Abstract
Foot pain is common in daily clinical practice but thrombosis of the foot veins is rarely considered as a differential diagnosis. Several cases of plantar veins thrombosis are reported in literature but a detailed description of ultrasonographic findings in case of thrombosis of the dorsal venous arch of the foot is lacking. We report a case of ours with a thrombosis of the medial marginal vein and dorsal venous arch of the foot, showing its close anatomical relation with the extensor hallucis longus tendon.
Keywords: Foot, Veins, Medial marginal vein, Dorsal venous arch, Thrombosis, Ultrasound
Introduction
Foot pain is common in clinical practice, but thrombosis of the foot veins is rarely considered as a differential diagnosis; moreover, in the pertinent literature, cases on plantar vein thrombosis are well described [1, 2], while data regarding thrombosis of the medial marginal vein (MMV) and/or dorsal venous arch (DVA) are lacking. Known risk factors of foot vein thrombosis include recent surgery, paraneoplastic conditions, anticardiolipin antibody syndrome and local trauma or mechanical injuries [1, 2]. Thrombosis of the foot veins related to mechanical causes is more frequent at the level of the plantar veins, considering possible strain to the sole of the foot [1]. We report a case with a clinical scenario of nodularity on the dorsal foot and sonographic findings of superficial vein thrombosis mainly ascribed to local compression.
Case report
A 45-year-old man presented to our clinic for a mass located on the dorsal medial side of his right foot. The local swelling had increased progressively during the last 2 months after the positioning of a foot orthosis that was prescribed for a hallux valgus. He denied any major trauma and declared that local anti-inflammatory drugs and ice packs had been somewhat effective. A physical examination revealed a 2-cm superficial oval mass on the dorsal side of the right foot that extended obliquely from medial to lateral in the region of the cuneo-metatarsal joint. It was mildly painful to palpation and resisted dorsal flexion of the hallux. The patient denied any other pathology except for the hallux valgus. Based on the history and clinical findings, the patient was suspected to have a ganglion cyst, probably originating from a joint of midfoot that became painful due to excessive external compression by the orthosis. Before prescribing a tailored therapy, an ultrasound (US) examination was carried out to correctly evaluate the local nodularity [3].
The US examination was performed with a Toshiba Aplio 500 and an 18–7 MHz multi-frequency transducer. The exam targeted the area of the palpable mass at the dorsal medial aspect of the midfoot.
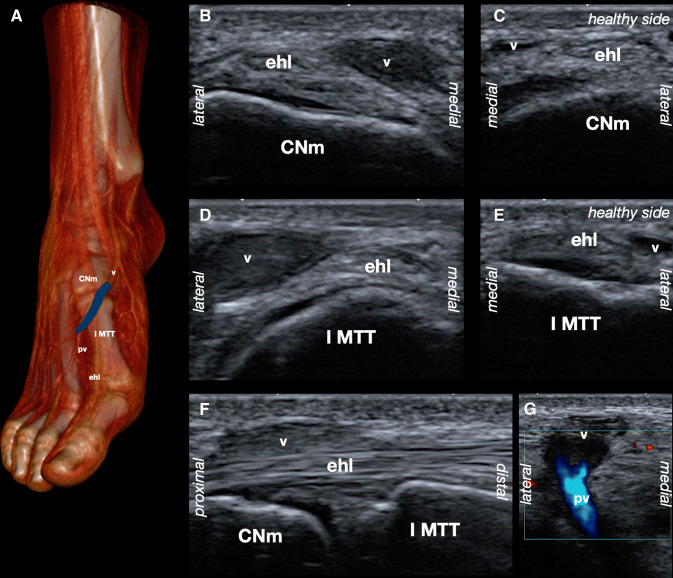
Grayscale and Color Doppler sonograms depicted a hypoechoic, non-compressible oval mass crossing the extensor hallucis longus (EHL) tendon in proximity to the Lisfranc joint, between the first metatarsal and the medial cuneiform bone, with no internal flow, as shown by the Color Doppler (Fig. 1). The mass was proximally in continuity with the MMV of the foot and distally with the DVA. A regular flow of the perforator (communicating) vein of first intermetatarsal space, which connects the DVA with the medial end of the deep plantar venous arch, was demonstrated by Color Doppler.
Fig. 1.
A schematic drawing of the right foot a shows the anatomical location of the medial branch (v) of the superficial dorsal venous arch of the foot (blue) at the level of the medial cuneiform bone (CNm) and the first metatarsal bone (I MTT). Ultrasound images in a short axis view from proximal b to distal d show the thrombosed vein (v) passing from the medial to the lateral side of the extensor hallucis longus (ehl) tendon; on the contralateral healthy side, a compressible superficial vein is visible (c, e). The ultrasound image in a long axis view (f) demonstrates the cross between the thrombosed vein (v) superficially and the extensor hallucis longus (ehl) tendon more deeply; the joint between CNm and I MTT is visible just below the tendon plane. A short axis view of the first intermetatarsal space g shows the confluence of the first intermetatarsal space perforator vein (pv), with Color Doppler signal, to the medial branch (v) of the superficial dorsal venous arch without Color Doppler signal
Based on the clinical and sonographic findings, the proposed diagnosis was superficial thrombosis of the MMV extending to the DVA of the foot due to mechanical compression of the vessel between the EHL tendon and the foot orthosis.
The patient was referred to a vascular surgeon, who suggested the use of compression stockings, comfortable shoes and removal of the foot orthosis. The patient was contacted by phone after 3 months and indicated a positive outcome.
Discussion
US imaging with a high-frequency transducer allows the physician to promptly evaluate the superficial structures of the foot, such as tendons, ligaments, vessels, nerves, capsulo-synovial tissues and cortical bones [3]. A painful mass located on the dorsal aspect of the foot can be related to several causes [4, 5].
In our case, the anatomical location of the nodularity on the medial side of the dorsal foot implied a problem of differential diagnosis between:
tendinopathy and/or tenosynovitis of the EHL tendon [6];
a foreign body causing a granulomatous reaction [7];
a synovial or ganglion cyst originating from the Lisfranc joint [4, 8];
osteoarthritis of the Lisfranc joint [4];
periostitis or stress fracture of the first metatarsal bone [4, 8];
adventitious bursitis related to mechanical stress [8];
metabolic disorders like tophaceous gout [8];
pathology of the dorsomedial cutaneous nerve of the hallux, which also crosses the EHL tendon [9];
pathology of the superficial venous network [10].
The vascular anatomy of the venous system of the foot is quite complicated. The MMV and the lateral marginal vein (LMV) are superficial dorsal vessels located on each side of the foot, connected anteriorly by the DVA. The MMV extends proximally in the great saphenous vein, while the LMV extends in the small saphenous vein. Several plexuses and anastomoses exist to optimize the function of the “venous foot pump”; the plantar veins communicate with the dorsal veins through communicating and perforating branches [10].
In particular, the perforating vein of the first interosseous space connects the DVA with the medial end of the deep plantar venous arch. In our case, it was important to exclude thrombosis of the perforating branch and, therefore, of the deep vessels of the foot; so a conservative approach was proposed, because anticoagulant treatment is believed to be reasonable in the management of plantar vein thrombosis [1].
Our search of the literature revealed only one report of dorsal arch thrombophlebitis in a patient 4 days before undergoing foam sclerotherapy [11] and one report of a partially thrombosed aneurysm of the medial marginal vein [12].
This is, to the best of our knowledge, the first report of a thrombosed MMV at the level of the crossing with the EHL, extending to the DVA, in a patient with an orthosis suggested for treating hallux valgus. Sonologists should be aware that a mass crossing the EHL in patients with chronic compression, i.e., related to the use of an orthosis as in the present case report, may be related to superficial vein thrombosis. Moreover, in patients with local swelling on the dorsal aspect of the foot, not only musculoskeletal disorders, but also vascular pathologies should be considered in the differential diagnosis, especially in the presence of predisposing conditions.
Funding
No funding was received.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Czihal M, Röling J, Rademacher A, et al. Clinical characteristics and course of plantar vein thrombosis: a series of 22 cases. Phlebology. 2015;30:714–718. doi: 10.1177/0268355514555385. [DOI] [PubMed] [Google Scholar]
- 2.Siegal DS, Wu JS, Brennan DD, et al. Plantar vein thrombosis: a rare cause of plantar foot pain. Skelet Radiol. 2008;37:267–269. doi: 10.1007/s00256-007-0419-y. [DOI] [PubMed] [Google Scholar]
- 3.Özçakar L, Kara M, Chang KV, et al. EURO-MUSCULUS/USPRM. Basic scanning protocols for ankle and foot. Eur J Phys Rehabil Med. 2015;51:647–653. [PubMed] [Google Scholar]
- 4.Bianchi S, Martinoli C. Foot. Ultrasound of the musculoskeletal system. Berlin: Springer; 2007. pp. 835–888. [Google Scholar]
- 5.Catalano O, Varelli C, Sbordone C, et al. (2019) A bump: what to do next? Ultrasound imaging of superficial soft-tissue palpable lesions. J Ultrasound. 2019 doi: 10.1007/s40477-019-00415-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ng JM, Rosenberg ZS, Bencardino JT, Restrepo-Velez Z, Ciavarra GA, Adler RS. US and MR imaging of the extensor compartment of the ankle. Radiographics. 2013;33(7):2047–2064. doi: 10.1148/rg.337125182. [DOI] [PubMed] [Google Scholar]
- 7.Becciolini M, Bonacchi G, Becciolini A. Sonographic findings in a case of cactus thorn arthritis. J Clin Ultrasound. 2017;45:240–241. doi: 10.1002/jcu.22455. [DOI] [PubMed] [Google Scholar]
- 8.Van Hul E, Vanhoenacker F, Van Dyck P, De Schepper A, Parizel PM. Pseudotumoural soft tissue lesions of the foot and ankle: a pictorial review. Insights into Imaging. 2011;2(4):439–452. doi: 10.1007/s13244-011-0087-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zdilla MJ, Miller KD, Swearingen JV, et al. The use of ultrasonography to identify the intersection of the dorsomedial cutaneous nerve of the hallux and the extensor hallucis longus tendon: a cadaveric study. J Foot Ankle Surg. 2018;57:296–300. doi: 10.1053/j.jfas.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uhl JF, Gillot C. Anatomy of the foot venous pump: physiology and influence on chronic venous disease. Phlebology. 2012;27:219–230. doi: 10.1258/phleb.2012.012b01. [DOI] [PubMed] [Google Scholar]
- 11.Shadid N, Frank J, Sommer A. Superficial thrombophlebitis of the venous dorsal arch of the foot and deep venous thrombosis after foam sclerotherapy. Int J Dermatol. 2008;47(SUPPL. 1):29–31. doi: 10.1111/j.1365-4632.2008.03955.x. [DOI] [PubMed] [Google Scholar]
- 12.Khodarahmi I, Alizai H, Adler R. Partially thrombosed aneurysm of the medial marginal vein. J Clin Ultrasound. 2019;47(7):436–438. doi: 10.1002/jcu.22723. [DOI] [PubMed] [Google Scholar]