Abstract
We present a 1-year-old boy who was asymptomatic and brought to the emergency room on suspicion of his having swallowed a pin. Confirmation of ingestion of the pin and its passage through the gut was achieved with abdominal radiography. The pin, which was followed with serial abdominal radiographs, was expected to leave the gastrointestinal tract, but was fixed to the right lower quadrant. When the pin had not passed after 10 days, and with increasing concern about the likelihood of perforation, ultrasonography was used to locate its exact position and allow surgical removal. Only a few cases involving the use of ultrasonography to reveal the exact location of an ingested foreign body prior to surgery have been reported ın the literature. This case presents an impressive example of the use of ultrasonography to reveal the intra-appendiceal location of an ingested foreign body, and to facilitate its surgical removal.
Electronic supplementary material
The online version of this article (10.1007/s40477-020-00431-4) contains supplementary material, which is available to authorized users.
Keywords: Foreign body, Ultrasound, Appendicitis, Ingestion
Introduction
Foreign-body ingestion is a common problem encountered in the pediatric age group. A variety of objects are reported to be lodged in the appendix. The most commonly reported foreign bodies are shots, bones, seeds, needles, stones, bullets, airgun pellets, pins, screws and buckshots [1]. Ingested foreign bodies generally do not cause any complications, and pass through the gastrointestinal tract spontaneously within a week. Their presence within the appendix is a very rare event [1, 2]. Ingested foreign bodies may remain immobile in the appendix without stimulating an inflammatory reaction for extended periods [3]. The clinical presentation can vary from hours to years. Complications usually depend on the size and shape of the foreign bodies. The prevalence of appendicitis due to foreign bodies is approximately 0.0005% [4].
Case report
A 1-year-old boy who was asymptomatic was brought to the emergency room on suspicion of his having swallowed a pin. Physical examination revealed that the abdomen was soft, with normal bowel sounds. The patient’s laboratory work-up was normal, and he was afebrile. Upon abdominal X-ray, a pin was found in the right lower quadrant (Fig. 1). The pin, which was followed with serial abdominal radiographs, was expected to leave the gastrointestinal tract, but was fixed to the right lower quadrant. When the pin had not passed after 10 days, and with increasing concern about the likelihood of perforation, ultrasonography was used to locate its exact position and to allow surgical removal. Abdominal ultrasonography was performed using a graded compression technique to determine the precise location of the appendix in the right lower quadrant. The sonographic examination was performed using a Hitachi HI Vision Preirus ultrasound scanner, with a 5–10 MHz linear array transducer. In the scan, the appendix appeared normal, with no signs of acute appendicitis. The pin was sonographically detected in the normal appendix (Figs. 2, 3). The pin was shown to lie with its head near the appendiceal tip. The appendix diameter was measured at 4.2 mm. No hyperemia was observed on the Doppler study, and there was no evidence of any periappendiceal fluid or adjacent inflammatory response to suggest perforation. As a result of the ultrasonographic findings, open appendicectomy was decided. Signs of inflammation, indicating acute appendicitis, were not detected during the operation (Fig. 4). The periappendiceal areas were clear. However, there was evidence of a new perforation from the tip of the pin in the middle of the appendix. There were no postoperative complications, and the patient was discharged 1 day after surgery. Histopathological examination of the specimen revealed a normal appendix without signs of inflammation.
Fig. 1.
The serial radiographs show a pin in the region of the right iliac fossa
Fig. 2.
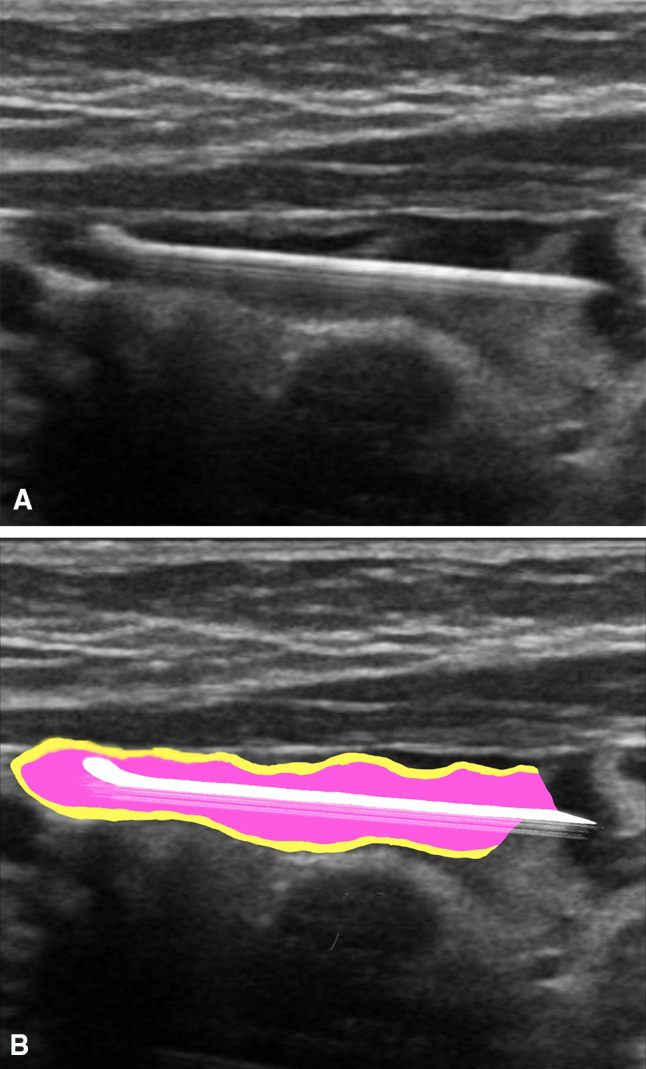
Longitudinal views. a The ultrasound scan of the appendix demonstrates the intraluminal position of the pin, with its head against the tip of the appendix. b The radiological illustration of the same image
Fig. 3.
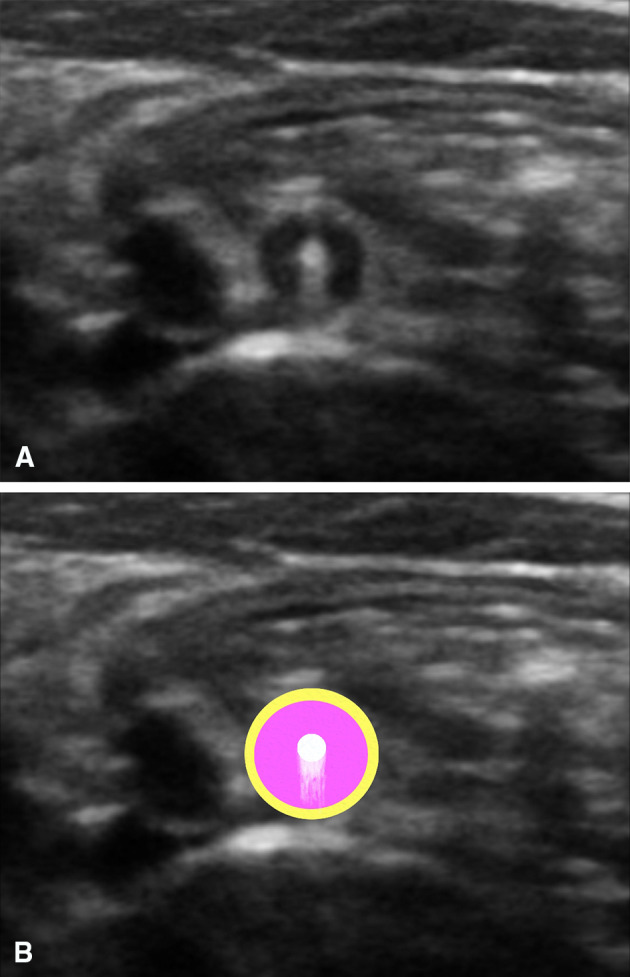
Transverse views. a The ultrasound scan of the appendix demonstrates the intraluminal position of the pin. b The radiological illustration of the same image
Fig. 4.

The intraoperative picture shows the tip of the pin extending outward from the normal appendix
Discussion
Close monitoring of children ingesting foreign bodies is important for minimizing morbidity. Children should be followed up by physical examination and serial abdominal X-rays, the family should be informed about the signs of acute abdomen and they should be called to routine outpatient controls. Even if an ingested foreign object is a pointed one, such as a needle, it often leaves the gastrointestinal tract without any problems [3]. Due to the risk of perforation, if there is no spontaneous drainage of the foreign body, an appendectomy is necessary to remove it [2].
Impaction of ingested foreign bodies inside the lumen of the appendix is a very rare finding, and only a small number of cases have been reported worldwide. This condition is called foreign-body appendicitis. Computed tomography or X-ray is often used to confirm the diagnosis. The use of ultrasonography is not common. However, it is known that ultrasound scanning of the gastrointestinal tract is a necessary tool for the diagnosis of acute gastrointestinal pathologies in the pediatric age group [5]. The use of radiography to detect and monitor foreign bodies in children is well documented. However, it is not always easy to determine the exact location of a foreign body by X-ray, as that can only show the presence of a foreign body in the right lower quadrant and not in the terminal ileum, cecum, or appendix. Plain radiography does not reliably show whether the object is in the intestinal lumen or whether it has passed through the intestinal wall to reach the peritoneal cavity. In this case, ultrasonography can help to confirm the location of the foreign body and to avoid unnecessary intervention. A foreign body is usually shown on ultrasonography as a hyperechoic interface with an accompanying acoustic shadow. The use of preoperative ultrasonography to localize the location of an ingested foreign body, and the determination of a foreign body within in the appendix using ultrasound was first reported by Piotto et al. [6].
Ultrasonography should be considered to determine the exact location of an ingested foreign body preoperatively, especially in pediatric patients, since it does not contain radiation and obtains more data for localization than X-ray. It should not be forgotten that ultrasonography may be a key diagnostic tool for the detection of foreign bodies in the abdomen, especially in children. In the problem-solving stage, it should always be noted as the modality to be chosen, given that—as this case demonstrates—it can be quite effective in experienced hands.
A small number of cases involving the use of ultrasonography to reveal the exact location of an ingested foreign body prior to surgery have been reported in the literature. This case report presents an impressive example of the use of ultrasonography to reveal the intra-appendiceal location of an ingested foreign body, and to facilitate its surgical removal.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Movie. 1 Longitudinal view of the appendix demonstrates the intraluminal position of the pin, with its head against the tip of the appendix (MP4 1156 kb)
Movie. 2 Transverse view of the appendix demonstrates the intraluminal position of the pin (MP4 1066 kb)
Compliance wıth ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Human or animals participant statement
This article does not contain any studies with human participants or animals performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Song YS, Covarrubias DA, Nardi PM. Foreign body appendicitis. AJR Am J Roentgenol. 2009;193:154–155. doi: 10.2214/AJR.08.2148. [DOI] [PubMed] [Google Scholar]
- 2.Benizri EI, Cohen C, Bereder JM, Rahili A, Benchimol D. Swallowing a safety pin: report of a case. World J Gastrointest Surg. 2012;4:20–22. doi: 10.4240/wjgs.v4.i1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yalçın S, Karnak I, Çiftci AO, et al. Foreign body ingestion in children: an analysis pediatric surgical practice. Pediatr Surg Int. 2007;23:755–761. doi: 10.1007/s00383-007-1958-y. [DOI] [PubMed] [Google Scholar]
- 4.Simkovic D, Hladík P, Lochman P. Unusual cause of the acute appendicitis. Rozhl Chir. 2004;83:365–367. [PubMed] [Google Scholar]
- 5.Esposito F, Di Serafino M, Mercogliano C, Ferrara D, Vezzali N, Di Nardo G, Martemucci L, Vallone G, Zeccolini M. The pediatric gastrointestinal tract: ultrasound findings in acute diseases. J Ultrasound. 2019;22:409–422. doi: 10.1007/s40477-018-00355-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Piotto L, Gent R, Kirby CP, Morris LL. Preoperative use of ultrasonography to localize an ingested foreign body. Pediatr Radiol. 2009;39:299–301. doi: 10.1007/s00247-008-1096-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Movie. 1 Longitudinal view of the appendix demonstrates the intraluminal position of the pin, with its head against the tip of the appendix (MP4 1156 kb)
Movie. 2 Transverse view of the appendix demonstrates the intraluminal position of the pin (MP4 1066 kb)



