Abstract
Objective
Evaluate tolerability and effectiveness of golimumab-IV versus infliximab in patients with rheumatoid arthritis (RA) in a real-world setting.
Methods
AWARE, a prospective, real-world, pragmatic, observational, multicenter, phase 4 study, enrolled RA patients when initiating golimumab-IV or infliximab. Treatment decisions were made by the treating rheumatologist. The approved doses for RA are 2 mg/kg at weeks 0, 4, then Q8W for golimumab-IV and 3 mg/kg at weeks 0, 2, 6, then Q8W (dose escalation permitted) for infliximab. A prespecified formal interim analysis was conducted. The primary endpoint was the incidence of infusion reactions (any adverse event that occurred during or within 1 h of infusion) through week 52. Major secondary endpoints were mean change from baseline in CDAI at months 6 and 12 in biologic-naïve patients (non-inferiority margin in the CDAI = 6). Baseline characteristics were adjusted using propensity scores with inverse probability of treatment weights (IPTW).
Results
In the formal interim analysis (golimumab-IV, n = 479; infliximab, n = 354), the incidence of infusion reactions was significantly lower with golimumab-IV vs. infliximab (3.6 vs. 17.6%, p < 0.001, IPTW-adjusted). Among biologic-naïve patients, mean changes from baseline in CDAI at month 6 (– 9.5 golimumab-IV vs. − 10.1 infliximab) and at month 12 (− 9.4 golimumab-IV vs. − 10.1 infliximab) demonstrated non-inferiority.
Conclusions
The proportion of patients with an infusion reaction was significantly lower with golimumab-IV vs. infliximab. Among biologic-naïve patients, mean change from baseline in CDAI at months 6 and 12 was non-inferior for golimumab-IV vs. infliximab. Compared with fixed-dose golimumab-IV, infliximab dose escalation did not provide any greater improvements in CDAI for patients with RA.
Trial Registration
ClinicalTrials.gov identifier, NCT02728934.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40744-021-00354-4.
Keywords: Intravenous golimumab, Infliximab, Infusion reaction, Clinical disease activity index, Real-world evidence
Key Summary Points
| Why carry out this study? |
| Golimumab and infliximab are both approved as intravenous (IV) therapies for patients with rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis; however, while golimumab-IV is approved at a fixed dose of 2 mg/kg, infliximab dosing in rheumatoid arthritis can range from 3 to 10 mg/kg. |
| This study provides real-world, comparative data for safety and effectiveness of golimumab-IV and infliximab in patients with rheumatoid arthritis. |
| What has been learned from this study? |
| Infusion reactions were less common in golimumab-IV-treated patients through week 52 when compared with infliximab-treated patients. |
| The effectiveness of golimumab-IV (as assessed using the Clinical Disease Activity Index) at 6 and 12 months from baseline was non-inferior to infliximab among biologic-naïve patients. |
| Dose escalation with infliximab did not provide any additional benefit with respect to clinical effectiveness when compared with golimumab-IV at stable doses of 2 mg/kg. |
Introduction
Golimumab [1] and infliximab [2] are intravenously administered, monoclonal antibody (mAb), tumor necrosis factor inhibitors (TNFi) approved to treat patients with moderate-to-severe rheumatoid arthritis (RA) in conjunction with methotrexate. In contrast to infliximab, which is a chimeric mAb given over 2 h every 8 weeks following initial doses (3 mg/kg) at weeks 0, 2, and 6, and allows for dose escalation [2], intravenous (IV) golimumab is fully human, infused over 30 min, and administered at a fixed dose of 2 mg/kg every 8 weeks after initial doses at week 0 and week 4.
The safety and efficacy of golimumab-IV and infliximab in RA patients have been well characterized in several reports [3–8]. While golimumab-IV and infliximab have similar efficacy in RA patients, based on non-head-to-head phase 3 trials, the therapies differ with respect to the reported incidence of certain adverse reactions [5, 7]. In the absence of a prospective, randomized, double-blind active-comparator trial for these therapies, a real-world comparative assessment can provide valuable information on effectiveness and safety for clinicians and patients [9]. The AWARE study (Comparative and Pragmatic Study of Simponi Aria [golimumab-IV] versus Remicade [infliximab] in Rheumatoid Arthritis) was designed to assess safety, with an emphasis on infusion reactions, and effectiveness, using the Clinical Disease Activity Index (CDAI) [10], in a real-world setting. Consistent with the intent to mirror routine practice, physicians were guided by the approved prescribing information, with no protocol-specific dose or dosing frequency of golimumab-IV or infliximab. AWARE also explored the relative effectiveness between fixed-dose golimumab-IV versus dose escalation of infliximab.
Methods
Study Design and Patients
AWARE (NCT02728934) was a prospective study of golimumab-IV versus infliximab in RA patients in the US. Treatment was not randomized, and once the treating rheumatologist prescribed either golimumab-IV or infliximab, independent of the patient’s study participation, eligible patients were enrolled when initiating treatment. The study intended to enroll ~ 30–40% biologic-naïve patients in each treatment group. The protocol did not restrict or introduce any concomitant medical interventions or medications, and the sponsor did not provide any therapeutic interventions. Treatment decisions, including prescribed medications, dose and dosing intervals, were at the discretion of the rheumatologist. Patient visits (and corresponding data collection) occurred according to usual clinical practice, but outcomes were consistently collected at month 6 and month 12 of treatment.
Eligible patients were adults (≥ 18 years) with a confirmed diagnosis of RA who were medically eligible for treatment with golimumab-IV or infliximab in accordance with the approved product labeling (e.g., tuberculosis screening, vaccinations, etc.). At enrollment, eligible patients had to have been prescribed, but never previously received, treatment with golimumab-IV (if initiating golimumab-IV) or infliximab (if initiating infliximab). Golimumab-IV is administered at a dose of 2 mg/kg, over 30 min, at week 0, week 4, and every 8 weeks thereafter. Infliximab is administered at a dose of 3 mg/kg, over 120 min, at week 0, week 2, week 6, and every 8 weeks thereafter. Per the approved label, infliximab dosage may be increased up to 10 mg/kg or administered as often as every 4 weeks. Previous therapy with biologics, disease-modifying anti-rheumatic drugs, and other RA-related treatments was permitted; concurrent disease-modifying anti-rheumatic drugs were also permitted. Patients were excluded if they were pregnant or planning a pregnancy or enrolled in an interventional study. Patients were also excluded if they received an investigational drug or used an invasive investigational medical device within 28 days before the planned first dose of golimumab-IV or infliximab. After study initiation, the US Food and Drug Administration approved an infliximab biosimilar; the study protocol was subsequently amended to allow enrollment of patients receiving biosimilar infliximab.
Adverse events (AEs) were documented throughout the study and are summarized through week 52. AEs of special interest included tuberculosis, opportunistic infections, serious infections, and malignancies. Clinical effectiveness was assessed using the CDAI at baseline and months 3, 6, and 12; disease activity was categorized as high disease activity (CDAI > 22), moderate disease activity (CDAI > 10 and ≤ 22), low disease activity (CDAI > 2.8 and ≤ 10), or remission (CDAI ≤ 2.8).
This study was conducted according to the Declaration of Helsinki and the International Committee on Harmonisation good clinical practices. The protocol was reviewed and approved by the overseeing institutional review board (Copernicus Group, Approval QUI1-15-645). All patients provided written informed consent.
Outcomes
The primary endpoint was the proportion of patients with an infusion reaction through week 52. Infusion reactions were defined as any AE that occurred during an infusion or within 1 h after the infusion. Major secondary endpoints were the change from baseline in the CDAI at month 6 and month 12 among biologic-naïve patients to evaluate real-world effectiveness in a patient population similar to that in the phase 3, registrational, GO FURTHER study [7].
Statistical Analysis
AWARE was planned as a 3-year study but was closed after 2 years when sufficient numbers of patients had been treated through week 52 and it was determined that the primary and major secondary endpoints were achieved. A formal, pre-planned interim analysis of the primary and major secondary endpoints was planned when approximately 50% of the patients completed week 52 or permanently discontinued the trial (Interim Analysis Set [IAS]). In the formal interim analysis, an overall hierarchical procedure was employed to control overall type 1 error rate, α, at 0.05 using α-spending functions. With 66% of patients included in the IAS, a p value < 0.0179 was required to achieve statistical significance. The analysis plan also prespecified that achievement of the primary and major secondary endpoints in the formal interim analysis would preclude further comparative statistical assessments between golimumab-IV and infliximab. Analyses conducted for the IAS were repeated for the Full Analysis Set (FAS) that included all enrolled patients who received ≥ 1 golimumab-IV or infliximab administration.
The primary endpoint analysis was a test of superiority of golimumab-IV compared with infliximab for the frequency of infusion reactions through week 52. The major secondary endpoint analysis (CDAI change from baseline at month 6 and month 12 in biologic-naïve patients) used hierarchical procedures and tested the non-inferiority of golimumab-IV compared with infliximab with a non-inferiority margin in the CDAI of 6 [11]. To maintain the overall type 1 error rate at α = 0.05 for the formal interim analysis, a more conservative confidence interval (96.42%) was used based on the α-spending function.
As patients were not randomized to treatment, post hoc analyses were undertaken to compare baseline characteristics between treatment cohorts; nominal p values were determined using analysis of covariance [ANCOVA] with van der Waerden rank test or Chi-square test. To account for imbalances in patient characteristics, all endpoints were adjusted via a propensity score weighted analysis using inverse probability of treatment weights (IPTW). The propensity score is an estimate of the probability of receiving golimumab-IV versus receiving infliximab, given the observed pretreatment baseline covariates. The propensity scores were estimated using logistic regression and included baseline covariates of age, sex, race, region, body mass index (BMI), weight, disease duration, CDAI, biologic-naïve, other medications, number of prior biologics received, prior TNFi therapy (yes/no), selected comorbidities, and smoking status. Standardized mean differences (SMDs) > 0.10 [12] were used to identify imbalances at baseline. A Chi-square test, adjusted for IPTW weighting, was performed to compare the proportion of patients with an infusion reaction.
CDAI scores and change in CDAI scores over time were summarized using descriptive statistics. Least square (LS) means, LS mean difference between treatment groups, and CDAI change from baseline were estimated using ANCOVA, adjusting for propensity scores and baseline CDAI. Missing CDAI values for month 6 and month 12 were imputed using Last Observation Carried Forward, and for patients who discontinued due to lack of efficacy, baseline values were assigned from the point of treatment failure onward. CDAI values were imputed for seven patients (golimumab-IV, n = 3; infliximab, n = 4) at baseline, 316 patients (golimumab-IV, n = 176; infliximab, n = 140) at month 6, and 547 patients (golimumab-IV, n = 312; infliximab, n = 235) at month 12.
Dose Escalation
The prescribed doses of golimumab-IV or infliximab were recorded at each infusion. Among infliximab patients, a normalized dose was calculated to assess the effect of potential changes in prescribed dose or contraction of the dosing interval. Dose escalation was defined as having ≥ 1 post-baseline normalized dose that was greater than the baseline dose. At baseline, the normalized dose was the prescribed dose. After baseline, the normalized dose was adjusted by the actual time interval from the previous visit as follows: Normalized dose = prescribed dose × (scheduled time interval [weeks])/(actual time interval [weeks]), where the scheduled time interval was 2 (infusion visit 2), 4 (infusion visit 3), then every 8 weeks (from infusion visit 4 onwards) and the actual time interval was (infusion visit date-previous infusion visit date)/7. Change from baseline in CDAI scores (using imputed and observed data) at months 6 and 12 were determined for patients who did and did not dose escalate.
Results
Patient Demographics and Disease Characteristics
The study was conducted at 88 US sites; data for this report were collected between February 25, 2016 and February 1, 2019. A total of 1270 patients (FAS) were enrolled and received golimumab-IV (n = 685) or infliximab (n = 585). Although generally well-balanced between the treatment groups, the treatment cohort differed in several baseline demographic and disease characteristics. Higher proportions of patients in the golimumab-IV than infliximab group were female (85 vs. 80%) and received prior biologic therapy (65 vs. 51%); patients in the golimumab-IV group were also older (61 vs. 58 years), had a slightly lower mean BMI (31 vs. 32 kg/m2), and had a longer mean duration of RA (9 vs. 7 years) compared with the infliximab group. Patients who previously received ≥ 3 biologic therapies comprised 20% of patients in the golimumab-IV group, compared with 11% in the infliximab group (Table 1). Twelve patients received ≥ 1 infusion of an infliximab biosimilar.
Table 1.
Baseline demographics and disease characteristics
| Characteristic | Golimumab-IV | Infliximab |
|---|---|---|
| Patients, n | 685 | 585 |
| Age, years | 60.9 ± 13.4 | 58.0 ± 12.9* |
| Female | 582 (85.0) | 465 (79.5)* |
| Race | ||
| White | 599 (87.4) | 496 (84.8) |
| Black/African American | 59 (8.6) | 57 (9.7) |
| Other/unknown | 27 (3.9) | 32 (5.5) |
| Disease duration, years | 9.2 ± 10.0 | 7.3 ± 9.7* |
| Weight, kg | 83.0 ± 22.9 | 86.6 ± 23.5* |
| BMI, kg/m2 | 30.7 ± 8.0 | 31.7 ± 8.2* |
| MTX use | 420 (61.3) | 356 (60.9) |
| Dose, mga | 16.4 ± 6.3 | 16.5 ± 7.2 |
| CDAI | 31.5 ± 15.2 | 33.2 ± 16.0 |
| Biologic-naïve | 242 (35.3) | 251 (42.9)* |
| Biologic-experienced | 443 (64.7) | 334 (57.1)* |
| 1 prior biologic | 198 (28.9) | 184 (31.5) |
| 2 prior biologics | 107 (15.6) | 87 (14.9) |
| 3 + prior biologics | 138 (20.1) | 63 (10.8) |
Data presented as mean ± standard deviation or n (%) unless otherwise noted
BMI body mass index, CDAI clinical disease activity index, IV intravenous, MTX methotrexate
*Nominal p < 0.05
aMean MTX dose at baseline calculations included patients with available data (golimumab-IV, n = 378; infliximab, n = 330)
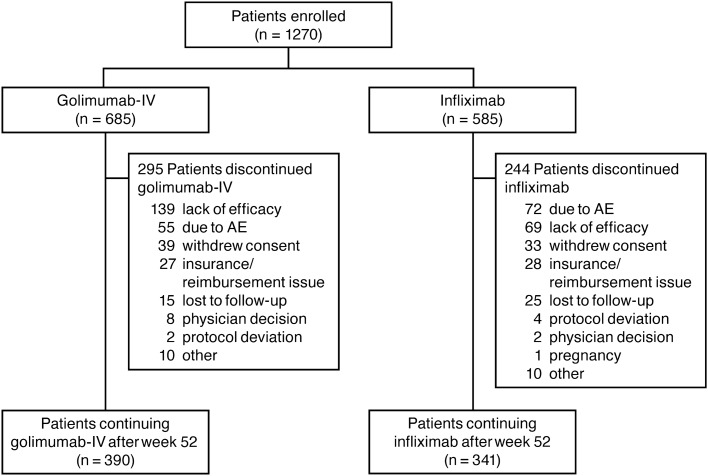
Of patients included in the FAS, 43% who received golimumab-IV and 42% who received infliximab discontinued the study, with the most common reasons being lack of efficacy (golimumab-IV, 20%; infliximab, 12%) and AEs (golimumab-IV, 8%; infliximab, 12%) (Fig. 1). Seven (1%) patients in the golimumab-IV group and 26 (4%) in the infliximab group discontinued due to an infusion reaction. Infusion reactions accounted for 13% of golimumab-IV AEs and 36% of infliximab AEs that led to discontinuation.
Fig. 1.
Patient disposition through week 52. AE adverse event, IV intravenous
Infusion Reactions
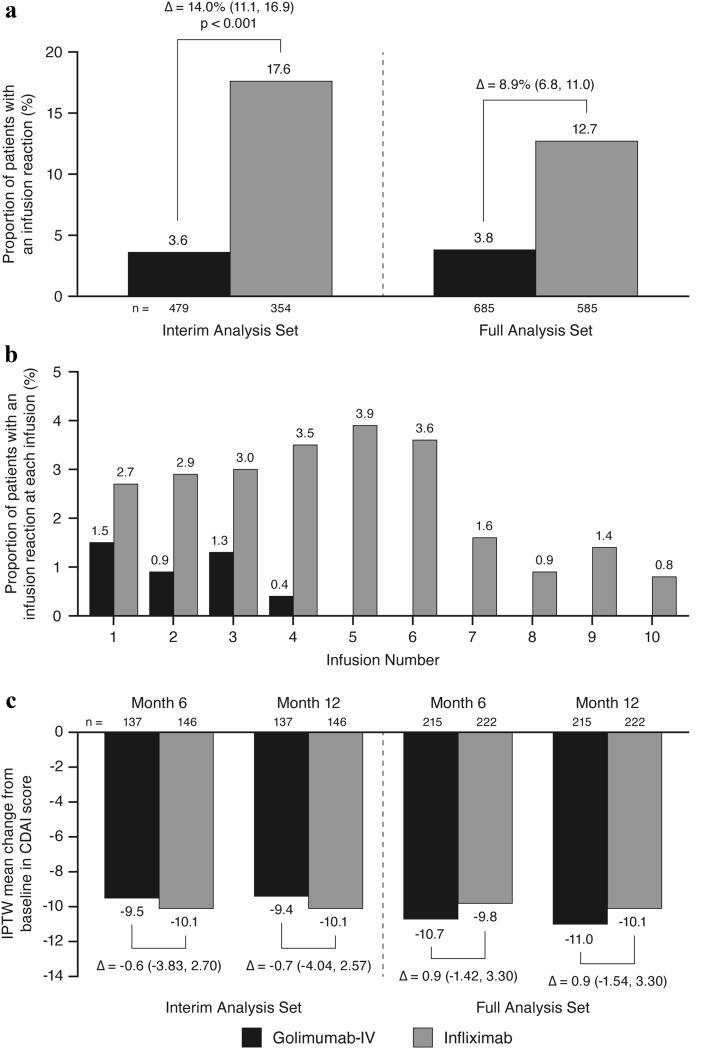
The formal interim analysis was conducted in February 2018, after 833 patients had completed 52 weeks of treatment or discontinued. The demographic and baseline disease characteristics of the patients included in the IAS were similar to the FAS (data not shown). In the IAS, the proportion of patients who experienced an infusion reaction was significantly lower in the golimumab-IV group compared with infliximab (4 vs. 18%; p < 0.001; difference [95% confidence interval (CI)] = 14.0 [11.1, 16.9]; Fig. 2a). In the FAS, including all enrolled patients (n = 1270) who completed week-52 assessments or discontinued the study, the incidence of infusion reactions was 4% in the golimumab-IV group and 13% in the infliximab group (difference [95% CI] = 8.9 [6.8, 11.0]; Fig. 2a).
Fig. 2.
The IPTW-adjusted proportion of patients with an infusion reaction through week 52 (a); the IPTW-adjusted proportion of patients with an infusion reaction at each infusion (b); and CDAI and IPTW-adjusted mean change in CDAI score among biologic-naïve patients at month 6 and month 12 (c). In panel c, the mean change from baseline in CDAI is based on ANCOVA after adjusting for both baseline CDAI and IPTW propensity score. ANCOVA analysis of covariance, CDAI Clinical Disease Activity Index, IPTW inverse probability of treatment weighted, IV intravenous
In the FAS, infusion reactions associated with golimumab-IV mainly occurred during the first four infusions, while those seen in infliximab-treated patients were reported by ≥ 1 patient during each of the first 10 infusions (Fig. 2b). Pre-infusion medication was used in 31% of golimumab-IV patients versus 84% of infliximab patients. Among patients in the FAS who experienced an infusion reaction, medication to treat the infusion reaction was administered for 54% of patients receiving golimumab-IV and 76% receiving infliximab.
Clinical Effectiveness
Prior to IPTW adjustment, 13 covariates (age, region, BMI, weight, disease duration, baseline CDAI, proportion of patients who were biologic-naïve, number of prior biologics, prior TNFi use, prior non-TNFi use, prednisone use, history of diabetes, and history of hyperlipidemia) exhibited SMDs > 0.10 [12] (range, 0.104–0.321). Following IPTW, all SMDs were < 0.10 (data not shown).
In the formal interim analysis, the mean changes in CDAI score (biologic-naïve patients only) at month 6 were − 9.5 in the golimumab-IV group and − 10.1 in the infliximab group (difference [96.42% CI]: − 0.6 [− 3.8, 2.7]) and at month 12 were − 9.4 and − 10.1, respectively (difference [96.42% CI]: – 0.7 [− 4.0, 2.6]; Fig. 2c). As the lower limit of the CIs at month 6 (– 3.8) and month 12 (– 4.0) were within the pre-defined non-inferiority margin of 6, the change from baseline in CDAI among golimumab-IV patients was considered non-inferior to that in infliximab patients at both months 6 and 12 (Fig. 2c).
For biologic-naive patients in the FAS, the mean changes from baseline in CDAI score at month 6 were – 10.7 in the golimumab-IV group and – 9.8 in the infliximab group (difference [95% CI]: 0.9 [– 1.4, 3.3]) and at month 12 were – 11.0 and – 10.1, respectively (difference [95% CI]: 0.9 [– 1.5, 3.3]; Fig. 2c). The shifts in categorical CDAI score (high disease activity, moderate disease activity, low disease activity, or remission) of biologic-naïve patients treated with golimumab-IV or infliximab after 3, 6, and 12 months of treatment are shown in Supplemental Table 1. The proportions of patients with high disease activity at baseline and months 3, 6, and 12 were 67%, 43%, 37%, and 35%, respectively, in the golimumab-IV group and 67%, 46%, 37%, and 37%, respectively, in the infliximab group.
Dose Escalation
By the 5th infusion of infliximab, 5% of patients had been prescribed ≥ 1 dose of 8 mg/kg or greater; the proportion of patients who received ≥ 1 dose of infliximab ≥ 8 mg/kg increased at each subsequent infusion and was 13% at the 9th infusion and 15% at the 10th infusion. When accounting for both prescribed dose and dosing interval (the normalized dose), 76% of infliximab patients were dose-escalated. In these patients, the mean infliximab dose increased at each infusion, with biologic-experienced patients having numerically greater increases than biologic-naïve patients (Supplemental Table 2). The effect of infliximab dose escalation (normalized dose) on CDAI using imputed data comparing golimumab-IV with dose-escalated and non-dose-escalated infliximab patients is shown in Table 2. The mean baseline CDAI (IPTW-adjusted) was similar among the three groups of biologic-naïve and biologic-experienced patients. The magnitude of change in CDAI between golimumab-IV patients and dose escalated infliximab patients was similar at both month 6 and month 12, independent of prior biologic therapy (Table 2). In the infliximab group, mean changes in CDAI at month 6 and month 12 were numerically smaller in the non-dose escalated patients than in the dose-escalated patients, regardless of prior biologic exposure. Similar patterns were seen with observed data, but with higher mean changes in CDAI (Supplemental Table 3).
Table 2.
Mean CDAI scoresa and mean change from baselinea (missing data imputed using LOCF) through month 12 for golimumab-IV, dose-escalated infliximabb, and non-dose-escalated infliximab among patients who were biologic-naïve or biologic-experienced
| Biologic-naïve patientsc | Biologic-experienced patients | |||||||
|---|---|---|---|---|---|---|---|---|
| Golimumab-IV | Dose-escalated infliximab | Non-dose-escalated infliximab | Combined infliximab | Golimumab-IV | Dose-escalated infliximab | Non-dose-escalated infliximab | Combined infliximab | |
| Patients, N | 215 | 172 | 50 | 222 | 398 | 234 | 53 | 287 |
| Baseline | ||||||||
| Score | 30.7 ± 21.3 | 30.7 ± 20.7 | 28.7 ± 21.8 | 30.3 ± 20.9 | 33.1 ± 20.6 | 34.3 ± 24.7 | 29.7 ± 20.2 | 33.5 ± 24.0 |
| Month 6 | ||||||||
| Score | 19.9 ± 23.6 | 20.3 ± 21.6 | 21.3 ± 23.1 | 20.6 ± 21.9 | 22.8 ± 21.0 | 25.7 ± 25.4 | 23.4 ± 24.2 | 25.3 ± 25.2 |
| Change from baseline | – 10.8 ± 19.8 | – 10.4 ± 18.9 | – 7.4 ± 15.2 | – 9.7 ± 18.2 | – 10.3 ± 18.8 | – 8.6 ± 21.7 | – 6.3 ± 18.4 | – 8.2 ± 21.1 |
| Month 12 | ||||||||
| Score | 19.7 ± 23.2 | 20.1 ± 21.7 | 20.8 ± 23.6 | 20.2 ± 22.1 | 22.1 ± 21.6 | 25.0 ± 25.6 | 23.0 ± 23.6 | 24.7 ± 25.2 |
| Change from baseline | – 11.1 ± 19.8 | – 10.7 ± 20.2 | – 7.9 ± 17.4 | – 10.0 ± 19.6 | – 11.0 ± 18.4 | – 9.3 ± 21.6 | – 6.7 ± 18.0 | – 8.9 ± 21.0 |
Data are presented as mean ± standard deviation
aInverse probability of treatment weighted (IPTW)-adjusted
bDose-escalated: Any patient with at least one normalized prescribed dose > baseline dose
cPopulation included in major secondary endpoint analysis
CDAI clinical disease activity index, IV intravenous, LOCF last observation carried forward
Safety
Through week 52, 51% of patients in the golimumab-IV group and 61% of patients in the infliximab group had ≥ 1 AE (Table 3). AEs in the system organ class of Infections and Infestations were the most common (golimumab-IV, 23%; infliximab, 26%). Serious AEs were reported for 10% of golimumab-IV patients and 10% of infliximab patients through week 52; most were singular events. Serious infections occurred in approximately 3% of patients in each treatment group. One case of latent tuberculosis (positive T-SPOT test with a negative chest radiograph) was reported; the non-serious AE occurred in a patient in the infliximab group (white female, aged 56 years). The AE was reported on study day 1, and the patient was treated with isoniazid and continued study treatment (through week 52). Opportunistic infections occurred in 1.5% of patients in each group.
Table 3.
Adverse events through week 52
| Golimumab-IV | Infliximab | |
|---|---|---|
| Patients, N | 685 | 585 |
| Mean follow-up, weeks | 41.3 | 41.3 |
| Patients with ≥ 1 AE | 348 (50.8) | 356 (60.9) |
| Patients with ≥ 1 serious AE | 66 (9.6) | 60 (10.3) |
| Patients with ≥ 1 infection or infestation | 156 (22.8) | 155 (26.5) |
| Patients with ≥ 1 opportunistic infection | 10 (1.5) | 9 (1.5) |
| Patients with ≥ 1 serious infection | 21 (3.1) | 20 (3.4) |
| Patients with ≥ 1 malignancy | 13 (1.9) | 10 (1.7) |
| Latent tuberculosis | 0 | 1 (0.2) |
| Most common AEs (occurring in ≥ 5% of either regimen) | ||
| Nausea | 20 (2.9) | 38 (6.5) |
| Worsening of rheumatoid arthritis | 23 (3.4) | 32 (5.5) |
| Upper respiratory tract infection | 28 (4.1) | 30 (5.1) |
| Pruritus | 10 (1.5) | 30 (5.1) |
Data presented as n (%) unless otherwise noted
AE adverse event, IV intravenous
Twenty-three patients had a malignancy, including melanoma and non-melanoma skin cancer and leukemia, through week 52, with similar incidence for golimumab-IV (n = 13 [1.9%]) and infliximab (n = 10 [1.7%]). Ten patients died through week 52: six in the golimumab-IV group (motor vehicle accident, congestive heart failure, acute respiratory failure, septic shock, stage 4 lung cancer, and one death of unknown cause) and four in the infliximab group (congestive heart failure, worsening pulmonary fibrosis, cardiac arrest, and possible aspiration pneumonia).
Discussion
The AWARE study is the first prospective, head-to-head pragmatic comparative study of golimumab-IV versus infliximab in RA patients. The primary endpoint, i.e., test of superiority of golimumab-IV compared with infliximab for the frequency of infusion reactions through week 52, utilized the same criteria to define an infusion reaction previously used in randomized, double-blind phase 3 trials of both therapies [6, 7, 13]. Although a phase 3, placebo-controlled, randomized, double-blind clinical trial remains the FDA-accepted standard for assessing novel drug efficacy and safety, there is growing recognition of the utility of real-world evidence, including regulatory decision-making [14]. It is salient to note that infusion reaction incidence rates are similar to those reported in phase 3 trials of infliximab[6] and golimumab-IV [7], indicating the potential for real-world data from open-label phase 4 studies to provide results near or equivalent to those obtained via a phase 3 trial.
The primary endpoint met statistical significance for superiority in the formal interim analysis, with a lower proportion of patients experiencing an infusion reaction in the golimumab-IV (4%) than in the infliximab (18%) group. Analyses based on the FAS were generally consistent with those using the IAS. Infusion reactions leading to discontinuation or requiring treatment were more common with infliximab than golimumab-IV. Additionally, infusion reactions with golimumab-IV were more likely to occur early in the treatment course, generally limited to the first four infusions, while infliximab infusion reactions continued to occur throughout the 1-year study period.
Analysis of changes in CDAI, the major secondary endpoint, demonstrated that golimumab-IV was non-inferior to infliximab after 6 months and 12 months of treatment in biologic-naïve patients. Discontinuation due to inadequate efficacy occurred more frequently in the golimumab-IV group. However, it should be noted that compared with the infliximab patients, the golimumab-IV patients tended to be older with a longer disease duration and were more likely to be female and to have received prior TNFi therapy; thus these patients were more likely to have recalcitrant disease. The impact of dose escalation (either the prescribed dose or dosing interval) on CDAI was also assessed in biologic-naïve vs. biologic-experienced patients, and in dose-escalated patients through week 52. Overall, 76% of infliximab patients, but no golimumab-IV patient, met the study definition of dose escalation. Despite this, treatment effects were consistent with a fixed dose of golimumab-IV versus frequent dose escalation with infliximab. However, the mean improvement in CDAI observed in this trial was lower than that observed for patients treated with golimumab-IV plus methotrexate in post hoc analyses of GO-FURTHER (change from baseline to week 24 = 20.2 [7]; change from baseline to week 52 = 22.3 [13]). Clinical responses rates such as ACR20 have also been consistent between golimumab-IV and infliximab in separate phase 3 trials [5, 7].
Through week 52, the safety profile was generally comparable across golimumab-IV and infliximab with few exceptions. The incidence of infusion reactions (statistically significant) and AEs was higher in infliximab- than golimumab-IV-treated patients. However, incidences of serious AEs, serious infections, opportunistic infections, malignancy, and death were similar in both treatment groups. The AEs reported during AWARE with either golimumab-IV or infliximab were consistent with the well-established safety profile of TNFi [15].
The results from AWARE are limited by the open-label nature of the study, which could lead to bias in the assessment of infusion reactions or disease activity. Because the patients enrolled in the study were not randomized to treatment groups, there may have been differences between the patients in the two treatment groups affecting the outcomes. Additionally, the discontinuation rate in AWARE was higher than in phase 3 trials; however, statistical methods were employed to mitigate the effect of imbalances between the treatment groups and account for missing data.
Conclusions
Analysis of real-world data generated in this RA study indicated that infliximab was associated with a higher rate of infusion reactions, which more frequently led to treatment discontinuation, when compared with golimumab-IV. The effectiveness of fixed-dose golimumab-IV was comparable to that of infliximab with dose escalation, which occurred in more than three-quarters of these patients. The apparent advantages of golimumab-IV are relevant when considering IV TNFi selection in RA patients.
In addition to the robust, statistically significant primary endpoint and statistically non-inferior major secondary endpoints achieved in AWARE, the study represents an effective, contemporaneous approach to efficiently obtaining meaningful comparative clinical results of approved therapies in patients with RA. This noninterventional real-world approach revealed that dose escalation of infliximab, as permitted by the FDA-approved label, was not associated with greater effectiveness compared with golimumab-IV, for which dose escalation is not an option. This novel finding indicates that RA patients were as effectively treated with non-dose-escalated golimumab-IV as with dose-escalated infliximab, thus allowing golimumab-IV patients to retain a constant dosing regimen. Findings from real-world evidence-based studies such as AWARE may have greater utility to practitioners and patients than those deriving from the more stringently controlled patient populations typically required in phase 3 trials.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank Rebecca E. Clemente, PhD, of Janssen Scientific Affairs, LLC, for editorial support.
Funding
This study and the journal’s Rapid Service Fee were funded by Janssen Scientific Affairs, LLC.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors’ Contributions
Study design: Jeffrey R. Curtis, Shawn Black, Shelly Kafka, Wayne Langholff, Dennis Parenti, Andrew Greenspan, Sergio Schwartzman. Data collection: Jeffrey R. Curtis, Sergio Schwartzman. Data analysis: Stephen Xu, Wayne Langholff. Data interpretation: Jeffrey R. Curtis, Soumya D. Chakravarty, Shawn Black, Shelly Kafka, Stephen Xu, Wayne Langholff, Dennis Parenti, Andrew Greenspan, Sergio Schwartzman. Drafting/revising the manuscript: Jeffrey R. Curtis, Soumya D. Chakravarty, Shawn Black, Shelly Kafka, Stephen Xu, Wayne Langholff, Dennis Parenti, Andrew Greenspan, Sergio Schwartzman.
Disclosures
Jeffrey R. Curtis has received grant/research support from AbbVie, Amgen, Bristol Myers Squibb, Corrona, Eli Lilly, Janssen, Myriad, Pfizer, Regeneron, Roche, and UCB and consulting fees from AbbVie, Amgen, Bristol Myers Squibb, Corrona, Eli Lilly, Janssen, Myriad, Pfizer, Regeneron, Roche, and UCB. Sergio Schwartzman has received speaker fees from AbbVie, Eli Lilly, Janssen, Novartis, Pfizer, Regeneron, Sanofi, and UCB; owns stock in Amgen, Boston Scientific, Gilead, Medtronic, and Pfizer; consulting fees from AbbVie, Eli Lilly, Gilead, Janssen, Myriad, Novartis, Regeneron, Samsung, Sanofi, and UCB; board member at National Psoriasis Foundation; and scientific advisory board at Jubilant, Myriad, and Stelexis. Soumya D. Chakravarty, Shelly Kafka, Dennis Parenti, and Andrew Greenspan are or were employees of Janssen Scientific Affairs, LLC, at the time this work was performed and own stock in Johnson & Johnson, of which Janssen Scientific Affairs, LLC is a wholly owned subsidiary. Shelly Kafka is currently an employee of and owns stock in AbbVie. Shawn Black, Stephen Xu, and Wayne Langholff are employees of Janssen Research & Development, LLC and own stock in Johnson & Johnson, of which Janssen Research & Development, LLC is a wholly owned subsidiary.
Compliance with Ethics Guidelines
This study was conducted according to the Declaration of Helsinki and the International Committee on Harmonisation good clinical practices. The protocol was reviewed and approved by the overseeing institutional review board (Copernicus Group, Approval QUI1-15–645). All patients provided written informed consent.
Data Availability
The data sharing policy of Janssen Pharmaceutical Companies of Johnson & Johnson is available at https://www.janssen.com/clinicaltrials/transparency. As noted on this site, requests for access to the study data can be submitted through Yale Open Data Access Project site at http://yoda.yale.edu.
References
- 1.Simponi ARIA. Package insert. Horsham: Janssen Biotech, Inc.; 2021. [Google Scholar]
- 2.Remicade: Package insert. Horsham, PA: Janssen Biotech, Inc.; 2020.
- 3.Bingham CO, 3rd, Mendelsohn AM, Kim L, et al. Maintenance of clinical and radiographic benefit with intravenous golimumab therapy in patients with active rheumatoid arthritis despite methotrexate therapy: Week-112 efficacy and safety results of the open-label long-term extension of a phase III, double-blind, randomized, placebo-controlled trial. Arthritis Care Res (Hoboken) 2015;67:1627–1636. doi: 10.1002/acr.22556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hsia EC, Ruley KM, Rahman MU. Infliximab (Remicade): from bench to clinical practice. A paradigm shift in rheumatology practice. APLAR J Rheumatol. 2006;9:107–118. doi: 10.1111/j.1479-8077.2006.00185.x. [DOI] [Google Scholar]
- 5.Lipsky PE, van der Heijde DM, St Clair EW, et al. Infliximab and methotrexate in the treatment of rheumatoid arthritis. N Engl J Med. 2000;343:1594–1602. doi: 10.1056/NEJM200011303432202. [DOI] [PubMed] [Google Scholar]
- 6.Maini R, St Clair EW, Breedveld F, et al. Infliximab (chimeric anti-tumour necrosis factor alpha monoclonal antibody) versus placebo in rheumatoid arthritis patients receiving concomitant methotrexate: a randomised phase III trial. Lancet. 1999;354:1932–1939. doi: 10.1016/S0140-6736(99)05246-0. [DOI] [PubMed] [Google Scholar]
- 7.Weinblatt ME, Bingham CO, 3rd, Mendelsohn AM, et al. Intravenous golimumab is effective in patients with active rheumatoid arthritis despite methotrexate therapy with responses as early as week 2: results of the phase 3, randomised, multicentre, double-blind, placebo-controlled GO-FURTHER trial. Ann Rheum Dis. 2013;72:381–389. doi: 10.1136/annrheumdis-2012-201411. [DOI] [PubMed] [Google Scholar]
- 8.Zhuang Y, Xu Z, Frederick B, et al. Golimumab pharmacokinetics after repeated subcutaneous and intravenous administrations in patients with rheumatoid arthritis and the effect of concomitant methotrexate: an open-label, randomized study. Clin Ther. 2012;34:77–90. doi: 10.1016/j.clinthera.2011.11.015. [DOI] [PubMed] [Google Scholar]
- 9.Blonde L, Khunti K, Harris SB, Meizinger C, Skolnik NS. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther. 2018;35:1763–1774. doi: 10.1007/s12325-018-0805-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aletaha D, Nell VPK, Stamm T, et al. Acute phase reactants add little to composite disease activity indices for rheumatoid arthritis: validation of a clinical activity score. Arthritis Res Ther. 2005;7:R796–806. doi: 10.1186/ar1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Curtis JR, Yang S, Chen L, et al. Determining the minimally important difference in the clinical disease activity index for improvement and worsening in early rheumatoid arthritis patients. Arthritis Care Res (Hoboken) 2015;67:1345–1353. doi: 10.1002/acr.22606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Austin PC. A tutorial and case study in propensity score analysis: an application to estimating the effect of in-hospital smoking cessation counseling on mortality. Multivariate Behav Res. 2011;46:119–151. doi: 10.1080/00273171.2011.540480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weinblatt ME, Westhovens R, Mendelsohn AM, et al. Radiographic benefit and maintenance of clinical benefit with intravenous golimumab therapy in patients with active rheumatoid arthritis despite methotrexate therapy: results up to 1 year of the phase 3, randomised, multicentre, double blind, placebo controlled GO-FURTHER trial. Ann Rheum Dis. 2014;73:2152–2159. doi: 10.1136/annrheumdis-2013-203742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baumfeld Andre E, Reynolds R, Caubel P, Azoulay L, Dreyer NA. Trial designs using real-world data: the changing landscape of the regulatory approval process. Pharmacoepidemiol Drug Saf. 2020;29:1201–1212. doi: 10.1002/pds.4932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hernandez MV, Sanmarti R, Canete JD. The safety of tumor necrosis factor-alpha inhibitors in the treatment of rheumatoid arthritis. Expert Opin Drug Saf. 2016;15:613–624. doi: 10.1517/14740338.2016.1160054. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data sharing policy of Janssen Pharmaceutical Companies of Johnson & Johnson is available at https://www.janssen.com/clinicaltrials/transparency. As noted on this site, requests for access to the study data can be submitted through Yale Open Data Access Project site at http://yoda.yale.edu.