Abstract
Background
Extended focused abdominal sonography for trauma (e-FAST) is part of the primary survey in patients with high-energy trauma. However, it does not identify patients with retroperitoneal haemorrhage associated with significant pelvic trauma. A traumatic diastasis of pubic symphysis, as well as an ‘open book’ (OB) pelvic injury, is a diagnostic clue to recognize unstable pelvis with higher risk of bleeding. FAST–PLUS (FAST–PL pleural –US ultrasound of symphysis) protocol is an addendum to the e-FAST, which takes into account the study of the pubic symphysis in a single transverse scan after the traditional focused evaluation of the abdomen and thorax.
Objectives
The aim of this study is to determine the value of FAST–PLUS protocol in the evaluation of pubic symphysis injuries and the identification of ‘open book’ (OB) unstable pelvic fractures.
Methods
Between January 2018 and December 2019, we retrospectively reviewed 67 polytraumatised patients with clinical suspicion of pelvic instability and with known anteroposterior pelvis compression injuries who underwent e-FAST with an additional transverse scan of the pubic symphysis, named the FAST–PLUS protocol and computed tomography (CT) exam in order to assess the correlation between them in defining the presence or absence of pubic symphyseal widening (SW). A cutoff value of 2.5 cm in transverse diameter was used to diagnose OB unstable pelvic injury. The results were analysed using Cohen's test, which uses the Kappa value as the reference index.
Results
The analysis carried out to assess the degree of agreement between FAST–PLUS and CT showed 5/67 patients (7.5%) with a critical pubic SW (> 2.5 cm transverse diameter) suggestive of unstable OB pelvic injury and 62/67 (92,5%) without any signs of SW at FAST–PLUS. At CT, findings of unstable OB pelvic fracture were confirmed in all patients with positive results at FAST–PLUS. Similarly, all patients with negative results for critical pubic SW (< 2.5 cm in transverse diameter) at FAST–PLUS were found to be negative at CT exam. The level of correlation between the two methods was high (Kappa value = 1)
Conclusion
The FAST–PLUS protocol shows a high correlation with CT exam, which is the gold standard for the detection of unstable pubic SW, as well as OB pelvic injury, in polytraumatised patients. Inclusion of FAST–PLUS in patient management in the shock room may lead to a quicker identification of patients with unstable pelvis and to faster therapeutic work-up.
Keywords: Trauma imaging, Ultrasound, e-FAST, FAST–PLUS, Pelvic fractures, Symphyseal widening, Open book pelvic fracture
Background and objectives
Pelvic ring fractures occur in 9.3% of patients with blunt trauma [1], although their incidence is increasing due to the high number of motor vehicle accidents, falls from a height, crush injuries and extreme sports [2–4]. These fractures are often associated with damage to the abdominal and pelvic organs, with a reported prevalence ranging from 11 to 20.3% [5]. According to the Young and Burgess classification, the biomechanics of pelvic ring disruption include 3 mechanisms (Table 1): anteroposterior compression, lateral compression and vertical shear [3, 6].
Table 1.
Young and Burgess classification
| Anteroposterior compression | Lateral compression | Vertical shear | Combined |
|---|---|---|---|
| I: Stable pubic diastasis < 2.5 cm | I: Stable oblique fracture of pubic rami ipsilateral anterior compression fracture of the sacral ala | Vertical displacement of hemipelvis, pubic and sacroiliac joint fractures | Complex fracture, including a combination of anteroposterior compression, lateral compression and/or vertical shear |
| II: Rotationally unstable, vertically stable pubic diastasis > 2.5 cm disruption and diastasis of the anterior part of the sacroiliac joint, with intact posterior sacroiliac joint ligaments |
II: Rotationally unstable, vertically stable fracture of pubic rami posterior fracture with dislocation of the ipsilateral iliac wing (crescent fracture) |
||
| III: Equates to a complete hemipelvis separation (but without vertical displacement); unstable pubic diastasis > 2.5 cm disruption-diastasis of both anterior and posterior sacroiliac joint ligaments with dislocation | III: Unstable ipsilateral lateral compression contralateral anteroposterior compression |
Due to the ring constitution of the pelvis, for each injury caused by a high-energy force vector in one area, another bone or ligamentous lesion must correspond on the opposite side [7, 8]. Exceptions include insufficiency fractures, caused by ‘low-energy’ force vectors, as occur in osteoporotic patients, or in avulsion fractures typical of juvenile sport injuries. Mortality in patients affected by pelvic fractures has been reported to be 4–15% [9, 10], and pelvic haemorrhage, multiple organ failure and sepsis are the most common causes of death [2, 3, 9, 10]. The early identification of patients at risk of pelvic haemorrhage who might benefit from operative management may reduce blood loss, prevent late complications and improve outcomes [1].
In unstable patients, pelvic ring evaluation is usually performed during the primary survey, with anteroposterior pelvic X-ray. In stable patients, CT is performed during the secondary survey and allows for a more precise evaluation of pelvic ring stability [11]. Contrast-enhanced ultrasound (CEUS) is limited to cases of low-energy isolated abdominal trauma, particularly in children or in the follow-up of low-grade traumatic lesions, thus avoiding or lowering levels of ionizing radiation [12, 13].
Focused Assessment with Sonography for Trauma (FAST) with extended FAST (e-FAST) is part of the primary survey in polytrauma patients [14–16]. It is a non-invasive, repeatable, safe, non-irradiating, cheap and quick technique that aims to exclude immediate life-threatening conditions such as pericardial tamponade, hemothorax, pneumothorax and hemoperitoneum [17, 18]. However, FAST (or e-FAST) cannot evaluate retroperitoneal haemorrhages, and cannot distinguish between blood and urine in severe unstable pelvic trauma [18, 19]. At the same time, the presence of the pubic symphyseal widening (SW) is a diagnostic clue to recognize unstable ‘open book’ (OB) pelvic fractures with higher risk of retroperitoneal bleeding [19]. FAST–PLUS (FAST—PL pleural—US ultrasound of symphysis) is an addendum to the e-FAST protocol which takes into account the study of the pubic symphysis in a single transverse scan after the traditional focused evaluation of the abdomen and thorax. The aim of this study is to determine the value of the FAST–PLUS protocol in the evaluation of pubic symphysis injuries and more particularly in the identification of unstable OB pelvic fractures.[1, 18, 19].
Materials and methods
Patients selection and study design
Between January 2018 and December 2019, 497 polytraumatised patients were admitted to our emergency department and underwent e-FAST during the primary survey. In 67/497 of them (43 males and 24 females; mean age 47 years; range 40–70 years) with abdominopelvic trauma and with a clinical suspicion of pelvic instability and the known injury mechanism of anteroposterior compression, an additional transverse scan of the pubic symphysis, called the FAST–PLUS protocol, was performed in order to evaluate the presence of symphyseal widening (SW). A cutoff value of 2.5 cm in transverse diameter was used to define the presence or absence of pubic SW suggestive of unstable pelvic OB fractures, according to the Young and Burgess classification [20]. All 67 patients underwent computed tomography (CT) scans after FAST–PLUS. We retrospectively reviewed all 67 patients who underwent FAST–PLUS and CT scans in order to assess the correlation between these exams in detecting critical SW (> 2.5 cm). The results were analysed using Cohen's test, which uses the Kappa value as the reference index. The CT technique was considered the gold-standard reference for the detection of pelvic ring fractures. Patients under 18 years of age and pregnant women were excluded, as they may have atraumatic symphyseal widening. Obese patients (body mass index–BMI > 30 kg/m2) were also excluded from the study, since the morphotype is a well-known limiting factor for US examination in general. Furthermore, patients with certain clinical evidence of pelvic instability and known injury mechanisms of lateral compression or vertical shear compression, or those who did not have FAST–PLUS performed, were excluded from the study.
Image acquisition
The FAST–PLUS exam was first carried out with a low-frequency probe (3.5–5 MHz convex transducer) for better penetration of tissues in the abdominal cavity, to exclude hemoperitoneum, according to the well-known FAST protocol (pericardial view; right and left flank view; pelvic view). It was subsequently performed again with a high-frequency probe (15–4 MHz linear transducer) for the evaluation of both hemithorax (i.e. the pleura) to exclude pneumothorax or hemothorax, according to the extended-FAST version and finally with the same high-resolution linear probe, the pubic symphysis was scanned with a transverse section (Table 2). Both probes are ready to use in the same US machine (MyLab™25, Esaote SpA, IT) without time-consuming adjustments. Measurements of pubic SW were made between the pubic tubercles on the transverse scan (Fig. 1). A pubic SW > 2.5 cm in transverse diameter was considered positive for unstable OB pelvic fracture. CT images were obtained with a multidetector row CT scanner with 64 detector rows (Somatom Sensation, Siemens Medical Systems, Erlangen, Germany) after intravenous contrast media administration to exclude active bleeding.
Table 2.
FAST–PLUS protocol
| FAST–PLUS protocol | ||
|---|---|---|
| FAST protocol | Pericardial view; right and left flank view; pelvic view | To exclude hemoperitoneum |
| e-FAST protocol | Pleural view | To exclude pneumothorax or hemothorax |
| Transverse scan on the pubic symphysis | Pubic symphysis view | To exclude unstable pelvic fractures |
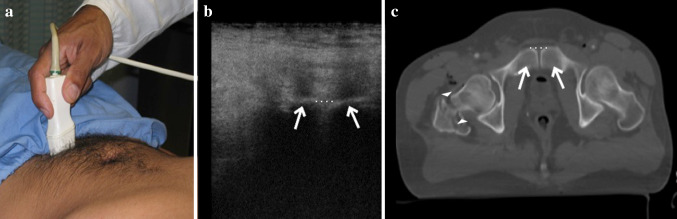
Fig. 1.
a Example of a transverse scan of the pubic symphysis performed with a high-frequency linear probe; b, c anatomical representation of the pubis at US transverse scans (b) and at CT axial scan of the pelvis (c) with evidence of branched (b, c, arrows) and not diastased symphysis (b, c, dotted line) in patient with femoral right neck fracture (c, arrowheads)
Results
The analysis carried out to assess the degree of agreement between FAST–PLUS and CT showed 5/67 patients (7.5%) with a critical pubic SW (> 2.5 cm in transverse diameter) suggestive of unstable OB pelvic fracture and 62/67 (92.5%) without any signs of SW at FAST–PLUS. At CT, findings of unstable OB pelvic fracture were confirmed in all patients with positive results at FAST–PLUS. Similarly, all patients with negative results for critical pubic SW (< 2.5 cm in transverse diameter) at FAST–PLUS were found to be negative at CT exam too (Figs. 2, 3, 4). The level of correlation between the two methods was high (Kappa value = 1).
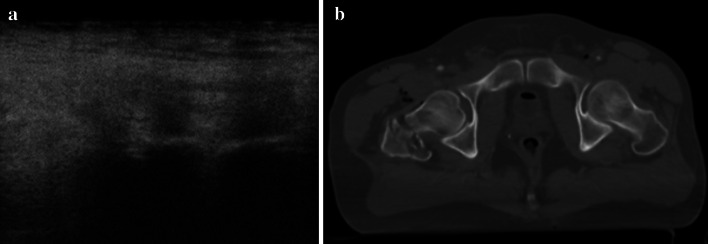
Fig. 2.
a US shows the normal aspect of pubic symphysis and b CT demonstrates the lack of diastasis of the pubic branches
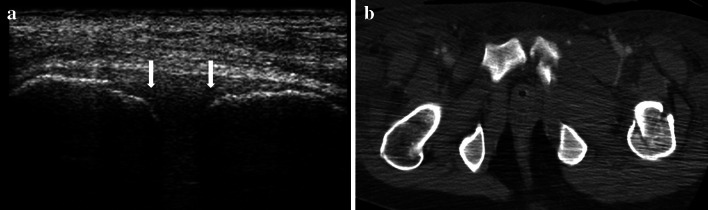
Fig. 3.
a US shows pubic symphysis widening; the distance between the two pubic tubercles (arrows) is < 2.5 cm. b CT confirms the diastasis of the pubic branches, less than 2.5 cm
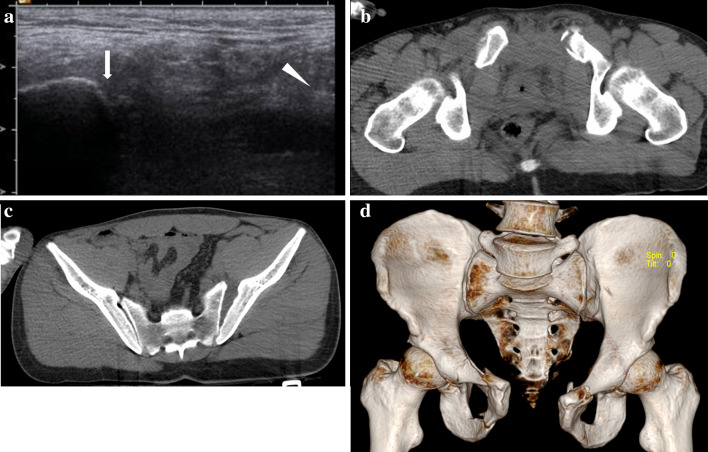
Fig. 4.
a US shows large diastasis of the pubic symphysis, greater than 2.5 cm. The right pubic branch is clearly visible (arrow), while only a detached fragment of the left branch is visible (arrowhead): b, c axial CT scan and d 3D reconstruction confirm the large widening of the pubic symphysis and the ‘open book’ fracture of the pelvis
Discussion
Similar to the results obtained by Bauman et al. [21], our study demonstrates that US evaluation of pubic symphysis during FAST–PLUS, may help to identify patients with unstable pelvic fractures presenting with pubic SW > 2.5 cm transverse diameter. Evaluation of pelvic ring anatomy and stability is usually performed with CT or X-ray. The X-ray anteroposterior projection, usually performed during the primary survey, provides a huge amount of information about the mechanism of injury. Additional projections (i.e. inlet view, outlet view and oblique projections) are useful for the evaluation of cranial dislocation of hemipelvis and for posterior sacroiliac joint or pubic branches dislocation. CT remains the gold-standard technique for the diagnosis and characterisation of pelvic ring fractures, allowing for panoramic exploration and greater anatomical detail [3]. US shows a high correlation with CT findings in detecting critical SW and OB unstable pelvic fractures. However, US has no accuracy in the detection of lateral compression and vertical shear injuries, because in these types of fractures, the symphysis usually remains intact, without any alteration at US exam. Moreover, as regards anteroposterior pelvis compression injuries, the FAST–PLUS protocol does not allow for identification of the different degrees of the Young and Burgess classification, but it is a reliable diagnostic clue to detect unstable OB pelvic fractures with a pubic SW over 2.5 cm in transverse diameter. According to these results, an additional single transverse scan on the pubic symphysis during the FAST–PLUS protocol is not time consuming and may provide a quick evaluation of the degree of critical SW, with a high diagnostic indication of pelvic ring instability and urgent operative management. Nevertheless, CT remains the gold-standard technique for the entire evaluation of pelvic anatomy and the detection of the type and degree of pelvic ring fractures and the associated injuries (such as vascular, urogenital and nerve lesions).
Conclusions
US evaluation of pubic symphysis with FAST–PLUS protocol shows a high correlation with CT findings in detection of pubic critical SW, as well as OB unstable pelvic fractures in patients with anteroposterior mechanism of injury. The FAST–PLUS protocol is not time-consuming and may provide a quick evaluation of the degree of critical SW, with a high diagnostic indication of pelvic ring instability and urgent operative management. Of course, further prospective studies on large case series are needed to verify this possible systematic use of US in traumatised patients.
Funding
The Authors declare that they do not receive any funding for the publication of this article.
Compliance with ethical standards
Conflict of interest
The Authors declare that they have no conflict of interest related to the publication of this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was acquired.
Research involving human participants and/or animals
This article does not contain any studies with animals performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Demetriades D, Karaiskakis M, Toutouzas K, et al. Pelvic fractures: epidemiology and predictors of associated abdominal injuries and outcomes. J Am Coll Surg. 2002;195:1–10. doi: 10.1016/S1072-7515(02)01197-3. [DOI] [PubMed] [Google Scholar]
- 2.Flint L, Cryer HG. Pelvic fracture: the last 50 years. J Trauma. 2010;69:483–488. doi: 10.1097/TA.0b013e3181ef9ce1. [DOI] [PubMed] [Google Scholar]
- 3.McCormak R, Strauss EJ, Alwatter BJ, et al. Diagnosis and management of pelvic fractures. Bull NYU Hosp Jt Dis. 2010;68:281–291. [PubMed] [Google Scholar]
- 4.Trainham L, Rizzolo D, Diwan A, et al. Emergency management of high-energy pelvic trauma. JAAPA. 2015;28:28–33. doi: 10.1097/01.JAA.0000473359.00222.a0. [DOI] [PubMed] [Google Scholar]
- 5.Yoon W, Kim JK, Jeong YY, et al. Pelvic arterial hemorrhage in patients with pelvic fractures: detection with contrast-enhanced CT. RadioGraphics. 2004;24:1591–1605. doi: 10.1148/rg.246045028. [DOI] [PubMed] [Google Scholar]
- 6.Pennal GF, Tile M, Waddell JP, et al. Pelvic disruption: assessment and classification. Clin Orthop Relat Res. 1980;151:12–21. [PubMed] [Google Scholar]
- 7.Gertzbein SD, Chenoweth DR. Occult injuries of the pelvic ring. Clin Orthop Relat Res. 1977;128:202–207. [PubMed] [Google Scholar]
- 8.Stahel PF, Hammerberg EM. History of pelvic fracture management: a review. World J Emerg Surg. 2016;11:18. doi: 10.1186/s13017-016-0075-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vaidya R, Scott AN, Tonnos F, et al. Patients with pelvic fractures from blunt trauma. What is the cause of mortality and when? Am J Surg. 2016;211:495–500. doi: 10.1016/j.amjsurg.2015.08.038. [DOI] [PubMed] [Google Scholar]
- 10.Chong KH, DeCoster T, Osler T, et al. Pelvic fractures and mortality. Iowa Orthop J. 1997;17:110–114. [PMC free article] [PubMed] [Google Scholar]
- 11.Sampson MA, Colquhoun KBM, Hennessy NLM. Computed tomography whole body imaging in multi-trauma: 7 years experience. Clin Radiol. 2006;61:365–369. doi: 10.1016/j.crad.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 12.Trinci M, Piccolo CL, Ferrari R, et al. Contrast-enhanced ultrasound (CEUS) in pediatric blunt abdominal trauma. J Ultrasound. 2019;22:27–40. doi: 10.1007/s40477-018-0346-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Piccolo CL, Trinci M, Pinto A. Role of contrast-enhanced ultrasound (CEUS) in the diagnosis and management of traumatic splenic injuries. J Ultrasound. 2018;21:315–327. doi: 10.1007/s40477-018-0327-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moylan M, Newgard CD, Ma OJ, et al. Association between a positive ED FAST examination and therapeutic laparotomy in normotensive blunt trauma patients. J Emerg Med. 2007;33:265–271. doi: 10.1016/j.jemermed.2007.02.030. [DOI] [PubMed] [Google Scholar]
- 15.Ianniello S, Di Giacomo V, Sessa B, et al. First-line sonographic diagnosis of pneumothorax in major trauma: accuracy of e-FAST and comparison with multidetector computed tomography. Radiol Med. 2014;119:674–680. doi: 10.1007/s11547-014-0384-1. [DOI] [PubMed] [Google Scholar]
- 16.Ianniello S, Piccolo CL, Trinci M. Extended-FAST plus MDCT in pneumothorax diagnosis of major trauma: time to revisit ATLS imaging approach? J Ultrasound. 2019;22:461–469. doi: 10.1007/s40477-019-00410-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stengel D, Bauwens K, Sehouli J, et al. Emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma. Cochrane Database Syst Rev. 2005;2015(9):004446. doi: 10.1002/14651858.CD004446.pub2. [DOI] [PubMed] [Google Scholar]
- 18.Kirkpatrick AW, Sirois M, Laupland KB, et al. Prospective evaluation of hand-held focused abdominal sonography for trauma (FAST) in blunt abdominal trauma. Can J Surg. 2005;48:453–460. [PMC free article] [PubMed] [Google Scholar]
- 19.Poletti PA, Wintermark M, Schnyder P, et al. Traumatic injuries: role of imaging in the management of the polytrauma victim (conservative expectation) Eur Radiol. 2002;12:969–978. doi: 10.1007/s00330-002-1353-y. [DOI] [PubMed] [Google Scholar]
- 20.Becker I, Woodley SJ, Stringer MD. The adult human pubic symphysis: a systematic review. J Anat. 2010;217:475–487. doi: 10.1111/j.1469-7580.2010.01300.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bauman M, Marinaro J, Tawil I, et al. Ultrasonographic determination of pubic symphyseal widening in trauma: the FAST-PS Study. J Emerg Med. 2011;40:528–533. doi: 10.1016/j.jemermed.2009.08.041. [DOI] [PubMed] [Google Scholar]