Abstract
Introduction
Clinical practice guidelines can help physicians provide evidence-based, standardized clinical decisions. We aimed to assess physician attitudes toward and barriers to guideline adherence.
Methods
We conducted a single center, cross-sectional, survey-based study. Physicians from many specialties participated in the study. All outcomes were measured using a validated survey tool. The primary outcome of interest was barriers to guideline adherence. Secondary outcomes included general attitudes toward guidelines and factors that could improve adherence to guidelines. Outcomes were measured by the survey tool. All outcomes were reported on a 5-point Likert scale.
Results
The email survey was received by 1819 physicians with 400 responders (22% response rate). About 50% (n=200) were in practice for >5 years, while 27% (n=107) were still in training. Trainees were less likely to understand the process of guideline development (RR= 0.76 [0.65–0.88], p=0.0017), to have input in guideline development (RR= 0.52 [0.41–0.65], p<0.0001), and to report up-to-date knowledge in practice guidelines (RR=0.53 [0.30–0.73], p=0.0002). Three factors were identified as major barriers to guideline adherence: complexity of guideline documents (61%, n=240), high number of weak or conditional recommendations (62%, n=245), and time constraints due to clinical responsibilities (65%, n=255). Factors that would improve guideline adherence included access to relevant guidelines at the point of care (87%), improved focus on guidelines during training (82%), and transparency on physician commercial affiliation (62%).
Conclusion
Improved focus on guidelines during training and access to relevant guidelines at the point of care may be important to improve adherence to guidelines.
Keywords: clinical practice guidelines, barriers, implementation
Background
Clinical practice guidelines, hereon referred to as guidelines, are produced by many professional societies. Guidelines serve many aims, including: guiding decisions based on best evidence, standardizing patient care, improving provider performance, setting standards of practice, and reducing variability in practice.1 Several studies have shown improvement in disease outcomes with appropriate guideline application, including increased survival,2,3 lower mortality,4–7 improved quality of care,8–10 and improved cost-effectiveness.11 Therefore, guidelines have seen a tremendous increase in recent years with hundreds of guidelines produced annually in the US.12 Despite their prevalence, adherence to national guidelines continues to be suboptimal.13 In recent years, there has been a push to make guidelines more evidence-based.1 Such an approach has been advocated by the Institute of Medicine and adopted by many professional societies. This approach requires guidelines to be based on systematic reviews and meta-analyses.14 The result has been an additional layer of complexity in written guidelines which some may find too cumbersome to follow.15,16 In addition, many societies may produce conflicting guidelines. This adds another layer of complexity and may be another important barrier to guideline adherence. Overall, we have little understanding of how physicians interact with practice guidelines. We aimed to conduct a cross-sectional study to assess physicians’ attitudes of guidelines, potential barriers to guideline implementation, and factors that may increase physician adherence to guidelines.
Methods
Survey Development & Validation
The survey tool was developed by a team of gastroenterologists with expertise in guideline development and survey methodology. The first section of the survey asked about basic physician demographics including specialty, type of practice, and years in practice. The second section asked physicians about attitudes toward practice guidelines and perceived barriers to implementation of the guidelines in their daily practice. Validation of the tool included establishing face, content and constructs validity. First, we offered the tool to three expert physicians and asked for feedback on what items to include or exclude from the survey, content, and wording of the questions. Then, a group of 33 physicians were asked to participate. After answering the questions in the survey, they were asked to fill out the debriefing questionnaire commenting on the survey content, appropriateness and ease of questions, and to make suggestions to help improve the survey.
Final Survey Tool
The 9-question validated survey tool was distributed to physicians in various specialties at a tertiary academic hospital. The survey asked basic physician demographics (years in practice, specialty, type of practice), several opinion-based questions regarding their attitude to guideline implementation, and perceived barriers to guideline application in their practice. Answers were based on a 5-point Likert scale (Appendix 1).
Population & Survey Distribution
We conducted an institution-wide, cross-sectional study. All physicians at the University of Florida Gainesville (UF) campus were eligible to participate in this survey, including physicians in training (residents and fellows). The validated survey was emailed via REDCap (Research Electronic Data Capture)17 to all physicians. The email contained a link to the survey. The link is individualized to the email address to prevent response duplication. First email went out on August 26, 2020. Weekly reminders were sent out for 4 weeks and data collection stopped on October 30, 2020.
Outcomes, Predictors & Confounders
The primary outcomes of interest were barriers to guideline adherence. We investigated a total of eleven potential barriers. These predictors were based on our literature review and our experience in guideline development. Complexity of guideline documents, high incidence of weak or conditional recommendations, and conflicting recommendations were of special interest. Secondary outcomes included general attitudes toward guidelines and factors that could improve adherence to guidelines. Trainees were defined at physicians in residency or fellowship in any specialty. The study was approved by the IRB at the University of Florida. Participants were informed that clicking on the survey link will serve as informed consent.
Statistical Analysis
All outcomes were reported on a 5-point Likert scale. Statistical analysis was performed on SAS 9.4 (Cary, NC). We chose 60% as a threshold to infer strong association between physician responses and category of interest. This was defined a priori and meant that if ≥ 60% of physicians chose agree or strongly agree, strong association was inferred.
A priori analyses were planned to assess the differences in responses between trainee vs non-trainee physicians and internal medicine vs non-internal medicine specialties. We reported proportions in each category. When comparing two groups, we reported relative risk (RR), and 95% confidence intervals (CI). P-value <0.05 was used for statistical significance. The study was approved by the IRB at the University of Florida, Gainesville.
Results
Survey Validation
Between October and November of 2019, 33 physicians were asked to participate. Of those, 91% (n=30) agreed to participate in the paper-based validation process. Of 30 physicians, 40% (n=12) have been in practice over 10 years. Specialties surveyed included internal medicine (43%), gastroenterology (33%), and others. Based on the debriefing questionnaire, only one participant reported that one question was difficult. This question was modified. Another 24% (n=8) of physicians had comments about additional barriers to guideline use, including concerns that guidelines do not apply to a single patient, patient refusal to comply with guidelines, physician apathy to abide by guidelines, lack of insurance coverage to certain guidelines, transparency about physician commercial affiliation, and lack of consideration of cost regarding some clinical interventions. These items were included in the final version of the survey tool (Appendix 1).
Survey Results
The survey was sent out via email to 2272 physicians at UF. We received error messages on 453 email accounts indicating an invalid email. These could have been physicians who left UF, trainees who graduated, or invalid email addresses. Therefore, 1819 physicians received the survey. Of these, 400 responded by filling out the survey. Therefore, the response rate was 22%. Basic demographics for responding physicians are listed in Table 1. Of all participants, 92% (n=366) were in academic positions, the remaining were hospital employees or part of a multi-specialty group. About 50% (n=200) were in practice for > 5 years, while 27% (n=107) were still in training. Physicians from many specialties participated in the study, including internal medicine and subspecialties, pediatric subspecialties, surgery subspecialties, among others. Of all physicians, 35% reported being involved in guideline development. Most physicians 77% (n=295) reported adequate training in guidelines application. Similarly, most physicians rated their adherence to guidelines as high or very high 70% (n=278).
Table 1.
Baseline Characteristics of the 400 Physicians Who Participated in the Study
| Specialty | Frequency | Percent |
|---|---|---|
| Internal Medicine and subspecialties | 143 | 36% |
| Pediatrics and subspecialties | 52 | 13% |
| Surgery and subspecialties | 26 | 7% |
| Anesthesia | 32 | 8% |
| Neurology | 20 | 5% |
| Family Medicine | 19 | 5% |
| Orthopedic Surgery | 16 | 4% |
| Emergency Medicine | 14 | 4% |
| Psychiatry | 12 | 3% |
| OB GYN | 12 | 3% |
| Other | 47 | 12% |
| Missing | 7 | 2% |
| Affiliation | ||
| Academic | 366 | 92% |
| Hospital employed | 29 | 7% |
| Multi-specialty group | 4 | 1% |
| Missing | 1 | 0% |
| Years in practice | ||
| 1–3 years | 54 | 14% |
| 3–5 years | 33 | 8% |
| 5–10 years | 43 | 11% |
| >10 years | 157 | 39% |
| Still in Training | 107 | 27% |
| Missing | 6 | 2% |
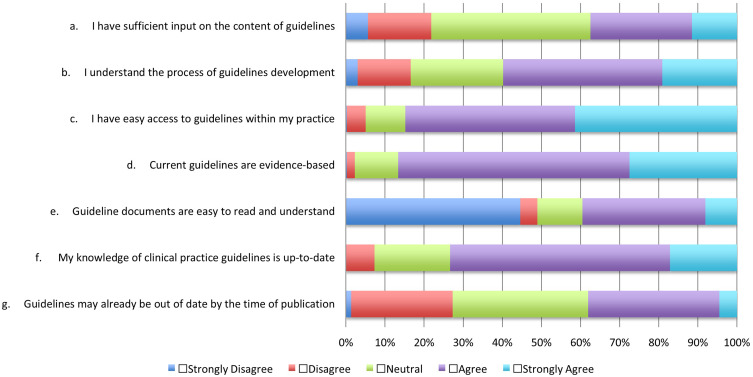
Attitudes Toward Guidelines
Attitudes toward guidelines were assessed in question 6, which included 8 statements.
There were remarkable differences in attitudes toward guidelines from physicians in training compared to post training. Trainees were less likely to understand the process of guideline development (RR= 0.76 [0.65–0.88], p=0.0017), to have input in guideline development (RR= 0.52 [0.41–0.65], p<0.0001), and to report up-to-date knowledge in practice guidelines (RR=0.53 [0.30–0.73], p=0.0002).
Trainee and non-trainee physicians thought that guidelines were evidence-based (73% vs 72%, p=0.902), and that guideline documents were easy to read and access (85% vs 84%, 0.84). A minority of physicians thought that guidelines might be out of date by the time of publication (40% of non-trainee vs 30% of trainee physicians, p=0.10). Overall attitudes toward guidelines among all physicians are summarized in Figure 1.
Figure 1.
Attitudes towards guidelines among surveyed physicians.
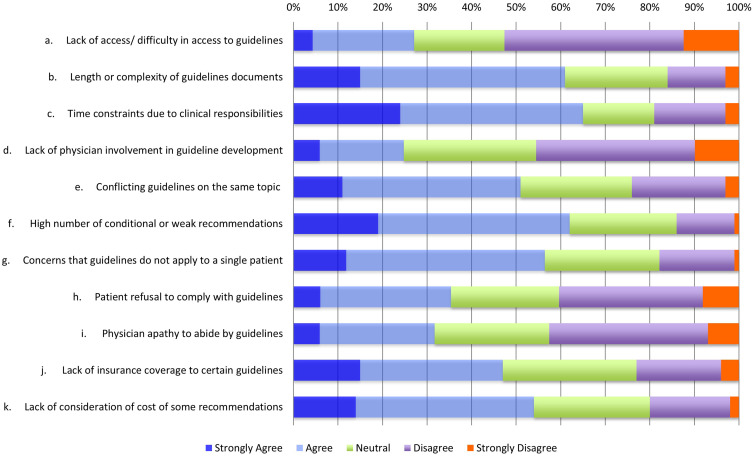
Barriers to Guidelines
We evaluated 11 factors that could be perceived as barriers to using guidelines in clinical practice. We used our a priori identified threshold of 60% to infer strong association. This means that if > 60% of physicians chose agree or strongly agree in response to the question, such factor identified as a significant barrier to guideline use. Based on this criterion, physicians identified three factors as significant barriers to guideline implementation. These factors included: complexity of guideline documents (61%, n=240), high number of weak or conditional recommendations (62%, n=245), and time constraints due to clinical responsibilities (65%, n=255). There were no differences between trainees and non-trainee physicians, and medicine vs non-medicine specialties in identification of these barriers to guidelines. Three additional factors were identified as barriers to guideline implementation using a 50% cutoff. These factors included: conflicting guidelines on the same topic (51%, n=212), perceived lack of cost consideration (54%, n=211), and concern about applicability of guidelines to a single patient (57%, n=224). Details on potential barriers assessed in the survey are summarized in Figure 2.
Figure 2.
Barriers to guideline implementation among surveyed physicians.
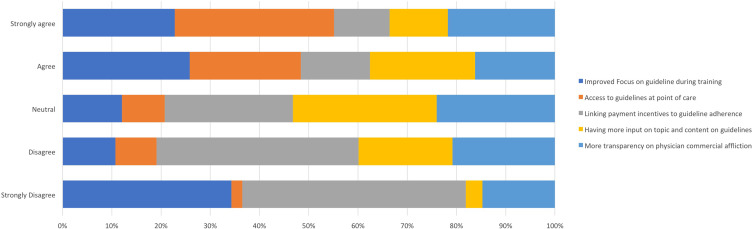
Improving Guideline Compliance
Several factors were identified which can help increase awareness of and adherence to clinical practice guidelines. Of these factors, access to relevant guidelines at the point of care (EMR) was most highly rated with 87% of physicians responding by agree (45%) or strongly agree (42%). Improved focus on guidelines during training was also rated very highly with 82% of physicians responding agree or strongly agree. Lastly, 60% of responders thought that more transparency on physician commercial affiliation can help increase adherence to guidelines. Details on factors that can increase awareness and adherence are summarized in Figure 3.
Figure 3.
Factors that may improve adherence to clinical practice guidelines.
Discussion
We performed a cross-sectional, survey-based study of 400 physicians using a validated physician survey. We aimed to assess attitudes toward clinical practice guidelines. We found that trainees were less likely to understand the process of guideline development and to report up-to-date knowledge in practice guidelines when compared to physicians who have finished their training and were in practice. The most important barriers to guideline adherence were complexity of guideline documents, high number of weak or conditional recommendations, and time constraints due to clinical responsibilities of physicians. Access to relevant guidelines at the point of care and improved focus on guidelines during training were identified as important factors that could improve guideline adherence among all physicians.
Understanding Conditional or Weak Recommendations
Clinical practice guidelines aim to help physicians make informed, evidence-based decisions on the daily management of their patients. The advent of evidence-based guidelines has been a hallmark of new clinical practice guidelines. Despite the obvious benefits of this approach, it appears to have introduced a potential barrier to guideline implementation: conditional or weak recommendations. One of the most frequently used guideline assessment methodologies is the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) system.18 Under this methodology, recommendations can be strong or conditional.19 While a detailed discussion of GRADE is beyond the scope of this study, our survey seems to be the first study to suggest that the large number of conditional recommendations is perceived as a barrier to guideline implementation by a large proportion of surveyed physicians. Based on our experience, there may be some misunderstanding of the term conditional recommendation. The intended meaning of conditional recommendation is that most patients would choose the recommended action, but that a substantial number of patients would not.19 In our experience, many medical decisions addressed in guidelines do not always lead themselves to string recommendations. For example, in a recent guideline, we reviewed the efficacy of metal stents compared to plastic stents in patients with cholangiocarcinoma. In order to make a strong recommendation, we would need to find strong evidence that metal stents are superior to plastic stents in most cases. Furthermore, we would have to show superior cost-effectiveness and patient acceptability. Clearly, reaching a strong recommendation in this case requires a high threshold, which was not reached, thus a conditional recommendation was made. Such scenarios seem common in medical literature where one intervention, test, or procedure, may be slightly better than another. Thus, a conditional recommendation is most appropriate. Dealing with this potential barrier will require a significant effort from guideline panels and societies. For instance, physicians need to be better informed about the meaning of conditional recommendations. Similarly, guideline panels should also keep this in mind and consider wording that can further explain the intended recommendations.
Complexity of Guidelines
The move toward evidence-based guidelines may have introduced another important barrier to guidelines: complexity of guideline documents.15 As guidelines have become more evidence-based, the length and complexity of guidelines has also increased.16 The process of guideline development now involves extensive systematic reviews, meta-analyses, evidence profiles, forest plots, and funnel plots.20,21 Panel compositions have also become more elaborate to include many stakeholders. Panels have to consider and report on many factors like cost-effectiveness, patients’ values, feasibility, and acceptability in addition to the quality and certainty of evidence. These factors have clearly improved the quality of guidelines. However, these same factors made guidelines more complex and lengthy. This complexity was identified as a major barrier to guideline use by our physician survey. While the process of producing evidence-based guidelines needs to be rigorous, the final product of the guideline should be user-friendly and easy to understand and interpret. With clarity and ease of use in mind, many societies now produce a summary document of the guideline.22 This summary contains the essential data needed by clinicians. The more technical part of the guideline can be showcased in a separate document. Other strategies may be to use figures, tables, social media posts, and video summaries to emphasize the essential parts of guidelines. The effectiveness of such strategies in improving guideline adherence are not clear but should be considered for future studies.
Importance of Guidelines for Training Programs
Despite the increase in number of guidelines in medical fields, adherence to guidelines is not well established. Our study showed that physicians in training had different attitudes towards guidelines compared to physicians in practice. Earlier studies indicated low level of adherence to guidelines among US-based Internal Medicine (IM) residents.23 One of the main factors for this may be that programs do not offer curricula which aims at teaching residents on how to use guidelines. For example, a survey of 434 IM and family practice programs found that only 14% reported providing written goals aimed at teaching guidelines to trainees.24 Hence, our results add to the existing body of evidence that training programs need to improve education of residents and fellows to include clear emphasis on guidelines. There are many ways this can be done: dedicating a larger proportion of journal clubs to reviewing new guidelines; making a list of must-read guidelines to be covered annually during training; and referencing guidelines during daily rounds. In support of this concept, our study showed that improved focus on guidelines during training would help improve adherence to guidelines. Lastly, professional societies, and guideline panels, may benefit from engaging residents and fellows and from developing guidelines specifically targeting trainees to increase guideline adoption.
Other Barriers
In addition, many physicians reported that “more transparency on physician commercial affiliation” would improve guideline adherence. Many physicians who lead guideline development receive financial support from industry. Such affiliation may create a conflict of interest (COI) which might affect how guideline recommendations are made. More transparency would allow physicians who use these guidelines to be more confident in the lack of COI.
Finally, many clinicians reported that time constraints are an important barrier to use of practice guidelines. One of the strategies that can help overcome this obstacle is the availability of and easy access to guidelines at the point of care. For example, electronic health systems could be linked to guidelines related to certain CPT codes. For example, if the physician enters a CPT code for Barrett’s esophagus, the system could provide a link to the most recent guidelines dealing with this topic. This concept seems appealing to physicians and should be further evaluated in actual clinical practice.
Strengths and Limitations
Our study has several strengths. We approached all physicians in a large tertiary care center. The study included a large variety of medical specialties, and the number of physicians included is large. On the other hand, there are several limitations to our study. One of the main limitations of our study, which is inherent to most survey studies, is the low response rate of 22%. In fact, several studies have shown that response rates have been declining in survey studies within the healthcare fields.25 Physicians receive many surveys on a daily bases making response rate low. We have no reason to suspect that non-responders had different views than responders. Therefore, the low response rate is unlikely to have changed our final results or conclusions. Another limitation is that most physicians worked at a single academic center, limiting generalizability of our findings. However, some of our findings are consistent with previous research studies. This suggests that barriers identified by our survey are likely reflective of a larger population of US physicians.
Finally, our study did not address how guideline use can affect health equity and the barriers to guideline implantation in underserved or underrepresented populations. In GRADE methodology, guideline developers are encouraged to consider how making a certain recommendation will affect equity in healthcare delivery. Future studies should assess how adherence to guidelines can be used to address health equity.
Conclusions
In conclusion, we identified several barriers to guideline implementation. These included complexity of guidelines, high number of conditional recommendations, and time constraints due to clinical responsibilities. Physicians in training reported lower understanding and involvement in guidelines. Improved focus on guidelines during training and easy access to relevant guidelines at the point of care may be important to improve adherence to guidelines.
Acknowledgments
We would like to acknowledge Dr. Chelsea Jacobs for her help in survey validation.
Disclosure
Dr. Draganov is a consultant for Olympus, Boston Scientific, Cook Medical, Lumendi and Microtech. The authors declare that they have no other conflicts of interest in this work.
References
- 1.Institute of Medicine Committee on Standards for Developing Trustworthy Clinical Practice G. Clinical practice guidelines we can trust. In: Graham R, Mancher M, Miller Wolman D, Greenfield S, Steinberg E, editors. Copyright 2011 by the National Academy of Sciences. All Rights Reserved. Washington (DC): National Academies Press (US); 2011. [PubMed] [Google Scholar]
- 2.Carrasco-Pena F, Bayo-Lozano E, Rodriguez-Barranco M, et al. Adherence to clinical practice guidelines and colorectal cancer survival: a retrospective high-resolution population-based study in Spain. Int J Environ Res Public Health. 2020;17:6697. doi: 10.3390/ijerph17186697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Derbel O, Cropet C, Meeus P, et al. Adhesion to clinical practices guidelines (CPG’S) and role on survival for soft tissue sarcoma patients. analysis of a population based cohort from Rhone-Alpes region. Ann Oncol. 2012;23:478. doi: 10.1093/annonc/mds414 [DOI] [Google Scholar]
- 4.Dean NC, Silver MP, Bateman KA, et al. Decreased mortality after implementation of a treatment guideline for community-acquired pneumonia. Am J Med. 2001;110:451–457. doi: 10.1016/S0002-9343(00)00744-0 [DOI] [PubMed] [Google Scholar]
- 5.VanWagner LB, Holl JL, Montag S, et al. Blood pressure control according to clinical practice guidelines is associated with decreased mortality and cardiovascular events among liver transplant recipients. Am J Transplant. 2020;20:797–807. doi: 10.1111/ajt.15706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hassan J, Temsah MH, Abdo A, et al. Implementation of septic shock clinical practice guidelines decreases mortality and shortens length of stay in Saudi pediatric intensive care setting. Intensive Care Med. 2011;37:S351–S351. [Google Scholar]
- 7.Gitt AK, Zeymer U, Towae F, et al. Better adherence to guidelines improved hospital mortality of STEMI in clinical practice between from 1994 and 2008: results of MITRAplus and OPTAMI. Eur Heart J. 2010;31:937–938. [Google Scholar]
- 8.Saint S, Scholes D, Fihn SD, et al. The effectiveness of a clinical practice guideline for the management of presumed uncomplicated urinary tract infection in women. Am J Med. 1999;106:636–641. doi: 10.1016/S0002-9343(99)00122-9 [DOI] [PubMed] [Google Scholar]
- 9.Brown E, Bergmann S, Jackson S, et al. Clinical practice guideline improves quality of care and emergency room discharge in uncomplicated vaso-occlusive crisis. Pediatr Blood Cancer. 2011;56:940–941. [Google Scholar]
- 10.Portela MC, Lima SML, Ferreira VMB, et al. Clinical guidelines and other practices for improving quality of care by health plans from the perspective of their operators in Brazil. Cad Saude Publica. 2008;24:253–266. doi: 10.1590/S0102-311X2008000200004 [DOI] [PubMed] [Google Scholar]
- 11.Nathwani D, Rubinstein E, Barlow G, et al. Do guidelines for community-acquired pneumonia improve the cost-effectiveness of hospital care? Clin Infect Dis. 2001;32:728–741. doi: 10.1086/319216 [DOI] [PubMed] [Google Scholar]
- 12.Upshur RE. Do clinical guidelines still make sense? No. Ann Fam Med. 2014;12:202–203. doi: 10.1370/afm.1654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–1465. doi: 10.1001/jama.282.15.1458 [DOI] [PubMed] [Google Scholar]
- 14.Wani S, Sultan S, Qumseya B, et al. The ASGE’S vision for developing clinical practice guidelines: the path forward. Gastrointest Endosc. 2018;87:932–933. doi: 10.1016/j.gie.2017.10.012 [DOI] [PubMed] [Google Scholar]
- 15.Francke AL, Smit MC, de Veer AJ, et al. Factors influencing the implementation of clinical guidelines for health care professionals: a systematic meta-review. BMC Med Inform Decis Mak. 2008;8:38. doi: 10.1186/1472-6947-8-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kann BH, Johnson SB, Aerts HJ, et al. Changes in length and complexity of clinical practice guidelines in oncology, 1996–2019. JAMA Netw Open. 2020;3:e200841–e200841. doi: 10.1001/jamanetworkopen.2020.0841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026 [DOI] [PubMed] [Google Scholar]
- 19.Andrews J, Guyatt G, Oxman AD, et al. GRADE guidelines: 14. Going from evidence to recommendations: the significance and presentation of recommendations. J Clin Epidemiol. 2013;66:719–725. doi: 10.1016/j.jclinepi.2012.03.013 [DOI] [PubMed] [Google Scholar]
- 20.Mazzone PJ, Silvestri GA, Patel S, et al. Screening for lung cancer: CHEST guideline and expert panel report. CHEST. 2018;153:954–985. doi: 10.1016/j.chest.2018.01.016 [DOI] [PubMed] [Google Scholar]
- 21.Qumseya B, Sultan S, Bain P, et al. ASGE guideline on screening and surveillance of Barrett’s esophagus. Gastrointest Endosc. 2019;90:335–359.e2. doi: 10.1016/j.gie.2019.05.012 [DOI] [PubMed] [Google Scholar]
- 22.Ko CW, Siddique SM, Patel A, et al. AGA clinical practice guidelines on the gastrointestinal evaluation of iron deficiency anemia. Gastroenterology. 2020;159:1085–1094. doi: 10.1053/j.gastro.2020.06.046 [DOI] [PubMed] [Google Scholar]
- 23.Barrison AF, Smith C, Oviedo J, et al. Colorectal cancer screening and familial risk: a survey of internal medicine residents’ knowledge and practice patterns. Am J Gastroenterol. 2003;98:1410–1416. doi: 10.1111/j.1572-0241.2003.07481.x [DOI] [PubMed] [Google Scholar]
- 24.Akl EA, Mustafa R, Wilson MC, et al. Curricula for teaching the content of clinical practice guidelines to family medicine and internal medicine residents in the US: a survey study. Implement Sci. 2009;4:59. doi: 10.1186/1748-5908-4-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cunningham CT, Quan H, Hemmelgarn B, et al. Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol. 2015;15:32. doi: 10.1186/s12874-015-0016-z [DOI] [PMC free article] [PubMed] [Google Scholar]