Abstract
Objective
To describe the impact of coronavirus disease-2019 (COVID-19) on the neonatology workforce, focusing on professional and domestic workloads.
Study design
We surveyed US neonatologists in December 2020 regarding the impact of COVID-19 on professional and domestic work during the pandemic. We estimated associations between changes in time spent on types of professional and domestic work and demographic variables with multivariable logistic regression analyses.
Results
Two-thirds (67.6%) of the 758 participants were women. Higher proportions of women than men were in the younger age group (63.3% vs 29.3%), held no leadership position (61.4% vs 46.3%), had dependents at home (68.8% vs 56.3%), did not have a partner or other adult at home (10.6% vs 3.2%), and had an employed partner (88.1% vs 64.6%) (P < .01 for all). A higher proportion of women than men reported a decrease in time spent on scholarly work (35.0% vs 29.0%; P = .02) and career development (44.2% vs 34.9%; P < .01). A higher proportion of women than men reported spending more time caring for children (74.2% vs 55.8%; P < .01). Reduced time spent on career development was associated with younger age (aOR, 2.21; 95% CI, 1.20-4.08) and number of dependents (aOR, 1.21; 95% CI, 1.01-1.45). Women were more likely to report an increase in time spent time doing domestic work (aOR, 1.53; 95% CI, 1.07-2.19) and a reduction in time on self-care (aOR, 0.49; 95% CI, 0.29-0.81).
Conclusions
COVID-19 significantly impacts the neonatology workforce, disproportionately affecting younger, parent, and women physicians. Targeted interventions are needed to support postpandemic career recovery and advance physician contributions to the field.
Keywords: pediatrics, workforce, gender differences
Abbreviations: AAP, American Academy of Pediatrics; COVID-19, Coronavirus disease-2019; SoNPM, Section on Neonatal Perinatal Medicine
The coronavirus disease-2019 (COVID-19) pandemic has significant effects on the physician workforce that have yet to be well characterized. The pandemic's adverse consequences have not affected physicians equally and threaten to intensify existing gender disparities in medical careers.1, 2, 3, 4, 5, 6, 7 Additionally, parents have faced extra challenges, with often inadequate workplace and domestic support.4 , 8 Women and parent physicians disproportionately have shouldered increased burdens and anxiety associated with domestic duties, restrictions in childcare access, home schooling, and higher productivity expectations given a perceived increase in available time during lockdown.7, 8, 9, 10, 11, 12, 13, 14, 15 The lack of in-person networking and conferences and a decrease in supplemental professional funds have negative impacts on career advancement.5 , 16 Healthcare workers, especially women, have reported increased stress and mental health concerns.2 , 3 , 15 , 17
Although women represent a significant proportion of the physician workforce,18 gender disparities still existed prepandemic in most aspects of medical careers, including inadequate representation in leadership and higher academic ranks, lower scholarly productivity and publication rates, lower compensation, delayed career success, and fewer opportunities for promotion among women physicians.1 , 12 , 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35 Numerous factors contribute to these differences, including bias, traditional gender role definitions, sexual harassment, and a relative paucity of women in leadership roles.19 , 36, 37, 38 An increased burden of domestic responsibilities is an additional challenge that often differentially affects women.4 , 39 Overall, women physicians are more likely than men to report spending more time on household activities and childcare and to state that domestic responsibility interferes with their professional duties.21 , 22 , 25 , 32 , 40, 41, 42, 43, 44, 45, 46 Women physicians, particularly those in intensive care fields, are more likely to experience burnout and mental health issues.19 , 45 , 47, 48, 49 The increasing proportion of women physicians in neonatology, a subspecialty with rigorous demands of intensive care,50 has led to greater recognition of the gender gap's impact on professional advancement in this field.
In the present study, we sought to describe the impact of the COVID-19 pandemic on the time spent on professional and domestic work of neonatologists and hypothesized that women and men had differential experiences. The COVID-19 pandemic has amplified the need to better support the workforce. A deeper understanding of the workload burdens that surfaced during the pandemic is key to building interventions that address the recovery of career trajectories and may support future gender equity for the pediatric workforce.
Methods
Sample and Data Collection
A cross-sectional survey study was conducted to examine the impact of the pandemic on neonatologists' professional and domestic workloads. A survey methodologist assisted with the survey design and the survey was programmed and stored in the REDCap database, a secure, internet-based research application designed for data storage and online surveys. Before survey dissemination, a core group of neonatologists tested the survey for constructive feedback and time and ease of completion. The Institutional Review Board at the Stanley Manne Institute at Ann & Robert H. Lurie Children's Hospital of Chicago deemed this study exempt. Signed written informed consent was not required, given that completion of the study implied participant consent.
We surveyed a convenience sample of academic and private practice neonatologists in the United States and Puerto Rico. We distributed the Internet survey link and an invitation to participate through the following listservs: the American Academy of Pediatrics (AAP) Section on Neonatal Perinatal Medicine (AAP SoNPM, approximately 3000 neonatologist members), the Neonatology Academic Division Chiefs’ (division chiefs were requested, but not required, to forward to their faculty members), MEDNAX Neonatology, and the Southern California Permanente Medical Group. We encouraged survey participation on social media platforms, including LinkedIn, Facebook, and Twitter. A single reminder email was sent via listserv 2 weeks after initial distribution.
The survey was administered from December 1, 2020 to December 18, 2020. It began with a short paragraph that stated the aim, instructions to complete the survey only once, and assurance of voluntary anonymous participation and confidentiality. The survey questions asked participants to reflect on their experience since the start of the pandemic.
Measures
The primary outcome of this study was the change in time spent on professional and domestic work since the start of the COVID-19 pandemic. The survey instrument (Appendix; available at www.jpeds.com) included 22 questions measuring the impact of the COVID-19 pandemic on the following: time spent on professional work (clinical care, scholarly work, institutional and national service, medical education, career development, and administrative work), accomplishments, productivity, and other professional issues, such as compensation and new work related to COVID-19 (eg, research or clinical redeployment to other units), time spent on domestic work (dependent care, housework), and time spent on self-care. Response options for time spent included “more,” “same,” “less,” or “not applicable” compared with the time before the pandemic. These categorical responses were chosen to minimize recall error and bias of precise hours given the longitudinal nature of the study, and to capture summative experience, even if individual workloads varied week to week during the pandemic. Demographic and professional characteristics included age, sex, race/ethnicity, years since completion of fellowship, nature of the practice, academic rank, full-time/part-time employment status, changes in employment status (including leave of absence), local and/or national leadership position (self-defined), number and age of dependents, and relationship status.
Statistical Analyses
Participant age was dichotomized into 2 groups based on the median age of the participating cohort: 31-47 years (younger) and 48-86 years (older). Career levels were determined by years since fellowship completion, in accordance with AAP SoNPM categorization: 0-7 years (early), 8-17 years (mid), and ≥18 years (late). Those who reported not spending time in a specific type of work (eg, clinical, dependent care) before and/or during the pandemic were excluded from the analysis for that specific type of work.
Descriptive analyses, including frequency analyses, were conducted using the χ2 test to detect differences (although not directionality) in participant characteristics and outcomes by gender. We selected outcomes that were statistically significantly different by gender in the bivariate analysis to fit multivariable logistic regression models. Multivariable logistic regression analyses were conducted to predict the probability of a reduction in time spent on the selected types of professional work and an increase in time spent on the selected types of domestic work. Potential covariates chosen based on risk factors noted in the literature4 , 7 , 12 , 22 , 34 included age (younger vs older), career level (early vs mid vs late), practice type (academic vs nonacademic), holding a leadership position (yes vs no), having a partner or live with other adults (yes vs no), having at least 1 young dependent (yes vs no), and having at least 1 school-age dependent (yes vs no). aORs and 95% CIs were estimated for these variables. Statistical significance was set at P < .05. C-statistics were used for overall model fit statistics.51 All analyses were conducted in SAS 9.4 (SAS Institute).
Results
Among 768 survey respondents, we excluded those who reported nonbinary gender (n = 1), preferred not to answer about gender (n = 4), or did not report any total work hours before or during the COVID-19 pandemic (n = 5). Of the remaining 758 respondents, 514 (68%) were women and 246 (32%) were men (Table I ). A higher proportion of women were in the younger age group, did not hold a leadership position, had dependents at home, did not have a partner or other adult in the home, and had a partner who was also employed (P < .01 for all).
Table I.
Characteristics of survey participants
| Characteristics | All, n (%) | Women, n (%) | Men, n (%) | P value, χ2 test |
|---|---|---|---|---|
| Total | 758 (100) | 512 (67.6) | 246 (32.4) | |
| Age group | <.01 | |||
| 31-47 y | 396 (52.2) | 324 (63.3) | 72 (29.3) | |
| 48-86 y | 362 (47.8) | 188 (36.7) | 174 (70.7) | |
| Race/ethnicity | .48 | |||
| White | 505 (66.6) | 342 (66.8) | 163 (66.3) | |
| Asian | 123 (16.2) | 83 (16.2) | 40 (16.3) | |
| Hispanic | 34 (4.5) | 19 (3.7) | 15 (6.1) | |
| Black | 31 (4.1) | 24 (4.7) | 7 (2.8) | |
| Mixed | 32 (4.2) | 20 (3.9) | 12 (4.9) | |
| Other | 13 (1.7) | 8 (1.6) | 5 (2.1) | |
| Prefer not to answer | 20 (2.6) | 16 (3.1) | 4 (1.6) | |
| Academic rank or practice setting∗ | <.01 | |||
| Instructor or assistant professor | 215 (28.9) | 174 (34.5) | 41 (17.1) | |
| Associate professor | 112 (15.1) | 72 (14.3) | 40 (16.7) | |
| Professor | 103 (13.8) | 47 (9.3) | 56 (23.3) | |
| Private practice | 244 (32.8) | 168 (33.3) | 76 (31.7) | |
| Other (eg, locum tenems only) | 70 (9.4) | 43 (8.5) | 27 (11.2) | |
| Career level† | <.01 | |||
| Early career | 266 (35.3) | 223 (43.7) | 43 (17.7) | |
| Mid-career | 271 (36.0) | 134 (26.3) | 137 (56.4) | |
| Late career | 216 (28.7) | 153 (30.0) | 63 (25.9) | |
| Part time | 63 (8.3) | 41 (8.0) | 22 (9.0) | .65 |
| Leadership position‡ | 329 (43.5) | 197 (38.6) | 132 (53.7) | <.01 |
| Age 31-47 y | 120 (30.4) | 89 (27.5) | 31 (43.1) | <.01 |
| Age 48-86 y | 209 (57.7) | 108 (57.4) | 101 (58.0) | .91 |
| Dependent(s) living in home§ | 490 (64.7) | 352 (68.8) | 138 (56.3) | <.01 |
| Dependent(s) younger than elementary school age | 180 (23.8) | 152 (29.7) | 28 (11.4) | <.01 |
| Dependent(s) of elementary school age (K-8) | 261 (34.4) | 196 (38.3) | 65 (26.4) | <.01 |
| Have a partner or live with other adults | 696 (91.8) | 458 (89.4) | 238 (96.8) | <.01 |
| Partner employed | 610 (80.5) | 451 (88.1) | 159 (64.6) | <.01 |
| Partner employed part time | 73 (9.6) | 29 (5.7) | 44 (17.9) | <.01 |
Missing, n = 14.
Missing, n = 5.
Missing, n = 1.
Missing, n = 1.
Table II presents the change in time spent on various types of professional and domestic work during the COVID-19 pandemic by gender. Most neonatologists reported working the same (60%) or more (32%) since the start of the pandemic, but a higher proportion of women (35%) than men (26%) reported this increase. The majority of respondents reported working the same amount of time in clinical care (76%). A higher proportion of women than men reported a decrease in time spent on scholarly work (35% vs 29%; P = .02) and on career development (44% vs 35%; P < .01). Most survey respondents with dependents reported spending more time caring for children since the start of the pandemic, but significantly more women than men reported this increase (74% vs 56%; P < .01). Most respondents also reported spending more time managing their children's education, and although a higher proportion of women than men reported this increase, the difference was not statistically significant. More women than men reported spending more time on domestic work. Although most respondents spent less time on self-care, significantly more women reported this change.
Table II.
Change in time spent in various types of professional and domestic work before and during the COVID-19 pandemic
| Type of work | All, n (%) | Women, n (%) | Men, n (%) | P value, χ2 test |
|---|---|---|---|---|
| Professional work | ||||
| Total work hours | .05 | |||
| More | 243 (32.0) | 179 (35.0) | 64 (26.0) | |
| Same | 453 (59.8) | 293 (57.2) | 160 (65.0) | |
| Less | 62 (8.2) | 40 (7.8) | 22 (9.0) | |
| Clinical care | .23 | |||
| More | 140 (18.6) | 103 (20.2) | 37 (15.2) | |
| Same | 572 (76.0) | 380 (74.7) | 192 (78.7) | |
| Less | 41 (5.4) | 26 (5.1) | 15 (6.1) | |
| Scholarly work | .02 | |||
| More | 99 (14.0) | 74 (15.5) | 25 (10.8) | |
| Same | 375 (53.0) | 236 (49.5) | 139 (60.2) | |
| Less | 234 (33.0) | 167 (35.0) | 67 (29.0) | |
| National and institutional service | .93 | |||
| More | 154 (26.2) | 101 (26.2) | 53 (26.4) | |
| Same | 320 (54.5) | 209 (54.2) | 111 (55.2) | |
| Less | 113 (19.3) | 76 (19.7) | 37 (18.4) | |
| Medical education | .34 | |||
| More | 73 (10.9) | 55 (12.1) | 18 (8.4) | |
| Same | 432 (64.7) | 290 (64.0) | 142 (66.0) | |
| Less | 163 (24.4) | 108 (23.8) | 55 (25.6) | |
| Career development | <.01 | |||
| More | 65 (9.0) | 50 (10.3) | 15 (6.3) | |
| Same | 361 (49.9) | 221 (45.5) | 140 (58.8) | |
| Less | 298 (41.2) | 215 (44.2) | 83 (34.9) | |
| Administrative work | 1.00 | |||
| More | 165 (22.8) | 111 (22.8) | 54 (22.7) | |
| Same | 505 (69.7) | 339 (69.8) | 166 (69.7) | |
| Less | 54 (7.5) | 36 (7.4) | 18 (7.6) | |
| Scholarly productivity | .17 | |||
| Positive impact | 42 (5.5) | 31 (6.0) | 11 (4.5) | |
| Neutral | 398 (52.5) | 257 (50.2) | 141 (57.3) | |
| Negative impact | 318 (42.0) | 224 (43.8) | 94 (38.2) | |
| National and institutional service productivity | .08 | |||
| Positive impact | 37 (4.9) | 30 (5.9) | 7 (2.9) | |
| Neutral | 444 (58.6) | 289 (56.4) | 155 (63.2) | |
| Negative impact | 276 (36.5) | 193 (37.7) | 83 (33.9) | |
| Medical education productivity | .39 | |||
| Positive impact | 37 (4.9) | 24 (4.7) | 13 (5.3) | |
| Neutral | 461 (60.8) | 304 (59.4) | 157 (63.8) | |
| Negative impact | 260 (34.3) | 184 (35.9) | 76 (30.9) | |
| Domestic work | ||||
| Caring for child(ren) directly | <.01 | |||
| More | 317 (69.4) | 250 (74.2) | 67 (55.8) | |
| Same | 132 (28.9) | 82 (24.3) | 50 (41.7) | |
| Less | 8 (1.7) | 5 (1.5) | 3 (2.5) | |
| Caring for family member(s) other than children | .16 | |||
| More | 158 (32.8) | 111 (35.1) | 47 (28.5) | |
| Same | 305 (63.4) | 196 (62.0) | 109 (66.1) | |
| Less | 18 (3.7) | 9 (2.9) | 9 (5.4) | |
| Managing or providing children's education | .11 | |||
| More | 304 (73.6) | 232 (76.3) | 72 (66.1) | |
| Same | 103 (24.9) | 68 (22.4) | 35 (32.1) | |
| Less | 6 (1.5) | 4 (1.3) | 2 (1.8) | |
| Housework (eg, laundry, cleaning) | <.01 | |||
| More | 332 (44.2) | 249 (48.8) | 83 (34.4) | |
| Same | 396 (52.7) | 242 (47.5) | 154 (63.9) | |
| Less | 23 (3.1) | 19 (3.7) | 4 (1.7) | |
| Self-care (eg, personal time, exercise) | <.01 | |||
| More | 90 (11.9) | 51 (10.0) | 39 (15.9) | |
| Same | 238 (31.6) | 131 (25.7) | 107 (43.7) | |
| Less | 426 (56.5) | 327 (64.2) | 99 (40.4) |
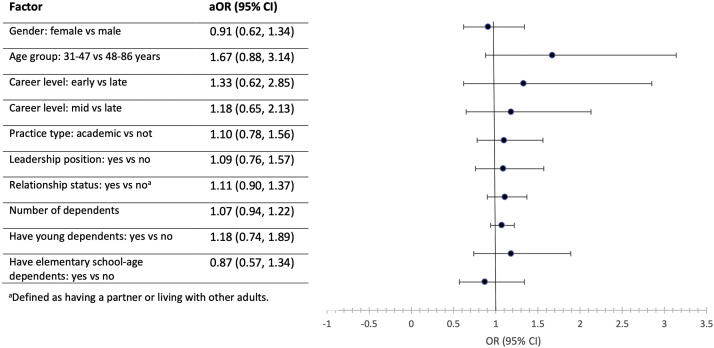
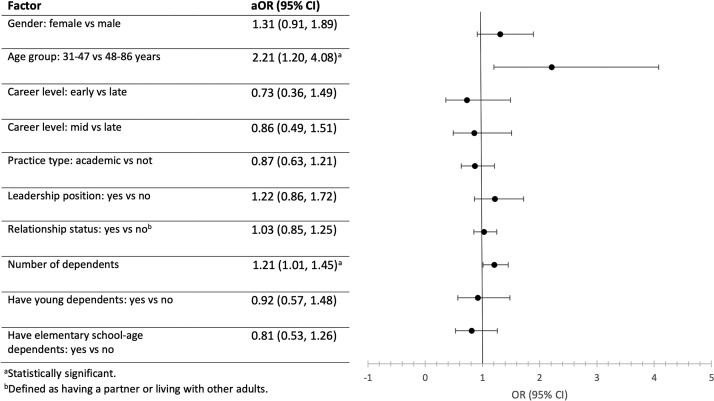
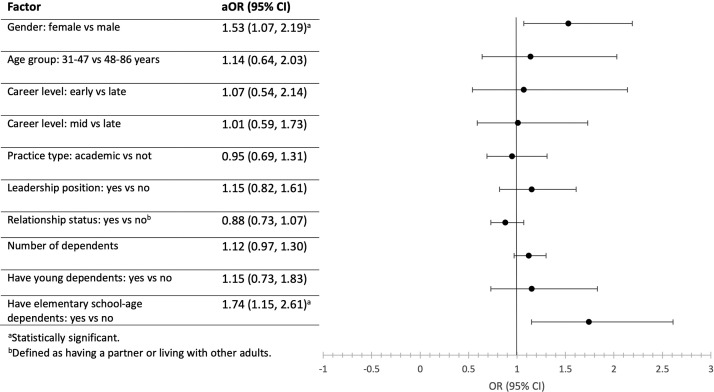
In the multivariable logistic regression analysis, women and men were similar when reporting a reduction in time spent on scholarly work. Although women tended to report a reduction in time spent on scholarly work more frequently than men, this bivariate finding was not statistically significant in the multivariable model (Figure 1; available at www.jpeds.com). A reduction in time spent on career development (Figure 2 ) was associated with younger age (aOR, 2.21; 95% CI, 1.20-4.08) and number of dependents (aOR, 1.21; 95% CI, 1.01-1.45). Women were more likely than men to report this change, but the trend was not statistically significant. Of respondents with children, those with young children and elementary school-age children reported a significant increase in time spent caring for children during the pandemic (aOR, 3.41 [95% CI, 1.58-7.36] and 4.72 [95% CI, 2.55-8.74], respectively). Women were more likely to report an increase in time doing housework (aOR, 1.53; 95% CI, 1.07-2.19) and a reduction in time spent on self-care (aOR, 0.49; 95% CI, 0.29-0.81) (Figure 3 ). No other demographic factors differed significantly in these analyses. C-statistics for the multivariable logistic regression models ranged from 0.60 to 0.76.
Figure 1.
Multivariable analysis of factors associated with reduced time spent on scholarly work (n = 653).
Figure 2.
Multivariable analysis of factors associated with reduced time spent on career development (n = 671).
Figure 3.
Multivariable analysis of factors associated with increased time spent on housework (n = 694).
The survey also indicated that 37.9% of respondents took on new work specifically related to COVID-19, 60% worked more from home, 14% took a leave of absence, and 45% experienced a reduction in salary and/or benefits, with no significant gender differences in these responses. In addition, 31% of respondents reported decreased career satisfaction, and 23% faced new or worsened mental health concerns. Of those respondents scheduled to take the Neonatal-Perinatal Certifying Exam in 2020 (n = 96), 30% deferred. Of those who took the examination, 22% did not pass.
Discussion
This study explored the effects of the COVID-19 pandemic on the neonatology physician workforce. Similar to other medical subspecialties, the neonatology workforce had to adapt to clinical uncertainties and constantly changing management of COVID-19–positive pregnant women and their newborns. Different from some fields, patient care in neonatology did not change significantly in volume, was not elective, and could not be provided remotely during the pandemic, as reflected in our results showing that most neonatologists worked the same or more clinically during this time. Most neonatologists reported a negative impact in important nonclinical domains (scholarly work, medical education, national and institutional service, and career development) during the pandemic. Nearly one-half experienced a reduction in salary or benefits, even though the majority work the same amount or more, and many experienced other negative career impacts (decreased career satisfaction, deferred board-certifying examination) and worsened mental health. The American Board of Pediatrics also reported a decrease in initial certifying examination takers (15%) but similar pass rates in 2020 compared with previous years.52 Studies have highlighted the stress of the pandemic on physician wellness and work–life balance, especially in those who continued to work in person during the pandemic as front-line providers.53 , 54
In addition to professional demands, domestic demands increased. Most neonatologists reported spending the same or more time caring for children, managing children's education, and performing housework, with less time on self-care. We speculate that this intersection of professional and domestic demands contributed to the negative impact in nonclinical domains for neonatologists. These impacts were experienced differently by different segments of the neonatologist workforce. We found the COVID-19 pandemic especially affected early-career neonatologists, those with younger dependents at home, and women, a finding echoed in studies of other subspecialties.6 , 55 The fact that the groups most affected by the pandemic—women of childbearing age and those with children at home33 , 50—represent the largest segment of the pediatric workforce has serious implications for not only individual physicians but the field overall.
Gender-based disparities, such as salary gaps and fewer leadership positions, adversely affected women in neonatology before the pandemic.16 , 22 We found that time spent on career-advancing work (scholarly work and career development) was decreased for women neonatologists since the start of the pandemic. Although the number of self-defined leadership positions in our older age category was similar between genders, the differences in our younger category and that other studies show in the position types and importance level remain concerning.16 , 36 Our gender-related findings were less significant than earlier pandemic reports from other specialties,1 , 6 , 17 , 29 , 56 perhaps due to our comprehensive inclusion of private practice neonatologists who tend to have less proportion of time devoted to scholarly work at baseline. Manuscript submissions increased for some journals in late spring 2020 (personal communication, P. Gallagher, 2021), with the greatest increase among male international authors.29 At baseline, early-career and women neonatologists have fewer primary authored publications20 and may have less protected scholarly time and resources (owing to fewer leadership positions16) and thus may be more affected by the pandemic. Because time spent on professional growth and scholarly work is needed for career advancement, this creates a vicious loop that hinders early career and women neonatologists from progressing their career into leadership positions.
The COVID-19 pandemic disrupted the balance between professional and domestic life, with inadequate support for household and parenting needs.2 , 4 , 7 , 8 , 26 Our study confirms that neonatologists, especially parents and women, faced increased responsibilities at home. Closed daycare centers, difficulty retaining in-home providers for physicians’ children, and home schooling responsibilities related to the pandemic disproportionately affected parents with young children. Caring for aging parents, relatives in long-term care, and ill family members, along with decreases in external household help and time for self-care, were additional burdens. Given that women in our study tended to be younger (and early their career), to have younger dependents, and to have an employed partner compared with men, similar to the prepandemic findings reported by Horowitz et al,16 these domestic effects may have burdened women differentially. Women physicians are at higher risk for burnout at baseline due to domestic demands compounding their professional responsibilities,27 , 48 especially women in intensive care fields.24 The additional domestic and professional stresses posed by the pandemic may increase the risk of burnout in women physicians.4
The number of women entering pediatric careers continues to rise, contributing to a predominance of women in the pediatric workforce.18 Yet gender inequity in medicine contributes to a leaky pipeline, with women's advancement slowed, stalled, or regressing.57 Gender-equity initiatives are driven mostly by underpaid and underrecognized women volunteers, with little institutional recognition or support. As we map our recovery from COVID-19, including women and parents disproportionately affected by COVID-19 as leaders at the decision making table is key. Building a stronger infrastructure to support domestic needs of both men and women, and viewing it as an investment with long-term benefits rather than additional costs, could allow women and parents to remain fully professionally engaged in the workforce. Importantly, this work would not simply support individuals and their careers, but also maximize their clinical and scholarly efforts to advance the care of their patients and the field of neonatology.
This study has some limitations. Our sample might not be truly representative of the complete neonatology physician workforce. The precise numbers, including gender, age, and career path, of actively practicing neonatologists in the US are not tracked comprehensively. More than one-half of neonatologists, three-quarters of recent fellows, and a lower proportion of those aged >60 years old are women (personal communication, AAP, Section of Neonatal Perinatal Medicine, 2021),50 which approximates our sample and allows reasonable generalizability to the population of US neonatologists. We gathered responses from both academic and private practice neonatologists; however, survey engagement was greater from academic neonatology practices. The expectations for research and scholarly productivity may be relevant mainly to neonatologists in academia; however, the negative impact on career development would be similar in both practice settings. Our results may be confounded by respondent bias. Neonatologists who experienced a greater adverse effect of the pandemic may have been more likely to respond to our survey, and those with heavier workloads during the pandemic might not have had time to complete the survey. As with any survey instrument, recall bias also may have impacted the responses. However, the survey was sent out in the fourth quarter of 2020, at which point the effects of the pandemic would have been felt for a long enough period for respondents to give an objective response, but not too distant to affect recall. We did not ask for a direct measure of domestic support but used relationship status as a proxy, while recognizing that its utility is variable and limited.
Our results call for the development of targeted interventions to support postpandemic career recovery, to support individual physicians and advance their contributions to the field.
Data Statement
Data sharing statement available at www.jpeds.com.
Acknowledgments
We thank Patricia Labellarte for her assistance with survey design and Leonardo Barrera for his assistance with statistical analysis and figure construction.
Footnotes
The statistical analysis of study was supported by an AAP, United States Section of Neonatal Perinatal Medicine Strategic Grant. The AAP Section of Neonatal Perinatal Medicine had no role in the design and conduct of the study. The authors declare no conflicts of interest.
Supplementary Data
Appendix
.
References
- 1.Andersen J.P., Nielsen M.W., Simone N.L., Lewiss R.E., Jagsi R. COVID-19 medical papers have fewer women first authors than expected. Elife. 2020;9:e58807. doi: 10.7554/eLife.58807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Minello A. The pandemic and the female academic. Nature. 2020 doi: 10.1038/d41586-020-01135-9. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Northwestern University Organization of Women Faculty Factoring in the pandemic experience to protect gender equity: memorializing the summer of 2020. https://cpb-us-e1.wpmucdn.com/sites.northwestern.edu/dist/0/2419/files/2020/09/OWFCovidExperiences.final_.pdf Accessed June 21, 2021.
- 4.Myers K.R., Tham W.Y., Yin Y., Cohodes N., Thursby J.G., Thursby M.C., et al. Unequal effects of the COVID-19 pandemic on scientists. Nat Hum Behav. 2020;4:880–883. doi: 10.1038/s41562-020-0921-y. [DOI] [PubMed] [Google Scholar]
- 5.Malisch J.L., Harris B.N., Sherrer S.M., Lewis K.A., Shepherd S.L., McCarthy P.C., et al. Opinion: In the wake of COVID-19, academia needs new solutions to ensure gender equity. Proc Natl Acad Sci U S A. 2020;117:15378–15381. doi: 10.1073/pnas.2010636117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferns S.J., Gautam S., Hudak M.L. COVID-19 and gender disparities in pediatric cardiologists with dependent care responsibilities. Am J Cardiol. 2021;147:137–142. doi: 10.1016/j.amjcard.2021.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Del Boca D., Oggero N., Profeta P., Rossi M. Women’s and men’s work, housework and childcare, before and during COVID-19. Rev Econ Househ. 2020;18:1001–1017. doi: 10.1007/s11150-020-09502-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Randell K.A., Patel A.K., Talib H.J. Parenting pressures among academic pediatricians during the COVID-19 pandemic. Pediatrics. 2021;147 doi: 10.1542/peds.2020-033159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al Sulais E., Mosli M., AlAmeel T. The psychological impact of COVID-19 pandemic on physicians in Saudi Arabia: a cross-sectional study. Saudi J Gastroenterol. 2020;26:249–255. doi: 10.4103/sjg.SJG_174_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Isaac C., Petrashek K., Steiner M., Manwell L.B., Byars-Winston A., Carnes M. Male spouses of women physicians: communication, compromise, and carving out time. Qual Rep. 2013;18:1–12. [PMC free article] [PubMed] [Google Scholar]
- 11.Jagsi R., Griffith K.A., Stewart A., Sambuco D., DeCastro R., Ubel P.A. Gender differences in salary in a recent cohort of early-career physician-researchers. Acad Med. 2013;88:1689–1699. doi: 10.1097/ACM.0b013e3182a71519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jolly S., Griffith K.A., DeCastro R., Stewart A., Ubel P., Jagsi R. Gender differences in time spent on parenting and domestic responsibilities by high-achieving young physician-researchers. Ann Intern Med. 2014;160:344–353. doi: 10.7326/M13-0974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keels E.L., Goldsmith J.P., American Academy of Pediatrics Committee on Fetus and Newborn Neonatal provider workforce. Pediatrics. 2019;144 doi: 10.1542/peds.2019-3147. [DOI] [PubMed] [Google Scholar]
- 14.Ly D.P., Seabury S.A., Jena A.B. Differences in incomes of physicians in the United States by race and sex: observational study. BMJ. 2016;353:i2923. doi: 10.1136/bmj.i2923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pearson C., Levine M., Messman A., Chopra T., Awali R., Robb L., et al. Understanding the impact of COVID-19 on physician moms. Disaster Med Public Health Prep. 2021 doi: 10.1017/dmp.2021.49. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Horowitz E., Randis T.M., Samnaliev M., Savich R. Equity for women in medicine–neonatologists identify issues. J Perinatol. 2021;41:435–444. doi: 10.1038/s41372-020-00897-4. [DOI] [PubMed] [Google Scholar]
- 17.Gabster B.P., van Daalen K., Dhatt R., Barry M. Challenges for the female academic during the COVID-19 pandemic. Lancet. 2020;395:1968–1970. doi: 10.1016/S0140-6736(20)31412-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Association of American Medical Colleges 2020 Physician specialty data report. https://www.aamc.org/data-reports/workforce/report/physician-specialty-data-report Accessed June 21, 2021.
- 19.Eloy J.A., Svider P.F., Cherla D.V., Diaz L., Kovalerchik O., Mauro K.M., et al. Gender disparities in research productivity among 9952 academic physicians. Laryngoscope. 2013;123:1865–1875. doi: 10.1002/lary.24039. [DOI] [PubMed] [Google Scholar]
- 20.Fishman M., Williams W.A., 2nd, Goodman D.M., Ross L.F. Gender differences in the authorship of original research in pediatric journals, 2001-2016. J Pediatr. 2017;191:244–249.e1. doi: 10.1016/j.jpeds.2017.08.044. [DOI] [PubMed] [Google Scholar]
- 21.Hill E.K., Stuckey A., Fiascone S., Raker C., Clark M.A., Brown A., et al. Gender and the balance of parenting and professional life among gynecology subspecialists. J Minim Invasive Gynecol. 2019;26:1088–1094. doi: 10.1016/j.jmig.2018.10.020. [DOI] [PubMed] [Google Scholar]
- 22.Horowitz E., Feldman H.A., Savich R. Neonatologist salary: factors, equity and gender. J Perinatol. 2019;39:359–365. doi: 10.1038/s41372-018-0304-7. [DOI] [PubMed] [Google Scholar]
- 23.Adesoye T., Mangurian C., Choo E.K., Girgis C., Sabry-Elnaggar H., Linos E., et al. Perceived discrimination experienced by physician mothers and desired workplace changes: a cross-sectional survey. JAMA Intern Med. 2017;177:1033–1036. doi: 10.1001/jamainternmed.2017.1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burnham E.L., Burns K.E.A., Moss M., Dodek P.M. Burnout in women intensivists: a hidden epidemic? Lancet Respir Med. 2019;7:292–294. doi: 10.1016/S2213-2600(19)30029-3. [DOI] [PubMed] [Google Scholar]
- 25.Kuo I.C., Levine R.B., Gauda E.B., Bodurtha J., Clements J., Fivush B., et al. Identifying gender disparities and barriers to measuring the status of female faculty: the experience of a large school of medicine. J Womens Health (Larchmt) 2019;28:1569–1575. doi: 10.1089/jwh.2018.7610. [DOI] [PubMed] [Google Scholar]
- 26.Nash M., Churchill B. Caring during COVID-19: a gendered analysis of Australian university responses to managing remote working and caring responsibilities. Gend Work Organ. 2020 doi: 10.1111/gwao.12484. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shenoi A.N., Kalyanaraman M., Pillai A., Raghava P.S., Day S. Burnout and psychological distress among pediatric critical care physicians in the United States. Crit Care Med. 2018;46:116–122. doi: 10.1097/CCM.0000000000002751. [DOI] [PubMed] [Google Scholar]
- 28.Spector N.D., Asante P.A., Marcelin J.R., Poorman J.A., Larson A.R., Salles A., et al. Women in pediatrics: progress, barriers, and opportunities for equity, diversity, and inclusion. Pediatrics. 2019;144 doi: 10.1542/peds.2019-2149. [DOI] [PubMed] [Google Scholar]
- 29.Williams W.A., 2nd, Li A., Goodman D.M., Ross L.F. Impact of the coronavirus disease 2019 pandemic on authorship gender in the Journal of Pediatrics: disproportionate productivity by international male researchers. J Pediatr. 2021;231:50–54. doi: 10.1016/j.jpeds.2020.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Woodhams C., Dacre J., Parnerkar I., Sharma M. Pay gaps in medicine and the impact of COVID-19 on doctors’ careers. Lancet. 2021;397:79–80. doi: 10.1016/S0140-6736(20)32671-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Acosta D.A., Lautenberger D.M., Castillo-Page L., Skorton D.J. Achieving gender equity is our responsibility: leadership matters. Acad Med. 2020;95:1468–1471. doi: 10.1097/ACM.0000000000003610. [DOI] [PubMed] [Google Scholar]
- 32.Lautenberger D.M., Dandar V.M. Association of American Medical Colleges; Washington (DC): 2020. The state of women in academic medicine 2018-2019: exploring pathways to equity. [Google Scholar]
- 33.American Academy of Pediatrics, Department of Research American Academy of Pediatrics Periodic Survey (PS) #98: Physcian health and wellness. 2017. https://www.aap.org/en-us/professional-resources/Research/pediatrician-surveys/Pages/periodic-survey-details.aspx?liid=90 Accessed June 21, 2021.
- 34.Jena A.B., Olenski A.R., Blumenthal D.M. Sex differences in physician salary in US public medical schools. JAMA Intern Med. 2016;176:1294–1304. doi: 10.1001/jamainternmed.2016.3284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burden M., Frank M.G., Keniston A., Chadaga S.R., Czernik Z., Echaniz M., et al. Gender disparities in leadership and scholarly productivity of academic hospitalists. J Hosp Med. 2015;10:481–485. doi: 10.1002/jhm.2340. [DOI] [PubMed] [Google Scholar]
- 36.Schor N.F. The decanal divide: women in decanal roles at U.S. medical schools. Acad Med. 2018;93:237–240. doi: 10.1097/ACM.0000000000001863. [DOI] [PubMed] [Google Scholar]
- 37.Lewiss R.E., Silver J.K., Bernstein C.A., Mills A.M., Overholser B., Spector N.D. Is academic medicine making mid-career women physicians invisible? J Womens Health (Larchmt) 2020;29:187–192. doi: 10.1089/jwh.2019.7732. [DOI] [PubMed] [Google Scholar]
- 38.Kang S.K., Kaplan S. Working toward gender diversity and inclusion in medicine: myths and solutions. Lancet. 2019;393:579–586. doi: 10.1016/S0140-6736(18)33138-6. [DOI] [PubMed] [Google Scholar]
- 39.Brubaker L. Women physicians and the COVID-19 pandemic. JAMA. 2020;324:835–836. doi: 10.1001/jama.2020.14797. [DOI] [PubMed] [Google Scholar]
- 40.Jagsi R., Griffith K.A., Stewart A., Sambuco D., DeCastro R., Ubel P.A. Gender differences in the salaries of physician researchers. JAMA. 2012;307:2410–2417. doi: 10.1001/jama.2012.6183. [DOI] [PubMed] [Google Scholar]
- 41.Freund K.M., Raj A., Kaplan S.E., Terrin N., Breeze J.L., Urech T.H., et al. Inequities in academic compensation by gender: a follow-up to the National Faculty Survey cohort study. Acad Med. 2016;91:1068–1073. doi: 10.1097/ACM.0000000000001250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Raj A., Carr P.L., Kaplan S.E., Terrin N., Breeze J.L., Freund K.M. Longitudinal analysis of gender differences in academic productivity among medical faculty across 24 medical schools in the United States. Acad Med. 2016;91:1074–1079. doi: 10.1097/ACM.0000000000001251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jones R.D., Miller J., Vitous C.A., Krenz C., Brady K.T., Brown A.J., et al. The most valuable resource is time: insights from a novel national program to improve retention of physician-scientists with caregiving responsibilities. Acad Med. 2019;94:1746–1756. doi: 10.1097/ACM.0000000000002903. [DOI] [PubMed] [Google Scholar]
- 44.Shanafelt T.D., West C.P., Sinsky C., Trockel M., Tutty M., Satele D.V., et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc. 2019;94:1681–1694. doi: 10.1016/j.mayocp.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 45.Ly D.P., Jena A.B. Sex differences in time spent on household activities and care of children among US physicians, 2003-2016. Mayo Clin Proc. 2018;93:1484–1487. doi: 10.1016/j.mayocp.2018.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Woitowich N.C., Jain S., Arora V.M., Joffe H. COVID-19 threatens progress toward gender equity within academic medicine. Acad Med. 2021;96:813–816. doi: 10.1097/ACM.0000000000003782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Strong E.A., De Castro R., Sambuco D., Stewart A., Ubel P.A., Griffith K.A., et al. Work-life balance in academic medicine: narratives of physician-researchers and their mentors. J Gen Intern Med. 2013;28:1596–1603. doi: 10.1007/s11606-013-2521-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dyrbye L.N., Shanafelt T.D., Balch C.M., Satele D., Sloan J., Freischlag J. Relationship between work-home conflicts and burnout among American surgeons. Arch Surg. 2011;146:211–217. doi: 10.1001/archsurg.2010.310. [DOI] [PubMed] [Google Scholar]
- 49.Starmer A.J., Frintner M.P., Matos K., Somberg C., Freed G., Byrne B.J. Gender discrepancies related to pediatrician work-life balance and household responsibilities. Pediatrics. 2019;144 doi: 10.1542/peds.2018-2926. [DOI] [PubMed] [Google Scholar]
- 50.American Board of Pediatrics, Certification Management System General information on all certified diplomates 2021. https://www.abp.org/content/general-information-all-certified-diplomates Accessed September 8, 2021.
- 51.Hosmer D.W., Jr., Lemeshow S., Sturdivant R.X. 3rd ed. Wiley; Hoboken (NJ): 2013. Applied logistic regression. [Google Scholar]
- 52.American Board of Pediatrics Initial certifying examination first-time taker passing rates 2021. https://www.abp.org/sites/abp/files/pdf/exam-pass-rates-init-cert.pdf Accessed September 8, 2021.
- 53.Chew N.W.S., Lee G.K.H., Tan B.Y.Q., Jing M., Goh Y., Ngiam N.J.H., et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Giusti E.M., Pedroli E., D'Aniello G.E., Stramba Badiale C., Pietrabissa G., Manna C., et al. The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front Psychol. 2020;11:1684. doi: 10.3389/fpsyg.2020.01684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yule A.M., Ijadi-Maghsoodi R., Bagot K.S., Bath E. Support for early career female physician-scientists as part of the COVID-19 Recovery Plan. Acad Med. 2021;96:e16–e17. doi: 10.1097/ACM.0000000000003891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pinho-Gomes A.C., Peters S., Thompson K., Hockham C., Ripullone K., Woodward M., et al. Where are the women? Gender inequalities in COVID-19 research authorship. BMJ Glob Health. 2020;5:1–4. doi: 10.1136/bmjgh-2020-002922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Moak T.N., Cress P.E., Tenenbaum M., Casas L.A. The leaky pipeline of women in plastic surgery: embracing diversity to close the gender disparity gap. Aesthet Surg J. 2020;40:1241–1248. doi: 10.1093/asj/sjz299. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.