Abstract
Potentially inappropriate medication (PIM) is a primary health concern affecting the quality of life of patients over 65. PIM is associated with adverse drug reactions including falls, increased healthcare costs, health services utilization and hospital admissions. Various strategies, clinical guidelines and tools (explicit and implicit) have been developed to tackle this health concern. Despite these efforts, evidence still indicates a high prevalence of PIM in the older adult population. This systematic review explored the practice of using explicit tools to review PIM in hospitalized patients and examined the outcomes of PIM reduction. A literature search was conducted in several databases from their inception to 2019. Original studies that had an interventional element using explicit criteria detecting PIM in hospitalized patients over 65 were included. Descriptive narrative synthesis was used to analyze the included studies. The literature search yielded 6116 articles; 25 quantitative studies were included in this systematic literature review. Twenty were prospective studies and five were retrospective. Approximately, 15,500 patients were included in the review. Various healthcare professionals were involved in reviewing PIM including physicians and hospital pharmacists. Several tools were used to review PIM for hospitalized patients over 65, most frequently Beer’s criteria and the STOPP/START tool. The reduction of PIM ranged from 3.5% up to 87%. The most common PIM were benzodiazepines and antipsychotics. This systematic review showed promising outcomes in terms of improving patient outcomes. However, the reduction of PIM varied in the studies, raising the question of the variance between hospitals in the explicit tools used for review. Additional studies need to be conducted to further investigate the outcomes of reviewing PIM at different levels, as well as assessing the cost-effectiveness of using explicit tools in reducing PIM.
Keywords: older population, adverse drug effects, drug review tools, PIM
Introduction
Potentially inappropriate medication (PIM) is a health concern that highly affects the quality of life for patients 65 years and over. Older patients who were prescribed such medication have experienced an increase in falls, adverse drug reactions,1,2 healthcare costs, health services utilization and hospital admissions.3,4 PIM are defined as medications for which the risk outweighs the potential benefits.5
Many interventions have been developed to tackle PIM. As part of the daily routine in hospitals, physicians, pharmacists, and other healthcare professionals (HCP) have assumed the responsibility to reduce PIM in patients over 65. An observational study was conducted in France for 6 months to evaluate the routine care provided in a geriatric unit.6 The study confirmed that the usual care included medication reviews done by geriatricians. This resulted in 275 medication changes, with 158 medications stopped, 53 medications replaced, and 64 new medications initiated. Notably, 132 (61.11% (95% CI = [54.61–67.61]) patients over 65 had at least one medication discontinued during their hospital stay. This study reflected the practice of optimizing older patients’ medication as part of routine care; however, the Hawthorne effect might have influenced the physician–patient communication.7 The changes in PIM prevalence during the hospital stay may indicate that HCP interventions contributed to PIM reduction. This was concluded by Laroche et al in a prospective study after the HCPs reduced PIMs by 22.4% during the older patients’ hospital stay.8 To further support that, a UK-based retrospective study was conducted in an acute hospital in England examining 195 patients over 65,9 which revealed that the prevalence of PIM on admission was 26.7% with 74 PIMs detected in 52 patients; at discharge, the prevalence of PIM was 22.6% with 51 PIMs detected in 44 patients. A statistically significant change in PIM prevalence was found between PIM on admission and discharge. Additionally, the study disclosed that a small number of patients received a follow-up letter when prescribed a PIM. Similar findings were observed by Komagamine in his retrospective study, based on a hospital database in Japan, which concluded that the number of PIM upon discharge was fewer than the number of PIM on admission, indicating a significant reduction rate (0.48 on admission vs 0.53 at discharge).10
An overview of systematic reviews that investigated interventions aimed at PIM reduction found that several interventions were employed to reduce PIM. These included medication review services, pharmaceutical intervention, computerized systems and educational interventions.11 The studies included in the overview were conducted in various health care settings such as hospitals, primary care clinics, nursing homes and long-term care facilities.
The tools to detect PIM can be categorized as implicit (judgment based), explicit (criteria based) or combined (both judgment and criteria based). Implicit tools contain questions that are designed to examine the effectiveness and safety of each medication such as the Medication Appropriateness Index (MAI). Explicit tools comprise a list of medications that are known, based on evidence, to be inappropriately prescribed to older patients. Examples of explicit tools are the Beers Criteria and the STOPP/START tool (Screening Tool of Older Persons’ Prescriptions/Screening Tool to Alert to Right Treatment). Clinical expertise is needed to apply the tools with recommendations tailored to each patient.12
The Beers Criteria was produced in 1991 through a Delphi technique of 13 experts.13 The Beers criteria was recently update in 2019 through the Delphi method of 13 experts (physicians, pharmacist, and nurses) who have already contributed to Beers criteria 2015 update. A literature search in both PubMed and Cochrane Library was conducted to identify relevant literature. The literature search yielded 67 systematic reviews and/or meta-analyses, 29 controlled clinical trials and 281 observational studies. This evidence went under review in a cycle of evaluation by the expert panel. Evidence evaluation was done through two approaches: the American College of Physicians (ACP) and the Grading of Recommendations Assessment, Development and Evaluation guidelines for clinical practice guideline development (GRADE). There were two criteria to assess the evidence which are quality of evidence (high–moderate–low) and strength of recommendation (strong or weak).
The STOPP/START tool was developed in 2008 and produced an update in 2015.14 The recent update was based on a literature search in three databases (PubMed, Embase and Cochrane Library) to find systematic reviews, randomised controlled trials and reviews. In addition to the literature search, British National Formulary (BNF) the National Institute for Health and Care Excellence (NICE) and the Scottish Intercollegiate Guidelines Network (SIGN) to search references of guidelines as well as recent published textbooks. The selected articles were categorized into the physiological systems after being assessed by the three members of the research team for their suitability as an evidence to be presented to the expert panel of 19 experts from 13 European countries. The expert panel was not asked to read the full articles nor assess the evidence through standardised rating; however, abstracts of the evidence was presented, and reference bank was supplied to access full articles if needed. To enable online Delphi panel, SurveyMonkey® was utilized to achieved consensus through 5-point Likert scale (0 = do not know; 1 = strongly agree; 2 = agree; 3 = neutral; 4 = disagree; 5 = strongly disagree). It is worth to note that the expert panel were initially asked to comment on the 2008 version of STOPP/START and to reflect on its validity and relevance.
Although the literature suggests that PIM are identified through explicit tools during a patient’s hospital stay, there is a paucity of data as to when these explicit tools are used within a hospital setting. This systematic review aimed to explore the practice of reviewing PIM in hospitalized patients over 65, using explicit tools. The objectives were:
To explore the PIM review process in terms of the explicit tools used, HCP involved, stage of hospitalization and resources utilized.
To identify the common PIM and their clinical relevance in hospitals.
To investigate the clinical and non-clinical outcomes of the PIM review.
Method
A systematic literature search was carried out from February 9 to February 13, 2019, using predefined search terms. The literature search was updated on 20th of April 2021. This review was registered in PROSPERO under the registration number CRD42019131104.
Based on the research question “how do healthcare professionals review PIM in hospitalized 65 years and over patients using explicit tools and what are the outcomes of the review process?”, the PIO format is shown in Table 1.
Table 1.
Population, Intervention, Outcome
| Population | Hospitalized 65 Years and Over Patients |
|---|---|
| Intervention | Explicit tool application |
| Outcome | PIM reduction (primary outcome) and clinical and non-clinical outcomes (secondary outcomes) |
The search terms were obtained from concepts of the research question, keywords of relevant articles and the search strategy of systematic reviews.15 The search terms were validated by the research team and an information manager. The search terms were piloted in PubMed and relevant data were found.16 The search term combination is detailed in Table 2. The search was restricted to English articles only; no filter was used to limit the studies in the selected period. The following databases were searched: PubMed, Scopus, PsycINFO, CINHAL plus, Web of Science, all Ovid journals and OpenGrey. All the results were exported to EndNote 9 as a reference manager and to eliminate duplication.
Table 2.
The Keywords Combination Used in Each Database for the Systematic Literature Review
| Database | Search Term |
|---|---|
| PubMed | (((((((“Inappropriate polypharmacy“[Title/Abstract] OR polypharmacy[Title/Abstract])) OR potentially inappropriate medication list[MeSH Terms])) OR ((((“inappropriate medic*“[Title/Abstract] OR “inappropriate drug?“[Title/Abstract] OR PIM[Title/Abstract])) OR (“pharmacological inappropriateness“[Title/Abstract] OR “Potentially harmful medic*“[Title/Abstract] OR “Potentially harmful drug?“[Title/Abstract])) OR (“inappropriate prescribing”[Title/Abstract] OR PIM[Title/Abstract] OR ”inappropriate prescribing”[Title/Abstract])))) AND (((((Elderly[Title/Abstract] OR ”older people”[Title/Abstract] OR ”older patient?”[Title/Abstract] OR ”older adult?”[Title/Abstract])) OR (seniors[Title/Abstract] OR ”65 years”[Title/Abstract] OR aging[Title/Abstract]))) OR ((aged[MeSH Terms]) OR (65 years and over[MeSH Terms])))) AND (((hospital*[Title/Abstract] OR discharge[Title/Abstract])) OR (admitted[Title/Abstract] OR admission?[Title/Abstract] OR ”secondary care”[Title/Abstract])) Sorted by: best match |
| Scopus | (TITLE-ABS-KEY (“pharmacological inappropriateness“ OR “harmful medication“ OR “inappropriate prescribing“ OR PIM “inappropriate medication“ OR “inappropriate medicine“ OR “ inappropriate drug“) OR TITLE-ABS-KEY (pim OR PIM OR “Inappropriate polypharmacy” OR polypharmacy) AND TITLE-ABS-KEY (elderly OR ”older people” OR ”older patient” OR ”older adults” OR seniors OR ”65 years” OR aged) AND TITLE-ABS KEY (hospital OR hospitalized OR admitted OR admissions OR ”secondary care” OR hospitalization)) AND (LIMIT-TO (LANGUAGE, ”English”)) |
| CINHAL PLUS | AB (“pharmacological inappropriateness“ OR “Potentially harmful medication“ OR ”inappropriate prescribing” OR PIM ‘inappropriate medication’ OR ‘inappropriate medicine’ OR ‘inappropriate drug’ OR PIM OR ‘Inappropriate polypharmacy’ OR Polypharmacy) AND AB (Elderly OR older people OR older adults OR seniors, 65 years and over OR aged) AND AB (Hospital OR hospitalized OR admitted OR admissions OR ”secondary care” OR hospitalization OR hospitalisation OR hospitalised) |
| All OVID journals, PsycINFO and Web of Science | ((“Inappropriate medic*“ or “inappropriate drug“ or “pharmacological inappropriateness“ or “inappropriate prescribing“ or “inappropriate polypharmacy” or polypharmacy or PIM or PIM) and (elderly or 65 years or age* or ”older people” or ”older adults” or ”older patient” or seniors) and (hospital* or admission or admitted or discharge or ”secondary care”)).ab. |
| OpenGrey | “Inappropriate polypharmacy“ OR polypharmacy OR “inappropriate medic*“ OR “inappropriate drug*“ OR PIM OR “pharmacological inappropriateness“ OR “Potentially harmful medic*“ OR “Potentially harmful drug*“ OR PIM OR ”inappropriate prescrib* AND elderly OR ”older people” OR ”older adult*” OR ”older patient*” OR senior* OR ”65 years” OR aged AND admissions OR ”secondary care” OR Hospital* OR hospitali* OR admitted lang:”en |
Selection
A set of predefined inclusion and exclusion criteria were constructed to answer the aim and objectives of this review (refer to Table 3). Two reviewers completed the title and abstract screening. Any disagreement was resolved by a discussion, then an agreed decision to include or exclude was reached.
Table 3.
List of Inclusion and Exclusion Criteria Applied to the Resulting Articles
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| ● The included study can be either a qualitative or quantitative original study ● Studies included should be focused on patients 65 years and over ● The study should use an explicit tool to review potentially inappropriate medications ● The included studies should be conducted in a hospital setting |
● Studies conducted in nursing homes, emergency department and primary care were excluded. ● Studies focused on terminal illness or end of life patients were excluded. ● Non- English studies were excluded. |
Data Extraction
The data extraction form was developed (Appendix 1) and Microsoft Excel was used to extract and tabulate the data of the included studies. Two reviewers conducted the data extraction and extracted the following information:
Author and year of publication
Country and setting of the study
Study design
Number and characteristics of participant
Explicit tool used and applied by whom
Sources of data used to assist the decision
Primary and secondary outcomes (clinical and non-clinical outcomes)
Analysis
The review included all relevant data without limitations to specific study design, thereby including various types of quantitative studies.
The included articles were narratively synthesized. Narrative synthesis answers research questions that are about the effect intervention and the implementation of the intervention. A description of the included studies contained country, sample, tool used, number of PIM before and after tool application, and additional relevant results.
In this study, the latest version of the Mixed Method Appraisal Tool (MMAT)17 was used to evaluate the quality of the included studies. The first version of the MMAT in 2006 was piloted and went through interrater reliability testing.18 It was revised in 2011 after being piloted in workshops, which led to the addition of new criteria to assess nonrandomised studies. Version 2018 of the MMAT was subject to content validity and usefulness. In the recent update, usefulness testing through interviews with 20 previous users was conducted to further improve the appraisal tool. In addition, a modified e-Delphi was conducted with 73 experts in the fields different research methods as well as literature reviewer on critical appraisal tool.
An adjacent score was presented in this study to reflect the quality of the study. Two reviewers from the research team conducted the quality assessment. Any disagreement was discussed and the final decision was reported.
Results
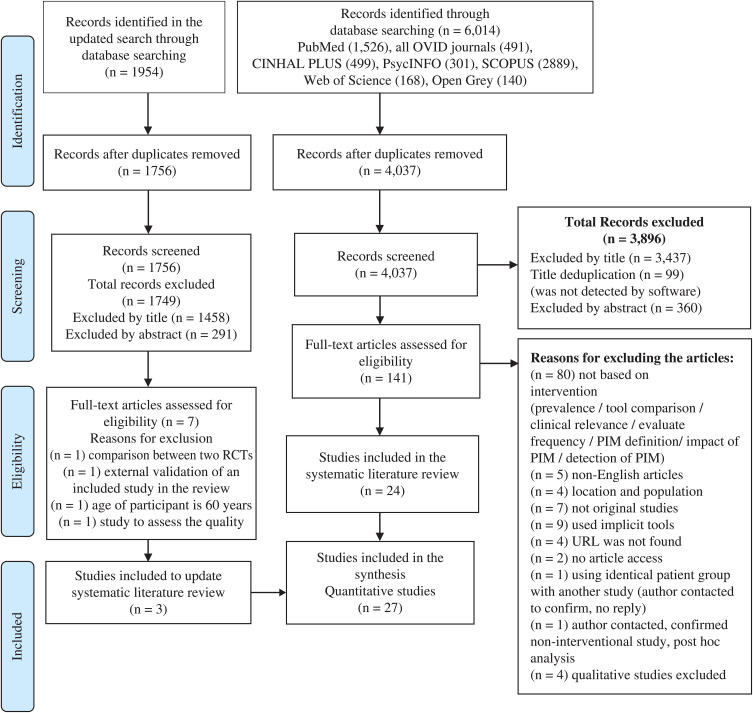
The original literature search yielded 6116 articles and the updated literature yielded 1954 articles. The PRISMA flow diagram below describes the screening process used as shown in Figure 1. The included articles are summarised in Table 4.
Figure 1.
Results and screening process according to PRISMA guidelines.
Note: Adapted from Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372:n71.19
Table 4.
Total of 25 Articles Included in the Synthesis in This Systematic Literature Review
| Author, Year | Country | Study Design | Participants | Explicit tool Utilised | Applied by | Explicit Tool Applied in | Source of Data | Primary Outcome | Overall Quality Rating |
|---|---|---|---|---|---|---|---|---|---|
| Cossette, 201720 | Canada | Pragmatic randomised controlled trial | 254 Elderly patients divided into 128 elderly patient in the control group and 126 elderly patient in the intervention group. | Exert panel selection from STOPP and Beers criteria in CAS alert system (geriatrician, internist, pharmacist). | Pharmacist checked the relevance of the CAS alert, then created a pharmacotherapeutic plan and discussed it with the treating physician to reduce PIM; blinding the pharmacist and the physician was not feasible (distribution of education material to all physicians, medical residents, and pharmacists). | During hospital stay | Electronic medical records which included clinical information and medications. | Medication change at 48 hours in the intervention group was 45.8% for drug cessation or dose reduction; 52 interventions were made. In the control group, 15.9% was associated with dose reduction or discontinue; 99 interventions were made. The mean time to analyse the patient file was 41 ± 16 minutes. |
4 |
| Dalleur, 201421 | Belgium | Randomised control study | 146 Patients divided into 74 in intervention group and 72 in control group. | STOPP/START tool | Inpatient geriatric consultant team (IGCT) consisting of nurses, geriatricians, dietitian, OT, PT, speech therapist and a psychologist. | On admission screening and recommendation for PIM to be discontinued during the hospital stay. | The nurse did the initial evaluation, then the patient was referred to the team and screened for geriatric syndrome, polypharmacy and MMSE, cognitive disorders, malnutrition, and functional dependency. Recommendations were communicated orally and available on the electronic medical record. | 125 PIMs were detected 68 of them found in the intervention group. Regarding stopping PIM, it was shown that the discontinuation of PIM was two times higher in the intervention group (93.7%) compared to the control group (19.3%). After 1 year follow up, the GP did not reinitiate PIM prescription in both the intervention and the control group. PIM discontinue rate of benzodiazepines in the intervention group was higher than the control group (23.1% vs 16.1%). Improvement in the drug therapy with at least one improvement was higher for the intervention group (25.7 vs 13.9%). |
5 |
| Gallagher, 201122 | Ireland | Randomised controlled trial | 400 patients: 18 died before intervention. Total of 382 patients were in the study. | STOPP/START tool | Primary research physician | Within 24 hrs of hospitalisation | The information was obtained from patient or the caregiver interview and chart review. The community pharmacy is contacted if needed. |
The primary research physician recommended 183 changes to 111 patients in the intervention group. 91% of the STOPP recommendation was accepted by the attending physician. 97% of the START recommendation were accepted by the attending physician. |
5 |
| Michalek, 201423 | Germany | Prospective randomised controlled trial | 114 Elderly patients. 58 patients were in intervention group, and 56 patients were in control group. | FORTA list | 2 physicians familiar with the FORTA list. | During hospital stay | Data collected on admission (patient and medication history, falls in the last 3 years, and Charlson index was utilized to describe the comorbidities burdens; geriatric assessment on admission, grip strength and nutritional status. | The number of medications was high in both groups; FORTA class A drugs were higher in the intervention group. It was observed that the application of FORTA had a positive impact on BI, which was pronounced in the intervention group compared to the control group. Only one patient in the intervention had a decline in BI, while 5 patients in the control group showed a decline in BI. Regarding falls during hospital stay, 2 patients in the intervention group experienced falls, and 12 patients experienced falls in control group. |
4 |
| Spinewine, 200724 | Belgium | Prospective randomised design | 203 Elderly patients. 103 of the elderly patients were allocated in the intervention group, while 100 of them were in the control group. | Beers and ACOVE | Pharmaceutical care was provided from admission to discharge by a clinical pharmacist. | During hospital stay | On admission the clinical pharmacist carried out medication history and medication reviews and conducted an interview with the patient or caregiver to obtain several information related to the clinical status of the patients. The pharmacist provided both oral and written information regarding the changes medication and a copy was also written to the GP. |
In the control group, less than half of the patients (34.4%) had at least one PIM on admission. In the intervention group, the prevalence of having at least one PIM on admission was 25%. Long-acting benzodiazepines were 65.1% prescribed for elderly patients on admission in the control. It was reduced at discharge to 60.3%. Long-acting benzodiazepines were prescribed to 58.6% of the patients on admission in the intervention group, and it dropped to 44.8% on discharge. After the application of Beers criteria 94% improvement in PIM prescribing in patients included in the intervention group, while only 86% improvement in PIM prescribing was noted in the patient in the control group. |
4 |
| Wehling, 201625 | Germany | Randomised controlled trial | 409 Patients were randomised, 202 patients were allocated in intervention group, while 207 were in the control group. | FORTA list | Trained physician | Not stated | At baseline: patient history and detailed history of medications, physical examination, leading diagnoses, electrocardiogram, chest X-ray, supine and standing blood pressure, smoking status, pain scale from 0 to 10, basic laboratory findings. The following geriatric assessments and other tests were performed: the Barthel Index (BI) for activities of daily living (ADL), and the instrumental activities of daily life (IADL), handgrip strength, mobility tests (Timed “Up and Go”, Tinetti), cognitive tests (Mini-Mental Status according to Folstein), Morisky Score and pain scale. ADL and pain scale were repeated upon discharge, as well as blood pressure and pulse rate. | The application of FORTA tool resulted in a large difference between the intervention group and the control group on admission and on discharge. In the control the difference between PIM on admission 3.4 ± 2.3 (Median 3) to 2.4 ± 2.2 on discharge (Median 2, P < 0.0001). In the intervention group the PIM reduced from 3.5 ± 2.7 (Median 3) to 0.8 ± 1.4 (Median 0, P < 0.0001). The application of FORTA in the intervention group showed a higher reduction in both over- and undertreatment compared to the control group. The clinical impact of PIM reduction was observed in the changes in blood pressure in the hospitalized elderly patients in both the control and intervention groups. The changes in blood pressure reading were significantly different between intervention and control group at discharge groups (P < 0.05). |
4 |
| Linden, 201726 | Belgium | Monocentric prospective controlled trial | 214 Elderly patients in which 97 of them in the control group and 117 in the intervention group. | RASP list | Trained clinical pharmacists (5 pharmacists) | On admission, part of medication reconciliation service and medication review during the hospital stay. The pharmacist also checked the prescription at discharge. recommendations were actively communicated to the attending physician. |
On admission, reconciliation phase. | 18% PIMs were stopped in the intervention group. More drugs were discontinued during hospital stay. On discharge, the number of drug discontinue in control average of 3 medications, while average of 5 medications in the intervention group. The changes in PIM were not statistically significant. |
4 |
| Lozano-Montoya, 201527 | Spain | Ambispective non-randomised study | 388 Patients 42 of them died in hospital. | STOPP/START | Clinical pharmacist expert in STOPP/START; detection of PIM on admission, then the clinical pharmacist sent recommendation to the multidisciplinary team to reach a decision. The team consisted of 3 geriatricians and 2 clinical pharmacists. | On admission | Medical records in hospital and primary clinic and comprehensive medication history from patients’ caregivers. | After the application of STOPP tool, 49.1% (170 of 346) of the elderly patients had at least 1 PIM. While the STOPP criteria identified that 61.3% (212 out of 346) of the patients had at least one PPO. The total number of identified PIMs were 284 (0.8 per elderly patient). Majority of PIM were stopped (247, 87.0%), while 37 (13%) of the cases in which the PIM was not stopped. On the other hand, 33.5% of the PPO recommended by the clinical pharmacist were accepted. |
4 |
| Mattison, 201028 | USA, Boston | Prospective before and after study | All patients in the period of pre-intervention and post-intervention. | Warning system (CPOE) using specific Beer’s criteria medications; the list was generated by a geriatrician and a pharmacist, supported their choices by the literature with the final list approved by the pharmacy and therapeutic committee from Beer’s criteria. | System flagged up the PIM to the HCP who ordered it. | On admission and throughout the hospital stay. | The hospital did not support electronic medication administration records; any physician order will flag up the PIM. | Improvement in prescribing medications that were not recommended per day reduced from 11.56 (0.36) to 9.94 (0.12). Reduction in prescribing unflagged medication, however, it was not statistically significant change. Limited reduction in mediations in which the recommendation was dose reduction. |
3 |
| Urfe, 201629 | Switzerland | Before and after trial, interventional study quasi-experimental | 900 Patients | STOPP/START | Not specified | On admission and checked on discharge. | Electronic medical records. | 266 (31%) of the 852 elderly patients that were included in the trial had more than 1 PIM prescribed at discharge. 160 (19%) had more than 1 PPO. A 22% reduction was observed in the patients prescribed more than 1 PIM in the intervention group. |
4 |
| Vu, 201930 | Vietnam | Before and after trial | 211 Medical records before intervention (4 months, 208 medical records after intervention (4 months). | Beers 2015 | Pharmacist (trained on Beer’s criteria) | During hospital stay | Medical records, notebook on Beers 2015 was provided to MD for reference. | Prevalence of PIMs in patients before and after intervention were 34.1% and 23.1%, respectively. No statistical difference was noted. | 4 |
| Abbasinazari, 202031 | Iran | Prospective interventional study | 240 Patients | Beer’s criteria | Clinical pharmacist | On admission (Day 1: medical history and medication reconciliation, Day 2: screening for PIM, Day 3: outcome of the recommendation checked). | Medical history and medication reconciliation. | Total of 95 PIMs were identified. 80 (33.3%) out of 240 participants had at least one PIM. The most common PIM identified were opioid and benzodiazepines. The clinical pharmacist recommendations were communicated verbally and written. There were 95 recommendations, 87 (91.5%) of which were accepted by the physician. |
4 |
| Darmawan, 202032 | Indonesia | Prospective interventional study | 123 Patients | STOPP/START tool and Beer’s criteria | Hospital pharmacist | On admission | Medical record and interviews with patients or family. | According to STOPP/START tool and Beer’s criteria 54 PIMs were found in 48 patients. The recommendations were communicated verbally and written to the physician. The physician accepted 17 (31%) of the hospital pharmacist recommendations. According to STOPP tool, NSAID was the most common PIM identified. While the most common PIM identified by Beer’s criteria was benzodiazepines. |
3 |
| Hannou, 201733 | Switzerland | Prospective interventional study | 102 Patients | STOPP/START | Clinical pharmacist | On admission and throughout the hospital stay. | Medication history and medication reconciliation. | The total number of the pharmacist recommendation was 697 in which 454 of them were based on routine pharmacist review. While the remaining 243 were based on STOPP/START tool. 68% global acceptance rate (78% of recommendations were accepted from the pharmacist routine review and 47% were accepted from STOPP tool 58% START tool. |
4 |
| Lang, 201234 | Switzerland | Prospective interventional study | 150 Patients | French adaptation of STOPP/START tool. | A geriatrician and psychiatric provided care for elderly patient from admission to discharge. A number of HCP were also included in the team such as geriatric nurse, physical therapist, psychologist, and therapeutic recreation specialist, but not a pharmacist. | During hospital stay | A senior resident performed complete medication history, medication and patient history, lab values and renal glomerular filtration rate recorded by the attending physician. Patient functional abilities were assessed by Katz daily living scale, Charlson cumulative comorbidity index form. For dementia patients, the clinical dementia rating scale was used |
The reduction of PIM decreased from 77.3% to 18.6%. The reduction of PPO was reduced from 47% to 11.2%. No change in the pharmacotherapy was done to 23 (35.1%) of elderly patients. 24 (17.9%) patients had a higher number of medications, which were mainly vitamin B6 and B12. |
4 |
| O’Sullivan, 201435 | Ireland | Prospective interventional study | 361 Patients | STOPP/TART, Beers and PRISCUS. | Hospital pharmacist | 48 hours of admission | Medication charts and notes of medical and nursing staff. Medication history was obtained from the patient’s caregiver and biochemical data. In order to fully reconcile elderly patient medication, either the community pharmacy or the GP were contacted. A follow up by the pharmacist was done at the 7th – 10th day of hospital stay or at patient discharge. |
Total number of PIMs that were identified after using STOPP was 449. These were found in 232 (64.2%) patients. The research pharmacist recommended 1000 interventions in 296 patients, which is equal to two intervention per patients. Total of 67 patients had more than 1 PIM and total of 577 (57.7%) recommended interventions were related to medication appropriateness issues. 548 (54.8%) recommendations were accepted by the physician. |
4 |
| Alosaimy, 201936 | USA | Prospective single centre pilot study | 43 Elderly patients | STOPP/START tool Beer’s criteria | Pharmacy team: six members of pharmacotherapy specialists in geriatric medication therapy management. | During hospital stay | Patient or family interview to create medication history and medication list. | 52% of the elderly patients included in the study had at least one PIM. A statistical significance change in PIM number was associated with pharmacist intervention. PIMs on admission (0.84 ± 1.12) before pharmacist intervention and were (0.56 ± 0.91)after pharmacist intervention. The percentage of acceptance of the pharmacist recommendation was 36%. |
4 |
| Chandrasekhar, 201837 | India | Prospective observational study | 210 Patients | STOPP/START tool | Not specified | During hospital stay | Case files, medication chart, interviews with patients’ caregivers collected in predesigned collection book. Lab values, vital parameters, prescription, and medical diagnosis; a form for data collection was created by the researcher. | The prevalence of PIM in the 1st phase was 43.5%, 40.2% in the 3rd phase. The PPO identified using START was 52.8% in the 1st phase and 53.9% in the 3rd phase. No statistical difference noted after the intervention in PIM or PPO. |
3 |
| Chu, 201438 | Taiwan | Prospective study | Number of elderly patients not stated. | Beers 2012 CPOE | There were two interventions: one with the decision support system and the other by the clinical pharmacist using Beer’s criteria. | Not specified | Not specified | Reduction of 6.42% by the CPEO and 5.47% by the clinical pharmacist. 71.4% of the recommendations generated by the CPEO were accepted and 92.5% of the pharmacist recommendation were accepted. |
2 |
| Kadri, 201739 | France | Prospective study | 81 Patients | STOPP/START | Pharmacist assessed the prescription and the PIM were documented to the physician in the patient records. After discharge both the geriatrician and the pharmacist investigated the cases in which STOPP/START recommendations were not approved. | Not stated | Patient pre-admission medication history. | 224 PIM were identified using STOPP, 168 (75%) were supported by the geriatrician; among 56 cases of not following the recommendation, 50 cases (90%) were justified among the PIM identified by STOPP; 94 medications identified by the physician but not STOPP supplementary medications 90. The geriatrician followed PPO identified by START 56 (62%), of which, 34 cases were not followed, 27 cases were justified; the geriatric identified medication that should be started and not in START tool. |
3 |
| Kimura, 201940 | Japan | Prospective observational study | 230 Patients (201 patients were from the cardiovascular surgical department and 29 were from cardiovascular internal medicine department). | STOPP tool and STOPP-J | Clinical pharmacists that were trained to detect and correct PIM. | On admission | Medical history, medication reconciliation and laboratory findings. | After the clinical pharmacist review, 122 of the patients (53%) were prescribed at least one PIM according to STOPP-J, while 75 PIMs were detected through STOPP tool in 33% of the patients. Total of 232 PIMs were identified through STOPP-J and 133 were identified through STOPP tool. 69 PIMs were found in both criteria. STOPP-J identified statically significant (P < 0.001) more PIMs than STOPP tool. The clinical pharmacist obtained patient approval before recommending changes or discontinue to the physician. Total number of recommendations of PIMs detected by STOPP-J were 116 out of 232, 61 PIMs (26%) were recommended to be changed and 50 PIMs (22%) were recommended to be discontinued. 82% of the clinical pharmacist recommendations by STOPP-J were accepted. Total number of recommendations of PIMs detected by STOPP tool were 155 out of 133, 61 PIMs (46%) were recommended to be changes, while 54 (41%) were recommended to be discontinued. 89% of the clinical pharmacist recommendation by STOPP tool were accepted. |
4 |
| Kympers, 201941 | Belgium | Prospective observational single-centre study | 60 Patients | GheOP3s tool | Pharmacist and communicated to the geriatrician. | Not stated | Medical records and some information were obtained from the geriatrician including age, gender living status. | The number of the total number of the prescribed medication was 610. Approximately every elderly patient had 10 medications. When the GheOP3S tool was applied to the medication, 250 medications were identified as a PIM in 57 (95%) elderly patients. Only 52% of the recommendation were fully accepted by the geriatrician. While 27% of the recommendation were partially accepted and 18% of the recommendation were not accepted by the geriatrician and the reason was “insufficient reason to stop”. |
4 |
| Pandraud-Riguet, 201742 | France | Prospective observational study | 1327 Patients | PIM list adopted from Beers, Laroche, and PRISCUS (Delphi panel) | Pharmacist (was trained to detect PIM) screened the prescription for PIM and sent them to the attending physician. | Not stated | Prescriptions | 1036 PIMs were detected (743 PIMs and 320 PIA); of the 1327 participants, 607 had at least 1 PIM (46%), 345 had 1 PIM (26%), 140 had 2 (11%), 74 had 3 (6%) and 48 (4%) had 4 or more. After an assessment by clinical pharmacist, 78% of the PIM maintained by physician. Total of 121 medications were subjected to changes either in discontinuation, or dose reduction or switched to safer alternative. 90 PIM assessments were unknown; decrease in PIM number from 11% to 22% before assessment; the mean number of PIM was 1.8, after assessment, the mean number was 1.6 |
4 |
| Brown, 200443 | USA | Retrospective case series design | 99 Patients | Beers 2003 | Pharmacist team | Not specified | Patients’ charts and computer database. | PIM was 10.1% on admission and reduced to 2.02% (statistically significant reduction of PIM). Patients were prescribed an average of 6.69 and 7.15 medications on admission and upon discharge, respectively. This resulted in a mean increase of 0.465 medications. |
5 |
| Cossette, 201644 | Canada | Segmented regression analysis of an interrupted time series | 8622 Patients discharged from hospital in period of 2013–2014. | Intervention based on educational presentations and the PIM list adopted from Beers 2012; changes were implemented after a multidisciplinary team expert panel sent to the pharmacy department, which approved the list, then it was emailed to all physician–pharmacist medical residents. | Pharmacist review CAS alert system: evaluated their clinical relevance, developed a plan, and discussed it with the attending physician. | Not specified | CAS system embedded in medical records. | At least 1 PIM was prescribed in 19.8% elderly patients. It was observed that patients aged 75 to 84 had a higher rate being prescribed a PIM (24.0%) compared to those who are older that the age of 84 (14.4%). After reviewing elderly patient medication, a 2.55% reduction was observed in PIM. This was followed by 0.11% of PIM prescribing monthly after the intervention period. A 3.5% decrease in PIM prescribing was observed after implementing the intervention and 0.11% increase of PIM prescribing month after intervention period. |
4 |
| Ghibelli, 201345 | Italy | Two-phase retrospective studies | The observation phase included 74 elderly patients and was conducted from April to May 2012. The intervention phase included 60 elderly patients and was conducted from June to July 2012. |
Beers 2002 in the InterCheck system. | Computerised system presenting alerts. | Not specified | Not specified | In the observation phase 39.1% of the elderly patients had at least one PIM on admission. While 37.8% of the elderly patients had at least one PIM on discharge. In the intervention phase 41.7% had at least one PIM on admission. While it was reduced to 11.6% upon discharge. This was statistically significant reduction of PIM number (p=0.001). |
4 |
| Kersten, 201546 | Norway | Retrospective study | 250 Patients | NORGEP | In the geriatric ward, the pharmacist used to review the medications of approximately 70% of the admissions. Any medication related concerns were sent to the attending physician for evaluation. The routine clinical assessment used to be done by the nurses within 72 hours of admission. |
During hospital stay | Several resources were used to obtain the medical history including the patient medical records, as well as the GP referral letter. | The mean number of medication on admission is 7.8, while the mean number of medication at discharge was 7.9. Despite the similar mean number of medications on admission and discharge, some changes were done to the medication regimens during the hospital stay. There were 133 medication removed and 102 dose reductions. Diuretics were the most common medication removed, or dose reduced or replaced. The PIM reduction during hospital stay in the geriatric ward was not statistically significant. In the geriatric ward 30% of new PIMs that were introduced included cardiovascular medications including prescribing ACE inhibitor and potassium/ potassium-sparing diuretics. However, none of the elderly patients that were prescribed these combination had hyperkalaemia. In conclusion, changes to the prescribed medication happened more often in the geriatric ward compare to other medical wards in the hospital. In addition, newly prescribed PIM was less found in geriatric ward compared to other medical wards. |
5 |
| Sennesael, 201747 | Belgium | Retrospective study in a geriatric unit consists of 4 part-time series in 1 month | 120 Patients | STOPP/START tool | Clinical pharmacist. | During hospital stay | Discharge letter was used to gather the demographics, clinical and pharmaceutical information. | The prevalence of having at least one PIM on admission was 65%. The total number of PIMs that were identified on admission using the STOPP tool were 101 PIMs. These were identified in 67 elderly patients. A number of PM 49% was discontinued in 33 out of 67 patients during the hospital stay. The prevalence of PIM was reduced at discharge to 46%. After applying logistic regression to the 4th phase, a statistically significant reduction was noted. After the application of START section, 86 PPO (51%) were identified in 61 patients. This was reduced to 39% at discharges (24/61). |
4 |
Notes: Key characteristics are shown in the table in addition to the quality assessment that was done using MMAT tool 2018. The MMAT tool has five questions. 1 means only one question answered yes. 2 means two out of five questions answered yes. 3 means three out of five questions answered yes. 4 means four questions answered yes. 5 means all questions answered yes.
Abbreviations: PIM, potentially inappropriate medication; PPO, potential prescribing omission; CPOE, computerised physician order entry; CAS, computerised alert system; GP, general practitioner; ADL, activities of daily living; NORGEP, Norwegian General Practice; FORTA, Fit fOR The Aged; RASP, rationalisation of home medication by an adjusted STOPP-list in older patients; GheOP3s tool, Ghent older people’s Prescription community pharmacy screening; ACOVE, Assessing Care of Vulnerable Elders; STOPP-J, Screening Tool for Older Person’s Appropriate Prescriptions for Japanese.
Study Characteristics
Twenty-seven studies were included in this systematic literature review, all of which were quantitative (Table 3). Most quantitative studies were prospective studies,20–42 with five retrospective studies.43–47 The prospective studies included six randomized controlled trials,20–25 one non-randomized controlled trial,26 and one ambispective non-randomized controlled study.27 Moreover, there was one pilot study,36 three before-and-after studies,28–30 four observational studies,37,38–42 and nine interventional studies.31–35,38,39. Approximately 16,093 patients were included in the studies. Two papers did not state the number of participants.
Explicit Tools
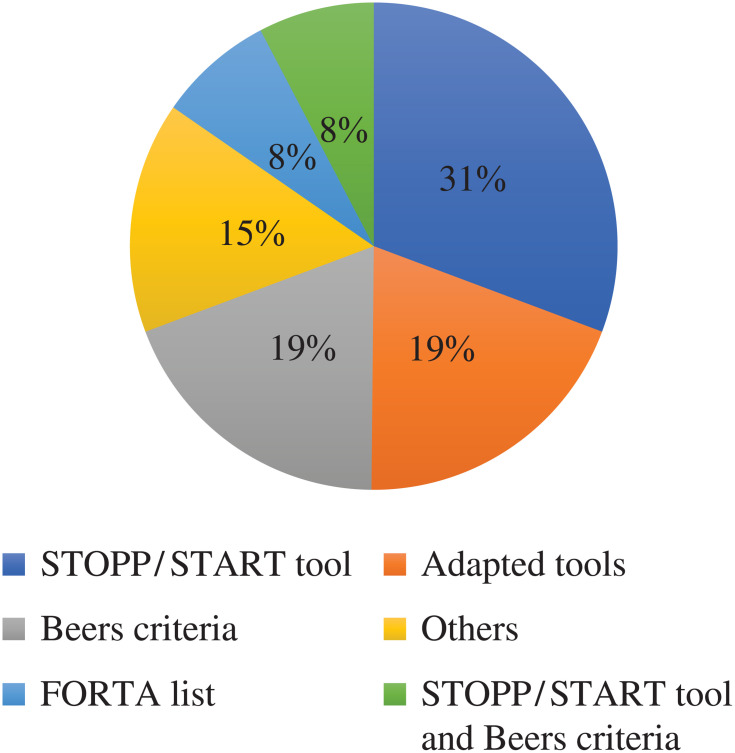
A wide range of tools was implemented to review PIM in hospitalized older patients. Most studies used various versions of the STOPP/START tool, which was originally developed in Ireland.21,22,27,29,33,37,39,47 This tool was used in studies conducted in Ireland, Belgium, India, Switzerland, Spain, and France. Beers criteria were implemented in six studies conducted in the United States, Belgium, Vietnam, Italy, Iran and Taiwan.24,30,31,43,45 Two studies used both STOPP/START and Beers criteria.32,36 One study implemented the intervention using three different tools STOPP/START, Beers criteria and PRISCUS list,35 and two studies used the FORTA list.23,25 Other tools were found to be used less frequently in reviewing PIM during hospital stay: the RASP, NORGEP, GheOP3S and STOPP-J tools. The RASP tool was used in a study conducted in Belgium,26 NORGEP was used in a study located in Norway,46 and the GheOP3S tool, originally designed for community pharmacy screening, was used in a Belgian study.41 STOPP-J was developed in Japan and was utilized in a Japanese study.40
The most adopted tools were STOPP/START and the Beers criteria. One study originating in Canada adapted STOPP/START and Beers criteria,20 two studies that adopted the Beers criteria were conducted in the United States and Canada,28,44 one study that adopted STOPP/START was conducted in Swaziland34 and one study conducted in France adopted three tools, PRISCUS, Beers and the Laroche list, through a Delphi panel.42 Figure 2 summarizes the tools used in PIM review.
Figure 2.
Explicit tools that were utilized to review elderly patients’ medication in hospitals.
HCP Involved in PIM Review
HCPs from different specialties were involved in implementing the intervention including physicians, hospital or clinical pharmacists, geriatricians, nurses, physical therapists, psychologist dietitians, occupational therapists, physical therapists, and speech therapists, with hospital or clinical pharmacists conducting the review in most studies (19 out of 27).20,24,26,27,30,33,35,36,38,39,41–44,46,47 In three studies, the physician used the STOP/START tool22 or the FORTA list.23,25 Three studies involved an interdisciplinary team: one included two hospital pharmacists and two geriatricians,42 another included nurses, geriatricians, dietitian, occupational therapist, physical therapist, speech therapist and a psychologist,21 while the other team consisted of a geriatrician and psychiatrist.34 The use of a computerized system instead of HCP to detect PIM was observed in two studies,28,45 and two studies did not report the HCP involved in implementing the intervention.29,37
PIM Review Process and Stage of Implementation
The application of explicit tools to reduce PIM during hospitalization was observed on admission (within 48 hours of hospitalization) and during the hospital stay, but not on discharge. Ten studies applied explicit tools on admission,21,22,26,28,29,31–33,35,40 nine studies during the hospital stay,20,23,24,30,34,36,37,46,47 and several studies did not report the stage of hospitalization in which the HCP used the tools.25,38,39,41–45
The HCPs involved in PIM detection based their decision on several sources, and any limitations in these sources may influence their clinical decisions. Several studies used only medication history and medication reconciliation26,29–31,33,39,42 while other studies depended on medication history and interviews with the patient or caregiver,27,32,36,47 and one article added a GP or community pharmacy contact.22 One study designed a collection book to record relevant data including medication list, lab values, vital signs and medical diagnosis.37 Four studies used clinical examination, medical records and reason for admission in addition to the medication history and interview with patient and caregiver.20,35,41,46 Five studies based their decision on patient specific data such as the Mini-Mental State Examination (MMSE), functional dependency, malnutrition, the Katz activities of daily living scale or the Charlson cumulative comorbidity index.21,23–25,34 Studies using a computerized system relied mainly on the patient profile in the system.20,28,44,45 One study did not report the type of data used to make their decision of PIM.38
The HCP or team included the medication list and other sources in the intervention review and communicated their recommendation verbally or in writing. In eight studies, the PIM was detected using explicit tools and the recommendations were communicated orally to the attending physician,20,21,24,26,33,35,36,44 while in four studies, the PIM was communicated in written form.27,39,41,42 Two studies communicated the recommendation verbally and written to the attending physician.31,32 Two studies used a computerized system to review PIM and communicated with the physician through an alert system,28,45 while in the other two studies, the computerized system and was assessed by the hospital pharmacist to detect PIM and the results communicated verbally to the attending physician.20,44 The remaining studies did not specify how the recommendations were communicated to the physician.22,23,25,29,33,34,37,38,40,43,46–48
Communicating the PIM review interventions to the GP was observed in two studies,26,34 with one study providing a letter to the patient or caregiver.27 The other study provided both the GP and the patient or caregiver with PIM changes made during hospitalization.24
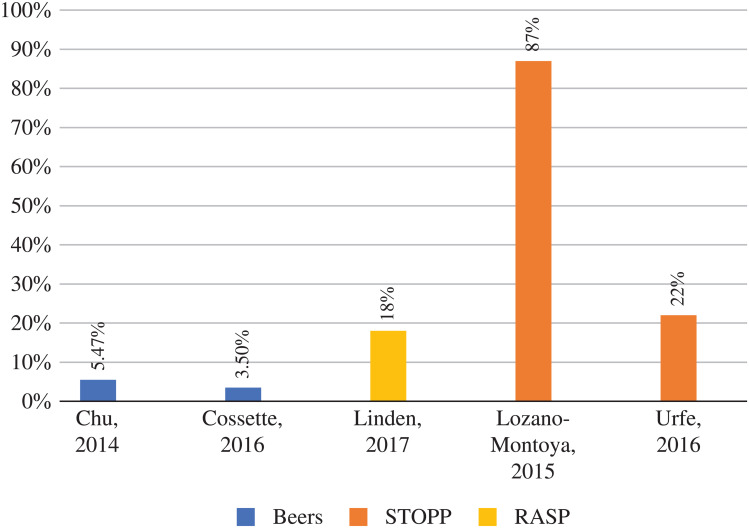
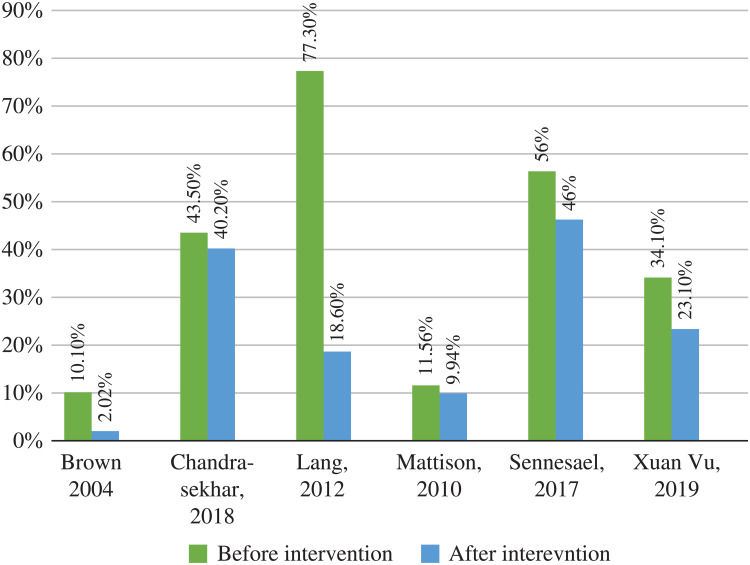
Intervention Outcomes: PIM Reduction
Two main methodologies were used to express the outcome of the intervention: the percentage of physician acceptance of intervention and/or the percentage of PIM reduction. Five studies measured the intervention outcome as the percentage reduction in PIM,26,27,29,38,44 with the reduction of PIM ranging from 3.5% up to 87% (Figures 3 and 4). The study associated with the highest PIM reduction was conducted by the hospital pharmacist, and the intervention was communicated to a team of three geriatricians and two clinical pharmacists.27 The lowest PIM reduction was observed in two studies in which the hospital pharmacist detected the PIM and it was sent to the attending physician.38,44
Figure 3.
Percentage of PIM reduction in hospitals with the tools used.
Figure 4.
Description of PIM reduction before and after tool implementation by HCP in hospitals.
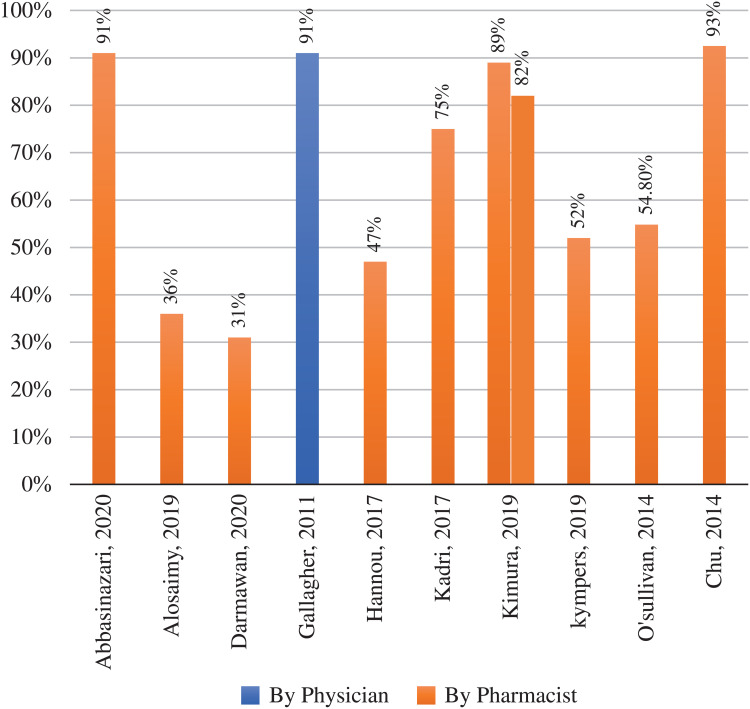
Physician acceptance of hospital or clinical pharmacist intervention varied from 36% to 92.5%, while interventions recommended by the physician generally were more accepted than those of the hospital or clinical pharmacist (91%) (Figure 5).
Figure 5.
The percentage accepting the recommendation for PIM reduction.
Seven studies used the STOPP/START tool and reported the potential prescribing omission (PPO).22,27,33,34,37,39,47 PPO were detected in 69 of 382 participants,22 195 of 210 patients,37 90 of 81 participants,39 and 397 of 346 participants.27 The highest acceptance rate was for PPO recommendations conducted by a physician at 97%, and the lowest rate of recommendation acceptance was 33.5% in a study conducted by a clinical pharmacist.
Two studies conducted in the United States and Canada measured the time required to complete the PIM review. One used a computerized system, and the mean time necessary to evaluate PIM was 41 ± 16 minutes per patient,20 while the other study was a pharmacist-led intervention and needed 49 ± 16 minutes per patients to fully complete the PIM review.36
Common PIM and Clinical Relevance
Sixteen articles identified the most commonly detected PIM,22,26–28,30,31,33,36,37,39–43,45,46 with benzodiazepines being the most common,27,30,31,33,36,41–43,45,46 followed by antipsychotics.33,37,41–43 Other common PIM included proton pump inhibitors (PPI),22,26 digoxin,45 NSAID,30,37,40 and anticholinergics.28,36,41,46
Two studies measured the clinical relevance of the recommendations by tools in the hospitalized older patients.21,41 A study evaluated the relevance of the GheOP3S tool by two criteria: 1) by the severity of the detected PM, which was evaluated by the treating geriatrician depending on the impact of ADR that could result if the clinical pharmacist did not intervene, and 2) the value of the clinical pharmacist recommendations using a validated patient specific scoring system.41 In the first evaluation of clinical relevance, it was shown that 182 (73%) of PIMs were serious and 67 (27%) were classified as significant.41 The second evaluation of clinical relevance found six items (2%) classified as very significant and 235 (94%) as significant. The second study used the STOPP/START tool and three experts evaluated the clinical relevance (geriatrician, GP and clinical pharmacist) using a 6-point scale system (minor: no benefit or minor benefit; moderate: improvement of the appropriateness of the level of practice or prevention of an adverse drug event of moderate importance; major: prevention of serious morbidity—including readmission—and serious adverse drug event; extreme: life-saving; deleterious: increased risk of health adverse event; non-applicable).21 The experts had access to the patient file to rate the recommendations independently and then discuss the discrepancies.21 The expert panel classified as major: 29%, moderate: 37, minor: 5%, deleterious 8%.21
Clinical and Non-Clinical Outcomes
Out of 25 studies included in this review, 8 examined the clinical effect of PIM reduction.20,22,27,28,30,33–35 Only one study looked at non-clinical effect, cost, of PIM reduction.16
Clinical Outcomes
PIM Reduction and Activities of Daily Living (ADL)
The ADL was measured by three articles,23,25,27 with one study reporting that non-statistically significant differences were found between ADL in the intervention and control groups (Barthel Index 70 in control and 80 in intervention group P<0.220).23 Two studies found a statistically significant relation between PIM reduction and improved ADL.25,27
PIM Reduction and Falls
The effect of reducing PIM in falls in older hospitalised patients was documented in three studies.22,23,26 Falls were lower in the intervention group; however, none of the three studies reported a statistically significant change in falls after the PIM reduction.
Hospitalization and Readmission
A number of studies measured the impact on hospital stay,20,22 in-hospital mortality,20,26,29 ED visits,20,27,33 and readmissions20,24,26,29 as well as GP visits.22 Two studies found a non-statistically significant link between PIM reduction and hospital stay.20,22 Similarly, a non-statistically significant link between PIM reduction and in-hospital mortality was reported in three studies.20,26,29 Four studies assessed the impact of PIM reduction on hospital readmission, and all four reported no statistical difference in hospital readmission between the intervention and control groups.20,24,26,29 Similarly, studies evaluating the association of ED visits and PIM reduction reported no difference or minimal difference, not statistically significant, between older patients in the intervention and those who were in the control groups.20,24,26 One study assessed GP visits and their relation to PIM reduction and reported that patients in the intervention group had fewer GP visits compared to patients in the control group; however, it was not statistically significant (P=0.063).22
Non-Clinical Outcomes
Assessing the cost associated with each intervention was rarely addressed in the literature, with one study measuring the total cost saving resulting from reducing PIM in terms of healthcare resources utilisation and medication.36 The study reported that the cost saving from the clinical intervention yielded approximately £63,000–144,000 as well as £68,000 annual medication savings.36
Discussion
This systematic review presented data from 25 studies that examined PIM review using explicit tools in hospitalized patients over 65 years old. This review specifically explored the explicit tools used in reviewing older patient medication in hospitals, which is usually done on admission and during the hospital stay. The hospital or clinical pharmacist was often found to review the medication of older patients. Variable PIM reduction percentages were reported by studies in this review.
In this review, several tools were identified as being used to detect PIM, with the STOPP/START tool being the most common. One reason for the preference of the STOPP/START tool over other tools might be the availability of a START list, which includes medications that should be prescribed for older adults. Moreover, STOPP/START tools have been shown to have higher PIM detection and higher clinical relevance than Beers criteria.48 However, another comparison study examined the detectability of PIM comparing two tools, STOPP/START and PIM-check, revealing that PIM-check detected three times more PIM than STOPP/START.43 This could be due to the fact that the PIM-check tool was developed by an international panel of experts, which may add another dimension to the detectability of PIM in research done in a country other the one where the tool was developed. A number of explicit tools were designed be used in a specific healthcare setting, but they are still effective in reducing PIM in other than the intended settings. For example, the Beers criteria were specifically designed to be used in nursing homes, but when it was used in hospitals, a statistically significant reduction in PIM was noted,38 even when it was integrated with a computerized system.45 In addition, the GheOP3S tool was proposed to be used in community pharmacies, but when it was applied in a hospital setting, it resulted in the physician accepting 52% of the recommendations, comparable to the acceptance rate of the STOPP/START tool.33 Nonetheless, careful adoption of explicit tools needs to be considered in healthcare settings other than those for which the tool was designed.24 Only two studies in this review have utilized the computerised automatic PIM detection. This could highly aid the HCP in PIM detection in hospitalized elderly. Future studies need to consider investigating the outcomes of the application of such automatic PIM detection in daily practice.
Another finding of this review is the point at which the PIM review occurred during hospitalization: on admission or during hospital stay. Several studies did not disclose when the PIM review took place, highlighting the lack of information regarding the most appropriate time to review PIM during hospitalization. It is difficult to recommend when the right time to detect PIM would take place because each point of the hospital journey has its pros and cons. For example, a full medication history is performed on admission, allowing identification of the causative agent that precipitated the admission.49,50 However, conducting the review during the hospital stay could help in improving the prescribing practice; many studies proved that the PIM increases during hospital stay.51,52 Among the various healthcare settings, hospital stay can be identified as the best place where PIM can be reviewed,49 because if there is a need to stop a PIM, the patient can be monitored by the HCP. The inpatient environment is considered one of the facilitators for deprescribing in hospitals, as the availability of resources and the patient mentioning to ensure safe deprescribing.53 Additionally, geriatricians and hospital pharmacist acknowledge their role to be more proactive and responsible in avoiding harm to patients. A study was done in a hospital in the UK to investigate whether medication reviews in a hospital lead to deprescribing of medications related to increase the risk of falls.54 The study recruited 100 patients over the age of 70 who were admitted due to falls, and these patients were followed prospectively. Medication reconciliations were done by pharmacists for 80% of the patients, and medication reviews were done for 86% of the patients. There are a number of patients (2%) that the doctor documented “review” to the pharmacist, but it was not carried out. Sixty-five out of 100 elderly patients were on medications that increased the risk of falls. After a comprehensive medication review, fall-risk medications of 23 of the 65 patients were reduced. After applying an analysis of the data, the medication review by the pharmacist was found statistically significant in reducing the fall-risk medications (P = 0.002).54 Deprescribing in 65 years and over inpatients shows promising outcomes as concluded Grazarin and colleagues study that was aimed at evaluating inpatient deprescribing initiatives.55 These studies emphasise how the hospital could be an opportunity to reduce PIM through collaborative work between physicians and pharmacists. On the other hand, a qualitative study reported that some physicians in primary care express some concerns regarding potentially adverse outcomes and follow-up from deprescribing and fast pace in daily practice.56
This review identified that physicians, pharmacist, and multidisciplinary teams are involved in the PIM review process in hospitals. Similarly to what was obtained in Thomas and Thomas (2019) review and Santos and colleagues (2019) review.11,57 To optimize the care of hospitalized elderly, HCPs need geriatric pharmacotherapy programs and training.58,59 Another important consideration is treating the patient in a holistic manner, as some physicians and specialist tend to focus their efforts on managing the acute state and reason for hospitalization.58,60,61
The reduction of PIM varied between studies, ranging from 3.5% up to 85%, and the recommendation acceptance ranged from 36% up to 93%. It is interesting to note that the physician has a higher PIM reduction and recommendation acceptance than the pharmacist, which may indicate a lack of effective communication.62 Additionally, the power dynamics might influence the relationship between pharmacists and physicians,63 as some physicians lack knowledge about the professional role and job description of the pharmacist. A possible way to strengthen the pharmacist–physician relationship is through a simulation involving face-to-face pharmacist and physician interaction,64 which could also increase the pharmacists’ confidence, helping them to be more proactive in collaboration with the physician. Physicians prefer face-to-face communication in terms of providing recommendations, as evident from a semi-structured interview:
The pharmacist comes and writes a note for you, but it’s not done face to face, and it actually is a bit antagonistic if anything …. having post-it [notes] stuck on things saying please review this, please review that, we all hate notes, everyone hates it, so I think that could be done better. So more pharmacy input, but more integrated pharmacy input.59
The method in which the recommendation is communicated to the physician is either written or verbal and could affect whether or not the recommendation status is approved.
Several explanations could elucidate the variation in PIM reduction. Firstly, the suitability of the explicit tool in the practice or setting. Advanced health care systems may reflect less PIM reduction as their practice is optimised by the guidelines and policies. Similarly, with geriatric hospitals or geriatric wards. The availability of the alternatives medications to PIM could lead to higher reductions. One of the influential aspect in the management and reduction of PIM is the patient choice as some of them might be physiologically attached to the prescribed medication. Fear and concerns are considered barriers to the reducing of the elderly’s medication as some of the elderly fear that they might miss the benefits of the deprescribed medication in the future.65–67 Another aspect that might hinder the deprescribing is related to patient expectations, as they are unfamiliar with the process of reducing instead of adding medication.65–68 One of the studies pointed out the influences on willingness to deprescribe, which could be carers or friends that have unsuccessfully stopped their medication.64 This will negatively influence the amount of medication stopped by physicians, which may reflect the variation in PIM reduction in this review.
Effective communication between primary care clinics and hospitals is essential for continuous healthcare.69 In several studies, the GP reported lack of sufficient information in discharge letters.70,71 Providing a letter to the patient and the GP indicating the changes and reasons behind stopping PIM is important so as not to reinitiate what was already discontinued. Engaging and empowering the patient will also help to sustain the changes, since many patients are reluctant to change or stop their medications.59 Additionally, improving the communication between hospitals and GPs is essential to increase patient safety.50,72 This can be improved by using a form that includes all vital information that needs to be sent to the GP.
The present review confirmed that only a few studies highlighted the clinical outcomes of PIM reduction. It was noted that reducing PIM was associated with improved ADL, fewer falls, fewer readmissions, and fewer GP visits. These findings were similar to what was reported by Hill-Taylor et al (2013) in a review that aimed to examine the impact of the STOPP/START tool application.73 The limited number of studies measuring PIM reduction clinical outcomes could be due to the nature of outcomes, which is often hard to evaluate. Additionally, it requires considerable effort of observation and reporting which could be labour and time consuming. Moreover, loss of follow-up could be one of the limitations investigating the clinical outcomes of PIM reduction. Despite that, it is vital to assess those outcomes to support deprescribing PIMs. Future studies need to address the clinical outcomes of such interventions.
It is worth noting that some of the study findings were not statistically significant. Confidence intervals and P values in the studies helped in assessing the clinical significance of the study results74; however, these statistical tools aid the decision but do not make the decision. Some effects are not statistically significant, but clinically, they can make a meaningful difference to the patient’s health.75 For a careful clinical decision and to deeply understand the impact of PIM reduction, more studies are required to investigate both the short- and long-term effects of reducing PIM as well as the economic aspect of this intervention.
Strengths and Limitations
This systematic review explored the application of different explicit tools in hospitals to review PIM, narratively synthesising the data to allow the identification of key aspects of the application of the explicit tools in the hospital, such as whether the HCP was involved in PIM review and what tools were utilized, the stage of hospitalization in which the PIM review occurred, as well as the clinical relevance of the PIM detected. In addition, numerous gaps and areas for future studies were noted. There were some limitations at the methodological level that are common in this kind of review, since non-English articles were excluded. The studies included in this review were located mostly in Europe and the United States, where the healthcare systems are more developed compared to other countries. In terms of analysis, studies used different methods to express the outcomes of the PIM review, so it was not possible to pool the data and perform statistical analysis for a meta-analysis.
Conclusion
PIM is a serious healthcare issue for older patients and can be improved through various means such as the use of implicit or explicit tools. This systematic review explored the practice of reviewing PIM in hospitalized patients using explicit tools, which showed promising outcomes in terms of improving PIM. Future studies need to consider the application of explicit tools in other healthcare settings setting to confirm the findings. PIM reduction is linked to better overall health of older patients and has a positive influence in reducing falls. Nonetheless, more studies need to be conducted to further investigate the outcomes of reviewing PIM at different levels, as well as assessing the clinical and cost-effectiveness of using such tools to minimize PIM.
Data Sharing Statement
Supplementary file upon request from the corresponding author (data extraction in Microsoft excel format).
Disclosure
The authors declare that they have no competing interests.
References
- 1.Jensen LD, Andersen O, Hallin M, Petersen J. Potentially inappropriate medication related to weakness in older acute medical patients. Int J Clin Pharm. 2014;36(3):570–580. doi: 10.1007/s11096-014-9940-y [DOI] [PubMed] [Google Scholar]
- 2.Renom-Guiteras A, Thürmann PA, Miralles R, et al. Potentially inappropriate medication among people with dementia in eight European countries. Age Ageing. 2018;47(1):68–74. doi: 10.1093/ageing/afx147 [DOI] [PubMed] [Google Scholar]
- 3.Morgan SG, Hunt J, Rioux J, Proulx J, Weymann D, Tannenbaum C. Frequency and cost of potentially inappropriate prescribing for older adults: a cross-sectional study. CMAJ Open. 2016;4(2):E346–E351. doi: 10.9778/cmajo.20150131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harrison SL, Kouladjian O’Donnell L, Milte R, et al. Costs of potentially inappropriate medication use in residential aged care facilities. BMC Geriatr. 2018;18(1):9. doi: 10.1186/s12877-018-0704-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. 2003;163(22):2716–2724. doi: 10.1001/archinte.163.22.2716 [DOI] [PubMed] [Google Scholar]
- 6.Piau A, Huet Y, Gallini A, Andre L, Vellas B, Nourhashemi F. Optimization of drug therapy in elderly individuals admitted to a geriatric unit. Clin Interv Aging. 2017;12:1691–1696. doi: 10.2147/CIA.S132309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goodwin MA, Stange KC, Zyzanski SJ, Crabtree BF, Borawski EA, Flocke SA. The Hawthorne effect in direct observation research with physicians and patients. J Eval Clin Pract. 2017;23(6):1322–1328. doi: 10.1111/jep.12781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laroche ML, Charmes JP, Nouaille Y, Fourrier A, Merle L. Impact of hospitalisation in an acute medical geriatric unit on potentially inappropriate medication use. Drugs Aging. 2006;23(1):49–59. doi: 10.2165/00002512-200623010-00005 [DOI] [PubMed] [Google Scholar]
- 9.Onatade R, Auyeung V, Scutt G, Fernando J. Potentially inappropriate prescribing in patients on admission and discharge from an older peoples’ unit of an acute UK hospital. Drugs Aging. 2013;30(9):729–737. doi: 10.1007/s40266-013-0097-5 [DOI] [PubMed] [Google Scholar]
- 10.Komagamine J. Prevalence of potentially inappropriate medications at admission and discharge among hospitalised elderly patients with acute medical illness at a single centre in Japan: a retrospective cross-sectional study. BMJ Open. 2018;8(7):e021152. doi: 10.1136/bmjopen-2017-021152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dos Santos NS, Marengo LL, Moraes FDS, Barberato-Filho S. Interventions to reduce the prescription of inappropriate medicines in older patients. Rev Saúde Pública. 2019;53:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sallevelt BTGM, Huibers CJA, Knol W, van Puijenbroek E, Egberts T, Wilting I. Evaluation of clarity of the STOPP/START criteria for clinical applicability in prescribing for older people: a quality appraisal study. BMJ Open. 2020;10(2):e033721. doi: 10.1136/bmjopen-2019-033721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American geriatrics society 2019 updated AGS Beers criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674–694. doi: 10.1111/jgs.15767 [DOI] [PubMed] [Google Scholar]
- 14.O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213–218. doi: 10.1093/ageing/afu145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Motter FR, Fritzen JS, Hilmer SN, Paniz ÉV, Paniz VMV. Potentially inappropriate medication in the elderly: a systematic review of validated explicit criteria. Eur J Clin Pharmacol. 2018;74(6):679–700. doi: 10.1007/s00228-018-2446-0 [DOI] [PubMed] [Google Scholar]
- 16.Higgins J, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. England: Wiley-Blackwell; 2008. [Google Scholar]
- 17.Hong QN, Pluye P, Fàbregues S, et al. Mixed methods appraisal tool (MMAT), version 2018. Canada: IC Canadian Intellectual Property Office; 2018. [Google Scholar]
- 18.Hong QN, Fàbregues S, Bartlett G, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34(4):285–291. doi: 10.3233/EFI-180221 [DOI] [Google Scholar]
- 19.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2017. Mar 29;372–n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cossette B, Éthier J-F, Joly-Mischlich T, et al. Reduction in targeted potentially inappropriate medication use in elderly inpatients: a pragmatic randomized controlled trial. Eur J Clin Pharmacol. 2017;73(10):1237–1245. doi: 10.1007/s00228-017-2293-4 [DOI] [PubMed] [Google Scholar]
- 21.Dalleur O, Boland B, Losseau C, et al. Reduction of potentially inappropriate medications using the STOPP criteria in frail older inpatients: a randomised controlled study. Drugs Aging. 2014;31(4):291–298. doi: 10.1007/s40266-014-0157-5 [DOI] [PubMed] [Google Scholar]
- 22.Gallagher PF, O’Connor MN, O’Mahony D. Prevention of potentially inappropriate prescribing for elderly patients: a randomized controlled trial using STOPP/START criteria. Clin Pharmacol Ther. 2011;89(6):845–854. doi: 10.1038/clpt.2011.44 [DOI] [PubMed] [Google Scholar]
- 23.Michalek C, Wehling M, Schlitzer J, Frohnhofen H. Effects of ‘Fit fOR The Aged’ (FORTA) on pharmacotherapy and clinical endpoints–a pilot randomized controlled study. Eur J Clin Pharmacol. 2014;70(10):1261–1267. doi: 10.1007/s00228-014-1731-9 [DOI] [PubMed] [Google Scholar]
- 24.Spinewine A, Swine C, Dhillon S, et al. Effect of a collaborative approach on the quality of prescribing for geriatric inpatients: a randomized, controlled trial. J Am Geriatr Soc. 2007;55(5):658–665. [DOI] [PubMed] [Google Scholar]
- 25.Wehling M, Burkhardt H, Kuhn-Thiel A, et al. VALFORTA: a randomised trial to validate the FORTA (Fit fOR The Aged) classification. Age Ageing. 2016;45(2):262–267. doi: 10.1093/ageing/afv200 [DOI] [PubMed] [Google Scholar]
- 26.der Linden LV, Decoutere L, Walgraeve K, et al. Combined use of the rationalization of home medication by an adjusted STOPP in older patients (RASP) list and a pharmacist-led medication review in very old inpatients: impact on quality of prescribing and clinical outcome. Drugs Aging. 2016;2(34):123–133. [DOI] [PubMed] [Google Scholar]
- 27.Lozano-Montoya I, Vélez-Diaz-Pallarés M, Delgado-Silveira E, Montero-Errasquin B, Cruz Jentoft AJ. Potentially inappropriate prescribing detected by STOPP–START criteria: are they really inappropriate? Age Ageing. 2015;44(5):861–866. doi: 10.1093/ageing/afv079 [DOI] [PubMed] [Google Scholar]
- 28.Mattison MLP, Afonso KA, Ngo LH, Mukamal KJ. Preventing potentially inappropriate medication use in hospitalized older patients with a computerized provider order entry warning system. Arch Intern Med. 2010;170(15):1331–1336. doi: 10.1001/archinternmed.2010.244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Urfer M, Elzi L, Dell-Kuster S, Bassetti S. Intervention to improve appropriate prescribing and reduce polypharmacy in elderly patients admitted to an internal medicine unit. PLoS One. 2016;11(11):e0166359. doi: 10.1371/journal.pone.0166359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xuan Vu T, Bui Thi Huong Q. The effect of the pharmacist’s intervention on potentially inappropriate medication use in older adults using the 2015 Beers criteria. Pharm Sci Asia. 2019;46(1):54–61. doi: 10.29090/psa.2019.01.017.0023 [DOI] [Google Scholar]
- 31.Abbasinazari M, Tavana A. Identification and acceptance of suggested therapeutic alternatives of potentially inappropriate medications amongst hospitalised geriatric patients in Iran. J Pharm Pract Res. 2020;50(1):75–77. doi: 10.1002/jppr.1583 [DOI] [Google Scholar]
- 32.Darmawan E, Ahmad H, Perwitasari DA, Kusumawardani N. Pharmacist intervention can reduce the potential use of inappropriate drugs medications in Indonesian geriatric patients. J App Pharm Sci. 2020;10(1):88–95. [Google Scholar]
- 33.Hannou S, Voirol P, Pannatier A, et al. Pharmacist intervention acceptance for the reduction of potentially inappropriate drug prescribing in acute psychiatry. Int J Clin Pharm. 2017;39(6):1228–1236. doi: 10.1007/s11096-017-0513-8 [DOI] [PubMed] [Google Scholar]
- 34.Lang PO, Vogt-Ferrier N, Hasso Y, et al. Interdisciplinary geriatric and psychiatric care reduces potentially inappropriate prescribing in the hospital: interventional study in 150 acutely ill elderly patients with mental and somatic comorbid conditions. J Am Med Dir Assoc. 2012;13(4):406.e1–406.e7. doi: 10.1016/j.jamda.2011.03.008 [DOI] [PubMed] [Google Scholar]
- 35.O’Sullivan D, O’Mahony D, O’Connor MN, et al. The impact of a structured pharmacist intervention on the appropriateness of prescribing in older hospitalized patients. Drugs Aging. 2014;31(6):471–481. doi: 10.1007/s40266-014-0172-6 [DOI] [PubMed] [Google Scholar]
- 36.Alosaimy S, Vaidya A, Day K, Stern G. Effect of a pharmacist-driven medication management intervention among older adults in an inpatient setting. Drugs Aging. 2019;36(4):371–378. doi: 10.1007/s40266-018-00634-9 [DOI] [PubMed] [Google Scholar]
- 37.Chandrasekhar D, Samjas M, Pattani D. Evaluation of potentially inappropriate medications among hospitalized geriatric patients in tertiary care referral hospital using STOPP/START criteria. Clin Epidemiol Glob Health. 2018. Available from http://www.sciencedirect.com/science/article/pii/S2213398418300216. Accessed October 15, 2021. [Google Scholar]
- 38.Chu LL, Su HC, Wang HY. Construct a CPOE decision supporting and monitoring system to decrease PIMS used in hospitalized elderly patients. Value Health. 2014;17(7):A754–A755. doi: 10.1016/j.jval.2014.08.220 [DOI] [PubMed] [Google Scholar]
- 39.Kadri B, Tritz T, Lecoeur A, Mercier FL, Cudennec T. CP-030 assessment of medical care for older patients in an acute geriatric department with the stopp/start criteria. Eur J Hosp Pharm. 2017;24(Suppl 1):A13. [Google Scholar]
- 40.Kimura T, Ogura F, Kukita Y, et al. Efficacy of pharmacists’ assessment and intervention based on Screening Tool for Older Persons’ Appropriate Prescriptions for Japanese compared with Screening Tool of Older Persons’ potentially inappropriate prescriptions criteria version 2 in older patients with cardiovascular disease. Geriatr Gerontol Int. 2019;19(11):1101–1107. [DOI] [PubMed] [Google Scholar]
- 41.Kympers C, Tommelein E, Van Leeuwen E, Boussery K, Petrovic M, Somers A. Detection of potentially inappropriate prescribing in older patients with the GheOP3S-tool: completeness and clinical relevance. Acta Clin Belg. 2019;74:126–136. [DOI] [PubMed] [Google Scholar]
- 42.Pandraud-Riguet I, Bonnet-Zamponi D, Bourcier E, et al. Monitoring of potentially inappropriate prescriptions in older inpatients: a French multicenter study. J Am Geriatr Soc. 2017;65(12):2713–2719. doi: 10.1111/jgs.15081 [DOI] [PubMed] [Google Scholar]
- 43.Brown B, Earnhart J. Pharmacists and their effectiveness in ensuring the appropriateness of the chronic medication regimens of geriatric inpatients [Internet]. 2004. [cited April 2, 2019]. Available from: https://www.ingentaconnect.com/content/ascp/tcp/2004/00000019/00000005/art00003. Accessed October 15, 2021. [DOI] [PubMed]
- 44.Cossette B, Bergeron J, Ricard G, et al. Knowledge translation strategy to reduce the use of potentially inappropriate medications in hospitalized elderly adults. J Am Geriatr Soc. 2016;64(12):2487–2494. doi: 10.1111/jgs.14322 [DOI] [PubMed] [Google Scholar]
- 45.Ghibelli S, Marengoni A, Djade CD, et al. Prevention of inappropriate prescribing in hospitalized older patients using a computerized prescription support system (INTERcheck(®)). Drugs Aging. 2013;30(10):821–828. doi: 10.1007/s40266-013-0109-5 [DOI] [PubMed] [Google Scholar]
- 46.Kersten H, Hvidsten LT, Gløersen G, Wyller TB, Wang-Hansen MS. Clinical impact of potentially inappropriate medications during hospitalization of acutely ill older patients with multimorbidity. Scand J Prim Health Care. 2015;33(4):243–251. doi: 10.3109/02813432.2015.1084766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sennesael A-L, Dalleur O, Henrard S, Artoisenet C, Schoevaerdts D, Spinewine A. Implementing a screening tool to improve prescribing in hospitalized older patients: a pilot study. Int J Clin Pharm. 2018;40(1):15–19. doi: 10.1007/s11096-017-0563-y [DOI] [PubMed] [Google Scholar]
- 48.Boland B, Guignard B, Dalleur O, Lang PO. Application of STOPP/START and Beers criteria: compared analysis on identification and relevance of potentially inappropriate prescriptions. 2016. [cited April 2, 2019]; Available from: https://www.sciencedirect.com/science/article/pii/S1878764916300286. Accessed October 15, 2021.
- 49.Henschel F, Redaelli M, Siegel M, Stock S. Correlation of incident potentially inappropriate medication prescriptions and hospitalization: an analysis based on the PRISCUS list. Drugs Real World Outcomes. 2015;2(3):249–259. doi: 10.1007/s40801-015-0035-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ní Chróinín D, Neto HM, Xiao D, et al. Potentially inappropriate medications (PIMs) in older hospital in-patients: prevalence, contribution to hospital admission and documentation of rationale for continuation. Australas J Ageing. 2016;35(4):262–265. doi: 10.1111/ajag.12312 [DOI] [PubMed] [Google Scholar]
- 51.Pérez T, Moriarty F, Wallace E, McDowell R, Redmond P, Fahey T. Prevalence of potentially inappropriate prescribing in older people in primary care and its association with hospital admission: longitudinal study. BMJ. 2018;363:k4524. doi: 10.1136/bmj.k4524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rothberg MB, Pekow PS, Liu F, et al. Potentially inappropriate medication use in hospitalized elders. J Hosp Med. 2008;Mar(2):91–102. doi: 10.1002/jhm.290 [DOI] [PubMed] [Google Scholar]
- 53.Scott S, Twigg MJ, Clark A, et al. Development of a hospital deprescribing implementation framework: a focus group study with geriatricians and pharmacists. Age Ageing. 2020;49(1):102–110. doi: 10.1093/ageing/afz133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Marvin V, Ward E, Poots AJ, Heard K, Rajagopalan A, Jubraj B. Deprescribing medicines in the acute setting to reduce the risk of falls. Eur J Hosp Pharm. 2017;24(1):10–15. doi: 10.1136/ejhpharm-2016-001003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gazarin M, Devin B, Tse D, et al. Evaluating an inpatient deprescribing initiative at a rural community hospital in Ontario. Can Pharm J. 2020;153(4):224–231. doi: 10.1177/1715163520929734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wallis KA, Andrews A, Henderson M. Swimming against the tide: primary care physicians’ views on deprescribing in everyday practice. Ann Fam Med. 2017;15(4):341–346. doi: 10.1370/afm.2094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thomas RE, Thomas BC. A systematic review of studies of the STOPP/START 2015 and American geriatric society Beers 2015 criteria in patients ≥ 65 years. Curr Aging Sci. 2019;12(2):121–154. doi: 10.2174/1874609812666190516093742 [DOI] [PubMed] [Google Scholar]
- 58.Al Shemeili S, Klein S, Strath A, Fares S, Stewart D. An exploration of health professionals’ experiences of medicines management in elderly, hospitalised patients in Abu Dhabi. Int J Clin Pharm. 2016;38(1):107–118. doi: 10.1007/s11096-015-0212-2 [DOI] [PubMed] [Google Scholar]
- 59.Cullinan S, Fleming A, O’Mahony D, et al. Doctors’ perspectives on the barriers to appropriate prescribing in older hospitalized patients: a qualitative study. Br J Clin Pharmacol. 2015;79(5):860–869. doi: 10.1111/bcp.12555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Manias E. Effects of interdisciplinary collaboration in hospitals on medication errors: an integrative review. Expert Opin Drug Saf. 2018;17(3):259–275. doi: 10.1080/14740338.2018.1424830 [DOI] [PubMed] [Google Scholar]
- 61.Spinewine A, Swine C, Dhillon S, et al. Appropriateness of use of medicines in elderly inpatients: qualitative study. BMJ. 2005;331(7522):935. doi: 10.1136/bmj.38551.410012.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ferner RE, Aronson JK. Medication errors, worse than a crime. Lancet. 2000;355(9208):947–948. doi: 10.1016/S0140-6736(00)99025-1 [DOI] [PubMed] [Google Scholar]
- 63.McDonald J, Jayasuriya R, Harris MF. The influence of power dynamics and trust on multidisciplinary collaboration: a qualitative case study of type 2 diabetes mellitus. BMC Health Serv Res. 2012;12(1):63. doi: 10.1186/1472-6963-12-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chui MA, Stone JA, Odukoya OK, Maxwell L. Facilitating collaboration between pharmacists and physicians using an iterative interview process. J Am Pharm Assoc. 2014;54(1):35–41. doi: 10.1331/JAPhA.2014.13104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Goyal P, Requijo T, Siceloff B, et al. Patient-reported barriers and facilitators to deprescribing cardiovascular medications. Drugs Aging. 2020;37(2):125–135. doi: 10.1007/s40266-019-00729-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Reeve E, Low L-F, Hilmer SN. Beliefs and attitudes of older adults and carers about deprescribing of medications: a qualitative focus group study. Br J Gen Pract. 2016;66(649):e552–e560. doi: 10.3399/bjgp16X685669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zechmann S, Trueb C, Valeri F, Streit S, Senn O, Neuner-Jehle S. Barriers and enablers for deprescribing among older, multimorbid patients with polypharmacy: an explorative study from Switzerland. BMC Fam Pract. 2019;20(1):64. doi: 10.1186/s12875-019-0953-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Luymes CH, van der Kleij RMJJ, Poortvliet RKE, de Ruijter W, Reis R, Numans ME. Deprescribing potentially inappropriate preventive cardiovascular medication: barriers and enablers for patients and general practitioners. Ann Pharmacother. 2016;50(6):446–454. doi: 10.1177/1060028016637181 [DOI] [PubMed] [Google Scholar]
- 69.Vermeir P, Vandijck D, Degroote S, et al. Communication in healthcare: a narrative review of the literature and practical recommendations. Int J Clin Pract. 2015;69(11):1257–1267. doi: 10.1111/ijcp.12686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Weetman K, Dale J, Spencer R, Scott E, Schnurr S. GP perspectives on hospital discharge letters: an interview and focus group study. BJGP Open. 2020;4(2):bjgpopen20X101031. doi: 10.3399/bjgpopen20X101031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wills M, Hyland L, Chearman T, Cross F, Verrier-Jones K. GP and hospital doctor perspectives on the hospital patient discharge process. Bull Royal Coll Surg Engl. 2011;93(1):1–4. doi: 10.1308/147363511X546518 [DOI] [Google Scholar]
- 72.Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841. doi: 10.1001/jama.297.8.831 [DOI] [PubMed] [Google Scholar]
- 73.Hill‐Taylor B, Sketris I, Hayden J, Byrne S, O’Sullivan D, Christie R. Application of the STOPP/START criteria: a systematic review of the prevalence of potentially inappropriate prescribing in older adults, and evidence of clinical, humanistic and economic impact. J Clin Pharm Ther. 2013;38(5):360–372. doi: 10.1111/jcpt.12059 [DOI] [PubMed] [Google Scholar]
- 74.Ferrill MJ, Brown DA, Kyle JA. Clinical versus statistical significance: interpreting P values and confidence intervals related to measures of association to guide decision making. J Pharm Pract. 2010;23(4):344–351. doi: 10.1177/0897190009358774 [DOI] [PubMed] [Google Scholar]
- 75.Page P. Beyond statistical significance: clinical interpretation of rehabilitation research literature. Int J Sports Phys Ther. 2014;9(5):726–736. [PMC free article] [PubMed] [Google Scholar]