Abstract
In this paper, we describe the pattern of an idiopathic corpus cavernosum (CC) abscess using contrast-enhanced ultrasound (CEUS) and compare this to the lesion characterization achieved using preliminary baseline ultrasound/color doppler (ECD). In a 43-year-old man, who arrived at our emergency department for a penile swelling and hematopyuria, ECD examination showed equivocal mucosal and subcutaneous tissue swelling, an inhomogeneous hypoechoic area in the left CC, and a suspected millimetric interruption of the albuginea. CEUS showed multiple avascular areas wrapped in a hyperperfused rim representing abscesses and a not-perfused balanopreputial-oriented fistula. A CEUS control documented clinical remission after surgery. CEUS is a noninvasive and bedside executable method that allows a more precise evaluation of the entity, localization, and possible complications of CC abscesses and, therefore, permits prescribing the most adequate therapy to the patient, as well as the evaluation of eventual postsurgical sequelae.
Keywords: CEUS, Abscess, Corpus cavernosum, Fistula
Introduction
A 43-year-old male was admitted to the emergency department with a 7-day history of progressive penile pain, tumescence, swelling, and fever of 39 °C associated with dysuria. He rejected any history of penile trauma, instrumentation, or high-risk sexual activity, nor did he have any appreciable past medical history. Local examination revealed an enlarged, swollen penis, more marked on the distal shaft of the penis. A millimetric mucosal lesion with pus discharge was noted on the dorsal aspect of the distal penis on the left side near the corona glandis. Hematological analysis on admission revealed a raised white cell count (14.670 × 103/μL) and C-reactive protein level (9.05 mg/L). Penile basal ultrasound (US), executed with Mylab Class C (Esaote, Genoa, Italy) equipped with a linear US probe (LA 533), revealed a hypoechoic and hypervascular area in the dorsal aspect of the corpus cavernosum (CC) with interruption of the tunica albuginea suggestive of a phlogistic intracavernous reaction originating from an idiopathic continuous solution in the balanopreputial seat (Fig. 1), a millimetric inhomogeneous hypoechoic area centered in the ventral portion of the left CC, and a mucosal and subcutaneous tissue swelling (Fig. 2). Because of a poor correlation between clinical presentation and US findings, we performed contrast-enhanced US (CEUS) using contrast-tuned imaging (CnTI) technology that allows for real-time angiosonography, using a second-generation US contrast agent. The real-time evaluation (6 min) was performed after an injection of 2.4 mL (5 mg/mL) of SonoVue (Bracco S.A., Geneva, Switzerland), followed by 10 mL saline flush via a cannula in the antecubital fossa. CEUS revealed the presence of a large avascular area wrapped in a hyperperfused rim in all the acquisition phases (typical semeiotics for abscesses in other organs) located at the ventral side of the middle and distal parts of the cavernous body (Fig. 3). This abscess extended up to the distal dorsal side of the cavernous body, where the interruption of the albuginea tunic (Fig. 4), with the presence of a fistula with the preputial sulcus, visualized as a not-perfused tubular string, was confirmed (Fig. 5). Furthermore, the prolonged survey has allowed us to highlight additional multiple micro abscesses located in both cavernous bodies (Fig. 6).
Fig. 1.
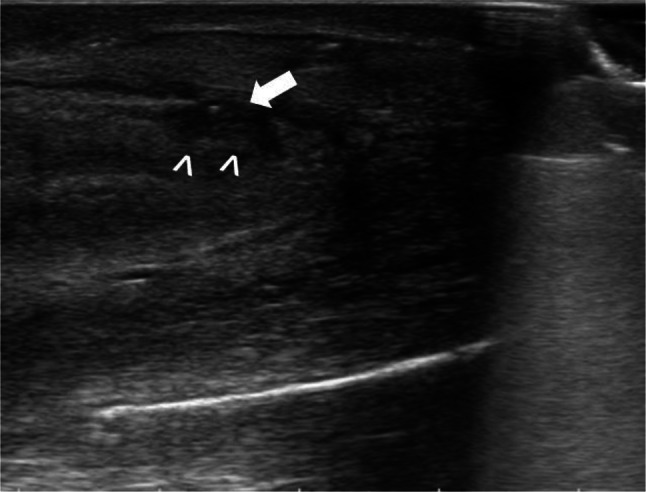
Grayscale US shows hypoechoic area in the dorsal side of CC (arrowhead) with interruption of the tunica albuginea (arrow) suspected of phlogosic intracavernous reaction
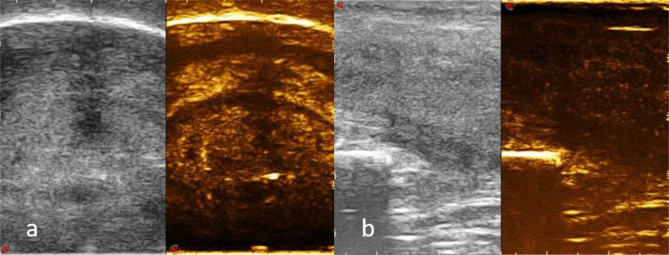
Fig. 2.
a ECD shows millimetric inhomogeneous hypoechoic and hypervascular area (arrowhead) centered in the ventral portion of the left CC; b mucosal and subcutaneous tissue swelling (arrow)
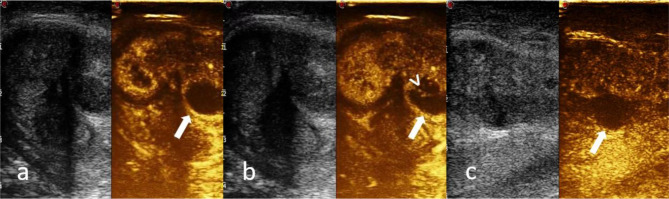
Fig. 3.
a–c CEUS shows a marginal rim enhancement in the arterial phase persistent in the tardive one (arrow), enhancement of the septa (arrowhead) and no perfusion of the necrotic areas
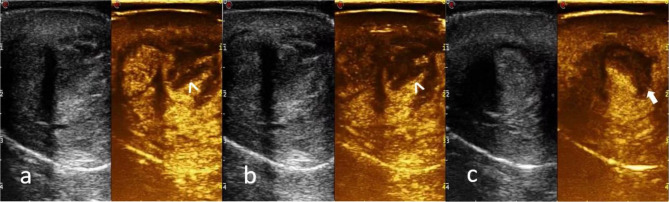
Fig. 4.
a, b CEUS shows a large abscess located in the ventral side of the middle and distal part of the cavernous body (arrowhead) and extended up to the distal dorsal side of the cavernous body (arrowhead) with the interruption of the albuginea tunic (arrow)
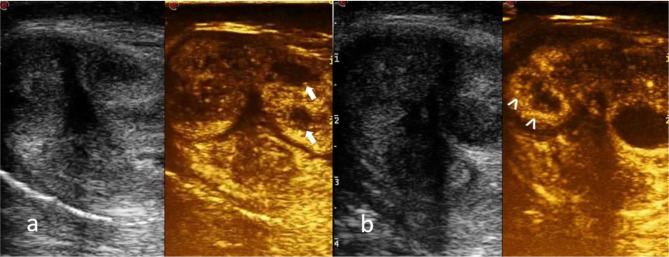
Fig. 5.
a, b CEUS shows the interruption of the albuginea tunic, with the presence of a fistula with the preputial sulcus (arrowhead); c purulent material in the subprepucial space (arrow)
Fig. 6.
a CEUS shows two abscesses in the left corpus cavernosum (arrow); b CEUS identificates two small abscesses in the right corpus cavernosum not evident in the basal evaluation (arrowhead)
The patient underwent corporotomy along the left corpora, which revealed a deep cavity extending from the distal to the middle CC portion. After thorough cleansing, the incision was closed with absorbable sutures. Samples taken during the incision and drainage gave positive results for Streptococcus anginosus. The patient’s symptoms disappeared after the curettage and intramuscular injection of broad-spectrum antibiotics for a week. He recovered fairly well after drainage without any further recurrence of abscesses. Outpatient assessments after 20 days and 8 weeks revealed the absence of early complications (Figs. 7, 8); after healing of the surgical wound (12 weeks after surgery), the patient started a regimen of vacuum therapy twice a day. The first valid sexual intercourse happened 14 weeks after surgery, although satisfactory erectile function was recovered only 5 months after the surgical procedure.
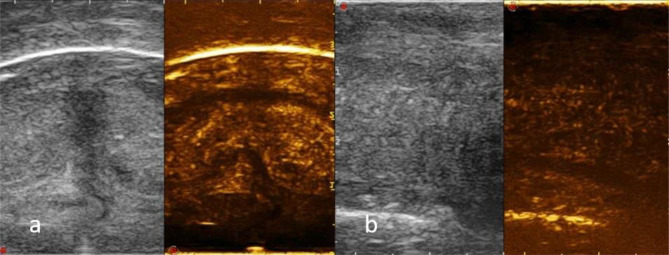
Fig. 7.
a, b (Outpatient assessment after 20 days) CEUS shows a homogeneous and progressive perfusion of CC without evidence of residual abscess
Fig. 8.
a, b (Outpatient assessment after 8 weeks) CEUS documents the restitutio ad integrum of CC
Discussion
An abscess of the CC is an uncommon clinical entity, with a scarcity of reported cases in the literature. Abscesses of the CC are etiologically classified into primary, secondary, and idiopathic (sine causa) abscesses. Primary abscesses are related to an intra-cavernosal injection, penile trauma, and iatrogenic causes. Secondary abscesses are related to perianal/perineal/intra-abdominal abscesses and/or hematogenic diffusion [1]. In this case, no demonstrable causative factor was identified, and it was therefore characterized as an idiopathic/spontaneous abscess.
Imaging options for abscesses of the CC include US, magnetic resonance (MR), and computed tomography (CT) [2]. US is the primary imaging modality in patients with penile disease [3]. US is an easily accessible, bedside executable, noninvasive technique that allows concurrent drainage of the penile abscess. In mild cases, baseline sonographic examination shows abnormal echogenicity, increased thickness of the mucosa, increased echogenicity of the subcutaneous tissue, limited inhomogeneous hypoechoic areas, and marked hyperemia of the cavernous bodies with color Doppler US (ECD) evaluation. In severe cases, B-mode US demonstrates anechoic or hypoechoic collections of fluid with sediment and poorly defined borders [4]. Although CT is not commonly indicated for primary evaluation of the penis, because of the use of ionizing radiation and low soft-tissue contrast resolution, it allows the identification of abscess location, demonstrates relationships with adjacent structures, and guides drainage. Penile abscesses manifest themselves at CT as fluid collections, sometimes containing an air bubble, with edema in the adjacent fat and with wall hyperemia after administration of contrast material. If available, MR provides a superior soft-tissue contrast resolution. At MR, a penile abscess demonstrates low signal intensity on T1-weighted images and high signal intensity on T2-weighted images, with rim enhancement after injection of gadolinium contrast material. CT or MR imaging evaluates the extent of the disease to the perineum, abdominal wall, fascial planes, and buttocks [5].
In our patient, clinical diagnosis was suspected after urological examination; however, the sonographic findings were not conclusive. Even though the latest EFSUMB (European Federation of Societies for Ultrasound in Medicine and Biology) guidelines do not include the use of SonoVue for studying the CC [6], given the particularity of the case and with prior informed consent, we decided to perform CEUS evaluation. CEUS is a real-time imaging technique performed by intravenously injecting microbubble-based contrast agents (SonoVue); the technique can be performed even in patients with impaired renal function. After intravenous injection, the microbubble-based contrast agents pass through the pulmonary filter and remain within the intravascular space (blood pool agents). CEUS gives rise to several typical elements that lead to a positive abscess diagnosis, such as marginal rim enhancement in the arterial phase persistent in the tardive one, enhancement of the septa, and no perfusion in the necrotic areas. In our case, CEUS was not only effective for the detection of the ventral abscess and the incipient fistula oriented toward the balanopreputial sulcus, visualized as a not-perfused tubular string; it also demonstrated the actual dimensions of the voluminous abscess occupying the distal middle third of the cavernous body (only slightly evident at the basal control) as well as bilaterally evident micro abscesses, which were not appreciable in the baseline examination. Since MR was not available at our hospital, we performed CEUS, which allowed us to obtain a precise evaluation of the entity and localization of CC abscesses.
The management options for cavernosal abscesses consist of antibiotic therapy and either open surgical incision and drainage or radiologically guided needle aspiration [7]. Owing to the complex and loculated nature of his abscess, the present patient underwent immediate incision of the left CC and drainage. CEUS was effective in outpatient assessments after 20 days and 8 weeks, which documented homogeneous and progressive perfusion of the CC without evidence of a residual abscess, fibrotic tissue, or other postsurgical complications. Evidently, the patient will undergo subsequent CEUS checks for at least the next 2 years given the possible late onset of fibrosis; in these patients, the clinical course is unpredictable, as in some cases the incubation lasts for a few years, while in other cases evolution is more rapid [8].
Conclusion
A CC abscess constitutes a rare urological condition. Prompt diagnosis and treatment may reduce the risk of long-term sequelae, which could result in cavernosal fibrosis (difficult maintenance of penile rigidity, worsening premature ejaculation, vague sensations of not well-defined tingling or glans tingling, a decrease in sexual desire, and deviations of the axis of the penis or its curvatures).
In the present case report, CEUS of a spontaneous CC abscess, to our knowledge for the first time, was applied as a supplement to the conventional US/CD examination. CEUS was of great value in the definitive diagnosis and a more precise evaluation of the entity and localization of the abscess as well as its tendency to create a fistulous via. All this allowed us to provide the patient with the most adequate therapy and to avoid an underestimation of the real extension of the abscess with consequent delaying of the surgical procedure. After therapy, given the possible late onset of fibrosis, follow-up with CEUS will have to be extended. If confirmed by prospective studies, CEUS could enter the diagnostic algorithm of CC abscesses, concerning the management of both the acute patient and the follow-up.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Lobianco Roberto, Email: roberto.lobianco@aslnapoli2nord.it.
Capuano Silvestro, Email: silviocapuano27@gmail.com.
D’Alessandro Lucia, Email: lucia.dalessandro@aslnapoli2nord.it.
Balestrieri Umberto, Email: umberto.balestrieri@aslnapoli2nord.it.
Coletta Antonella, Email: antonella.coletta@aslnapoli2nord.it.
Masala Daniele, Email: daniele.masala@aslnapolinord.it.
References
- 1.Dugdale CM, Tompkins A, Reece R, Gardner A. Cavernosal abscess due to Streptococcus anginosus: a case report and comprehensive. Rev Literature Curr Urol. 2013;7:51–56. doi: 10.1159/00034355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thanos L, Tsagouli P, Eukarpidis T, Mpouhra K, Kelekis D. Computed tomography-guided drainage of a corpus cavernosum abscess: a minimally invasive successful treatment. Cardiovasc Intervent Radiol. 2011;34:217–219. doi: 10.1007/s00270-010-9923-x. [DOI] [PubMed] [Google Scholar]
- 3.Bertolotto M, Pavlica P, Serafini G, Quaia E, Zappetti R. Painful penile induration: imaging findings and management. RadioGraphics. 2009;29:477–493. doi: 10.1148/rg.292085117. [DOI] [PubMed] [Google Scholar]
- 4.Serafini G, Bertolotto M, Lacelli F, Sconfienza L, Perrone N. Penile inflammation. In: Bertolotto M, editor. Color Doppler US of the penis. Berlin: Springer; 2008. pp. 147–151. [Google Scholar]
- 5.Kickuth R, Adams S, Kirchner J, Pastor J, Simon S, Liermann D. Magnetic resonance imaging in the diagnosis of Fournier’s gangrene. Eur Radiol. 2001;11:787–790. doi: 10.1007/s003300000599. [DOI] [PubMed] [Google Scholar]
- 6.Sidhu PS, Cantisani V, et al. The EFSUMB guidelines and recommendations for the clinical practice of contrast-enhanced ultrasound (CEUS) in non-hepatic applications: update 2017 (long version) Ultraschall Med. 2018;39(2):e2–e44. doi: 10.1055/a-0586-1107. [DOI] [PubMed] [Google Scholar]
- 7.Ehara H, Kojima K, Hagiwara N, Phuoc NB, Deguchi T. Abscess of the corpus cavernosum. Int J Infect Dis. 2007;11:553–554. doi: 10.1016/j.ijid.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Levine L, Larsen S. Diagnosis and management of peyronie disease. In: Wein A, editor. Campbell–Walsh urology. 11. Philadelphia: Elsevier; 2016. pp. 722–748. [Google Scholar]