018) [73] | Korean National Health Insurance Service from 2005 to 2015 | AMI, ischemic stroke, hemorrhagic stroke, HF |
AMI: I21, I22; ischemic stroke: I63, I64; hemorrhagic stroke: I60-I62; HF: I11.0, I50, I97.1 (ICD-10). NR |
NR |
| Kiss et al. (2018) [74] | National Health Insurance Fund database 2010–2013 | AMI, stroke |
AMI: I21–24; stroke: I61–63 (ICD-10). NR |
NR |
| Ohm et al. (2018) [75] | Swedish national quality registry SWEDEHEART, sub-registry SEPHIA from 2006 to 2013 | AMI, ischemic stroke, CV death |
AMI: I21.0–4, I21.9, I22.0–1, I22.8–9; ischemic stroke: I63.0–9 (ICD-10); and CV death: I46.1, I46.9. NR |
NR |
| Winell et al. (2018) [76] | National Hospital Discharge Register, National Causes of Death Register from 2000 to 2011 | ACS, ischemic stroke |
ACS: 410, 411 (ICD-9) I20.0, I21, I22 (ICD-10); stroke: 433–436, excluding 434.9x (ICD-9), I63, I64, G45 (ICD-10). NR |
Authors cite multiple studies which have validated the use of these ICD codes for this database [77, 78]. |
| Yang et al. (2018) [79] | Taiwan National Health Research Insurance database from 1996 to 2013 | AMI, ischemic stroke |
AMI: 410; ischemic stroke: 433–436 (ICD-9). NR |
NR |
| Young et al. (2018) [80] | Optum™ Integrated Real World Evidence Electronic Health Records and Claims de-identified database from 2006 to 2016 | AMI, stroke, CV death |
AMI: 410.xx (ICD-9), I21.xx, I22.xx (ICD-10); stroke: 430.xx, 431.xx, 434.xx, 436.xx (ICD-9), I60.xx, I61.xx, I63.3-I63.9, I66.xx (ICD-10); CV death (defined as death within 30 days of AMI, stroke or the following ICD codes): 411.xx-414.xx, 415.xx-417.xx, 420.xx-427.xx, 428.xx, 429.xx, 432.xx, 433.xx, 435.xx, 437.xx, 785.51 (ICD-9), I20.x, I23.xx-I25.xx, I46.9, I30.xx-I52.xx, I62.xx, I63.0-I63.2, I64.xx, I65.xx, I67.xx, I68.xx, R57.0 (ICD-10). NR |
NR |
| Arnaout et al. (2019) [81] | California Healthcare Cost and Utilization Project database from 2005 to 2009 | AMI, stroke, HF |
AMI: 410.00–410.92; stroke: 434.91, 434.11, 459.0; HF: 402.01, 402.11, 402.91, 404.91, 404,93, 425.0–425.1, 425.11, 425.18, 425.2, 425.3, 425.4, 425,5, 425.7–425.9, 428,0–428.2, 428.20–428.21, 428.22–428.23, 428.30–428.33, 428.4, 428.40–428.43, 428.9 (ICD-9). NR |
Authors cite multiple studies that have demonstrated good sensitivity and specificity for AMI, stroke and HF using these ICD codes [10–12]. |
| Chen et al. (2019) [82] | Taiwan National Health Research Insurance database from 2000 to 2008 | IHD, HF |
IHD: 410–414; HF: 428 (ICD-9). NR |
Authors cite study that validated ICD codes for AMI [65]. |
| Giral et al. (2019) [83] | Système National d’Information Inter-Régimes de l’Assurance Maladie from 2012 to 2014 | Coronary event, cerebrovascular event, other vascular event |
Coronary event: I20, I21, I22, I23, I24; cerebrovascular event: G45, G46, H34.0, H34.1, H34.2, H34.9, I60, I61, I62, I63, I64, I65, I66, I67.0; other vascular event: I70.01, I70.21, I70.81, I70.91, I71.0, I71.1, I71.3, I71.5, I71.8, I72, I74, K55.9 (ICD-10). NR |
NR |
| Hsueh et al. (2019) [84] | Taiwan National Health Research Insurance database from 2000 to 2013 | IHD, HF |
IHD: 410–414; HF: 428 (ICD-9). NR |
Authors cite study that validated ICD codes for AMI using this database [65]. |
| Kim et al. (2019) [85] | South Korean National Health Information Database from 2006 to 2014 | IHD, ischemic stroke, cardiac revascularization procedure |
IHD: I21–24; ischemic stroke: I63, I65, I66; (ICD-10). Authors did not cite ICD codes for cardiac revascularization procedures. Primary position. |
NR |
| Kuo et al. (2019) [86] | Taiwan National Health Research Insurance database from 1999 to 2010 | AMI, IHD, HF, cerebrovascular disease, all cause death |
AMI: 410, 412; IHD: 411, 413, 414, V45.81, V45.82, 00.66C, 36.0, 36.1, 36.2, 36.3, 36.9, 88.5, 37.8; HF: 428; cerebrovascular disease: 430–437, 438, V12.54, 38.11, 38.12 (ICD-9) NR |
Authors cited multiple studies that previously validated the accuracy of these ICD codes [50, 65, 87–90]. |
| Li et al. (2019) [91] | Taiwan National Health Insurance Research Database from 2000 to 2011 | CAD, HF, atrial fibrillation, stroke |
CAD: 410–414; AMI: 410; HF: 428; atrial fibrillation: 427.31; stroke: 430–438 (ICD-9). NR |
NR |
| Mureddu et al. (2019) [92] | Italian National Registry of Hospital Discharge Records (ItHDR) from 2004 to 2008, 2009–2010, 2011–2015 | AMI, stroke, all-cause death |
AMI: 410, 412; stroke: 433.×1, 434.× 1 (with the exclusion of 431, 432.x) (ICD-9). NR |
NR |
| Lin et al. (2019) [93] | Taiwan National Health Insurance Research Database from 1999 to 2011 | AMI, ischemic stroke |
AMI: 410.x; ischemic stroke: 433.x, 434.x, 436 (ICD-9). NR |
Authors cite two studies validating ICD codes for AMI and stroke using this database [50, 65]. |
| Bourrier et al. (2020) [94] | The Manitoba Health Insurance Registry, Medical Services, Discharge Abstract Database, and Diagnostic Services of Manitoba (Manitoba, Canada) from 2007 to 2014 | AMI, stroke, HF |
AMI: 410, 411, I21, I22, I23; stroke: 431, 432, 434, I61, I62, I63, I64; HF: 428, I50 (ICD-9 and 10). NR |
NR |
| Lin et al. (2020) [95] | Taiwan National Health Insurance Research Database from 2008 to 2012 | AMI, stroke, PCI, CABG, all-cause mortality. |
AMI: 410–410.9, stroke: 430–437, PCI: 36.0–36.03, 36.05–36.09; CABG: 36.1–36.99, V45.81 (ICD-9). NR |
NR |
| Madsen et al. (2020) [96] | Copenhagen General Population Study from 2003 to 2015 | AMI, CABG, PCI, stroke, CV death. |
AMI: I21-I22; CABG: NOMESCO: KNFA-KFNE; PCI: NOMESCO: KFNG00–05); stroke: I60-I61, I63-I64; CV death: I01-I87, I95-I99, R96 (ICD-10) NR |
NR |
| Petersen et al. (2020) [97] | Danish health data including the clinical laboratory information system (LABKA), the Danish National Patient Registry, the Aarhus University Prescription Database (AUPD) and the Danish Civil Registration System from 2006 to 2014. | AMI, stroke, all-cause mortality. |
AMI: I21; stroke: I61, I62, I64, I65 (ICD-10). NR |
NR |
| Seong et al. (2020) [98] | National Health Insurance Service-Elderly Cohort Database (NHIS-ECD) by the Korean National Health Insurance Service (KNHIS) from 2003 to 2008. | AMI, IHD, stroke, and CV death. |
AMI: I21-I23, I25.2; IHD: I20-I25; stroke: I63; CV death: I60-I69 (ICD-10). Any position. |
NR |
Abbreviations: NR Not reported, ICD International Classification of Diseases, CV Cardiovascular, AMI Acute myocardial infarction, IHD Ischemic heart disease, ACS Acute coronary syndrome, CAD Coronary artery disease, UA Unstable angina, PVD Peripheral vascular disease, HF Heart failure, TIA Transient ischemic attack, PCI Percutaneous coronary intervention, CABG Coronary artery bypass graft
Table 2.
Most common components of MACE (N = 58 studies)
| MACE Components | ICD-9 | ICD-10 | Both ICD-9/10 |
|---|---|---|---|
| Individual components | |||
| AMI (n = 45) | 29 | 14 | 2 |
| Acute coronary syndrome / Ischemic Heart disease (n = 18) | 12 | 5 | 1 |
| Stroke (n = 50) | 30 | 17 | 3 |
| Heart failure (n = 15) | 12 | 2 | 1 |
| All-cause death (n = 15) | 10 | 5 | 0 |
| CV death (n = 9) | 1 | 6 | 2 |
| Revascularization (n = 11) | 7 | 4 | 0 |
| Other (n = 19) | 15 | 3 | 1 |
| Combinations | |||
| Three-point MACE: AMI + Stroke+CV death (n = 5) | 1 | 3 | 1 |
| Four-point MACE: AMI + Stroke+UA + CV death (n = 0) | 0 | 0 | 0 |
| Five-point MACE: AMI + Stroke+UA + HF + CV death (n = 0) | 0 | 0 | 0 |
| AMI + stroke+all-cause death (n = 8) | 5 | 3 | 0 |
| AMI + stroke+HF + CV death (n = 0) | 0 | 0 | 0 |
| AMI + stroke+HF + all-cause death (n = 2) | 1 | 1 | 0 |
Abbreviations: MACE Major adverse cardiovascular events, ICD International Classification of Diseases, AMI Acute myocardial infarction, CV Cardiovascular, UA Unstable angina, HF Heart failure
Table 3.
Most commonly used MACE components
| MACE Components | Frequency, n (%) |
|---|---|
| AMI, stroke | 9 (15.5) |
| AMI, stroke, all-cause death | 8 (13.8) |
| AMI, stroke, CV death | 5 (8.6) |
| ACS/IHD, stroke | 3 (5.2) |
| AMI, stroke, HF | 3 (5.2) |
| Other definitions (≤2 studies using each) | 30 (51.7) |
Abbreviations: MACE Major adverse cardiovascular events, AMI Acute myocardial infarction, CV Cardiovascular, ACS Acute coronary syndrome, IHD Ischemic heart disease, HF Heart failure
MACE component definitions
Acute myocardial infarction
There were 45 studies that included AMI as a component of MACE (Table 2). Of these, 64.4% (29/45) defined outcomes using ICD-9-CM and 31.1% (14/45) used ICD-10-CM. Among these studies, 20% (9/45) defined AMI in the primary diagnosis position, 6.7% (3/45) in any position, and 73.3% (33/45) did not report the position used. The most common diagnosis codes were: 410.xx, making up 72% (21/29) of the ICD-9-CM studies; and I21.xx, I22.xx, making up 35.7% (5/14) of the ICD-10-CM studies (Table 4).
Table 4.
ICD codes by clinical outcome
| Outcome | ICD-9 code | ICD-10 Code | Both ICD-9/10 Codes |
|---|---|---|---|
| AMI (n = 45) |
1. 410.xx (n = 21) 2. 410.xx, 412.xx (n = 3) 3. Other (n = 5) |
1. I21.xx, I22.xx (n = 5) 2. I21.xx (n = 4) 3. Other (n = 5) |
1. 410.xx, I21.xx, I22.xx (n = 1) 2. 410–411.xx, I21-I23.xx (n = 1) |
| ACS/IHD (n = 18) |
1. 410.xx-414.xx (n = 3) 2. 410.xx, 411.xx (n = 2) 3. Other (n = 7) |
1. I21.xx-I24.xx (n = 2) 2. Other (n = 3) |
1. 410.xx, 411.xx, I20.0, I21.xx, I22.xx (n = 1) |
| Stroke (n = 50) |
1. 433.xx, 434.xx, 436.xx (n = 4) 2. 430.xx-437.xx (n = 4) 3. Other (n = 22) |
1. I63.xx, I65.xx, I66.xx (n = 3) 2. I63.xx (n = 3) 3. Other (n = 11) |
2. 430.xx, 431.xx, 434.xx, 436.xx, I60.xx, I61.xx, I63.3-I63.9, I66.xx (n = 1) 3. 433.xx-436, excluding 434.9x, I63, I64, G45 (n = 1) 4. 431.xx-432.xx, 434.xx, I61.xx-I64.xx (n = 1) |
| Heart Failure (n = 15) |
1. 428.xx (n = 6) 2. Other (n = 6) |
1. I11.0, I50.xx, I97.1 (n = 1) 2. I50.xx, K76.1, I97.1, I11.0 (n = 1) |
1. 428.xx, I50.xx (n = 1) |
| CV Death (n = 9) | 1. None listed (n = 1) |
1. I00.xx-I99.xx (n = 2) 2. I46.1, I46.9 (n = 1) 3. Other or none listed (n = 3) |
1. 411.xx-414.xx, 415.xx-417.xx, 420.xx-427.xx, 428.xx, 429.xx, 432.xx, 433.xx, 435.xx, 437.xx, 785.51, I20.xx, I23.xx-I25.xx, I46.9, I30.xx-I52.xx, I62.xx, I63.0-I63.2, I64.xx, I65.xx, I67.xx, I68.xx, R57.0 (n = 1) 2. 410.xx-414.xx, 428.xx, 430.xx-438.xx, I20.xx–I25.xx, I50.xx, I60.xx-I69.xx (n = 1) |
Abbreviations: ICD International Classification of Diseases, AMI Acute myocardial infarction, ACS Acute Coronary Syndrome, IHD Ischemic Heart Disease, CV Cardiovascular
Acute coronary syndrome / ischemic heart disease
There were 18 studies that defined ACS/IHD as a component of MACE. ICD-9-CM diagnosis codes only were used in 66.7% (12/18) of studies and 27.7% (5/18) used ICD-10-CM only. Studies used the primary diagnosis position 22.2% (4/18), any position 11.1% (2/18), and did not report the position 66.7% (12/18) of the time. The most common diagnosis codes were: 410–414.xx, 25% (3/12) of the ICD-9-CM studies; and I21-I24.xx, 40% (2/5) of the ICD-10-CM studies.
Stroke
There were 50 studies that included stroke, either ischemic or hemorrhagic, as a component of MACE. Of these, 60% (30/50) utilized ICD-9-CM only and 34% (17/50) used ICD-10-CM only. The primary diagnosis position was used 24% (12/50) of the time, any position used 8% (4/50), and no position reported 68% (34/50) of the time. Diagnosis codes used to define stroke were highly variable with no clear most common definition. Codes included: 433.xx, 434.xx, 436.xx, 13.3% (4/30) of ICD-9-CM studies; 430–437.xx, 13.3% (4/30) of ICD-9-CM studies; I63.xx, I65.xx, I66.xx, 17.6% of ICD-10-CM studies (3/17); and I63.xx, 17.6% (3/17) of ICD-10-CM studies.
Heart failure
A total of 15 studies included HF as a component of MACE. Of these studies, 80% (12/15) used ICD-9-CM only, and 13.3% (2/15) used ICD-10-CM only. The primary diagnosis position was used 20% (3/15) of the time but was otherwise not reported in 80% (12/15) of studies. The most common diagnosis codes used were: 428.xx, 50% (6/12) of ICD-9-CM studies; I11.0, I50.xx, I97.1, 50% (1/2) of ICD-10-CM studies; and I50.xx, K76.1, I97.1, I11.0, 50% (1/2) of ICD-10-CM studies.
All-cause death and cardiovascular death
There were nine studies that included cardiovascular death as a component of MACE. Of these, 11.1% (1/9) of studies utilized ICD-9-CM codes only for MACE components and 66.7% (6/9) used ICD-10-CM. The diagnosis position for cardiovascular death was primary 11.1% (1/9), any position 33.3% (3/9), and not reported 55.6% (5/9) of the time. The most common diagnosis codes used were: No codes listed, 100% (1/1) for studies using ICD-9-CM only; and I00.xx-I99.xx, 33.3% (2/6) for those using ICD-10-CM only. There were 15 studies including all-cause death as a component of MACE. Due to the nature of all-cause death, diagnosis codes positions are not necessary and were not reported.
Discussion
In our systematic review, we found substantial heterogeneity for MACE composite endpoints used in the literature. The two most common composite MACE definitions were “AMI and stroke”, and “AMI, stroke, and all-cause death,” but they only made up 15.5 and 13.8% of studies, respectively. Compared to MACE definitions used in RCTs, only 8.6% of included observational studies had definitions aligned with three-point MACE and none match four-point or five-point MACE. A large majority of studies included AMI and stroke but there was a lack of consensus with other components included in composite MACE endpoints. For instance, over half of included publications defined MACE using a definition that only was concordant with up to one other study. This diversity makes it challenging to compare findings across studies or to aggregate multiple study results for meta-analyses or systematic reviews when considering different treatment or research questions. Addressing the heterogeneity of MACE definitions used in practice requires attention due to the advantages of the MACE endpoint. Utilizing MACE as a composite outcome can potentially reduce the number of patients that need to be enrolled or identified in a retrospective cohort study, and reduce the follow-up time necessary to observe differences between different treatment groups [99]. These benefits not only potentially reduce research costs but can more expediently answer clinical questions, leading to improved patient care. Therefore, given that MACE endpoints will likely see increasing use as time goes on, there should be a continued effort to standardize and transparently report MACE definitions used in observational studies.
In 2007, findings similar to our study were observed when comparing prospective trials conducted for percutaneous coronary interventions [100]. However, although the FDA in 2008 and the EMA in 2012 attempted to standardize the MACE endpoint definition for RCTs, we found a continued discordance between how observational studies define MACE. Furthermore, we found that the majority of studies did not include mention of the diagnosis position used to define outcomes. Lack of this information prevents the ability to distinguish between incident and prevalent outcomes. While the primary position has been historically used in observational studies to define incident outcomes, the use of only primary diagnosis positions, compared to using secondary positions, may underestimate the rates of MACE for prevalent conditions [101]. The lack of reporting of diagnosis position prevents the ability to make this distinction and prohibits the full interpretation of findings.
Heterogeneity not only existed in defining MACE components but also in which ICD-9-CM and ICD-10-CM codes were used to define each individual MACE component. In our study, none of the top five components of MACE had a consensus ICD-9-CM or ICD-10-CM code that was used among all of the studies. These discrepancies contribute additional variability to our findings, as outcome classification, assuming a standard definition, inherently relies on the providers and medical billers accurately coding diseases. For example, in a study conducted in 11 Canadian emergency departments, the authors reported about 82–86% of agreement with regards to coding hospital conditions [102]. Additionally, a study looking at stroke data collected through the United States Paul Coverdell National Acute Stroke Program found that discordance existed with how strokes were coded, especially at smaller hospitals (< 200 beds) and when differentiating between ischemic strokes, transient ischemic attacks, and subarachnoid and intracerebral hemorrhages [103].
There have been many attempts to validate diagnosis or procedure codes for various MACE component outcomes [32, 104]. Research has predominantly focused on the older ICD-9-CM codes, particularly studies using U.S. administrative data, but studies utilizing ICD-10-CM have more recently been published. Using data from the Centers for Medicare and Medicaid Services, a 2018 study found that the most accurate ICD-9-CM code for coding AMI was 410.xx, with a positive predictive value of 67% [104]. Additionally, the U.S. FDA commissioned the Mini-Sentinel pilot program to systematically assess the validation of common healthcare outcomes in administrative databases [32]. These studies were important steps to identify standard outcome definitions for use across disparate data sources and populations. As part of the program, systematic literature reviews from the U.S. and Canada found that the most accurate ICD-9-CM code for heart failure was 428.xx, with a positive predictive value of 84–100%, while the most accurate ICD-9-CM codes for stroke were 430.x, 431.x and 434.x, all with separate positive predictive values > 80%, and 436.x, which had a positive predictive value > 70% [32, 33]. The Mini-Sentinel program also assessed the ICD-9-CM codes, 410.× 0 or 410.× 1, for AMI and found a positive predictive value of 76.3–94.3% [105]. Fewer validations exist for ICD-10-CM codes. One study conducted in Japan attempted to validate the ICD-10-CM code I21.x for AMI and found a positive predictive value of 82.5% [106]. Another study in Canada found the positive predictive value for correctly coding stroke was 92% for the ICD-10-CM codes, I60.x-I61.x, I63.x-I64.x, H34.1 and G45.x [69]. Based on our findings, the most common ICD-9-CM and 10-CM codes used for AMI were also the most validated, 410.xx and I21.xx, respectively. The most validated and most common ICD-9-CM code used for heart failure was 428.xx. On the other hand, stroke had some discrepancies when comparing the most validated versus the most commonly used ICD codes. This discordance likely existed because of the differences with which stroke can be defined, particularly whether to include acute ischemic strokes with transient ischemic attacks, intracerebral hemorrhages or subarachnoid hemorrhages [69].
There are several limitations to our study. We excluded papers published before 2010, prior to the first published reviews of the Mini-Sentinel program, in order to present a contemporary review of the subject [32]. However, this cutoff likely skewed our results towards more modern MACE definitions and excluded different definitions that were potentially used for older publications. Older studies likely exhibited greater variety in the outcome definitions used. Additionally, because the words “major adverse cardiovascular events” were rarely explicitly written, we had to include any composite definitions that were thought to represent MACE but were listed using another composite name, such “acute cardiovascular events,” based on the discretion of the reviewer. This method potentially excluded studies that used variations of MACE endpoints, but did not conform to similar naming conventions.
Conclusion
Significant heterogeneity exists in how MACE is defined and which ICD-9-CM and 10-CM codes are used to represent each respective MACE outcome in observational studies using administrative databases. The utility of future studies will improve with the use of validated definitions of AMI, stroke, cardiovascular mortality, unstable angina, and HF for the evaluation of MACE outcomes. Further, investigators should ensure that both the ICD diagnosis codes and the code positions are reported in a transparent way. Given the significant heterogeneity that already exists across administrative databases, we recommend the use of more standardized MACE definitions and corresponding ICD-9-CM and ICD-10-CM codes. This practice will allow researchers to more accurately compare findings across studies improve the reproducibility of observational studies, and decrease the potential for misleading conclusions.
Supplementary Information
Additional file 1: Supplementary Text 1. Systematic Review Protocol.
Additional file 2: Supplementary Table 1. PRISMA 2020 Checklist.
Additional file 3: Supplementary Text 2. Search terms.
Acknowledgements
Not applicable.
Abbreviations
- ACS
Acute coronary syndrome
- ACS/IHD
Acute coronary syndrome or ischemic heart disease
- AMI
Acute myocardial infarction
- CABG
Coronary artery bypass graft
- CAD
Coronary artery disease
- CV
Cardiovascular
- HF
Heart failure
- ICD
International Classification of Diseases
- ICD-9-CM
International Classification of Diseases, 9th Revision, Clinical Modification
- ICD-10-CM
International Classification of Diseases, 10th Revision, Clinical Modification
- IHD
Ischemic heart disease
- MACE
Major adverse cardiovascular events
- PCI
Percutaneous coronary intervention
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- PRISMA-P
Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols
- PROSPERO
International Prospective Register of Systematic Reviews
- PVD
Peripheral vascular disease
- RCT
Randomized controlled trial
- TIA
Transient ischemic attack
- UA
Unstable angina
Authors’ contributions
E.B., L.H., E.S., K.W.M, and S.G. took part in conceiving the initial plans of the study. E.B., L.H., and E.S. developed the search criteria, reviewing abstracts and full texts, extracted study data, and prepared the initial draft of the manuscript. E.B., L.H., E.S., K.W.M, and S.G took part in analyzing and interpreting the results, providing critical revisions for the manuscript, and approving the final manuscript.
Funding
Unfunded.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
E.B., L.H., and E.S. declare no competing interests. K.W.M reports investigator-initiated grants from Seqirus, Pfizer and Sanofi Pasteur. S.G. reports grants from Seqirus, Sanofi; and consulting or speaker fees from Sanofi, Seqirus, Merck, and the Gerontological Society of America related to vaccines or nursing home care quality. The content and views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Elliott Bosco and Leon Hsueh contributed equally to this work.
References
- 1.Gal D, Thijs B, Glanzel W, Sipido KR. Hot topics and trends in cardiovascular research. Eur Heart J. 2019;40(28):2363–2374. doi: 10.1093/eurheartj/ehz282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 3.Sharma A, Pagidipati NJ, Califf RM, McGuire DK, Green JB, Demets D, George JT, Gerstein HC, Hobbs T, Holman RR, et al. Impact of regulatory guidance on evaluating cardiovascular risk of new glucose-lowering therapies to treat type 2 diabetes mellitus: lessons learned and future directions. Circulation. 2020;141(10):843–862. doi: 10.1161/CIRCULATIONAHA.119.041022. [DOI] [PubMed] [Google Scholar]
- 4.Marx N, McGuire DK, Perkovic V, Woerle HJ, Broedl UC, von Eynatten M, George JT, Rosenstock J. Composite primary end points in cardiovascular outcomes trials involving type 2 diabetes patients: should unstable angina be included in the primary end point? Diabetes Care. 2017;40(9):1144–1151. doi: 10.2337/dc17-0068. [DOI] [PubMed] [Google Scholar]
- 5.Gavrielov-Yusim N, Friger M. Use of administrative medical databases in population-based research. J Epidemiol Community Health. 2014;68(3):283–287. doi: 10.1136/jech-2013-202744. [DOI] [PubMed] [Google Scholar]
- 6.Franklin JM, Schneeweiss S. When and how can real world data analyses substitute for randomized controlled trials? Clin Pharmacol Ther. 2017;102(6):924–933. doi: 10.1002/cpt.857. [DOI] [PubMed] [Google Scholar]
- 7.Wang SV, Pinheiro S, Hua W, Arlett P, Uyama Y, Berlin JA, Bartels DB, Kahler KH, Bessette LG, Schneeweiss S. STaRT-RWE: structured template for planning and reporting on the implementation of real world evidence studies. BMJ (Clinical research ed) 2021;372:m4856. doi: 10.1136/bmj.m4856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Franklin JM, Patorno E, Desai RJ, Glynn RJ, Martin D, Quinto K, Pawar A, Bessette LG, Lee H, Garry EM, et al. Emulating randomized clinical trials with nonrandomized real-world evidence studies: first results from the RCT DUPLICATE Initiative. Circulation. 2021;143(10):1002–1013. doi: 10.1161/CIRCULATIONAHA.120.051718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.International Statistical Classification of Diseases and Related Health Problems (ICD). World Health Organization; 2021. https://www.who.int/standards/classifications/classification-of-diseases. Accessed 28 Feb 2021.
- 10.McCormick N, Bhole V, Lacaille D, Avina-Zubieta JA. Validity of diagnostic codes for acute stroke in administrative databases: a systematic review. PLoS One. 2015;10(8):e0135834. doi: 10.1371/journal.pone.0135834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCormick N, Lacaille D, Bhole V, Avina-Zubieta JA. Validity of myocardial infarction diagnoses in administrative databases: a systematic review. PLoS One. 2014;9(3):e92286. doi: 10.1371/journal.pone.0092286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCormick N, Lacaille D, Bhole V, Avina-Zubieta JA. Validity of heart failure diagnoses in administrative databases: a systematic review and meta-analysis. PLoS One. 2014;9(8):e104519. doi: 10.1371/journal.pone.0104519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, Group P-P Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clinical research ed) 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wallace B, Small K, Brodley CE, Lau J, Trikalinos TA. Proceedings of the ACM International Health Informatics Symposium (IHI) 2012. Deploying an interactive machine learning system in an evidence-based practice center: abstrackr; pp. 819–824. [Google Scholar]
- 16.Chapman RH, Yeaw J, Roberts CS. Association between adherence to calcium-channel blocker and statin medications and likelihood of cardiovascular events among US managed care enrollees. BMC Cardiovasc Disord. 2010;10:29. doi: 10.1186/1471-2261-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gudbjornsson B, Thorsteinsson SB, Sigvaldason H, Einarsdottir R, Johannsson M, Zoega H, Halldorsson M, Thorgeirsson G. Rofecoxib, but not celecoxib, increases the risk of thromboembolic cardiovascular events in young adults-a nationwide registry-based study. Eur J Clin Pharmacol. 2010;66(6):619–625. doi: 10.1007/s00228-010-0789-2. [DOI] [PubMed] [Google Scholar]
- 18.Charlot M, Grove EL, Hansen PR, Olesen JB, Ahlehoff O, Selmer C, Lindhardsen J, Madsen JK, Køber L, Torp-Pedersen C, et al. Proton pump inhibitor use and risk of adverse cardiovascular events in aspirin treated patients with first time myocardial infarction: nationwide propensity score matched study. BMJ (Clinical research ed) 2011;342:d2690. doi: 10.1136/bmj.d2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Madsen M, Davidsen M, Rasmussen S, Abildstrom SZ, Osler M. The validity of the diagnosis of acute myocardial infarction in routine statistics: a comparison of mortality and hospital discharge data with the Danish MONICA registry. J Clin Epidemiol. 2003;56(2):124–130. doi: 10.1016/s0895-4356(02)00591-7. [DOI] [PubMed] [Google Scholar]
- 20.Krarup LH, Boysen G, Janjua H, Prescott E, Truelsen T. Validity of stroke diagnoses in a National Register of Patients. Neuroepidemiology. 2007;28(3):150–154. doi: 10.1159/000102143. [DOI] [PubMed] [Google Scholar]
- 21.Kociol RD, Hammill BG, Hernandez AF, Klaskala W, Mills RM, Curtis LH, Fonarow GC. Pharmacologic prophylaxis for venous thromboembolism and 30-day outcomes among older patients hospitalized with heart failure: an analysis from the ADHERE national registry linked to Medicare claims. Clin Cardiol. 2011;34(11):682–688. doi: 10.1002/clc.20986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen ZY, Chiang CH, Huang CC, Chung CM, Chan WL, Huang PH, Lin SJ, Chen JW, Leu HB. The association of tooth scaling and decreased cardiovascular disease: a nationwide population-based study. Am J Med. 2012;125(6):568–575. doi: 10.1016/j.amjmed.2011.10.034. [DOI] [PubMed] [Google Scholar]
- 23.Chen HJ, Bai CH, Yeh WT, Chiu HC, Pan WH. Influence of metabolic syndrome and general obesity on the risk of ischemic stroke. Stroke. 2006;37(4):1060–1064. doi: 10.1161/01.STR.0000206458.58142.f3. [DOI] [PubMed] [Google Scholar]
- 24.Degli Esposti L, Saragoni S, Batacchi P, Benemei S, Geppetti P, Sturani A, Buda S, Degli Esposti E. Adherence to statin treatment and health outcomes in an Italian cohort of newly treated patients: results from an administrative database analysis. Clin Ther. 2012;34(1):190–199. doi: 10.1016/j.clinthera.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 25.Parker ED, Margolis KL, Trower NK, Magid DJ, Tavel HM, Shetterly SM, Ho PM, Swain BE, O'Connor PJ. Comparative effectiveness of 2 β-blockers in hypertensive patients. Arch Intern Med. 2012;172(18):1406–1412. doi: 10.1001/archinternmed.2012.4276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Karthikesalingam A, Bahia SS, Patterson BO, Peach G, Vidal-Diez A, Ray KK, Sharma R, Hinchliffe RJ, Holt PJ, Thompson MM. The shortfall in long-term survival of patients with repaired thoracic or abdominal aortic aneurysms: retrospective case-control analysis of hospital episode statistics. Eur J Vasc Endovasc Surg. 2013;46(5):533–541. doi: 10.1016/j.ejvs.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 27.Mortensen EM, Halm EA, Pugh MJ, Copeland LA, Metersky M, Fine MJ, Johnson CS, Alvarez CA, Frei CR, Good C, et al. Association of azithromycin with mortality and cardiovascular events among older patients hospitalized with pneumonia. JAMA. 2014;311(21):2199–2208. doi: 10.1001/jama.2014.4304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Neumann A, Maura G, Weill A, Ricordeau P, Alla F, Allemand H. Comparative effectiveness of rosuvastatin versus simvastatin in primary prevention among new users: a cohort study in the French national health insurance database. Pharmacoepidemiol Drug Saf. 2014;23(3):240–250. doi: 10.1002/pds.3544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vanasse A, Courteau J, Asghari S, Leroux D, Cloutier L. Health inequalities associated with neighbourhood deprivation in the Quebec population with hypertension in primary prevention of cardiovascular disease. Chronic Dis Inj Can. 2014;34(4):181–194. [PubMed] [Google Scholar]
- 30.Chou SH, Tung YC, Lin YS, Wu LS, Lin CP, Liou EJ, Chang CJ, Kung S, Chu PH. Major adverse cardiovascular events in treated periodontitis: a population-based follow-up study from Taiwan. PLoS One. 2015;10(6):e0130807. doi: 10.1371/journal.pone.0130807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Desai JR, Vazquez-Benitez G, Xu Z, Schroeder EB, Karter AJ, Steiner JF, Nichols GA, Reynolds K, Xu S, Newton K, et al. Who must we target now to minimize future cardiovascular events and total mortality?: lessons from the surveillance, prevention and management of diabetes mellitus (SUPREME-DM) cohort study. Circ Cardiovas Qual Outcomes. 2015;8(5):508–516. doi: 10.1161/CIRCOUTCOMES.115.001717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saczynski JS, Andrade SE, Harrold LR, Tjia J, Cutrona SL, Dodd KS, Goldberg RJ, Gurwitz JH. A systematic review of validated methods for identifying heart failure using administrative data. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):129–140. doi: 10.1002/pds.2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Andrade SE, Harrold LR, Tjia J, Cutrona SL, Saczynski JS, Dodd KS, Goldberg RJ, Gurwitz JH. A systematic review of validated methods for identifying cerebrovascular accident or transient ischemic attack using administrative data. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):100–128. doi: 10.1002/pds.2312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362(23):2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 35.Doll JA, Hellkamp A, Thomas L, Ho PM, Kontos MC, Whooley MA, Boyden TF, Peterson ED, Wang TY. Effectiveness of cardiac rehabilitation among older patients after acute myocardial infarction. Am Heart J. 2015;170(5):855–864. doi: 10.1016/j.ahj.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 36.Jernberg T, Hasvold P, Henriksson M, Hjelm H, Thuresson M, Janzon M. Cardiovascular risk in post-myocardial infarction patients: nationwide real world data demonstrate the importance of a long-term perspective. Eur Heart J. 2015;36(19):1163–1170. doi: 10.1093/eurheartj/ehu505. [DOI] [PubMed] [Google Scholar]
- 37.Linnersjö A, Hammar N, Gustavsson A, Reuterwall C. Recent time trends in acute myocardial infarction in Stockholm, Sweden. Int J Cardiol. 2000;76(1):17–21. doi: 10.1016/s0167-5273(00)00366-1. [DOI] [PubMed] [Google Scholar]
- 38.Korsnes JS, Davis KL, Ariely R, Bell CF, Mitra D. Health care resource utilization and costs associated with nonfatal major adverse cardiovascular events. J Manag Care Spec Pharm. 2015;21(6):443–450. doi: 10.18553/jmcp.2015.21.6.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Roussel R, Chaignot C, Weill A, Travert F, Hansel B, Marre M, Ricordeau P, Alla F, Allemand H. Use of fibrates monotherapy in people with diabetes and high cardiovascular risk in primary care: a French nationwide cohort study based on national administrative databases. PLoS One. 2015;10(9):e0137733. doi: 10.1371/journal.pone.0137733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sirois C, Moisan J, Poirier P, Gregoire JP. Comparative effectiveness of cardioprotective drugs in elderly individuals with type 2 diabetes. Int J Clin Pract. 2015;69(3):305–312. doi: 10.1111/ijcp.12503. [DOI] [PubMed] [Google Scholar]
- 41.Levy AR, Tamblyn RM, Fitchett D, McLeod PJ, Hanley JA. Coding accuracy of hospital discharge data for elderly survivors of myocardial infarction. Can J Cardiol. 1999;15(11):1277–1282. [PubMed] [Google Scholar]
- 42.Stochkendahl MJ, Mickley H, Vach W, Aziz A, Christensen HW, Hartvigsen J, Høilund-Carlsen PF. Clinical characteristics, myocardial perfusion deficits, and clinical outcomes of patients with non-specific chest pain hospitalized for suspected acute coronary syndrome: a 4-year prospective cohort study. Int J Cardiol. 2015;182:126–131. doi: 10.1016/j.ijcard.2014.12.054. [DOI] [PubMed] [Google Scholar]
- 43.Blin P, Philippe F, Bouee S, Laurendeau C, Torreton E, Gourmelin J, Leproust S, Levy-Bachelot L, Steg PG. Outcomes following acute hospitalised myocardial infarction in France: an insurance claims database analysis. Int J Cardiol. 2016;219:387–393. doi: 10.1016/j.ijcard.2016.06.102. [DOI] [PubMed] [Google Scholar]
- 44.Cheng CA, Chien WC, Hsu CY, Lin HC, Chiu HW. Risk analysis of carotid stent from a population-based database in Taiwan. Medicine. 2016;95(35):e4747. doi: 10.1097/MD.0000000000004747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chuang CS, Ho SC, Lin CL, Lin MC, Kao CH. Risk of cerebrovascular events in pneumoconiosis patients: a population-based study, 1996-2011. Medicine. 2016;95(9):e2944. doi: 10.1097/MD.0000000000002944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fortuna LA, Pawloski PA, Parker ED, Trower NK, Kottke TE. Proton pump inhibitor use by aspirin-treated coronary artery disease patients is not associated with increased risk of cardiovascular events. Eur Heart J Cardiovasc Pharmacother. 2016;2(1):13–19. doi: 10.1093/ehjcvp/pvv036. [DOI] [PubMed] [Google Scholar]
- 47.Kottke TE, Baechler CJ, Parker ED. Accuracy of heart disease prevalence estimated from claims data compared with an electronic health record. Prev Chronic Dis. 2012;9:E141. doi: 10.5888/pcd9.120009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hsu CY, Chen YT, Huang PH, Leu HB, Su YW, Chiang CH, Chen JW, Chen TJ, Lin SJ, Chan WL. The association between urinary calculi and increased risk of future cardiovascular events: a nationwide population-based study. J Cardiol. 2016;67(5):463–470. doi: 10.1016/j.jjcc.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 49.Lindblad U, Råstam L, Ranstam J, Peterson M. Validity of register data on acute myocardial infarction and acute stroke: the Skaraborg hypertension project. Scand J Soc Med. 1993;21(1):3–9. doi: 10.1177/140349489302100102. [DOI] [PubMed] [Google Scholar]
- 50.Cheng C-L, Kao Y-HY, Lin S-J, Lee C-H, Lai ML. Validation of the national health insurance research database with ischemic stroke cases in Taiwan. Pharmacoepidemiol Drug Saf. 2011;20(3):236–242. doi: 10.1002/pds.2087. [DOI] [PubMed] [Google Scholar]
- 51.Shih C-J, Chen H-T, Chao P-W, Kuo S-C, Li S-Y, Yang C-Y, Tarng D-C, Ou S-M, Chen Y-T. Angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers and the risk of major adverse cardiac events in patients with diabetes and prior stroke: a nationwide study. J Hypertens. 2016;34(3):567–575. doi: 10.1097/HJH.0000000000000804. [DOI] [PubMed] [Google Scholar]
- 52.Hsieh CY, Chen CH, Li CY, Lai ML. Validating the diagnosis of acute ischemic stroke in a National Health Insurance claims database. J Formos Med Assoc. 2015;114(3):254–259. doi: 10.1016/j.jfma.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 53.Solomon DH, Liu CC, Kuo IH, Zak A, Kim SC. Effects of colchicine on risk of cardiovascular events and mortality among patients with gout: a cohort study using electronic medical records linked with Medicare claims. Ann Rheum Dis. 2016;75(9):1674–1679. doi: 10.1136/annrheumdis-2015-207984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH. Accuracy of Medicare claims-based diagnosis of acute myocardial infarction: estimating positive predictive value on the basis of review of hospital records. Am Heart J. 2004;148(1):99–104. doi: 10.1016/j.ahj.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 55.Birman-Deych E, Waterman AD, Yan Y, Nilasena DS, Radford MJ, Gage BF. Accuracy of ICD-9-CM codes for identifying cardiovascular and stroke risk factors. Med Care. 2005;43(5):480–485. doi: 10.1097/01.mlr.0000160417.39497.a9. [DOI] [PubMed] [Google Scholar]
- 56.Babazade R, Yilmaz HO, Leung SM, Zimmerman NM, Turan A. Systemic lupus erythematosus is associated with increased adverse postoperative renal outcomes and mortality: a historical cohort study using administrative health data. Anesth Analg. 2017;124(4):1118–1126. doi: 10.1213/ANE.0000000000001911. [DOI] [PubMed] [Google Scholar]
- 57.de Miguel-Yanes JM, Jimenez-Garcia R, Hernandez-Barrera V, Mendez-Bailon M, de Miguel-Diez J, Lopez-de-Andres A. Impact of type 2 diabetes mellitus on in-hospital-mortality after major cardiovascular events in Spain (2002-2014) Cardiovasc Diabetol. 2017;16(1):126. doi: 10.1186/s12933-017-0609-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lindahl B, Baron T, Erlinge D, Hadziosmanovic N, Nordenskjöld A, Gard A, Jernberg T. Medical therapy for secondary prevention and long-term outcome in patients with myocardial infarction with nonobstructive coronary artery disease. Circulation. 2017;135(16):1481–1489. doi: 10.1161/CIRCULATIONAHA.116.026336. [DOI] [PubMed] [Google Scholar]
- 59.Policardo L, Seghieri G, Francesconi P, Anichini R, Franconi F, Del Prato S. Gender difference in diabetes related excess risk of cardiovascular events: when does the ‘risk window’ open? J Diabetes Complicat. 2017;31(1):74–79. doi: 10.1016/j.jdiacomp.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 60.Tung YC, Huang YC, Wu LS, Chang CJ, Chu PH. Medication compliance and clinical outcomes of fixed-dose combinations vs free combinations of an angiotensin II receptor blocker and a calcium channel blocker in hypertension treatment. J Clin Hypertens (Greenwich) 2017;19(10):983–989. doi: 10.1111/jch.13035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Arinze N, Farber A, Sachs T, Patts G, Kalish J, Kuhnen A, Kasotakis G, Siracuse JJ. The effect of statin use and intensity on stroke and myocardial infarction after carotid endarterectomy. J Vasc Surg. 2018;68(5):1398–1405. doi: 10.1016/j.jvs.2018.02.035. [DOI] [PubMed] [Google Scholar]
- 62.Baviera M, Bertele V, Avanzini F, Vannini T, Tettamanti M, Fortino I, Bortolotti A, Merlino L, Roncaglioni MC. Peripheral arterial disease: Changes in clinical outcomes and therapeutic strategies in two cohorts, from 2002 to 2008 and from 2008 to 2014. A population-based study. Eur J Prev Cardiol. 2018;25(16):1735–1743. doi: 10.1177/2047487318770299. [DOI] [PubMed] [Google Scholar]
- 63.Chan CW, Yu CL, Lin JC, Hsieh YC, Lin CC, Hung CY, Li CH, Liao YC, Lo CP, Huang JL, et al. Glitazones and alpha-glucosidase inhibitors as the second-line oral anti-diabetic agents added to metformin reduce cardiovascular risk in type 2 diabetes patients: a nationwide cohort observational study. Cardiovasc Diabetol. 2018;17(1):20. doi: 10.1186/s12933-018-0663-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wu VC, Chen SW, Ting PC, Chang CH, Wu M, Lin MS, Hsieh MJ, Wang CY, Chang SH, Hung KC, et al. Selection of β-blocker in patients with cirrhosis and acute myocardial infarction: a 13-year nationwide population-based study in Asia. J Am Heart Assoc. 2018;7(19):e008982. doi: 10.1161/JAHA.118.008982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cheng CL, Lee CH, Chen PS, Li YH, Lin SJ, Yang YH. Validation of acute myocardial infarction cases in the national health insurance research database in Taiwan. J Epidemiol. 2014;24(6):500–507. doi: 10.2188/jea.JE20140076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Degli Esposti L, Perrone V, Veronesi C, Buda S, Rossini R. All-cause mortality, cardiovascular events, and health care costs after 12 months of dual platelet aggregation inhibition after acute myocardial infarction in real-world patients: findings from the platelet-aggregation inhibition: persistence with treatment and cardiovascular events in real world (PIPER) study. Vasc Health Risk Manag. 2018;14:383–392. doi: 10.2147/VHRM.S162004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hussain MA, Saposnik G, Raju S, Salata K, Mamdani M, Tu JV, Bhatt DL, Verma S, Al-Omran M. Association between statin use and cardiovascular events after carotid artery revascularization. J Am Heart Assoc. 2018;7(16):e009745. doi: 10.1161/JAHA.118.009745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Juurlink D, Preyra C, Croxford R, Chong A, Austin P, Tu J, Laupacis A. Canadian institute for health information discharge abstract database: a validation study. Toronto: ICES investigative report Institute for Clinical Evaluative Sciences; 2006. [Google Scholar]
- 69.Kokotailo RA, Hill MD. Coding of stroke and stroke risk factors using international classification of diseases, revisions 9 and 10. Stroke. 2005;36(8):1776–1781. doi: 10.1161/01.STR.0000174293.17959.a1. [DOI] [PubMed] [Google Scholar]
- 70.Jin P, Matos Diaz I, Stein L, Thaler A, Tuhrim S, Dhamoon MS. Intermediate risk of cardiac events and recurrent stroke after stroke admission in young adults. Int J Stroke. 2018;13(6):576–584. doi: 10.1177/1747493017733929. [DOI] [PubMed] [Google Scholar]
- 71.Goldstein LB. Accuracy of ICD-9-CM coding for the identification of patients with acute ischemic stroke: effect of modifier codes. Stroke. 1998;29(8):1602–1604. doi: 10.1161/01.str.29.8.1602. [DOI] [PubMed] [Google Scholar]
- 72.Roumie CL, Mitchel E, Gideon PS, Varas-Lorenzo C, Castellsague J, Griffin MR. Validation of ICD-9 codes with a high positive predictive value for incident strokes resulting in hospitalization using Medicaid health data. Pharmacoepidemiol Drug Saf. 2008;17(1):20–26. doi: 10.1002/pds.1518. [DOI] [PubMed] [Google Scholar]
- 73.Kim D, Yang PS, Kim TH, Jang E, Shin H, Kim HY, Yu HT, Uhm JS, Kim JY, Pak HN, et al. Ideal blood pressure in patients with atrial fibrillation. J Am Coll Cardiol. 2018;72(11):1233–1245. doi: 10.1016/j.jacc.2018.05.076. [DOI] [PubMed] [Google Scholar]
- 74.Kiss Z, Rokszin G, Abonyi-Toth Z, Jermendy G, Kempler P, Aradi D, Wittmann I. Dissimilar impact of type 2 diabetes on cardiovascular outcomes according to age categories: a nationwide population study from Hungary. Cardiovasc Diabetol. 2018;17(1):107. doi: 10.1186/s12933-018-0751-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ohm J, Skoglund PH, Discacciati A, Sundstrom J, Hambraeus K, Jernberg T, Svensson P. Socioeconomic status predicts second cardiovascular event in 29,226 survivors of a first myocardial infarction. Eur J Prev Cardiol. 2018;25(9):985–993. doi: 10.1177/2047487318766646. [DOI] [PubMed] [Google Scholar]
- 76.Winell K, Arffman M, Pietila A, Salomaa V. Regional differences in the incidence of diabetic cardiovascular events reflect the quality of care. Scand Cardiovasc J. 2018;52(5):232–237. doi: 10.1080/14017431.2018.1497198. [DOI] [PubMed] [Google Scholar]
- 77.Pajunen P, Koukkunen H, Ketonen M, Jerkkola T, Immonen-Räihä P, Kärjä-Koskenkari P, Mähönen M, Niemelä M, Kuulasmaa K, Palomäki P, et al. The validity of the Finnish hospital discharge register and causes of death register data on coronary heart disease. Eur J Cardiovasc Prev Rehabil. 2005;12(2):132–137. doi: 10.1097/00149831-200504000-00007. [DOI] [PubMed] [Google Scholar]
- 78.Tolonen H, Salomaa V, Torppa J, Sivenius J, Immonen-Räihä P, Lehtonen A. The validation of the Finnish hospital discharge register and causes of death register data on stroke diagnoses. Eur J Cardiovasc Prev Rehabil. 2007;14(3):380–385. doi: 10.1097/01.hjr.0000239466.26132.f2. [DOI] [PubMed] [Google Scholar]
- 79.Yang CT, Kor CT, Hsieh YP. Long-term effects of spironolactone on kidney function and hyperkalemia-associated hospitalization in patients with chronic kidney disease. J Clin Med. 2018;7(11):459. doi: 10.3390/jcm7110459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Young JB, Gauthier-Loiselle M, Bailey RA, Manceur AM, Lefebvre P, Greenberg M, Lafeuille MH, Duh MS, Bookhart B, Wysham CH. Development of predictive risk models for major adverse cardiovascular events among patients with type 2 diabetes mellitus using health insurance claims data. Cardiovasc Diabetol. 2018;17(1):118. doi: 10.1186/s12933-018-0759-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Arnaout R, Nah G, Marcus G, Tseng Z, Foster E, Harris IS, Divanji P, Klein L, Gonzalez J, Parikh N. Pregnancy complications and premature cardiovascular events among 1.6 million California pregnancies. Open Heart. 2019;6(1):e000927. doi: 10.1136/openhrt-2018-000927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chen S, Hsu WY, Lin YN, Wang CY, Wu CH, Chang KH. Incidence and risk of major adverse cardiovascular events in middle-aged patients with chronic kidney disease: a population-based cohort study. Int Urol Nephrol. 2019;51(7):1219–1227. doi: 10.1007/s11255-019-02157-7. [DOI] [PubMed] [Google Scholar]
- 83.Giral P, Neumann A, Weill A, Coste J. Cardiovascular effect of discontinuing statins for primary prevention at the age of 75 years: a nationwide population-based cohort study in France. Eur Heart J. 2019;40(43):3516–3525. doi: 10.1093/eurheartj/ehz458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hsueh CM, Wey JH, Yeh JS, Wu CH, Liou TH, Chang KH. Incidence and risk of major heart diseases in middle-aged adults with moderate to severe vision impairment: a population-based cohort study. Br J Ophthalmol. 2019;103(8):1054–1059. doi: 10.1136/bjophthalmol-2018-312471. [DOI] [PubMed] [Google Scholar]
- 85.Kim K, Kwak A, Choi CU, Kim JH, Kim MG, Oh JM, Ji E. Differences in preventing new-onset cardiovascular events with statin therapy in seniors aged 75 years and over: a cohort study in the South Korean National Health Insurance Database. Basic Clin Pharmacol Toxicol. 2019;125(2):108–116. doi: 10.1111/bcpt.13229. [DOI] [PubMed] [Google Scholar]
- 86.Kuo S, Yang CT, Wu JS, Ou HT. Effects on clinical outcomes of intensifying triple oral antidiabetic drug (OAD) therapy by initiating insulin versus enhancing OAD therapy in patients with type 2 diabetes: a nationwide population-based, propensity-score-matched cohort study. Diabetes Obes Metab. 2019;21(2):312–320. doi: 10.1111/dom.13525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chang CH, Lee YC, Tsai CT, Chang SN, Chung YH, Lin MS, Lin JW, Lai MS. Continuation of statin therapy and a decreased risk of atrial fibrillation/flutter in patients with and without chronic kidney disease. Atherosclerosis. 2014;232(1):224–230. doi: 10.1016/j.atherosclerosis.2013.11.036. [DOI] [PubMed] [Google Scholar]
- 88.Lin YS, Chen TH, Chi CC, Lin MS, Tung TH, Liu CH, Chen YL, Chen MC. Different implications of heart failure, ischemic stroke, and mortality between nonvalvular atrial fibrillation and atrial flutter-a view from a national cohort study. J Am Heart Assoc. 2017;6(7):e006406. doi: 10.1161/JAHA.117.006406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wu CS, Lai MS, Gau SS, Wang SC, Tsai HJ. Concordance between patient self-reports and claims data on clinical diagnoses, medication use, and health system utilization in Taiwan. PLoS One. 2014;9(12):e112257. doi: 10.1371/journal.pone.0112257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sung SF, Hsieh CY, Lin HJ, Chen YW, Yang YH, Li CY. Validation of algorithms to identify stroke risk factors in patients with acute ischemic stroke, transient ischemic attack, or intracerebral hemorrhage in an administrative claims database. Int J Cardiol. 2016;215:277–282. doi: 10.1016/j.ijcard.2016.04.069. [DOI] [PubMed] [Google Scholar]
- 91.Li SY, Chen HH, Lin CL, Yeh SY, Kao CH. The different cardiovascular outcomes between long-term efficacy of hydrophilic and lipophilic statin therapy in both Asian diabetic sexes. Dose Response. 2019;17(3):1559325819876766. doi: 10.1177/1559325819876766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Mureddu GF, Greco C, Rosato S, D’Errigo P, De Luca L, Badoni G, et al. High thrombotic risk increases adverse clinical events up to 5 years after acute myocardial infarction. A nationwide retrospective cohort study. Monaldi Arch Chest Dis. 2019;89(3). 10.4081/monaldi.2019.1166. [DOI] [PubMed]
- 93.Lin Y-F, Chen L, Lin S-L, Yeh Y-C, Huang T-M, Chou Y-H, Chang F-C, Chen Y-T, Yang S-Y, Lai T-S, et al. Potential target-organ protection of mineralocorticoid receptor antagonist in acute kidney disease. J Hypertens. 2019;37(1):125–134. doi: 10.1097/HJH.0000000000001876. [DOI] [PubMed] [Google Scholar]
- 94.Bourrier M, Ferguson TW, Embil JM, Rigatto C, Komenda P, Tangri N. Peripheral artery disease: its adverse consequences with and without CKD. Am J Kidney Dis. 2020;75(5):705–712. doi: 10.1053/j.ajkd.2019.08.028. [DOI] [PubMed] [Google Scholar]
- 95.Lin CP, Tung YC, Hsiao FC, Yang CH, Kao YW, Lin YS, et al. Fixed-dose combination of amlodipine and atorvastatin improves clinical outcomes in patients with concomitant hypertension and dyslipidemia. J Clin Hypertens (Greenwich). 2020;22:1846-53. [DOI] [PMC free article] [PubMed]
- 96.Madsen CM, Kamstrup PR, Langsted A, Varbo A, Nordestgaard BG. Lipoprotein(a)-lowering by 50 mg/dL (105 nmol/L) may be needed to reduce cardiovascular disease 20% in secondary prevention: a population-based study. Arterioscler Thromb Vasc Biol. 2020;40(1):255–266. doi: 10.1161/ATVBAHA.119.312951. [DOI] [PubMed] [Google Scholar]
- 97.Petersen I, Nicolaisen SK, Ricciardi F, Sharma M, Thomsen RW, Baio G, Pedersen L. Impact of being eligible for type 2 diabetes treatment on all-cause mortality and cardiovascular events: regression discontinuity design study. Clin Epidemiol. 2020;12:569–577. doi: 10.2147/CLEP.S251704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Seong JM, Shin D, Sung JW, Cho S, Yang J, Kang S, Moon HW, Lee KW, Ha US. Gonadotropin-releasing hormone agonists, anti-androgens and the risk of cardio-cerebrovascular disease in prostate cancer patients: an asian population-based observational study. J Cancer. 2020;11(14):4015–4022. doi: 10.7150/jca.38237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Freemantle N, Calvert M, Wood J, Eastaugh J, Griffin C. Composite outcomes in randomized trials: greater precision but with greater uncertainty? JAMA. 2003;289(19):2554–2559. doi: 10.1001/jama.289.19.2554. [DOI] [PubMed] [Google Scholar]
- 100.Kip KE, Hollabaugh K, Marroquin OC, Williams DO. The problem with composite end points in cardiovascular studies: the story of major adverse cardiac events and percutaneous coronary intervention. J Am Coll Cardiol. 2008;51(7):701–707. doi: 10.1016/j.jacc.2007.10.034. [DOI] [PubMed] [Google Scholar]
- 101.Kerr AJ, Wang TKM, Jiang Y, Grey C, Wells S, Poppe KK. The importance of considering both primary and secondary diagnostic codes when using administrative health data to study acute coronary syndrome epidemiology (ANZACS-QI 47). Eur Heart J Qual Care Clin Outcomes. 2020;7:548-55. [DOI] [PubMed]
- 102.Peng M, Eastwood C, Boxill A, Jolley RJ, Rutherford L, Carlson K, Dean S, Quan H. Coding reliability and agreement of international classification of disease, 10(th) revision (ICD-10) codes in emergency department data. Int J Popul Data Sci. 2018;3(1):445. doi: 10.23889/ijpds.v3i1.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chang TE, Lichtman JH, Goldstein LB, George MG. Accuracy of ICD-9-CM codes by hospital characteristics and stroke severity: Paul Coverdell National Acute Stroke Program. J Am Heart Assoc. 2016;5(6):e003056. doi: 10.1161/JAHA.115.003056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Bush M, Sturmer T, Stearns SC, Simpson RJ, Jr, Brookhart MA, Rosamond W, Kucharska-Newton AM. Position matters: validation of medicare hospital claims for myocardial infarction against medical record review in the atherosclerosis risk in communities study. Pharmacoepidemiol Drug Saf. 2018;27(10):1085–1091. doi: 10.1002/pds.4396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cutrona SL, Toh S, Iyer A, Foy S, Daniel GW, Nair VP, Ng D, Butler MG, Boudreau D, Forrow S, et al. Validation of acute myocardial infarction in the Food and Drug Administration’s Mini-sentinel program. Pharmacoepidemiol Drug Saf. 2013;22(1):40–54. doi: 10.1002/pds.3310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ando T, Ooba N, Mochizuki M, Koide D, Kimura K, Lee SL, Setoguchi S, Kubota K. Positive predictive value of ICD-10 codes for acute myocardial infarction in Japan: a validation study at a single center. BMC Health Serv Res. 2018;18(1):895. doi: 10.1186/s12913-018-3727-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary Text 1. Systematic Review Protocol.
Additional file 2: Supplementary Table 1. PRISMA 2020 Checklist.
Additional file 3: Supplementary Text 2. Search terms.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.