Abstract
Introduction
The psychological wellbeing of healthcare workers has been impacted by the high levels of stress many have experienced during the Coronavirus Disease 2019 (COVID-19) pandemic. This study aimed to examine the feasibility and acceptability of a brief online course focused on introducing evidence-based skills that could increase resilience and decreases emotional distress in healthcare workers during the pandemic.
Materials and methods
Employees of a large healthcare system completed a mental health survey at baseline, and then one month and two months after some employees participated in an online resilience-enhancement course consisting of three 12–19 min videos focused on mindfulness, mentalization, and self-compassion.
Results
A total of 554 participants completed the baseline survey, endorsing moderate to high levels of emotional distress. Of those who completed all three assessments and participated in the course (n = 38), significant improvements in resilience and reductions in emotional distress were found one and two months later, in comparison to those who did not participate in the course (n = 110). Discussion: These findings suggest that a brief, online intervention can improve the mental health of healthcare workers during a crisis such as the COVID-19 pandemic.
Keywords: COVID-19, Healthcare workers, Resilience, Mental health, Pandemic
1. Introduction
The World Health Organization has stated that supporting the mental wellbeing of healthcare workers during the Coronavirus Disease 2019 (COVID-19) pandemic is a critical priority (World Health Organization, 2020). During the pandemic, this population has experienced persistently elevated levels of stress related to the greatly increased clinical demands placed on them, during a time when they may also lack their typical sources of support, due to the isolation and reduced staffing associated with the pandemic. The psychological impact of the pandemic on this population was first observed in healthcare workers in Wuhan, China, where 45–50% reported depression and anxiety and 71% reported increases in emotional distress (Lai et al., 2020). Consistent with this initial finding, a systematic review of 44 studies conducted during the COVID-19 pandemic reported high rates of depression, anxiety, and acute stress reactions in healthcare workers in the United States and 14 other countries (Sanghera et al., 2020). Also, disruptions in sleep and elevated anxiety have been found in healthcare workers across a wide range of roles (Liang et al., 2020), with frontline workers reporting worse mental health symptoms than others (Meo et al., 2021). Healthcare workers in Singapore also reported a high rate of physical symptoms such as headaches, suggesting increases in somatization (Ng et al., 2020). These effects are reminiscent of the increased rates of depression, anxiety, and other signs of distress observed in healthcare workers during the Severe Acute Respiratory Syndrome (SARS) and Influenza A (H1N1) epidemics (Busch et al., 2021; Maunder et al., 2006) and highlight the need for interventions that protect healthcare workers from the psychological sequalae of major healthcare crises, which can be long-lasting in some cases (Lee et al., 2018).
Research conducted during these prior epidemics suggest that even brief psychosocial interventions delivered to healthcare workers during such outbreaks can improve mental health outcomes. For example, during the H1N1 epidemic in 2008, an intervention for healthcare workers was developed that focused on education about the anticipated epidemic and potential illnesses, as well as resilience training tools, such as mindfulness and other coping strategies (Maunder et al., 2010). Improvements in self-efficacy, confidence in their training, and reductions in interpersonal problems were reported by healthcare workers after the intervention (Maunder et al., 2010).
Based on this prior work, in March 2020, during the early stages of the initial surge in COVID-19 cases and hospitalizations in the Northeast United States, we developed a brief online course that aimed to introduce healthcare workers to psychological techniques that might enhance their ability to handle stress. Evidence from prior research conducted in a range of populations suggests that certain skills, such as mindfulness and other emotion regulation and stress management techniques, can increase an individual's capacity to manage and adapt to stressful circumstances (Kemper et al., 2015). Resilience, defined as the ability to “bounce back” or grow from challenging, highly stressful life events (Rutter, 1985), is thought to be a modifiable capacity and process linked to adaptive outcomes (Choi et al., 2019).
The online course, called Resilience Training (RT) for Healthcare Workers, consists of three 12–19 min videos that include didactic information, experiential exercises, and testimonials from healthcare workers that focus on three evidence-based skills or capacities shown to maintain or increase aspects of emotional resilience: mindfulness (Potes et al., 2018), mentalization (Daubney and Bateman, 2015), and self-compassion (Neff and Germer, 2013). The course materials were adapted from a related, existing program developed for young adults (Burke et al., 2020).
In this study, we first collected baseline information about levels of distress in healthcare workers, as reflected by self-reported anxiety, depression, and worries about the pandemic. In order to make the program rapidly and widely available at the onset of the COVID-19 outbreak in Boston, we employed a pragmatic non-randomized design, testing whether levels of resilience improved and distress decreased in the healthcare workers who opted to take the course compared to those who did not. In addition, we assessed whether baseline and improvements in resilience correlated with reductions in distress. Lastly, we tested whether exposure to patients with COVID-19 influenced these outcomes, since such exposure has been previously shown to correlate with distress in healthcare workers during the pandemic (Meo et al., 2021; Muller et al., 2020).
2. Methods
The three-session online RT course was one component of a larger set of wellness offerings for employees within the Massachusetts General Brigham (MGB) healthcare system that included two other online courses, as well as an overall effort to disseminate numerous wellness resources to employees (see: https://www.massgeneral.org/psychiatry/guide-to-mental-health-resources/general-mental-health-and-coping). Given the immediate need for such materials during the beginning of the COVID-19 pandemic in Boston, Massachusetts, these resources were offered to all employees. The RT course was made available via an online platform (HealthStream™) used to deliver mandatory trainings to employees of the MGB healthcare system. The course was advertised in system-wide emails listing wellness resources for employees. Those who enrolled in the study completed self-report surveys (without compensation) via REDCap at baseline, prior to participation in the online resilience training, and then one month and two months later. Neither completion of the surveys nor participation in the course were required; the course was offered to all MGB employees in order to provide unfettered access to any useful support for employees during the COVID-19 crisis. Inclusion criteria included being: 1) a current employee of the MGB Healthcare System, 2) 18 years or older in age. The study protocol was approved by the MGB Institutional Review Board (protocol number: 2020P000936; Principal Investigator: Daphne Holt, MD, PhD).
2.1. Resilience training course
The online RT for Healthcare Workers course consists of didactic materials delivered in pre-recorded videos by experienced doctoral level clinicians, testimonials of healthcare workers about their experiences during the pandemic and their use of the skills taught in the course, and brief experiential exercises. Session 1 (19 min) focused on the concept of resilience and mindfulness skills (Potes et al., 2018); session 2 (16 min) focused on enhancing cognitive flexibility via cognitive behavioral (Beck et al., 1979) and mentalization (Daubney and Bateman, 2015) skills; and session 3 (12 min) focused on the development of self-compassion (Neff and Germer, 2013). All three sessions emphasized ways to implement these concepts and skills in everyday life, highlighting specific challenges faced by healthcare workers during the COVID-19 pandemic.
2.2. Survey
Participants completed an online 23-item mental health survey three times: at baseline (prior to viewing the course), and approximately one month and two months after completion of the course. To minimize participant burden, particularly in light of the substantial workload of healthcare workers during the pandemic, the survey was composed of a limited number of items selected from validated questionnaires, with the exception of the Patient Health Questionnaire-4 (PHQ-4; (Löwe et al., 2010), which was included in its entirety (four items, two assessing anxiety and two assessing depression) to capture emotional distress. Other questions assessed a range of outcomes including demographic characteristics, COVID-19 related anxiety, resilience (with two items from the Brief Resilience Scale (Smith et al., 2008)), one item assessing one's ability to utilize coping skills (Park et al., 2021); loneliness (with two items from the UCLA Loneliness Scale (Russell, 1996)); self-compassion (with one item from the Self-Compassion Scale (Neff et al., 2019)), and burn-out (with one item from the Maslach Burnout Inventory (Maslach et al., 1986).
2.3. Statistical analyses
Our primary analyses focused on two outcomes: 1) resilience (the sum of agreement from 1 to 5 on the following three items: “I am able to bounce back quickly after hard times,” “I am able to come through difficult times with little trouble,” and “I am able to cope with the stress in my life”) and 2) emotional distress (the sum of endorsement ratings on a 1–4 scale on the following four items of the PHQ-4: “feeling nervous, anxious or on edge,” “not being able to stop or control worrying,” “feeling down, depressed, or hopeless,” and “little interest or pleasure in doing things”). Frequencies and Pearson's correlations were calculated first in the baseline sample, then in the longitudinal sample (i.e., those who completed all three assessments) separately. To examine the effect of the RT course on resilience and emotional distress, paired sample t-tests were used to compare the baseline and the two longitudinal time points. Repeated measures ANOVAs were then used to assess the two primary outcomes in those who participated in the RT intervention compared to those who did not. The ANOVA exploring the effects of RT on emotional distress included COVID-19 related anxiety as a covariate, since it was significantly associated with emotional distress (p < .001). All analyses were conducted using SPSS, version 26.
3. Results
The results reported here are based on analyses of the participants who completed the baseline survey (n = 554), those who completed the baseline and second survey (n = 163), and those who completed all three surveys (n = 148). Of those who completed all three surveys, 38 viewed at least one session of the RT course, 28 viewed at least two sessions and 27 viewed all three.
3.1. The baseline sample
3.1.1. Demographic characteristics
A total of 554 MGB employees completed the baseline survey (between April 14, 2020 and July 30, 2020). During that time, the number of confirmed COVID-19 cases in Massachusetts increased from 28,163 to 109,400 (Massachusetts Department of Public Health, 2021). Of the baseline participants, 87% reported that they were working in the hospital and 42% reported having at least some contact with COVID-19 patients. Within the three main healthcare worker groups (nurses (26.9%), physicians (13.9%), and other hospital roles (59.2%)), 81% of nurses, 75% of physicians, and 45% of those with other hospital roles were working in-person at their healthcare facility at the time of taking the survey. A total of 68% of nurses, 57% of physicians, and 27% of other workers had had at least one contact with a COVID-19 positive individual. The baseline sample had a mean age of 44.14 years (SD = 13.50) and the longitudinal sample had a mean age of 43.32 years (SD = 13.07). Additional participant characteristics are reported in Table 1 .
Table 1.
Participant characteristics.
| Baseline Sample (n = 554) | Longitudinal Sample (n = 148) | |||
|---|---|---|---|---|
| N |
% |
N |
% |
|
| Gender | ||||
| Male | 61 | 11% | 13 | 8.5% |
| Female | 482 | 87% | 134 | 90.5% |
| Other | 11 | 2% | 1 | 1% |
| Ethnicity | ||||
| Hispanic | 30 | 5.8% | 13 | 8.6% |
| Not Hispanic | 479 | 91.9% | 133 | 90% |
| Prefer not to answer | 12 | 2.3% | 2 | 1.4 |
| Race | ||||
| White | 448 | 85.4% | 130 | 87.8% |
| Black/African American | 16 | 3.1% | 2 | 1.4% |
| Asian | 40 | 7.6% | 11 | 7.4% |
| Native American | 5 | 1% | 1 | 0.7% |
| Other | 15 | 2.9% | 4 | 2.7% |
| Hospital Role | ||||
| Physician | 76 | 13.9% | 23 | 15.5% |
| Nurse | 147 | 26.9% | 46 | 31.1% |
| Administrator | 76 | 13.9% | 15 | 10.1% |
| Pharmacist | 9 | 1.6% | 4 | 2.7% |
| Research | 40 | 7.3% | 8 | 5.4% |
| Therapist | 39 | 7.1% | 10 | 6.8% |
| Technician | 28 | 5.1% | 6 | 4.1% |
| Medical assistant | 15 | 2.7% | 3 | 2% |
| Other clinical role | 117 | 21.4% | 33 | 22.3% |
| Living Situation | ||||
| Live alone | 89 | 17.9% | 26 | 18.4% |
| Live with one other person | 172 | 34.9% | 55 | 39% |
| Live with more than one other person | 293 | 70.3% | 67 | 42.6% |
3.1.2. Associations
Across all participants, moderate to high levels of baseline emotional distress (M = 8.15, SD = 2.92 on a scale of 1–12, with scores of 6–8 on the PHQ-4 representing “moderate” levels of anxiety and depression (Löwe et al., 2010)) were found. Participants endorsed feeling lonely “several days” per week on average (M = 1.7, SD = 0.77). Exposure to patients with COVID-19 did not correlate with baseline emotional distress or loneliness (r = 0.046 and 0.058, respectively). However, in the full sample, greater exposure to COVID-19 patients was associated with a greater likelihood of having the feeling of positively impacting others (r = 0.171, p < .001). A feeling of positively impacting others was also significantly related to lower emotional distress (r = -.285, p < .001). Lastly, significant correlations were found between emotional distress, loneliness, COVID-19-related anxiety, and resilience (see Table 2 ).
Table 2.
Baseline correlations (N = 554, Pearson's r values).
| Emotional Distress | Loneliness | COVID-19 Related Anxiety | |
|---|---|---|---|
| Emotional Distress | |||
| Loneliness | .539** | ||
| COVID-19 Related Anxiety | .275** | .264** | |
| COVID-19 Exposure | .046 | .058 | .100* |
| Resilience | -.535** | -.304** | -.138 |
| Self-Compassion | -.334** | -.202** | -.162** |
| Positively Impacting Others | -.284** | -.168** | -.058 |
Note: *p < .05; **p < .001.
3.2. The longitudinal sample
3.2.1. Demographic characteristics
The mean dates-of-completion for the second and third time point were June 20, 2020 and July 31, 2020, respectively. 86% of this sample was working in-person during this time and 44.6% had contact with a COVID-19 patient. The demographic characteristics of this sample were similar to those of the baseline sample (see Table 1).
3.2.2. Associations of baseline resilience with longitudinal outcomes
Greater levels of baseline resilience were associated with lower levels of emotional distress (rated on the PHQ-4) at both the second (r = -.407, p < .001) and third (r = -.445, p < .001) timepoints. Similar relationships with baseline resilience were observed for loneliness at the second (r = -.384, p < .001) and third (r = -.406, p < .001) timepoints. Greater exposure to COVID-19 patients at baseline was not related to emotional distress at subsequent time points (all ps > .05).
3.2.3. Effects of the RT course within subjects
231 participants (of 554 (41.7%)) viewed at least a portion of the RT course, with 115 (of 554 (20.7%)) viewing all three sessions. Among those who took the RT course and completed all of the assessments (n = 38), there was no significant change in resilience levels from baseline to one month following the course (t = 1.46, p = .153) but subsequently, resilience levels significantly increased from baseline to two months following the course (t = 2.88, p = .010). In addition, significant decreases in emotional distress were observed at one month (t = 3.09, p = .004) and two months following the course (t = 2.97, p = .009).
3.2.4. Comparisons between those who took the RT course and those who did not
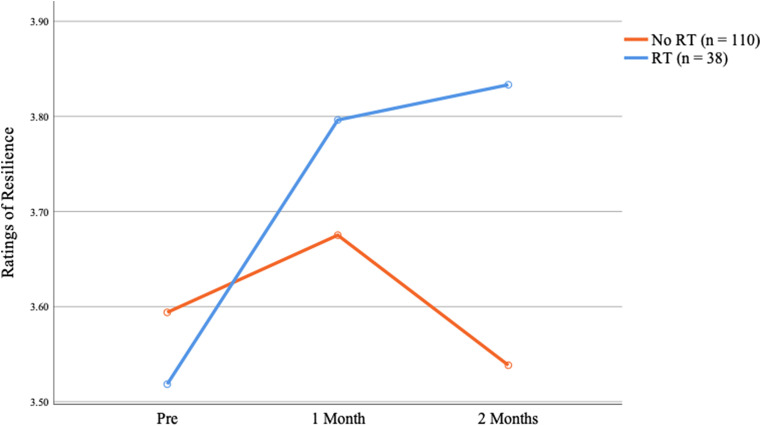
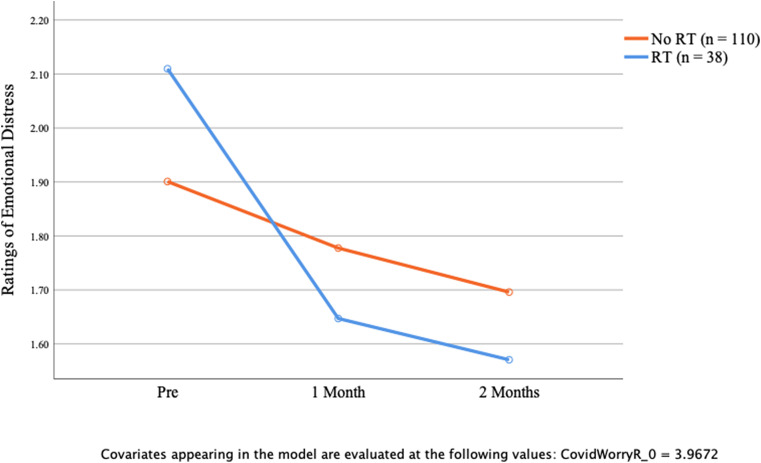
Among the 148 participants who completed all three assessments, there were no significant differences in demographic variables, or in baseline resilience and emotional distress, between those who took the RT course (n = 38) compared to those who did not (n = 110) (all ps > .10). A repeated measure ANOVA testing for effects of the RT course on resilience revealed a significant group by time interaction (F(2, 122) = 3.56, p = .031); those who took the RT course showed sustained improvements in resilience over the two month follow-up period compared to those who did not (Fig. 1 ). Similarly, a repeated measures ANOVA testing for effects of the RT course on emotional distress also revealed a significant group by time interaction (F(2, 116) = 3.15, p = .047), due to reductions in emotional distress in the RT participants compared to those who did not take the course (Fig. 2 ).
Fig. 1.
Self-reported resilence, as measured using a 4-item composite scale, improved in the MGB employees who chose to take the Resilience Training (RT) for Healthcare Workers 3-session online course over the two month follow-up period, compared to those who did not, as reflected by a significant group by time interaction = F(2, 122) = 3.562, p = .031.
Fig. 2.
Self-reported levels of anxiety and depression, as measured using the 4-item PHQ-4 scale, decreased in the MGB employees who chose to take the Resilience Training (RT) for Healthcare Workers 3-session online course over the two month follow-up period, compared to those who did not, as reflected by a significant group by time interaction F(2,116) = 3.145, p = .047, with COVID-19 worry included as a covariate.
Consistent with these results, within the group that took the RT course, improvements in resilience correlated with decreases in emotional distress at one month (r = −.560 p < .001) and two months (r = -.666, p = .003) following the course.
4. Discussion
This study replicates findings of other studies of the mental health of healthcare workers during the COVID-19 pandemic (Lai et al., 2020) and prior pandemics (Busch et al., 2021; Maunder et al., 2006), which have shown that this vulnerable population experiences moderate to high levels of distress and a sense of isolation during such crises. In addition, in the intervention portion of the current study, which by necessity used a pragmatic, nonrandomized design, improvements in resilience and decreases in emotional distress were observed in healthcare employees who chose to participate in the brief online resilience training course. These initial findings, while they must be interpreted with caution given the small size of the sample and the non-randomized design, further support the possibility that a brief, online intervention can be beneficial to healthcare workers even in the midst of a crisis (Maunder et al., 2010), potentially providing a much-needed boost to mental health during a time of extraordinary stress. Moreover, these results are consistent with prior evidence that healthcare workers are willing to engage in online, wellness-focused courses (Blake et al., 2020), and that such courses can be effective for this population (Maunder et al., 2010).
Of note, surprisingly (Muller et al., 2020), exposure to patients with COVID-19 was not significantly correlated with emotional distress in this sample, possibly because the majority of the participants may have felt the psychological impact of the pandemic regardless of whether or not they had had direct exposure to a patient infected with the virus. During the first surge of the pandemic in the U.S. when testing was infrequent (when much of these data were collected), healthcare workers may have been highly aware of the increased risk of infection for themselves and their family members that was associated with their jobs (Adams and Walls, 2020; Black et al., 2020). Thus, these healthcare employees may have been generally impacted by knowledge of this risk, independent of their degree of COVID-19 exposure.
However, greater exposure to COVID-19 patients was associated with a greater likelihood of having a feeling of positively impacting others, suggesting that being involved in the care of such patients may have been psychologically protective to some extent, conferring a greater sense of purpose and meaning during the crisis. This is consistent with prior evidence for links between having a sense of purpose and greater resilience (Ostafin and Proulx, 2020).
All three of the skills taught in the RT intervention, mindfulness, mentalization, and self-compassion, have been shown to decrease various forms of emotional distress, such as symptoms of anxiety and depression (Frostadottir and Dorjee, 2019; Hayden et al., 2018; Hofmann and Gómez, 2017). These skills were the focus of the course in order to serve its goal of fostering key emotion regulation capacities, and allowing healthcare workers to engage in a type of active resilience building (Kalisch et al., 2015). They were also selected because of evidence for their positive effects on social functioning (Burke et al., 2020; Lindsay et al., 2019). Given the increased social isolation experienced by many during the COVID-19 pandemic, including healthcare workers who have often been required to work long hours in masks and other protective equipment while maintaining “social distance” from others, enhancing capacities that may lead to more meaningful connections with others may help to preserve well-being during this unusual period in history and its aftermath, as well as during other times of adversity.
In light of the need for such interventions for healthcare workers both during and following the COVID-19 pandemic, programs like this merit further study while being simultaneously rapidly implemented. In designing follow-up work, several limitations of this study should be considered. The non-randomized design of this study, although necessary given the high level of need of the population, limits the inferences that can be made from these findings. Also, enrollment was likely affected by the fact that these healthcare employees were being flooded daily with lengthy emails regarding COVID-19-related information and supports, some of which included information about this study. This “information overload”, and the other multiple new demands associated with the crisis, may have also interfered with the capacity of participants to view the videos and complete all three assessments. It should also be noted that the follow-up period of this study was only two months, leaving open the question of how long the observed effects were maintained.
In summary, this study provides preliminary evidence for the efficacy of a brief online intervention for improving resilience and decreasing emotional distress in healthcare workers during the COVID-19 pandemic. Because some healthcare workers will likely need ongoing, additional support over time, perhaps even well after the pandemic has subsided, new resilience-enhancing interventions that are tailored to meet the changing needs of this population should also be developed and implemented.
Funding details
This study was supported by funding from the Ruderman Family Foundation, the Good Samaritan Inc., and the Department of Psychiatry of Massachusetts General Hospital.
Data availability statement
All data are available here.
Declaration of competing interest
Dr. Perlis has received consulting fees from Burrage Capital, RID Ventures, Genomind, and Takeda, and he holds equity in Outermost Therapeutics and Psy Therapeutics; these activities are unrelated to the present work. Dr. Sylvia has served as a consultant for United Biosource Corporation, Clintara, Bracket, and Clinical Trials Network and Institute. She receives royalties from New Harbinger and has received grant/research support from NIMH, PCORI, AFSP, and Takeda. Dr. Fava's lifetime financial disclosures are listed here. All other authors have no disclosures to report.
Acknowledgements
We would like to thank a number of critical contributors to the development of the online intervention and data collection (including healthcare workers and experts who provided testimonials or advice within the course, members of the film crew, and research staff, listed alphabetically): Amber Leonard Alibrio, Archana Basu, Wisteria Deng, Brad Dickerson, Darcie Edwards, Rich Fomo, Nevita George, Chris Germer, Chad Gobert, Diana Johnson, Rachel Kakos, Megan Koster, Seth Margolis, Mia Mazzaferro, Roberto Mighty, Julia Newbold, Olivia Okereke, Steven Pugliese, Phoebe Ramler, Christopher Richard, Matthew Robinson, Nancy Rotter, Lauren Schiffner, Lauren Washington, Lynn Weissman, Suzanne Willard-Kiess, Sarah Zapetis, and Janet Zedler. We would also like to thank all of the staff of the MGH Resilience and Prevention Program who contributed to the content and/or implementation of previous iterations of the course material.
References
- Adams J.C., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. J. Am. Med. Assoc. 2020;15:323. doi: 10.10001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- Beck A., Rush J., Shaw B., Emery G. Gilford Press; New York, NY: 1979. Cognitive Therapy of Depression. [Google Scholar]
- Black J.R.M., Bailey C., Przewrocka J., Dijkstra K.K., Swanton C. COVID-19: the case for health-care worker screening to prevent hospital transmission. Lancet. 2020;395:1418–1420. doi: 10.1016/S0140-6736(20)30917-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake H., Bermingham F., Johnson G., Tabner A. Mitigating the psychological impact of COVID-19 on healthcare workers: a digital learning package. Int. J. Environ. Res. Publ. Health. 2020;17:2997. doi: 10.3390/ijerph17092997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke A.S., Shapero B.G., Pelletier-Baldelli A., Deng W.Y., Nyer M.B., Leathem L., Namey L., Landa C., Cather C., Holt D.J. Rationale, methods, feasibility, and preliminary outcomes of a transdiagnostic prevention program for at-risk college students. Front. Psychiatr. 2020;10:1030. doi: 10.3389/fpsyt.2019.01030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busch I.M., Moretti F., Mazzi M., Wu A.W., Rimondini M. What we have learned from two decades of epidemics and pandemics: a systematic review and meta-analysis of the psychological burden of frontline healthcare workers. Psychother. Psychosom. 2021;1–13 doi: 10.1159/000513733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi K.W., Stein M.B., Dunn E.C., Koenen K.C., Smoller J.W. Genomics and psychological resilience: a research agenda. Mol. Psychiatr. 2019;24:1770–1778. doi: 10.1038/s41380-019-0457-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daubney M., Bateman A. Mentalization-based therapy (MBT): an overview. Australas. Psychiatr. 2015;23:132–135. doi: 10.1177/1039856214566830. [DOI] [PubMed] [Google Scholar]
- Frostadottir A.D., Dorjee D. Effects of mindfulness based cognitive therapy (MBCT) and compassion focused therapy (CFT) on symptom change, mindfulness, self-compassion, and rumination in clients with depression, anxiety, and stress. Front. Psychol. 2019;10:1099. doi: 10.3389/fpsyg.2019.01099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayden M.C., Müllauer P.K., Gaugeler R., Senft B., Andreas S. Improvements in mentalization predict improvements in interpersonal distress in patients with mental disorders. J. Clin. Psychol. 2018;74:2276–2286. doi: 10.1002/jclp.22673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann S.G., Gómez A.F. Mindfulness-based interventions for anxiety and depression. Psychiatr. Clin. 2017;40:739–749. doi: 10.1016/j.psc.2017.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalisch R., Müller M.B., Tüscher O. A conceptual framework for the neurobiological study of resilience. Behav. Brain Sci. 2015;38:e92. doi: 10.1017/S0140525X1400082X. [DOI] [PubMed] [Google Scholar]
- Kemper K.J., Mo X., Khayat R. Are mindfulness and self-compassion associated with sleep and resilience in health professionals? J. Alternative Compl. Med. 2015;21:496–503. doi: 10.1089/acm.2014.0281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to Coronavirus Disease 2019. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.M., Kang W.S., Cho A.-R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatr. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang Y., Chen M., Zheng X., Liu J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J. Psychosom. Res. 2020;133:110102. doi: 10.1016/j.jpsychores.2020.110102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay E.K., Young S., Brown K.W., Smyth J.M., Creswell J.D. Mindfulness training reduces loneliness and increases social contact in a randomized controlled trial. Proc. Natl. Acad. Sci. Unit. States Am. 2019;116:3488–3493. doi: 10.1073/pnas.1813588116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Wahl I., Rose M., Spitzer C., Glaesmer H., Wingenfeld K., Schneider A., Brähler E. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J. Affect. Disord. 2010;122:86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- Maslach C., Jackson S., Leiter M., Schaufeli W., Schwab R. vol. 21. Consulting Psychologists Press; Palo Alto, CA: 1986. (Maslach Burnout Inventory). [Google Scholar]
- Maunder R., Lancee W., Balderson K., Bennett J., Borgundvaag B., Evans S., Fernandes C., Goldbloom D., Gupta M., Hunter J., McGillis Hall L., Nagle L., Pain C., Peczeniuk S., Raymond G., Read N., Rourke S., Steinberg R., Stewart T., VanDeVelde-Coke S., Veldhorst G., Wasylenki D. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 2006;12:1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder R.G., Lancee W.J., Mae R., Vincent L., Peladeau N., Beduz M.A., Hunter J.J., Leszcz M. Computer-assisted resilience training to prepare healthcare workers for pandemic influenza: a randomized trial of the optimal dose of training. BMC Health Serv. Res. 2010;10:72. doi: 10.1186/1472-6963-10-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meo S.A., Alkhalifah J.M., Alshammari N.F., Alnufaie W.S. Comparison of generalized anxiety and sleep disturbance among frontline and second-line healthcare workers during the COVID-19 pandemic. Int. J. Environ. Res. Publ. Health. 2021;18:5727. doi: 10.3390/ijerph18115727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller A.E., Hafstad E.V., Himmels J.P.W., Smedslund G., Flottorp S., Stensland S.Ø., Stroobants S., Van de Velde S., Vist G.E. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatr. Res. 2020;293:113441. doi: 10.1016/j.psychres.2020.113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff K.D., Germer C.K. A pilot study and randomized controlled trial of the mindful self-compassion program: a pilot and randomized trial of msc program. J. Clin. Psychol. 2013;69:28–44. doi: 10.1002/jclp.21923. [DOI] [PubMed] [Google Scholar]
- Neff K.D., Tóth-Király I., Yarnell L.M., Arimitsu K., Castilho P., Ghorbani N., Guo H.X., Hirsch J.K., Hupfeld J., Hutz C.S., Kotsou I., Lee W.K., Montero-Marin J., Sirois F.M., de Souza L.K., Svendsen J.L., Wilkinson R.B., Mantzios M. Examining the factor structure of the Self-Compassion Scale in 20 diverse samples: support for use of a total score and six subscale scores. Psychol. Assess. 2019;31:27–45. doi: 10.1037/pas0000629. [DOI] [PubMed] [Google Scholar]
- Ng Q.X., De Deyn M.L.Z.Q., Lim D.Y., Chan H.W., Yeo W.S. The wounded healer: a narrative review of the mental health effects of the COVID-19 pandemic on healthcare workers. Asian J. Psychiatry. 2020;54:102258. doi: 10.1016/j.ajp.2020.102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostafin B.D., Proulx T. Meaning in life and resilience to stressors. Hist. Philos. Logic. 2020;33:603–622. doi: 10.1080/10615806.2020.1800655. [DOI] [PubMed] [Google Scholar]
- Park E.R., Sylvia L.G., Streck J.M., Luberto C.M., Stanton A.M., Perez G.K., Baim M., Bliss C.C., Convery M.S., Crute S., Denninger J.W., Donelan K., Dossett M.L., Fava M., Fredriksson S., Fricchione G., George N., Hall D.L., Hart B.R., Herman J., Hirschberg A., Holt D., Looby S.E., Malloy L., Meek J., Mehta D.H., Millstein R.A., Mizrach H., Rosa K., Slawsby E., Stupinski A.C., Traeger L., Vanderkruik R., Vogeli C., Wilhelm S. Launching a resiliency group program to assist frontline clinicians in meeting the challenges of the COVID-19 pandemic: results of a hospital-based systems trial. Gen. Hosp. Psychiatr. 2021;68:111–112. doi: 10.1016/j.genhosppsych.2020.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potes A., Souza G., Nikolitch K., Penheiro R., Moussa Y., Jarvis E., Looper K., Rej S. Mindfulness in severe and persistent mental illness: a systematic review. Int. J. Psychiatr. Clin. Pract. 2018;22:253–261. doi: 10.1080/13651501.2018.1433857. [DOI] [PubMed] [Google Scholar]
- Russell D.W. UCLA loneliness scale (version 3): reliability, validity, and factor structure. J. Pers. Assess. 1996;66:20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Rutter M. Resilience in the face of adversity: protective factors and resistance to psychiatric disorder. Br. J. Psychiatry. 1985;147:598–611. doi: 10.1192/bjp.147.6.598. [DOI] [PubMed] [Google Scholar]
- Sanghera J., Pattani N., Hashmi Y., Varley K.F., Cheruvu M.S., Bradley A., Burke J.R. The impact of SARS‐CoV‐2 on the mental health of healthcare workers in a hospital setting—a Systematic Review. J. Occup. Health. 2020;62 doi: 10.1002/1348-9585.12175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B.W., Dalen J., Wiggins K., Tooley E., Christopher P., Bernard J. The brief resilience scale: assessing the ability to bounce back. Int. J. Behav. Med. 2008;15:194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2020. Mental Health and Psychosocial Considerations during the COVID-19 Outbreak. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are available here.