Abstract
Purpose
We have focused on the two-dimensional (B-mode) and the time-motion (M-mode) analysis of the zone of apposition to determine the reliability of diaphragm ultrasonography in the clinical environment.
Methods
Ten healthy volunteers were enrolled and studied by three operators with different skills in ultrasonography. For every volunteer, each operator acquired three images of the diaphragm for each side, both in B-mode and in M-mode. Then a fourth operator calculated the thickening fraction (TF), by means of the formula TF = (TEI − TEE)/TEE (TEI is the thickness at end inspiration and TEE the thickness at end expiration). Afterwards, intraclass correlation coefficients (ICCs) were computed on TF to establish reproducibility and repeatability both in the B- and M-modes. A Coefficient of Repeatability or repeatability (CR) ≤ 0.3 was considered acceptable.
Results
Both B-mode (CRs 0.16–0.26) and M-mode (CRs 0.10–0.15) were sufficiently repeatable to assess TF, except for the less experienced operator (CRs B-Mode 0.20–0.32). Reproducibility was moderate to good between operators with CRs much narrower for the M-Mode (0.13–0.14).
Conclusions
The results of our study have shown that diaphragm ultrasound is repeatable and reproducible when carried out by a radiologist or an intensivist with a basic curriculum in ultrasonography. The method is more accurate when using the M-mode for less experienced operators, and in this case, repeatability and reproducibility are not sufficient to make clinical decisions. No TF value lower than 36% was obtained using both techniques. This suggests the existence of a cut-off value that could be used as an initial tool to discriminate healthy subjects from those affected by diaphragmatic dysfunction.
Clinical trial registration
EUDRACT 2015-004635-12.
Keywords: Diaphragm ultrasonography, Repeatability
Introduction
The diaphragm is the main respiratory muscle, but evaluation of its function remains elusive. Ultrasonography is a portable, non-invasive and ionizing radiation-free technique which may represent a good tool for diaphragm functional analysis [1].
In 1989, Wait et al. described for time-motion (M-mode) ultrasonography a linear relationship between diaphragm thickening and lung volumes [2]. The study of the diaphragm using ultrasonography has been expanded from this initial observation. More recent studies have focused on the amplitude of excursion of the diaphragmatic dome using M-mode ultrasonography [3, 4]. This method seemed suitable to show postoperative diaphragmatic dysfunction after major abdominal surgery [3, 4]. A variant of this method was applied after cardiac surgery in patients who required prolonged mechanical ventilation [5]. Finally, sequential two-dimensional (B-mode) analysis of the “zone of apposition” (ZOA) of the diaphragm to the rib cage has been used to determine recovery from diaphragmatic paralysis in medical patients [6].
Although sonography has become a widely used tool, capable of providing a non-invasive, bedside evaluation of diaphragmatic function, a significant limitation lies in its intrinsic operator dependency [7]. A recent study showing the relationship between diaphragm thickening, assessed by M-mode scanning of the ZOA, and respiratory muscle effort showed low intra-observer variability [8], but all measurements were carried out by two equally experienced physicians, and the inter-observer variability was not addressed [9]. Indeed, diaphragm ultrasonography was not positively associated with prediction of extubation in ICU patients [10], and in a “real-life” ICU, the extent of expertise in ultrasonography greatly varies among operators.
Therefore, the aim of this study was to determine reproducibility and repeatability of ultrasound assessment of the ZOA and to identify which method between B-mode or M-mode is associated with less variability (including right side vs left side). The measurements were carried out by three operators with different experiences in the field of echographic imaging: a radiologist, a resident in anesthesiology and intensive care, and a medical student.
Materials and methods
This protocol was approved by the Internal Review Board of the local Ethics Committee Comitato Etico Area Vasta Centro on March 23, 2015 (protocol number 2015/0010819, number of approval OSS.14.091), and written informed consent was collected from the volunteers enrolled.
Ultrasonography was carried out by three operators: a radiologist, a resident in anesthesiology and intensive care with basic knowledge and skills in critical care ultrasonography [11], and a medical student. Before the study began, all operators underwent a training period of ten sessions during which all the operators learnt how to recognize the anatomical landmarks used in the protocol proposed (see below). All the measurements were taken using an Esaote MyLab 25 System (Esaote, Genoa, Italy) equipped with a 12 MHz linear probe, after positioning each volunteer in a semi-recumbent position (with the head of the bed elevated at an angle of 45° calculated by a goniometer).
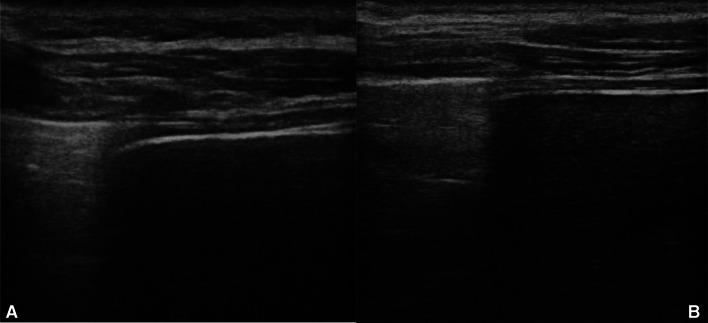
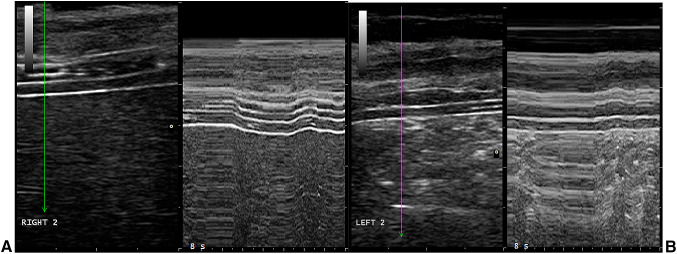
Initially, each operator identified the caudal border of the costophrenic sinus as the zone of transition from the artefactual representation of the aerated lung to the visualization either of the diaphragm and liver or of the diaphragm and spleen (“curtain sign”), respectively, on the right and on the left sides. The diaphragm was identified by the two hyperechoic lines of pleural and peritoneal membranes. In B-mode, two frames were used: the inspiratory one, in which there is the greatest diaphragm thickness, and the expiratory one, in which the thickness is at its thinnest (Fig. 1). In M-mode, both the respiratory phases are represented in the same frame (Fig. 2). The ZOA lies 0.5–2 cm below the costophrenic sinus. Then each operator acquired a recording for each side, both in B-mode and in M-mode, for a total of four acquisitions for each volunteer [8]. To test the intra-operator variability and to minimize the memory bias of each operator, the acquisitions were repeated 3 times, at a distance of at least 10 min. Recordings made by the various operators took place according to a predetermined random order, generated by the algorithm of the site www.randomization.com.
Fig. 1.
B-mode: right (a) and left side (b)
Fig. 2.
M-mode: right (a) and left side (b)
First, the ultrasound recordings were stored in the echographic system, then saved in a USB flash drive, transferred to a personal computer, and analyzed by a fourth operator, not involved in image acquisitions and unaware of which operator had carried out the recordings.
For both methods, each operator measured the diaphragm thickness at end-inspiration (TEI), the diaphragm thickness at end-expiration (TEE) and calculated the thickening fraction (TF) using the formula TF = (TEI − TEE)/TEE [8].
Statistical analysis
Using repeated-measure ANOVA, the sample size was set as 10 volunteers on whom 90 measurements were carried out for each side of the diaphragm in B-mode and M-mode. The total number of measurements was 10 * 3 * 3 * 2 * 2 = 360.
Data have been analyzed by means of intraclass correlation coefficients (ICCs) using the icc command available in Stata 15.1 (StataCorp, College Station, TX). The xtreg command has been used to fit random-effects linear models, which have computed within-volunteer and between-volunteer measurement error based on multiple repeated measures. Measurement error was used to calculate the 95% coefficient of repeatability and reproducibility by multiplication for the square root of 2 since measurement between any two occasions adds up on the variance scale.
The threshold limit was fixed to 0.3: an index below 0.1 is considered optimal, but also an index between 0.1 and 0.3 is considered acceptable, especially in the case of measurements which are very difficult to acquire [12].
Results
A total of ten young adults, healthy volunteers (five males and five females) with the demographic and anthropometric characteristics shown in Table 1 were enrolled. Each volunteer was scanned by the three operators on the same day. Operator 1 corresponds to the radiologist, operator 2 to the resident and operator 3 to the medical student. The fourth operator found that the diaphragm had been correctly identified in each image acquisition by observing the saved videoclips.
Table 1.
Demographic and anthropometric characteristics of the enrolled subjects. Data is presented as means and 95% confidence intervals (parentheses)
| Female n = 5 |
Male n = 5 |
|
|---|---|---|
| Weight (kg) | 58.80 (CI 95%: 51.65–65.95) | 77.40 (CI 95%: 68.95– 85.85) |
| Height (cm) | 165.20 (CI 95%: 160.28–170.12 | 184 (CI 95%: 176.60–191.40) |
| BMI | 21.54 (CI 95%: 19.14–23.94) | 22.82 (CI 95%: 21.65–23.99) |
| Age (Years) | 32 (CI 95%: 29–36) | 31 (CI 95%: 30–32) |
Table 2 shows within-rater intraclass correlation coefficient (ICC) and 95% coefficient of repeatability for both the B-mode and the M-mode.
Table 2.
Intraclass correlation coefficient and coefficient of repeatability for each operator
| Intraclass correlation coefficient | Coefficient of repeatability | ||||
|---|---|---|---|---|---|
| Right | Left | Right | Left | ||
| Operator 1 | B | 0.75 (0.46–0.92) | 0.72 (0.42–0.91) | ± 0.16 | ± 0.15 |
| M | 0.69 (0.33–0.89) | 0.76 (0.47–0.92) | ± 0.10 | ± 0.12 | |
| Operator 2 | B | 0.55 (0.18–0.84) | 0.45 (0.07–0.79) | ± 0.23 | ± 0.26 |
| M | 0.81 (0.57–0.94) | 0.80 (0.54–0.94) | ± 0.14 | ± 0.14 | |
| Operator 3 | B | 0.61 (0.26–0.87) | 0.39 (0.01–0.76) | ± 0.20 | ± 0.32 |
| M | 0.77 (0.50–0.93) | 0.83 (0.61–0.95) | ± 0.13 | ± 0.15 | |
B-mode: A better ICC was obtained for the right side compared to the left side for all operators, although they were almost identical for Operator 1. We also observed better ICCs for Operator 1 compared to the others. A similar pattern was observed across operators for 95% coefficient of repeatability, which was better for Operator 1 (0.15/0.16 for right and left sides, respectively) compared to Operators 2 and 3 (0.23/0.26 and 0.20/0.32, respectively).
M-mode: The difference in reproducibility between right and left sides was decreased or reverted in this mode. In fact, ICCs were between 0.76 and 0.83 for the left side for all three operators compared to 0.60–0.81 for the right side. 95% coefficients of repeatability were similar for the right and left sides and for all operators.
Table 3 shows between-rater ICCs as well as the 95% coefficient of reproducibility. For B-mode, all ICCs were moderate to good (0.55–0.68); however, 95% coefficients of reproducibility were wide (0.32–0.36). For M-mode, all ICCs were better than for B-mode (0.72–0.78); moreover, coefficients of reproducibility were much narrower for M-mode (0.13–0.14) compared to B-mode.
Table 3.
Intraclass correlation coefficient and coefficient of reproducibility between raters
| Intraclass correlation coefficient | Coefficient of reproducibility | ||||
|---|---|---|---|---|---|
| Operator 1 | Operator 2 | Operator 1 | Operator 2 | ||
| Operator 2 | B | 0.55 (0.32–0.76) | ± 0.33 | ||
| M | 0.74 (0.55–0.87) | ± 0.14 | |||
| Operator 3 | B | 0.68 (0.47–0.84) | 0.65 (0.43–0.82) | ± 0.36 | ± 0.32 |
| M | 0.72 (0.51–0.86) | 0.78 (0.60–0.89) | ± 0.13 | ± 0.14 | |
Discussion
Ultrasound technology is a safe, accurate and cost-effective bedside tool, capable of easing physical examination if used by well-trained physicians [13]. In the last decades, ultrasound machines have become very popular to manage critically ill patients, both in emergency departments and in ICUs. To the best of our knowledge, one of the first applications of ultrasonography to the diaphragm was in 1989 [2]. Since then there has been an increasing interest in diaphragm echography. The main fields of research have been post-operative paralysis [4–6], assessment of neuromuscular disorders [14–16], weaning from mechanical ventilation [17, 18], management of medical patients with dyspnea [6], evaluation of diaphragm rupture in trauma patients [19] and pleural effusions by craniocaudal displacement [20].
A variety of ultrasonographic methods have been used to evaluate diaphragm thickness or excursion, such as two-dimensional evaluation of the craniocaudal displacement [21], M-mode of the thick echogenic line visualized through the liver acoustic window [3, 4, 22, 23], two-dimensional and M-mode evaluation of the diaphragm in the ZOA [2, 6, 8, 24, 25], and by indirect liver movement [26]. This study tested the precision of the diaphragm thickening in the ZOA—both in M- and B-Modes—using a 12 MHz linear probe. We chose this method because it may be more suitable for both medical and surgical patients, especially those undergoing major abdominal surgery. Both the right and the left sides of the diaphragm were scanned. Although the images of the left side were more difficult to obtain in some cases, a bilateral analysis was conducted for all the enrolled volunteers.
Based on the recent literature, ultrasonography has been generally regarded as an accurate method for diaphragm functional imaging due to its reproducibility and repeatability [2, 3, 18, 24, 27]. The findings of this study would confirm the accuracy of this imaging tool; however, in B-Mode, a skilled operator is necessary to obtain reliable measurements. Based on the 95% CR coefficient of repeatability, the radiologist showed 0.15 and 0.16 for the right and left hemi-diaphragms, respectively. On the other hand, operators 2 and 3 accounted for a 95% CR between 0.20 and 0.36 for each side, respectively; the latter value cannot be considered acceptable to consider this method accurate [12]. For the reproducibility, the ICC showed good to moderate correlation when operator 1 was compared to operators 2 and 3, respectively, but the coefficient of reproducibility was wide ranging. Healthcare providers with little or no experience in ultrasonography (such as our medical student) need to be trained extensively before using the ultrasound machine as a tool to scan diaphragm activity by measuring its thickness.
The TF values observed in our study were never lower than 36%, a threshold which could be useful to discriminate between healthy subjects and those with diaphragmatic dysfunction. This threshold is higher than that observed in previous studies, where TF was lower than 30% [25, 28, 29], but it was calculated in a different way from the present study. Consistent with previous studies, the left side was more difficult to analyze, probably due to the non-optimal acoustic window offered by the spleen.
In this study, the applied methods were considered accurate enough to assess diaphragmatic function, given that the 95% Coefficient of Repeatability were lower than 30%, with operators with baseline or extensive skills. This result confirms to a certain extent what has been reported in previous studies although there are some differences. First, in our study, an ANOVA with ICC was used to assess two different measurement methods (B-mode and M-mode diaphragm ultrasonography), while other authors used, for example, the Pearson correlation analysis [3, 8, 18], which makes any comparison extremely difficult. Second, to best reproduce the reality of daily clinical practice, and given that not all ICU physicians have the same expertise in clinical ultrasonography, this study compared the ability of three operators with different levels of experience, a factor which may have introduced a bias. Finally, statistical analysis was conducted only on TF, which was calculated after measuring TEE and TEI. This greatly increased the margin of error in this study compared to other studies, which, for example, taking into consideration the craniocaudal displacement of the left portal vein, only evaluated the reproducibility of a single, non-derivative measurement [30]. Moreover, although only 10 volunteers were included in the study 360 measurements were collected. Finally, the major limit of the study is represented by the fact that only healthy volunteers were taken into consideration. However, we can reasonably presume that if a method is not reproducible in healthy people, it could scarcely be accurate in patients.
According to our study, despite several sessions of training, the medical student was not capable of making accurate scans, especially in B-mode. On the contrary, an intensivist with a curriculum in ultrasonography without particular expertise in lung or diaphragm ultrasonography can perform an accurate scan of the diaphragm in daily practice.
The present study suggests that echography of the ZOA is quite accurate to measure diaphragm thickness and TF, whichever method is used, with experienced operators. For less experienced operators, adequate training is recommended to improve reproducibility if B-mode is used, whereas M-mode is more reproducible, although it provides less informative images. Since our data were obtained in healthy volunteers, we cannot directly apply these results to patients. However, no TF value lower than 36% was obtained using both techniques. This suggests the existence of a cut-off value that could be used as an initial tool to discriminate healthy subjects from those affected by diaphragmatic dysfunction. Further studies could be conducted to more accurately define this cut-off.
In conclusion, our experience suggests that a rough evaluation of diaphragmatic thickening could be performed by an operator with basic skills in bedside ultrasonography [11, 31]. When it is necessary to precisely measure thickening fractioning, an operator with a high level of expertise and training is mandatory to obtain reliable values.
Acknowledgements
CA, FP, IC, SM, and VG had access to all of the data in the study; CA took responsibility for the integrity of the data and the accuracy of data analysis. FP, IC, SM and MB contributed substantially to the study design, data collection, analysis, and interpretation. IC and FP wrote this manuscript. AC, BM, and VG revised and approved the proof, before submission.
Abbreviations
- CT
Computed tomography
- MRI
Magnetic resonance imaging
- M-mode
Time-motion ultrasonography
- B-mode
Two-dimensional morphological ultrasonography
- ZOA
Zone of apposition of the diaphragm to the rib cage
- MV
Mechanical ventilation
- NIV
Non-invasive ventilation
- ICU
Intensive care unit
- R&R
Repeatability and reproducibility
- TEI
Diaphragm thickness at end inspiration
- TEE
Diaphragm thickness at end expiration
- TF
Thickening fraction
- ANOVA
Analysis of variance
Funding
Chiara Adembri was funded by the University of Florence.
Compliance with ethical standards
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
All procedures performed in the present study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Ethical approval has been obtained for Comitato Etico Area Vasta Toscana Centro with EUDRACT number 2015-004635-12.
Informed consent
Informed consent has been collected from all participants enrolled in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kharma N. Dysfunction of the diaphragm: imaging as a diagnostic tool. Curr Opin Pulm Med. 2013;19(4):394–398. doi: 10.1097/MCP.0b013e3283621b49. [DOI] [PubMed] [Google Scholar]
- 2.Wait JL, Nahormek PA, Yost WT, Rochester DP, Rochester P. Diaphragmatic thickness-lung volume relationship in vivo volume relationship in vivo. J Appl Physiol. 1989;67:1560–1568. doi: 10.1152/jappl.1989.67.4.1560. [DOI] [PubMed] [Google Scholar]
- 3.Boussuges A, Gole Y, Blanc P. Diaphragmatic motion studied by M-mode ultrasonography methods, reproducibility, and normal values. Chest. 2009;135(2):391–400. doi: 10.1378/chest.08-1541. [DOI] [PubMed] [Google Scholar]
- 4.Kim SH, Na S, Choi JS, Na SH, Shin S, Koh SO. An evaluation of diaphragmatic movement by M-mode sonography as a predictor of pulmonary dysfunction after upper abdominal surgery. Anesth Analg. 2010;110(5):1349–1354. doi: 10.1213/ANE.0b013e3181d5e4d8. [DOI] [PubMed] [Google Scholar]
- 5.Lerolle N, Guérot E, Dimassi S, Zegdi R, Faisy C, Fagon J-Y, Diehl J-L. Ultrasonographic diagnostic criterion for severe diaphragmatic dysfunction after cardiac surgery. Chest. 2009;135(2):401–407. doi: 10.1378/chest.08-1531. [DOI] [PubMed] [Google Scholar]
- 6.Summerhill EM, El-Sameed YA, Glidden TJ, McCool FD. Monitoring recovery from diaphragm paralysis with ultrasound. Chest. 2008;133(3):737–743. doi: 10.1378/chest.07-2200. [DOI] [PubMed] [Google Scholar]
- 7.Oppersma E, Hatam N, Doorduin J, van der Hoeven JG, Marx G, Goetzenich A, Fritsch S, Heunks LMA, Bruells CS. Functional assessment of the diaphragm by speckle tracking ultrasound during inspiratory loading. J Appl Physiol. 2017;123(5):1063–1070. doi: 10.1152/japplphysiol.00095.2017. [DOI] [PubMed] [Google Scholar]
- 8.Vivier E, Mekontso Dessap A, Dimassi S, Vargas F, Lyazidi A, Thille AW, Brochard L. Diaphragm ultrasonography to estimate the work of breathing during non-invasive ventilation. Intensiv Care Med. 2012;38(5):796–803. doi: 10.1007/s00134-012-2547-7. [DOI] [PubMed] [Google Scholar]
- 9.Bellani G, Pesenti A. Assessing effort and work of breathing. Curr Opin Crit Care. 2014;20(3):352–358. doi: 10.1097/MCC.0000000000000089. [DOI] [PubMed] [Google Scholar]
- 10.Vivier E, Muller M, Putegnat JB, Steyer J, Barrau S, Boissier F, Bourdin G, Mekontso-Dessap A, Levrat A, Pommier C, et al. Inability of diaphragm ultrasound to predict extubation failure a multicenter study. Chest. 2019;155(6):1131–1139. doi: 10.1016/j.chest.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Fagley RE, Haney MF, Beraud AS, Comfere T, Kohl BA, Merkel MJ, Pustavoitau A, von Homeyer P, Wagner CE, Wall MH. Critical care basic ultrasound learning goals for American Anesthesiology Critical Care Trainees: recommendations from an expert group. Anesth Analg. 2015;120(5):1041–1053. doi: 10.1213/ANE.0000000000000652. [DOI] [PubMed] [Google Scholar]
- 12.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2017;16(4):346–346. doi: 10.1016/j.jcm.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guillory RK, Gunter OL. Ultrasound in the surgical intensive care unit. Curr Opin Crit Care. 2008;14(4):415–422. doi: 10.1097/MCC.0b013e3283060a27. [DOI] [PubMed] [Google Scholar]
- 14.DeBruin PF, Ueki J, Bush A, Khan Y, Watson A, Pride NB. Diaphragm thickness and inspiratory strength in patients with Duchenne muscular dystrophy. Thorax. 1997;52(5):472–475. doi: 10.1136/thx.52.5.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hardy F, Walker J, Sawyer T. Sonographic measurement of diaphragm movement in patients with tetraplegia. Spinal Cord. 2009;47(11):832–834. doi: 10.1038/sc.2009.45. [DOI] [PubMed] [Google Scholar]
- 16.Yoshioka Y, Ohwada A, Sekiya M, Takahashi F, Ueki J, Fukuchi Y. Ultrasonographic evaluation of the diaphragm in patients with amyotrophic lateral sclerosis. Respirology. 2007;12(2):304–307. doi: 10.1111/j.1440-1843.2006.01029.x. [DOI] [PubMed] [Google Scholar]
- 17.DiNino E, Gartman EJ, Sethi JM, McCool FD. Diaphragm ultrasound as a predictor of successful extubation from mechanical ventilation. Thorax. 2014;69(5):423–427. doi: 10.1136/thoraxjnl-2013-204111. [DOI] [PubMed] [Google Scholar]
- 18.Kim WY, Suh HJ, Hong S-B, Koh Y, Lim C-M. Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation. Crit Care Med. 2011;39(12):2627–2630. doi: 10.1097/CCM.0b013e3182266408. [DOI] [PubMed] [Google Scholar]
- 19.Blaivas M, Brannam L, Hawkins M, Lyon M, Sriram K. Bedside emergency ultrasonographic diagnosis of diaphragmatic rupture in blunt abdominal trauma. Am J Emerg Med. 2004;22(7):601–604. doi: 10.1016/j.ajem.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 20.Hassan M, Rizk R, Essam H, Abouelnour A. Validation of equations for pleural effusion volume estimation by ultrasonography. J Ultrasound. 2017;20(4):267–271. doi: 10.1007/s40477-017-0266-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Subotic DR, Stevic R, Gajic M, Vesovic R. Diaphragm motion and lung function prediction in patients operated for lung cancer—a pilot study on 27 patients. J Cardiothorac Surg. 2013;8:213–213. doi: 10.1186/1749-8090-8-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lloyd T, Tang YM, Benson MD, King S. Diaphragmatic paralysis: the use of M mode ultrasound for diagnosis in adults. Spinal Cord. 2006;44(8):505–508. doi: 10.1038/sj.sc.3101889. [DOI] [PubMed] [Google Scholar]
- 23.Nason LK, Walker CM, McNeeley MF, Burivong W, Fligner CL, Godwin JD. Imaging of the diaphragm: anatomy and function. Radiographics. 2012;32(2):E51–E70. doi: 10.1148/rg.322115127. [DOI] [PubMed] [Google Scholar]
- 24.Cohn D, Benditt JO, Eveloff S, McCool FD. Diaphragm thickening during inspiration. J Appl Physiol. 1997;83(1):291–296. doi: 10.1152/jappl.1997.83.1.291. [DOI] [PubMed] [Google Scholar]
- 25.Harper CJ, Shahgholi L, Cieslak K, Hellyer NJ, Strommen Ja, Boon AJ. Variability in diaphragm motion during normal breathing, assessed with B-mode ultrasound. J Orthop Sports Phys Ther. 2013;43(12):927–931. doi: 10.2519/jospt.2013.4931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sæverud HA, Falk RS, Dowrick A, Eriksen M, Aarrestad S, Skjønsberg OH. Measuring diaphragm movement and respiratory frequency using a novel ultrasound device in healthy volunteers. J Ultrasound. 2019 doi: 10.1007/s40477-019-00412-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goligher EC, Laghi F, Detsky ME, Farias P, Murray A, Brace D, Brochard LJ, Sebastien-Bolz S, Rubenfeld GD, Kavanagh BP, et al. Measuring diaphragm thickness with ultrasound in mechanically ventilated patients: feasibility, reproducibility and validity. Intensiv Care Med. 2015;41(4):642–649. doi: 10.1007/s00134-015-3687-3. [DOI] [PubMed] [Google Scholar]
- 28.Boon AJ, Harper CJ, Ghahfarokhi LS, Strommen Ja, Watson JC, Sorenson EJ. Two-dimensional ultrasound imaging of the diaphragm: quantitative values in normal subjects. Muscle Nerve. 2013;47(6):884–889. doi: 10.1002/mus.23702. [DOI] [PubMed] [Google Scholar]
- 29.Ranieri G, Luigi M, Belsito F, Rocco M, Blasi RAD. Propofol sedation reduces contraction and motion of diaphragm in humans: preliminary results. Crit Care. 2015;19(Suppl 1):P481–P481. doi: 10.1186/cc14561. [DOI] [Google Scholar]
- 30.Grams ST, von Saltiél R, Mayer AF, Schivinski CIS, de Nobre SLF, Nóbrega IS, Jacomino MEMLP, Paulin E. Assessment of the reproducibility of the indirect ultrasound method of measuring diaphragm mobility. Clin Physiol Funct Imaging. 2014;34(1):18–25. doi: 10.1111/cpf.12058. [DOI] [PubMed] [Google Scholar]
- 31.Arbelot C, Dexheimer Neto FL, Gao Y, Brisson H, Chunyao W, Lv J, Valente Barbas CS, Perbet S, Prior Caltabellotta F, Gay F, et al. Lung ultrasound in emergency and critically ill patients: number of supervised exams to reach basic competence. Anesthesiology. 2020;132(4):899–907. doi: 10.1097/ALN.0000000000003096. [DOI] [PubMed] [Google Scholar]