Abstract
Background
Hypertension is one of the most common noncommunicable diseases affecting several individuals globally. However, the level of nonadherence to self-care practices, antihypertensive medications, and associated factors among hypertensive patients in a follow-up clinic at Asella Referral and Teaching Hospital is unknown.
Objective
To assess the level of nonadherence to self-care practices, antihypertensive medications, and associated factors among hypertensive patients in a follow-up clinic at Asella Referral and Teaching Hospital, Arsi Zone, Oromia Regional State, Ethiopia, in 2020.
Methods
An institution-based cross-sectional survey was conducted on 115 hypertensive patients who visited the follow-up clinic at Asella Referral and Teaching Hospital from December 24, 2020, to January 15, 2021. Data were entered into EpiData version 4.2.0.0 and exported to SPSS version 21.0 for statistical analysis. Binary and multivariable logistic regression analysis was used to assess the presence of statistical association between dependent and independent variables.
Results
A total of 115 hypertensive patients were enrolled into the study, giving a response rate of 98.29%. The mean age of the study participants was 55.17 years (SD = 17.986). More than half of them (59 (51.3%)) were females. More than half of them (58 (50.4%)) were married. Nearly two-thirds of them (79 (68.7%)) had formal education. The level of nonadherence to self-care practices was 67.0% (n = 77, 95% CI: 60.0, 75.7). Meanwhile, the patient's level of nonadherence to antihypertensive medications was 16.5% (n = 19, 95% CI: 10.4, 24.3). The multivariable logistic regression analysis showed that age >45 years (AOR = 2.89, 95% CI: 1.16, 7.18), having no formal education (AOR = 1.67, 95% CI: 1.32, 3.74), and having ≤5 years' duration since diagnoses of hypertension (AOR = 1.56, 95% CI: 1.07, 3.25) were factors significantly associated with nonadherence to self-care practices. Being male (AOR = 2.09, 95% CI: 1.93, 9.59), being married (AOR = 4.22, 95% CI: 1.29, 13.76), and having an average monthly income of ≤2500 ETB (AOR = 1.58, 95% CI: 1.09, 7.08) were factors significantly associated with nonadherence to medications.
Conclusion
In the present study, the level of both nonadherence to self-care practices and antihypertensive medications was relatively high. There is a need to initiate programs that could create awareness about adherence to self-care practices and antihypertensive medications among hypertensive patients to improve their level of adherence.
1. Background
Hypertension is a higher systemic blood pressure (BP) that leads to an obvious upsurge of cardiovascular risk [1]. Resistant hypertension is linked to an augmented risk of cardiovascular disease (CVD) [2]. The relationship between BP and the risk of CVD is not depending on other risk factors [3]. CVDs were the main cause of morbidity and mortality in Ethiopia [4]. Hypertension is a worldwide community health problem [5]. It is a community health problem and is not well controlled [6]. It is upsetting approximately 1 billion individuals worldwide [7]. It remains as a giant community health and economic burden worldwide [8]. It is one of the world's most fatal diseases [9].
The magnitude of hypertension is growing in Africa. However, people were not aware of their situation [10]. In Africa, there were poor awareness, treatment, and control of hypertension [11]. Hypertension is a substantial public health test globally and this condition should acquire high priority [12]. Supportive efforts are instantaneously compulsory to fight the developing hypertension burden [13]. BP dropping markedly declines vascular risk and comorbidities [14].
The probable causes of uncontrolled BP were poor medication adherence, lack of information about hypertension, and side effects [15]. A steady medication adherence is a crucial factor to sustained BP control. Healthcare providers require understanding the main clues related to suboptimal adherence or nonadherence that can lead to poor outcomes [16]. In turn, nonadherence to antihypertensive medications was related to an augmented risk of stroke [17]. Low adherence to antihypertensive medications remains a population health burden. Knowing the barriers and determinants, factors of adherence to antihypertensive medication may benefit and recognize interventions to increase adherence [18].
The strategies to decrease BP in the high-risk population should be a national priority [2]. Healthy lifestyle recommendations play a significant role in controlling BP [19]. This is evidenced by adherence to a healthy lifestyle which is associated with a lower risk of hypertension [20]. When used effectively, lifestyle modifications have a significant role in the management of hypertension [21]. A long-term adherence to antihypertensive medication has verified the importance [22]. Furthermore, compliance with antihypertensive medications was found to be improved after providing education about hypertension and its related complications [23]. Counseling hypertensive individuals towards adherence to medication and the public with suitable information about hypertension management would improve the patient's level of adherence [24]. In addition to this, to decrease hypertension related morbidity and mortality, identifying individuals at risk of nonadherence to treatment and poor blood pressure control can lead to targeted interventions [25].
As explained overhead, the burden of hypertension is increasing worldwide. Gaining information concerning the level of nonadherence to self-care practices, medications, and associated factors will be used as integrated management in managing and controlling hypertension. Since the present study has determined the level of nonadherence to self-care practices, medications, and associated factors among hypertensive patients, the result would aware the hospitals, healthcare professionals, government stakeholders, and researchers.
2. Objectives
2.1. General Objective
The general objective is to assess the level of nonadherence to self-care practices, antihypertensive medications, and associated factors among hypertensive patients in a follow-up clinic at Asella Referral and Teaching Hospital, Arsi Zone, Oromia Regional State, Ethiopia, in 2020.
2.2. Specific Objectives
To determine the level of nonadherence to self-care practices among hypertensive patients in follow-up clinics at Asella Referral and Teaching Hospital, Arsi Zone, Oromia Regional State, Ethiopia, in 2020
To determine the level of nonadherence to antihypertensive medications among hypertensive patients in follow-up clinics at Asella Referral and Teaching Hospital, Arsi Zone, Oromia Regional State, Ethiopia, in 2020
To identify factors associated with nonadherence to self-care practices among hypertensive patients in follow-up clinics at Asella Referral and Teaching Hospital, Arsi Zone, Oromia Regional State, Ethiopia, in 2020
To identify factors associated with nonadherence to antihypertensive medications among hypertensive patients in follow-up clinics at Asella Referral and Teaching Hospital, Arsi Zone, Oromia Regional State, Ethiopia, in 2020
3. Methods
3.1. Study Area and Period
The study was conducted in Asella Referral and Teaching Hospital from December 24, 2020, to January 15, 2021. Asella Referral and Teaching Hospital is located in Asella town which is located about 175 KMs southeast from Addis Ababa, the capital city of Ethiopia [26].
3.2. Study Design
An institution-based cross-sectional survey was conducted at Asella Referral and Teaching Hospital.
3.3. Source Population
The source population was all hypertensive patients who visited the follow-up clinic at Asella Referral and Teaching Hospital.
3.4. Study Population
The study population was all hypertensive patients who visited the follow-up clinic at Asella Referral and Teaching Hospital and fulfilled the inclusion criteria.
3.5. Eligibility Criteria
3.5.1. Inclusion Criteria
Inclusion criteria included all hypertensive patients aged ≥18 years.
3.5.2. Exclusion Criteria
Hypertensive patients who were severely ill and physically unable to be interviewed at the time of data collection were excluded.
3.6. Sample Size Determination
Survey was conducted among hypertensive patients who visited the follow-up clinic at Asella Referral and Teaching Hospital. Since the survey was undertaken, all hypertensive patients attending the follow-up clinic at Asella Referral and Teaching Hospital were included in the study. The final sample size was 115 (n = 115).
3.7. Sampling Technique and Procedures
During the survey, the hypertensive patient was checked using the medical registration card. Afterwards, all hypertensive patients present on the day of the survey and who were willing to participate in the survey were included in the study.
3.8. Study Variables
3.8.1. Dependent Variable
Nonadherence to self-care practices
Nonadherence to antihypertensive medications
3.8.2. Independent Variables
Sociodemographic variables are gender, age, religion, ethnicity, marital status, educational level, occupation, and average monthly income. Health-related factors include comorbidity and duration since diagnosed hypertension.
3.9. Operational Definitions
Adherence to self-care practices is when the patient scored the mean or above mean score [27]. Nonadherence to self-care practices is when the patient scored below the mean score [27].
3.10. Data Collection Instrument
The questionnaire was adapted and developed from relevant literatures with modification fit to the local context [27–32]. During this, various experts were involved in it. The questionnaire was prepared in English and translated to Afan Oromo and finally translated back to English to maintain consistency.
3.11. Data Collection Procedures
A semistructured interviewer-administered questionnaire and patients' medical records review was used to collect data. Data were collected by four nurses with Bachelor of Science degree, and the study was supervised by one nurse with Master of Science degree.
3.12. Data Quality Control
The questionnaire was pretested on 5% of the sample size. Data collectors were trained for one day on the data collection instrument and data collection procedure. The reliability of the questionnaire was checked by reliability analysis and Cronbach's alpha value was 0.79 which suggested a reliable tool. During the data collection period, a close supervision was done by the supervisor.
3.13. Data Processing and Analysis
Data was checked, coded, and entered into EpiData version 4.2.0.0, and then it was exported to Statistical Package for the Social Sciences (SPSS) version 21.0 (IBM Corporation, North Castle Drive, Armonk, NY, USA) for statistical analysis. The outcome variable was dichotomized and coded as 0 and 1 representing adherence and nonadherence, respectively. Texts, tables, and figures were used to summarize the descriptive statistics.
Both bivariable and multivariable logistic regression analyses were carried out to find the variables associated with the dependent variables. Both the crude odds ratios (COR) and adjusted odds ratio (AOR) with the corresponding 95% confidence were determined to show the strength of the association. Finally, variables with P value <0.05 in the multivariable logistic regression were considered as statistically significant.
4. Results
4.1. Sociodemographic Characteristics of Study Participants
In the present study, a total of 115 hypertensive patients were enrolled into the study, giving a response rate of 98.29%. The mean age of the patients was 55.17 years (SD = 17.986), while the majority of the patients (72 (62.6%)) were aged >45 years. More than half of the patients (59 (51.3%)) were females. Regarding religion, 58 patients (50.4%) were Muslims. The majority of patients (80 (69.6%)) were Oromo by ethnic background. More than half of the patients (58 (50.4%)) were married. Nearly two-thirds of the patients (79 (68.7%)) had formal education (Table 1).
Table 1.
Sociodemographic characteristics of hypertensive patients in a follow-up clinic of Asella Referral and Teaching Hospital, Asella Town, Arsi Zone, Oromia Regional State, Ethiopia, 2020 (n = 115).
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Gender | Male | 56 | 48.7 |
| Female | 59 | 51.3 | |
|
| |||
| Age | ≤45 years | 43 | 37.4 |
| >45 years | 72 | 62.6 | |
|
| |||
| Religion | Orthodox | 41 | 35.7 |
| Muslim | 58 | 50.4 | |
| Protestant | 15 | 13.0 | |
| Catholic | 1 | 0.9 | |
|
| |||
| Ethnicity | Oromo | 80 | 69.6 |
| Amhara | 25 | 21.7 | |
| Gurage | 6 | 5.2 | |
| Others | 4 | 3.5 | |
|
| |||
| Marital status | Married | 58 | 50.4 |
| Unmarried | 57 | 49.6 | |
|
| |||
| Educational level | No formal education | 36 | 31.3 |
| Formal education | 79 | 68.7 | |
|
| |||
| Occupation | Employed | 60 | 52.2 |
| Unemployed | 55 | 47.8 | |
|
| |||
| Average monthly income | ≤2500 ETB | 73 | 63.5 |
| >2500 ETB | 42 | 36.5 | |
4.2. Health-Related Factors
Among the study participants, 75 (65.2%) were ≤5 years since diagnosis with hypertension. 52 (45.2%) of them have been on hypertensive treatment for four or more years. Regarding the number of types of medications, 108 (93.9%) of them took less than or equal to the two types of medications. Furthermore, 23 (20.0%) of them reported that they had comorbidities, such as diabetics (43.5%), stroke (30.5%), and chronic kidney disease (13.0%) (Table 2).
Table 2.
Health related factors among hypertensive patients in a follow-up clinic of Asella Referral and Teaching Hospital, Asella Town, Arsi Zone, Oromia Regional State, Ethiopia, 2020 (n = 115).
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Duration since diagnosis | ≤5 years | 75 | 65.2 |
| >5 years | 40 | 34.8 | |
|
| |||
| Duration of antihypertensive treatment | Less than two years | 16 | 13.9 |
| Two to four years | 47 | 40.9 | |
| Four or more years | 52 | 45.2 | |
|
| |||
| Number of types of medications | ≤Two | 108 | 93.9 |
| >Two | 7 | 6.1 | |
|
| |||
| Presence of comorbidities | Yes | 23 | 20.0 |
| No | 92 | 80.0 | |
|
| |||
| Diagnosed comorbidities (n = 23) | Diabetes mellitus | 10 | 43.5 |
| Chronic kidney disease | 3 | 13.0 | |
| Stroke | 5 | 21.7 | |
| Chronic heart diseases | 2 | 8.7 | |
4.3. Adherence to the Components of Self-Care Practices
4.3.1. Adherence to Dietary Modifications
Among the study participants, 50 (43.5%) of them reported that they had rarely included fruits, vegetables, grains, and beans in their diet after they were diagnosed with hypertension. Moreover, nearly more than half of them (58 (50.4%)) reported that they had rarely consumed foods that contain high saturated fat such as cheese, coconut oil, cotton seed oil, and mutton fat since being diagnosed. Furthermore, 66 (57.4%) of them never consumed spicy foods since they were diagnosed. 64 (55.7%) of them never consumed salt in their foods. 80 (69.6%) of them never read nutritional facts on food labels to compare the amount of sodium in the products (Table 3).
Table 3.
Adherence to dietary modifications among hypertensive patients in a follow-up clinic of Asella Referral and Teaching Hospital, Asella Town, Arsi Zone, Oromia Regional State, Ethiopia, 2020 (n = 115).
| Variables | Responses | |||
|---|---|---|---|---|
| Never | Rarely | Usually | Always | |
| Included fruit, vegetables, grains, and beans in their diet after being diagnosed with hypertension | 37 (32.2%) | 50 (43.5%) | 22 (19.1%) | 6 (5.2%) |
| Consumed foods that contain high saturated fat | 49 (42.6%) | 58 (50.4%) | 6 (5.2%) | 2 (1.7%) |
| Consumed spicy foods since being diagnosed | 66 (57.4%) | 42 (36.5%) | 3 (2.6%) | 4 (3.5%) |
| Consumed salt in their food | 64 (55.7%) | 29 (25.2%) | 12 (10.4%) | 10 (8.7%) |
| Read nutritional facts on food labels to compare amount of sodium in products | 80 (69.6%) | 26 (22.6%) | 4 (3.5%) | 5 (4.3%) |
4.3.2. Adherence to Exercise
The majority of the participants (98 (85.2%)) answered that they performed physical exercise. Regarding the frequency of performing physical exercise, 47 (48.0%) of them performed physical exercise more than three times per week. Walking (69.4%), jogging (25.5%), and cycling (5.1%) were the major types of exercise performed by these hypertensive patients. Regarding the duration of performing physical exercise, 52 (53.1%) of them reported less than 30 minutes (Table 4).
Table 4.
Adherence to exercise among hypertensive patients in a follow-up clinic of Asella Referral and Teaching Hospital, Asella Town, Arsi Zone, Oromia Regional State, Ethiopia, 2020 (n = 115).
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Perform physical exercise (N = 115) | Yes | 98 | 85.2 |
| No | 17 | 14.8 | |
|
| |||
| How often do you exercise? (N = 98) | <Three times per week | 30 | 30.6 |
| Three times per week | 21 | 21.4 | |
| >Three times per week | 47 | 48.0 | |
|
| |||
| Types of exercise performed (N = 98) | Walking | 68 | 69.4 |
| Jogging | 25 | 25.5 | |
| Cycling | 5 | 5.1 | |
|
| |||
| Duration of exercise per session | <30 minutes | 52 | 53.1 |
| >30 minutes | 46 | 46.9 | |
4.3.3. Adherence to Cessation of Smoking
The majority of hypertensive patients (96 (83.5%)) never used tobacco. Among those cigarette smokers, 8 (42.1%) of them were still smokers and 6 (75%) of them tried to quit smoking (Table 5).
Table 5.
Adherence to cessation of smoking among hypertensive patients in a follow-up clinic of Asella Referral and Teaching Hospital, Asella Town, Arsi Zone, Oromia Regional State, Ethiopia, 2020 (n = 115).
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Ever used tobacco (N = 115) | Yes | 19 | 16.5 |
| No | 96 | 83.5 | |
|
| |||
| Still smoking cigarettes (N = 19) | Yes | 8 | 42.1 |
| No | 11 | 57.9 | |
|
| |||
| Ever tried to quit smoking (N = 8) | Yes | 6 | 75.0 |
| No | 2 | 25.0 | |
4.3.4. Adherence to Moderation of Alcohol Consumption
The majority of hypertensive patients (98 (85.2%)) never consumed alcohol even on occasion. Most of them (97 (84.3%)) reported that they were advised to cut down drinking alcohol by relatives/friends/doctors/health workers (Table 6).
Table 6.
Adherence to moderation of alcohol consumption among hypertensive patients in a follow-up clinic of Asella Referral and Teaching Hospital, Asella Town, Arsi Zone, Oromia Regional State, Ethiopia, 2020 (n = 115).
| Variables | Never | <1 month | Monthly | Weekly | Daily |
|---|---|---|---|---|---|
| How often do you have 8 drinks (men)/6 drinks (women) or more on occasion? | 98 (85.2%) | 8 (7.0%) | 4 (3.5%) | 4 (3.5%) | 1 (0.9%) |
| How often in the last year have you not been able to remember what happened when drinking the night before? | 112 (97.4%) | 2 (1.7%) | 0 (0) | 1 (0.9%) | 0 (0) |
| Has a relative/friend/doctor/health worker been concerned about your drinking or advised you to cut down on your drinking? | Yes | 97 (84.3%) | |||
| No | 18 (15.7%) | ||||
4.4. Level of Nonadherence to Self-Care Practices
The level of nonadherence to self-care practices was 67.0% (n = 77, 95% CI: 60.0, 75.7) (Figure 1).
Figure 1.
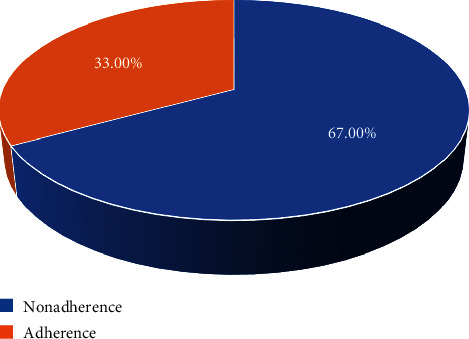
The level of nonadherence to self-care practices among hypertensive patients in a follow-up clinic at Asella Referral and Teaching Hospital, Asella Town, Arsi Zone, Oromia Regional State, Ethiopia, 2020 (n = 115).
4.5. Level of Nonadherence to Antihypertensive Medications
The patients' level of nonadherence to antihypertensive medications was 16.5% (n = 19, 95% CI: 10.4, 24.3) (Figure 2).
Figure 2.
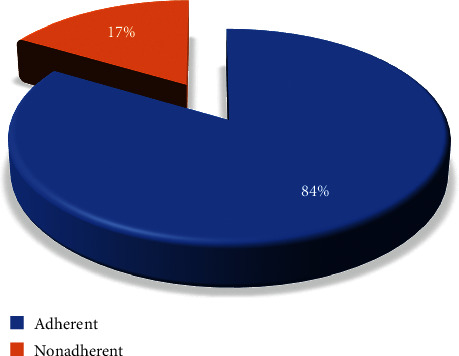
The level of nonadherence to antihypertensive medications among hypertensive patients in a follow-up clinic at Asella Referral and Teaching Hospital, Asella Town, Arsi Zone, Oromia Regional State, Ethiopia, 2020 (n = 115).
4.6. Factors Associated with Nonadherence to Self-Care Practices
To identify independent factors associated with nonadherence to self-care practices, gender, age, marital status, educational level, occupation, average monthly income, duration since diagnosis, and comorbidities were entered into both binary and multivariable logistic regression analyses. However, only age, educational level, and duration since diagnosis were factors significantly associated with nonadherence to self-care practices.
The odds ratio of having nonadherence to self-care practices among hypertensive patients who were aged >45 years was 2.89 times (AOR = 2.89, 95% CI: 1.16, 7.18) higher than hypertensive patients who were aged ≤45 years. Likewise, the likelihood of having nonadherence to self-care practices among hypertensive patients who had no formal education was 1.67 times (AOR = 1.67, 95% CI: 1.32, 3.74) more when compared with those who had a formal education. Those hypertensive patients who had ≤5 years' duration since diagnosis of hypertension were 1.56 times (AOR = 1.56, 95% CI: 1.07, 3.25) more likely to have nonadherence to self-care practices when compared to hypertensive patients who had >5 years' duration since diagnosis of hypertension (Table 7).
Table 7.
Bivariable and multivariable analysis of factors associated with nonadherence to self-care practices among hypertensive patients in a follow-up clinic at Asella Referral and Teaching Hospital, Asella Town, Arsi Zone, Oromia Regional State, Ethiopia, 2020.
| Variables | Categories | Self-care practices | COR (95% CI) | AOR (95% CI) | P value | |
|---|---|---|---|---|---|---|
| Adherence | Nonadherence | |||||
| Gender | Male | 20 (35.7%) | 36(64.3%) | 1 | 1 | |
| Female | 18 (30.5%) | 41(69.5%) | 1.27(0.58, 2.76) | 1.36(0.56, 3.20) | 0.487 | |
|
| ||||||
| Age in years | ≤45 | 21 (48.8%) | 22(51.2%) | 1 | 1 | |
| >45 | 17 (23.6%) | 55 (76.4%) | 3.09 (1.38, 6.93) | 2.89 (1.16, 7.18) | 0.023 | |
|
| ||||||
| Marital status | Unmarried | 16 (28.1%) | 41 (71.9%) | 1.57 (0.72, 3.43) | 1.76 (0.76, 4.11) | 0.189 |
| Married | 22 (37.9%) | 36 (62.1%) | 1 | 1 | ||
|
| ||||||
| Educational status | No formal education | 9 (25%) | 27 (75%) | 1.74 (0.72, 4.20) | 1.67 (1.32, 3.74) | 0.034 |
| Formal education | 29 (36.7%) | 50 (63.3%) | 1 | 1 | ||
|
| ||||||
| Occupation | Unemployed | 20 (36.4%) | 35 (63.6%) | 0.75 (0.34, 1.63) | 0.62 (0.22, 1.71) | 0.352 |
| Employed | 18 (30%) | 42 (70%) | 1 | 1 | ||
|
| ||||||
| Average monthly income | ≤2500 ETB | 22 (30.1%) | 51 (69.9%) | 1.43 (0.64, 3.17) | 1.30 (0.49, 3.43) | 0.591 |
| >2500 ETB | 16 (38.1%) | 26 (61.9%) | 1 | 1 | ||
|
| ||||||
| Duration since diagnoses | ≤5 years | 23 (30.7%) | 52 (69.3%) | 1.36 (0.61, 3.04) | 1.56 (1.07, 3.25) | 0.042 |
| >5 years | 15 (37.5%) | 25 (62.5%) | 1 | 1 | ||
|
| ||||||
| Presence of comorbidities | Yes | 9 (39.1%) | 14 (60.9%) | 1 | 1 | |
| No | 29 (31.5%) | 63 (68.5%) | 1.40 (0.54, 3.59) | 1.61 (0.58, 4.49) | 0.362 | |
4.7. Factors Associated with Nonadherence to Antihypertensive Medications
Likewise, to identify independent factors associated with nonadherence to medications, gender, age, marital status, educational level, occupation, average monthly income, duration since diagnosis, and comorbidities were entered into both bivariable and multivariable logistic regression analyses. However, only gender, marital status, and average monthly income were factors significantly associated with nonadherence to antihypertensive medications.
The odds ratio of having nonadherence to antihypertensive medications among hypertensive patients who were male was 2.09 times (AOR = 2.09, 95% CI: 1.93, 9.59) higher than hypertensive patients who were female. Those hypertensive patients who were married were 4.22 times (AOR = 4.22, 95% CI: 1.29, 13.76) more likely to have nonadherence to medications when compared to hypertensive patients who were unmarried. Furthermore, the likelihood of having nonadherence to medications among hypertensive patients who had an average monthly income of ≤2500 ETB was 1.58 times (AOR = 1.58, 95% CI: 1.09, 7.08) more when compared with those who had a >2500 ETB average monthly income (Table 8).
Table 8.
Bivariable and multivariable analysis of factors associated with nonadherence to antihypertensive medications among hypertensive patients in a follow-up clinic at Asella Referral and Teaching Hospital, Asella Town, Arsi Zone, Oromia Regional State, Ethiopia, 2020 (n = 115).
| Variables | Categories | Medications | COR (95% CI) | AOR (95% CI) | P value | |
|---|---|---|---|---|---|---|
| Adherence | Nonadherence | |||||
| Gender | Male | 43 (76.8%) | 13 (23.2%) | 2.67 (0.94,7.61) | 2.09 (1.93,9.59) | 0.035 |
| Female | 53 (89.8%) | 6 (10.2%) | 1 | 1 | ||
|
| ||||||
| Age in years | ≤45 | 35 (81.4%) | 8 (18.6%) | 1.27 (0.47,3.45) | 1.55 (0.45,5.29) | 0.487 |
| >45 | 61 (84.7%) | 11 (15.3%) | 1 | 1 | ||
|
| ||||||
| Marital status | Unmarried | 52 (91.2%) | 5 (8.8%) | 1 | 1 | |
| Married | 44 (75.9%) | 14 (24.1%) | 3.31 (1.11,9.91) | 4.22 (1.29,13.76) | 0.017 | |
|
| ||||||
| Educational status | No formal education | 30 (83.3%) | 6 (16.7%) | 1.02 (0.35,2.93) | 0.95 (0.27,3.36) | 0.936 |
| Formal education | 66 (83.5%) | 13 (16.5%) | 1 | 1 | ||
|
| ||||||
| Occupation | Unemployed | 44 (80%) | 11 (20%) | 1.63 (0.60,4.39) | 2.03 (0.54,7.66) | 0.296 |
| Employed | 52 (86.7%) | 8 (13.3%) | 1 | 1 | ||
|
| ||||||
| Average monthly income | ≤2500 ETB | 59 (80.8%) | 14 (19.2%) | 1.76 (0.58,5.28) | 1.58 (1.09,7.08) | 0.041 |
| >2500 ETB | 37 (88.1%) | 5 (11.9%) | 1 | 1 | ||
|
| ||||||
| Duration since diagnosis | ≤5 years | 63 (84%) | 12 (16%) | 0.89 (0.32,2.49) | 0.84 (0.27,2.66) | 0.769 |
| >5 years | 33 (82.5%) | 7 (17.5%) | 1 | 1 | ||
|
| ||||||
| Presence of comorbidities | Yes | 16 (69.6%) | 7 (30.4%) | 2.92 (0.99,8.55) | 2.76 (0.83,9.15) | 0.097 |
| No | 80 (87%) | 12 (13%) | 1 | 1 | ||
5. Discussion
Ensuring hypertensive patients' adherence to medications and self-care practices to manage and prevent complications of hypertension remains a major challenge to public health globally. Poor adherence to treatment is a reason for uncontrolled hypertension, serious complications, and wastage of healthcare resources. The present study determined the level of nonadherence to self-care practices, antihypertensive medications, and associated factors among hypertensive patients in the follow-up clinic at Asella Referral and Teaching Hospital, Ethiopia.
5.1. Nonadherence to Self-Care Practices and Associated Factors
The patients' level of nonadherence to self-care practices was 67.0% (n = 77, 95% CI: 60.0, 75.7). The present study's finding was lower when compared with a study done in Addis Ababa, Ethiopia (77%) [27]. The variation might be due to the duration since the study was conducted, while the study of Addis Ababa was done in 2016. Within this long duration, there could be a lot of information dissemination through different sources such as mass media and newspapers. The present study's finding was also lower when compared with a study done in Dessie Referral Hospital, Ethiopia (76.4%) [33]. The possible justification could be the differences in sociodemographic characteristics of the study participants. However, the present study's finding was higher when compared with a study conducted in Harari Region, Ethiopia (37.9%) [34]. This might be due to the differences in sociodemographic characteristics of the study participants.
The odds ratio of having nonadherence to self-care practices among hypertensive patients who were aged >45 years was 2.89 times (AOR = 2.89, 95% CI: 1.16, 7.18) higher than hypertensive patients who were aged ≤45 years. The likelihood of having a nonadherence to self-care practices among hypertensive patients who had no formal education was 1.67 times (AOR = 1.67, 95% CI: 1.32, 3.74) more when compared with those who had a formal education. In fact, education has the power to create awareness for patients concerning disease seriousness. Those hypertensive patients who had ≤5 years' duration since diagnosis of hypertension were 1.56 times (AOR = 1.56, 95% CI: 1.07, 3.25) more likely to have nonadherence to self-care practices when compared to hypertensive patients who had >5 years' duration since diagnosis of hypertension.
5.2. Nonadherence to Antihypertensive Medication and Associated Factors
The patients' level of nonadherence to antihypertensive medications was 16.5% (n = 19, 95% CI: 10.4, 24.3). The present study's finding was also lower when compared with a study done in Nedjo, Ethiopia (68.6%) [30]. This might be the length since the study was conducted, which was from March 15 to May 5, 2015, for the study done in Nedjo. In fact, through this duration of time, there could be a change in the treatment protocol and there might be involvement of the mass media on the awareness and creation of the disease and pharmacologic treatment.
The present study's finding was lower when compared with a study done in Buea, Cameroon (67.7%) [28]. This might be due to the differences in the sociodemographic characteristics of the study participants. Besides, there are differences in the study setting, while the study done in Buea, Cameroon, was a community-based study. The present study's finding was also lower when compared with a multicenter study done in Ghana and Nigeria (66.7%) [31]. This might be due to the length of duration since the study was done, which was from April to September 2013 for the study done in Ghana and Nigeria. Besides, the differences in the sociodemographic characteristics of the study participants could play a significant role in this variation.
The present study's finding was also lower when compared with a study done in Kinshasa, Democratic Republic of Congo (54.2%) [35]. This might be due to the differences in sociodemographic characteristics of the study participants. The present study's finding was also lower when compared with a study done in Nigeria (45.8%) [36]. The present study's finding was also lower when compared with a study done in Brazil (71%) [29]. This might be due to the length of duration since the study was done, where the study of Brazil was done from November 2012 to April 2013. The present study's finding was consistent when compared with a study done in Korea (13.2%) [32].
The odds ratio of having nonadherence to medications among hypertensive patients who were male was 2.09 times (AOR = 2.09, 95% CI: 1.93, 9.59) higher than hypertensive patients who were female. Those hypertensive patients who were married were 4.22 times (AOR = 4.22, 95% CI: 1.29, 13.76) were more likely to have nonadherence to medications when compared to hypertensive patients who were unmarried. The likelihood of having nonadherence to medications among hypertensive patients who had an average monthly income of ≤2500 ETB was 1.58 times (AOR = 1.58, 95% CI: 1.09, 7.08) more when compared with those who had a >2500 ETB average monthly income. The present study's finding was supported by the study done in Nedjo, Ethiopia [30]. This might be due to the scarcity of money which could affect the expense of transport and accessibility to sources of information such as mass media and newspapers. Meanwhile, in turn, these could influence the level of adherence to antihypertensive medications.
6. Conclusion
In the present study, the hypertensive patients' level of nonadherence to self-care practices was 67.0%. Meanwhile, the patients' level of nonadherence to antihypertensive medications was 16.5%. The multivariable logistic regression analysis showed that age, educational level, and duration since diagnosis were factors significantly associated with nonadherence to self-care practices, whereas gender, marital status, and average monthly income were factors significantly associated with nonadherence to medications.
Moreover, the present study offers significant information to motivate the public for their health concerns. Ensuring hypertensive patients' adherence to self-care practices and antihypertensive medications to manage and prevent complications of hypertension is the foundation method. This is because nonadherence to self-care practices and medications is a principal reason for uncontrolled hypertension, serious complications, and wastage of healthcare resources. Thus, the findings of the present study also give a basis to support healthcare providers to consider hypertension management and encourage them to focus on it and design methods to address this problem. Finally, we suggest that there is a need to initiate programs that could create awareness about adherence to self-care practices and antihypertensive medications among hypertensive patients to improve their level of adherence.
6.1. Limitations of the Study
The present study had some limitations. The first limitation was the study design we have used, which was a cross-sectional survey. Another is there was a scarcity of the studies undertaken, which affects the discussion of various variables of the present study. Hopefully, the present study could minimize such challenges being baseline for the researchers who wish to discuss this topic in the future.
Acknowledgments
The authors would like to thank the participating supervisors, data collectors, patients, Asella Referral and Teaching Hospital, and Arsi University.
Data Availability
The data used to support the findings of this study are available upon request from the corresponding author.
Ethical Approval
The ethical clearance was approved by Nursing Department on behalf of the Institutional Ethical Review Board of Arsi University. The letter of permission was sent to Asella Referral and Teaching Hospital, and permission was obtained. The study participants were informed about the significance and objectives of the study prior to data collection. For the reason of privacy and confidentiality, personal identifiers were not used. The study participants were also informed that they have the right to withdraw from the study at any phase. Besides, all protocols were carried out in accordance with relevant guidelines and regulations.
Consent
Verbal informed consent was obtained from the study participants.
Conflicts of Interest
The authors declare no conflicts of interest.
Authors' Contributions
All authors have contributed to the conception of the study, data analysis, and drafting or revising the article, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
References
- 1. Guidelines on Clinical and Programmatic Management of Major Non Communicable Diseases: Federal Democratic Republic of Ethiopia Ministry of Health: Addis Ababa . 2016. https://extranet.who.int/ncdccs/Data/ETH_D1_National%20NCD%20Guideline%20June%2010,%202016%20for%20print.pdf . [Google Scholar]
- 2.Blumenthal J. A., Sherwood A., Smith P. J., et al. Lifestyle modification for resistant hypertension: the TRIUMPH randomized clinical trial. American Heart Journal . 2015;170(5):986–994. doi: 10.1016/j.ahj.2015.08.006. e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National Heart, Lung and Blood Institute; National High Blood Pressure Education Program . 2004. https://www.nhlbi.nih.gov/files/docs/guidelines/jnc7full.pdf . [PubMed] [Google Scholar]
- 4. National Strategic Action Plan (NSAP) for Prevention & Control of Non-Communicable Diseases in Ethiopia; Federal Democratic Republic of Ethiopia Ministry of Health; 2014–2016 . https://www.iccp-portal.org/system/files/plans/ETH_B3_National%20Strategic%20Action%20Plan%20%28NSAP%29%20for%20Prevention%20and%20Control%20of%20Non-Communicable%20Diseases%20-%20Final.pdf . [Google Scholar]
- 5.Peberdy V. Hypertension: Putting the Pressure on the Silent Killer . 2016. https://www.ifpma.org/wp-content/uploads/2016/05/hyper-digital-v7-1.pdf . [Google Scholar]
- 6.Mirzaei M., Mirzaei M., Bagheri B., Dehghani A. Awareness, treatment, and control of hypertension and related factors in adult Iranian population. BMC Public Health . 2020;20(1):p. 667. doi: 10.1186/s12889-020-08831-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Acelajado M. C., Calhoun D. A. Resistant hypertension, secondary hypertension, and hypertensive crises: diagnostic evaluation and treatment. Cardiology Clinics . 2010;28(4):639–654. doi: 10.1016/j.ccl.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 8.Akinseye O. A., Leah I. A. Home blood pressure monitoring and hypertension control. Primary Health Care: Open Access . 2015;05(01):p. 182. doi: 10.4172/2167-1079.1000182. [DOI] [Google Scholar]
- 9.Bromfield S., Muntner P. High blood pressure: the leading global burden of disease risk factor and the need for worldwide prevention programs. Current Hypertension Reports . 2013;15(3):134–136. doi: 10.1007/s11906-013-0340-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3699411/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adeloye D., Basquill C. Estimating the prevalence and awareness rates of hypertension in africa: a systematic analysis. PLoS One . 2014;9(8) doi: 10.1371/journal.pone.0104300.e104300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kayima J., Wanyenze R. K., Katamba A., Leontsini E., Nuwaha F. Hypertension awareness, treatment and control in Africa: a systematic review. BMC Cardiovascular Disorders . 2013;13(1):p. 54. doi: 10.1186/1471-2261-13-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kearney P. M., Whelton M., Reynolds K., Muntner P., Whelton P. K., He J. Global burden of hypertension: analysis of worldwide data. The Lancet . 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 13.Mills K. T., Bundy J. D., Kelly T. N., et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation . 2016;134(6):441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ettehad D., Emdin C. A., Kiran A., et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. The Lancet . 2016;387(10022):957–967. doi: 10.1016/S0140-6736(15)01225-8. [DOI] [PubMed] [Google Scholar]
- 15.Macedo A. F., Morgado M., Castelo-Branco M., Rolo S., Pereira L. Predictors of uncontrolled hypertension and antihypertensive medication nonadherence. Journal of Cardiovascular Disease Research . 2010;1(4):196–202. doi: 10.4103/0975-3583.74263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamrahian S. M. Medication non-adherence: a major cause of resistant hypertension. Current Cardiology Reports . 2020;22(11):p. 133. doi: 10.1007/s11886-020-01400-3. [DOI] [PubMed] [Google Scholar]
- 17.Lee H. J., Jang S. I., Park E. C. Effect of adherence to antihypertensive medication on stroke incidence in patients with hypertension: a population-based retrospective cohort study. BMJ Open . 2017;7(6) doi: 10.1136/bmjopen-2016-014486.e014486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krousel-Wood M. A., Muntner P., Islam T., Morisky D. E., Webber L. S. Barriers to and determinants of medication adherence in hypertension management: perspective of the cohort study of medication adherence among older adults. Medical Clinics of North America . 2009;93(3):753–769. doi: 10.1016/j.mcna.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alhalaiqa F., Al-Nawafleh A., Batiha A. M., Masa’deh R., Abd Al-razek A. A descriptive study of adherence to lifestyle modification factors among hypertensive patients. Turkish Journal of Medical Sciences . 2017;47:273–281. doi: 10.3906/sag-1508-18. [DOI] [PubMed] [Google Scholar]
- 20.Bai G., Zhang J., Zhao C., Wang Y., Qi Y., Zhang B. Adherence to a healthy lifestyle and a DASH-style diet and risk of hypertension in Chinese individuals. Hypertension Research . 2017;40(2):196–202. doi: 10.1038/hr.2016.119. [DOI] [PubMed] [Google Scholar]
- 21.Fargally M., Elsadek A., Abdelhady A. S. Effect of lifestyle modification in hypertensive patients in greater cairo. The Egyptian Journal of Hospital Medicine . 2013;53:991–1006. doi: 10.12816/0001662. [DOI] [Google Scholar]
- 22.Flack J. M., Novikov S. V., Ferrario C. M. Benefits of adherence to anti-hypertensive drug therapy. European Heart Journal . 1996;17(suppl A):16–20. doi: 10.1093/eurheartj/17.suppl_A.16. [DOI] [PubMed] [Google Scholar]
- 23.Gupta M., Gupta D. D., Sood A. Impact of awareness about hypertension on compliance to antihypertensive medication. International Journal of Basic & Clinical Pharmacology . 2018;7(2):244–251. doi: 10.18203/2319-2003.ijbcp20180093. [DOI] [Google Scholar]
- 24.Gebrezgi M. T., Trepka M. J., Kidane E. A. Barriers to and facilitators of hypertension management in Asmara, Eritrea: patients’ perspectives. Journal of Health, Population and Nutrition . 2017;36(1):p. 11. doi: 10.1186/s41043-017-0090-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Menanga A., Edie S., Nkoke C., et al. Factors associated with blood pressure control amongst adults with hypertension in Yaounde, Cameroon: a cross-sectional study. Cardiovascular Diagnosis and Therapy . 2016;6:439–445. doi: 10.21037/cdt.2016.04.03. https://cdt.amegroups.com/article/view/10366 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wake A. D., Tuji T. S., Gonfa B. K., et al. Knowledge, attitude, practice and associated factors towards patient safety among nurses working at asella referral and teaching hospital, Ethiopia: a cross-sectional study. PLoS One . 2021;16(7) doi: 10.1371/journal.pone.0254122.e0254122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tibebu A., Bekele D. M., Negesa L. Adherence to recommended lifestyle modifications and factors associated for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa, Ethiopia. Patient Preference and Adherence . 2017;11:323–330. doi: 10.2147/PPA.S126382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Adidja N. M., Agbor V. N., Aminde J. A., Ngwasiri C. A., Ngu K. B., Aminde L. N. Non-adherence to antihypertensive pharmacotherapy in Buea, Cameroon: a cross-sectional community-based study. BMC Cardiovascular Disorders . 2018;18(1):p. 150. doi: 10.1186/s12872-018-0888-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Almeida A., de S., Bernardi C., Costa I. A. Factors determining non-adherence to hypertension treatment. Enfermería Global . 2016:p. 13. [Google Scholar]
- 30.Berisa H. D., Dedefo M. G. Non-adherence related factors to antihypertensive medications among hypertensive patients on follow up at nedjo general hospital in West Ethiopia. The Open Public Health Journal . 2018;11(1):62–71. doi: 10.2174/1874944501811010062. [DOI] [Google Scholar]
- 31.Boima V., Ademola A. D., Odusola A. O., et al. Factors associated with medication nonadherence among hypertensives in Ghana and Nigeria. International Journal of Hypertension . 2015;2015:8. doi: 10.1155/2015/205716.205716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cho S. J., Kim J. Factors associated with nonadherence to antihypertensive medication. Nursing & Health Sciences . 2014;16(4):461–467. doi: 10.1111/nhs.12145. [DOI] [PubMed] [Google Scholar]
- 33.Andualem A., Gelaye H., Damtie Y. Adherence to lifestyle modifications and associated factors among adult hypertensive patients attending chronic follow-up units of dessie referral hospital, North East Ethiopia. Integrated Blood Pressure Control . 2020;13:145–156. doi: 10.2147/IBPC.S275575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nadewu A. N., Geda B. Adherence to healthy lifestyle among hypertensive patients in Harar region, Eastern Ethiopia. Primary Health Care Open Access . 2018;08(04) doi: 10.4172/2167-1079.1000308. [DOI] [Google Scholar]
- 35.Lulebo A. M., Mutombo P. B., Mapatano M. A., et al. Predictors of non-adherence to antihypertensive medication in Kinshasa, Democratic Republic of Congo: a cross-sectional study. BMC Research Notes . 2015;8(1):p. 526. doi: 10.1186/s13104-015-1519-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kabir M., Iliyasu Z., Abubakar L., Jibril M. Compliance to medication among hypertensive patients in murtala mohammed specialist hospital, Kano, Nigeria. Journal of Community Medicine and Primary Health Care . 2004;16(1):16–20. doi: 10.4314/jcmphc.v16i1.32401. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available upon request from the corresponding author.


