Data on severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) seroprevalence can help to guide public health care responses. Antenatal blood samples are a unique and minimally biased set for seroprevalence studies; prenatal care has an exceptional uptake of >95% and represents patients from all geographic jurisdictions, including remote areas, and socioeconomic and cultural backgrounds. As a pilot study to the larger Canadian Population Serological Survey Utilizing Antenatal Serum Samples, we used near-delivery and first-trimester antenatal serum samples from two time periods in British Columbia to assess adult SARS-CoV-2 seroprevalence using multiple assays.
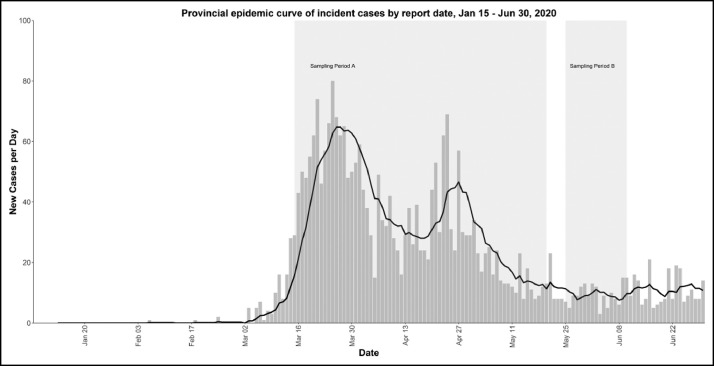
The median age of participants was 32 years (range 16–48), and geographic locations represented the provincial population distribution (23.4% Vancouver Coastal, 30.9% Fraser, 22.0% Interior, 15.2% Vancouver Island, and 8.6% Northern Health Authorities). We used three clinical anti-Spike/RBD antibody assays (DiaSorin IgG, Ortho VITROS Total antibody, and Siemens Total antibody) to screen near-delivery serum samples (D-serum): (1) 501 samples collected from March 15 to May 20, 2020 (period A) and (2) 520 samples collected from May 25 to June 10, 2020 (period B) (Figure ). For any positive D-serum, the corresponding participant's first-trimester sample (P-serum) was tested using all three anti-Spike/RBD antibody assays and clinical anti-Nucleocapsid assay (Abbott IgG). All D-serum and P-serum samples that tested positive on any clinical assay were tested using a research multiplex serology assay, with simultaneous detection of anti-Spike, anti-RBD, anti-Nucleocapsid, and anti–seasonal coronavirus spike IgG (V-PLEX COVID-19 Coronavirus Panel 3 IgG, Meso Scale Discovery, Rockville, MD). This robust testing approach and ability to assess for seroconversion (P-sera to D-sera) allowed high confidence in ascertainment of true versus false positive test results.
Figure.
Provincial epidemic curve with study sampling periods.
No D-sera from period A and only one D-serum from period B was conclusively positive for anti-SARS-CoV-2 antibodies. Two D-sera from period A and one D-serum from period B were found to be reactive on only one clinical anti-Spike/RBD assay, with additional testing of corresponding P-serum samples and additional clinical and research assays indicative of false-reactive results. All false-reactive samples showed high levels of anti–seasonal coronavirus spike IgG antibodies.
One D-serum from period B was found to be reactive on all clinical anti-Spike/RBD assays and anti-Nucleocapsid assay, with corresponding P-serum being fully nonreactive; Meso Scale Discovery assay yielded concordant results for both samples. This represented a true case of seroconversion.
Overall, the seroprevalence of SARS-CoV-2 in this representative sample of a healthy adult population was <1%, consistent with findings in Canada and elsewhere from that time period.1 , 2 The potential strength of this approach relative to other seroprevalence studies in Canada is its use of a less biased sample compared to blood donors or residual outpatient serum samples.
We demonstrated the ability to use antenatal serum samples as a minimally biased window into the adult population seroprevalence, finding a low seroprevalence of <1%. We were also able to demonstrate a true seroconversion during pregnancy. The ability to detect seroconversions and to correlate them with clinical outcomes through linkage to perinatal datasets could be highly impactful in understanding the effects of SARS-CoV-2 infection during pregnancy. A national Canadian study using antenatal serum samples that is endorsed by the COVID-19 Immunity Task Force and supported by the Public Health Agency of Canada is facing great challenges owing to differences across Canada in the ability to obtain approval for this work and share these data. We hope to have some results in the near future (https://ridprogram.med.ubc.ca/cancovid-preg-antenatal-serostudies/).
As the pandemic has continued, we have seen dramatically increased rates of infection among reproductive-age adults, which will certainly result in increased seroprevalence detected within antenatal serum samples over time. In addition, seroprevalence studies and the SARS-CoV-2–neutralizing capacity of antibody-positive individuals could provide critical information on ongoing population immunity after vaccine introduction.
Footnotes
Disclosures:C.E. has served as an advisory board member for Gilead, as a reproductive infectious disease specialist. G.O. and D.M. are members of the Canadian COVID-19 Immunity Task Force. M.K. reports grants/contracts paid to his institution from Roche/Hologic/Siemens. D.M. has received past funding for unrelated work from Merck, GSK, Sanofi, and Novartis. E.M. is supported by a CANFAR/CTN Postdoctoral Fellowship Award and an MSFHR Research Trainee Award. This work was supported in kind by the Provincial Health Services Authority through the BC Centre for Disease Control and the UBC Reproductive Infectious Diseases Program and Women's Health Research Institute.
All authors have indicated they meet the journal's requirements for authorship.
REFERENCES
- 1.Danuta M, Skowronski IS, Sabaiduc S, et al. Low SARS-COV-2 sero-prevalence based on anonymized residual sero-survey before and after first wave measures in British Columbia, Canada, March-May 2020. Available at: https://www.medrxiv.org/content/10.1101/2020.07.13.20153148v1.full.pdf.
- 2.Services CB. COVID-19 seroprevalence report. August 19, 2020. https://www.blood.ca/sites/default/files/CBS_COVID-19_Seroprevalence_Public_Report_ Aug272020.pdf. Accessed on January 8, 2021.