Abstract
Introduction
Acute-on-chronic liver failure (ACLF) patients are susceptible to invasive fungal infections. We evaluated the prognosis and antifungal options in ACLF patients with invasive pulmonary aspergillosis (IPA).
Methods
ACLF patients with IPA from 15 hospitals were retrospectively screened from 2011 to 2018, and 383 ACLF patients without lung infections were included from a prospective cohort (NCT02457637). Demographic, laboratory, clinical data, and 28-day outcomes were documented in the two cohorts.
Results
ACLF patients with probable IPA (n = 145) had greater 28-day mortality (33.6% vs. 15.7%, p < 0.001) than those without (n = 383). The respiratory failure-associated 28-day mortality was greater in ACLF patients with IPA than in those without before (17.1% vs. 0.3%, p < 0.001) and after (16.0% vs. 0.0%, p < 0.001) propensity score matching in 116 pairs. IPA patients with lung injury had greater 28-day all-cause mortality (66.5% vs. 24.2%, p < 0.001) and IPA-associated mortality (45.8% vs. 8.1%, p < 0.001) than patients without lung injury (PaO2/FiO2 ≥ 400 mmHg). Antifungal therapy was prescribed to 139 of 145 patients, and 102 patients were treated with voriconazole alone (n = 59) or sequential/combined therapy (n = 43) with varying loading doses (100–800 mg) and daily maintenance doses (0–800 mg). A proposed optimal voriconazole regimen (loading dose, 200 mg twice daily; daily maintenance dose, 100 mg) achieved comparable short-term survival and optimal trough drug concentrations (1–5 μg/mL) on therapeutic drug monitoring in 26 patients.
Conclusion
Presence of IPA increases the short-term mortality of ACLF patients mainly due to respiratory failure. An optimal voriconazole regimen is needed for such critical patients.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40121-021-00524-5.
Keywords: Acute-on-chronic liver failure, Invasive pulmonary aspergillosis, Lung injury, Organ failure, Prognosis, Propensity score matching, Respiratory failure, Voriconazole, Therapeutic drug monitoring
Key Summary Points
| Why carry out this study? |
| Acute-on-chronic liver failure (ACLF) patients are susceptible to invasive fungal infections. |
| We evaluated the prognosis and antifungal options in ACLF patients with invasive pulmonary aspergillosis (IPA). |
| What was learned from the study? |
| Presence of IPA increases the short-term mortality of ACLF patients mainly due to respiratory failure. |
| An optimal voriconazole regimen is needed for such critical patients. |
Introduction
Acute-on-chronic liver failure (ACLF) is a critical syndrome caused by acute deterioration of underlying chronic liver diseases characterized by organ failure(s) and high short-term mortality [1, 2]. An immune paresis accompanied with intensive systemic inflammation is observed in ACLF patients, which imposes an increased risk of developing infections [3]. For example, the incidence of bacterial infections in ACLF increases to as high as two times that of decompensated cirrhosis [4, 5]. Moreover, ACLF also increases the risk of opportunistic infections, including fungal and cytomegalovirus infections [4, 6]. In addition to multi-drug resistance, Aspergillus flavus is another leading cause of antibiotic treatment failure [7].
Invasive pulmonary aspergillosis (IPA) is one of the opportunistic infections seen in severely immunocompromised patients, including those undergoing hematopoietic stem cell transplantation, and in non-neutropenic patients, including those with liver cirrhosis or recipients of orthotopic liver transplantations, both of whom have high morbidity and mortality [8–10]. An increasing incidence of IPA is also observed in patients with critical liver disorders, suggesting that severely impaired liver function is a risk factor for IPA [11–15]. We previously reported that the incidence of IPA in patients with critical liver diseases ranges from 4 to 14%, and the short-term mortality rate has increased by more than 70% over the past decade [14].
However, data about IPA in liver failure patients has always been scarce. Given the rarity of cases of IPA in patients with ACLF, this multicenter study included 15 tertiary hospitals. However, as making a definite IPA diagnosis by a lung biopsy or bronchoscopy with bronchoalveolar lavage is practically challenging in such patients because of severe coagulopathy and significant thrombocytopenia [16], we focused on patients who met the diagnostic criteria for probable IPA. The purposes of our research were to characterize clinical features of ACLF patients complicated with IPA, to investigate the effect of IPA on the prognosis of ACLF, to explore the risk factors associated with the short-term prognosis, and to explore the benefit and safety of different antifungal treatments.
Method
Patients
ACLF patients with probable IPA were retrospectively screened from hospitalized ACLF patients admitted to 15 tertiary hospitals between January 1, 2011, and September 22, 2018, across China. ACLF was diagnosed according to the Asian Pacific Association for the Study of the Liver consensus [1]. Patients were excluded from the study if they had lung infections without a possible diagnosis of IPA, or did not meet probable IPA diagnostic criteria (Fig. 1a). The number of ACLF patients with IPA enrolled from each hospital is listed in Figure S1. Clinical and laboratory data were collected as a diagnosis of probable IPA was established in these ACLF patients, and organ injuries/failures and 28-day outcomes were also documented.
Fig. 1.
Flow chart of patient selection: a ACLF patients with probable IPA diagnosis were enrolled retrospectively from 15 hospitals; b ACLF patients without lung infections were enrolled from a multicenter and prospective cohort
ACLF patients without lung infection were drawn from a prospective cohort (NCT02457637) enrolled from 11 tertiary hospitals from 2015 to 2016, and the protocol has been described previously [17]. Patients with ACLF diagnosis and lung infections evidenced by chest computed tomography or radiographs were excluded (Fig. 1b). Clinical data for these ACLF patients at admission were collected and 28-day outcomes were also documented.
Diagnosis of IPA
The diagnosis of IPA was classified as proven, probable, possible IPA, or Aspergillus colonization according to the definitions of the European Organization for Research and Treatment of Cancer/Mycoses Study Group [10]. Due to the severe coagulopathy and the concern of bleeding complication, none of the ACLF patients underwent bronchoscopy for needle aspiration, biopsy, or bronchoalveolar lavage. Considering ACLF as a host risk factor for IPA [18], patients with possible IPA were defined as having probable IPA if they met both of the following criteria: (1) the presence of abnormal radiologic findings compatible with pulmonary infection, including classical signs of IPA (dense, well-circumscribed lesions with or without a halo sign, air crescent sign, or cavity) or non-classical findings such as masses and (2) the presence of Aspergillus species indicated by direct test (direct microscopy or culture) or galactomannan antigen detected in plasma with a cut-off point value of 0.5 [10].
Treatment of ACLF and IPA
The management of ACLF patients ranged from treatment against acute precipitating events/complications to nutrition and organ supporting, as previously reported [19]. A total of ten patients underwent liver transplantation in control and IPA groups, with four in IPA group. All the four patients had resolved IPA before LT.
Most patients with ACLF complicated by IPA were treated with either voriconazole alone, echinocandin alone, or a combination of voriconazole and echinocandin. Amphotericin B (AmB) was used in four patients, of which two received aerosol inhalation and the other two received systemic use of AmB. With respect to potentially drug-induced liver injury [20], the loading and maintenance doses of voriconazole varied among centers and patients; these were determined independently by the attending physicians [14]. Therapeutic drug monitoring was performed in some patients treated with voriconazole at two institutions (Nanfang Hospital and the 5th Medical Center, PLA General Hospital) as described previously [14].
Data Collection, Outcome and Follow-Up
The following data were collected in a pre-designed unified electronic data capture system by an assessor from each center: (1) demographic information including age, sex, height, and body weight; (2) host factors including smoking history, diabetes, hematological or oncological malignancy, congenital or acquired immunodeficiency, and recent use of cytotoxic agents or glucocorticoids; (3) signs and symptoms resembling IPA, radiological findings, microbiological data, and plasma voriconazole concentrations; and (4) laboratory panels, complications and organ failures. Organ failures in ACLF patients were defined according to the chronic liver failure–sequential organ failure assessment (CLIF-SOFA) score as: respiratory failure: PaO2/FiO2 ≤ 200 or SpO2/FiO2 ≤ 214; liver failure: bilirubin ≥ 12 mg/dl; Kidney failure: creatinine ≥ 2.0 mg/dl; cerebral failure: HE grade III and IV; coagulation failure: INR ≥ 2.5 or platelet count ≤ 20 × 109/l; and circulation failure: use of vasoactive drugs. The ACLF grades were classified according to the number of organ failures as ACLF grade 1, ACLF grade 2, and ACLF grade 3.
The primary outcome of the study was 28-day transplant-free mortality and 28-day transplant-free mortality associated with respiratory failure. Data on the 28-day clinical outcome information were obtained by checking medical records or telephone contact. The ethics committee of the Nanfang Hospital reviewed and approved this study. Written consent from patients or their authorized representatives was waived because of the retrospective nature of the study.
Statistical Analysis
Continuous variables between groups were compared using the Student’s t test or Mann–Whitney U test. Nominal variables were compared using the chi-squared test. Cumulative survival curves were presented using Kaplan–Meier plots and compared by the log-rank test. All survival curves were detected using the two-stage test. Patients receiving liver transplantation were excluded from the survival analysis. The performance of the SOFA lung score in discriminating the prognosis of ACLF patients with IPA was assessed by the area under the receiver operating characteristic curve (AuROC).
To avoid the potential bias of covariates not evenly distributed between IPA patients and non-IPA patients at baseline, a propensity score matching (PSM) analysis was performed. The propensity score was determined using a logistic regression model. The model included all the covariables for which a significant difference (p < 0.20) was found between the two groups: albumin, serum sodium, creatinine, and total bilirubin. In this analysis, we estimated the PSM models using 1-to-1 nearest-neighbor matching techniques without replacement and a caliper level of 0.05. It allowed the matching of 116 pairs of patients with similar characteristics. All statistical analyses were performed using SPSS v.20.0 (SPSS, Chicago, IL, USA). All tests were two-sided and p < 0.05 was considered statistically significant.
Results
Clinical Characteristics of ACLF Patients with IPA
A total of 145 ACLF patients with probable IPA were included in the study (Fig. 1a). The median time from admission due to ACLF to IPA diagnosis was 11 (0–61) days. The clinical characteristics of the enrolled IPA patients are shown in Table 1. The most frequent signs or symptoms observed in IPA patients were dyspnea (46.9%), refractory fever (46.2%), and worsening respiratory insufficiency (38.6%) (Table 2).
Table 1.
Clinical characteristics of ACLF patients with IPA
| Whole cohort (n = 145) | |
|---|---|
| Sex, M/F, | 123/22 |
| Age in years, mean(SD) | 46.77 (12.72) |
| Weight in kg, mean(SD) | 69.29 (14.62) |
| BW > 40 kg, n (%) | 120 (82.8%) |
| HBV, n (%) | 120 (82.8%) |
| Alcoholic hepatitis | 20 (13.8%) |
| Autoimmune liver disease | 9 (6.2%) |
| Platelet count > 100 × 109/L, | 22 (15.2%) |
| 50 < Platelet count < 100 × 109/L | 56 (38.6%) |
| Platelet count < 50 × 109/L, | 67 (46.2%) |
| International normalized ratio > 2.5 | 59 (40.7%) |
| 1.5 < International normalized ratio ≤ 2.5, | 79 (54.5%) |
| International normalized ratio < 1.5 | 7 (4.8%) |
| Organ failure | |
| Cerebral failure | 12 (8.3%) |
| Circulation failure | 6 (4.1%) |
| Coagulation failure | 63 (43.4%) |
| Kidney failure | 14 (9.7%) |
| Liver failure | 129 (89.0%) |
| SOFA lung score = 0 | 63 (43.4%) |
| SOFA lung score = 1 | 20 (13.8%) |
| SOFA lung score = 2 | 47 (32.4%) |
| SOFA lung score = 3 | 14 (9.7%) |
| SOFA lung score = 4 | 1 (0.7%) |
BW body weight, HBV hepatitis B virus, EASL-CLIF European Association for the Study of the Liver-Chronic Liver Failure consortium, SOFA sequential organ failure assessment score
Table 2.
Clinical sign and mycological findings of ACLF patients with IPA
| Whole cohort (n = 145) | |
|---|---|
| Signs and symptoms | |
| Refractory fever | 67 (46.2%) |
| Recrudescent fever | 36 (24.8%) |
| Pleuritic chest pain | 4 (2.8%) |
| Pleuritic rub | 15 (10.3%) |
| Dyspnea | 68 (46.9%) |
| Hemoptysis | 32 (22.1%) |
| Worsening respiratory insufficiency | 56 (38.6%) |
| Disseminated infection | 3 (2.1%) |
| Leukocyte count in 109/l, mean(SD) | 12.38 (7.40) |
| Neutrophils, mean (SD) | 80.00 (10.86) |
| Neutrophils count in 109/l, mean(SD) | 10.30 (6.78) |
| C-reactive protein in mg/l, mean(SD) | 35.75 (26.26) |
| Procalcitonin in ng/ml, median (interquartile range) | 1.08 [0.12,129.00] |
| Mycological findings, n (%) | |
| Direct test (cytology, direct microscopy, or culture) | 100 (69.0%) |
| Aspergillus fumigatus | 69 (69.0%) |
| Aspergillus flavus | 22 (22.0%) |
| Galactomannan antigen detected in plasma | 71 (49.0%) |
BW body weight, HBV hepatitis B virus, EASL-CLIF European Association for the Study of the Liver- Chronic Liver Failure consortium, SOFA sequential organ failure assessment score, Refractory fever fever refractory to at least 3 d of appropriate antibiotic therapy, Recrudescent fever recrudescent fever after a period of defervescence of at least 48 h while still on antibiotics and without other apparent cause, Worsening respiratory insufficiency worsening respiratory insufficiency in spite of appropriate antibiotic therapy and ventilatory support
Regarding the classical radiological features of IPA, dense, well-circumscribed lesions with or without a halo sign were observed in 27.6%, cavity in 15.9%, and air crescent sign in 1.4% of the cases. Regarding mycological findings, 69.0% (100/145) of ACLF patients with IPA had direct positive Aspergillus sputum examination or cultures. A. fumigatus and A. flavus were identified as the pathogens in 69 and 22 cases, respectively. Half (49.0%, 71/145) of the ACLF patients with IPA had direct positive galactomannan antigen in plasma (Table 2). Only 26 patients had both microbiological and serological evidence of IPA.
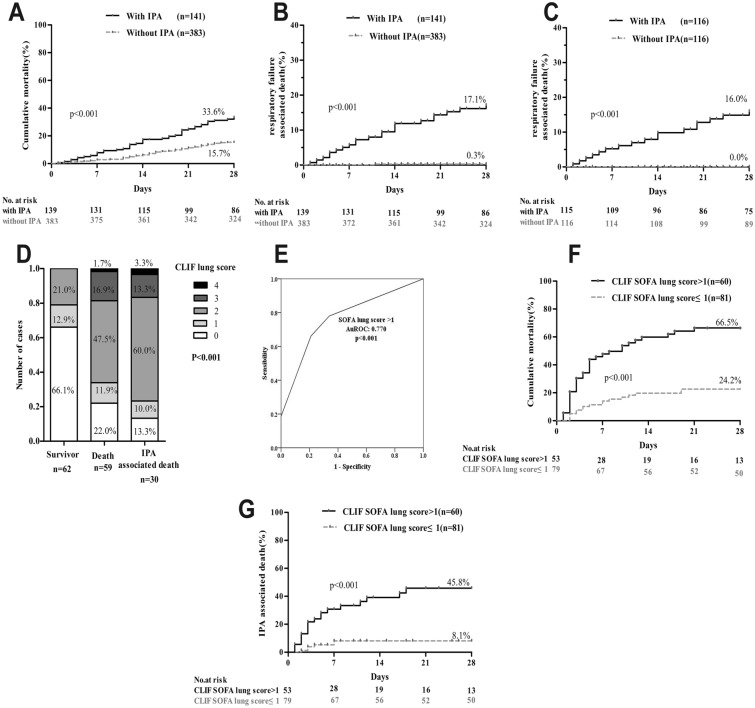
Liver transplantation was performed in four ACLF patients with IPA who were resolved by antifungal therapies, and these patients were excluded from the survival analysis. PSM was performed between IPA patients and non-IPA patients, and clinical data before and after PSM are shown in Supplementary Table 1. The 28-day mortality was significantly greater in the IPA group than in the control group (33.6% vs. 15.7%, p < 0.001; Fig. 2a). The 28-day mortality attributed to respiratory failure was low in the control group (0.3%, 1/383) but as high as 17.1% (22/141) in the IPA group (p < 0.001; Fig. 2b). After PSM, 116 pairs of ACLF patients were included in survival analysis. The 28-day mortality attributed to respiratory failure was also greater in ACLF patients with IPA (p < 0.001; Fig. 2c) than in ACLF patients without IPA.
Fig. 2.
Impact of IPA on mortality: a cumulative 28-day mortality of patients with or without IPA. Log-rank test performed (33.6% vs. 15.7%, p < 0.001); b cumulative respiratory failure-associated mortality of patients with or without IPA before PSM (17.1% vs. 0.4%, p < 0.001); c cumulative respiratory failure-associated mortality of patients with or without IPA after PSM (16.0% vs. 0.0%, p < 0.001); d distribution of SOFA lung score in survivors and IPA-associated deaths; e ROC curves of SOFA lung score in differentiating death and survival; f cumulative 28-day mortality of patients with lung score > 1 and lung score ≤ 1 (66.5% vs. 24.2%, p < 0.001); g cumulative respiratory failure-associated mortality of patients with lung score > 1 and lung score ≤ 1(45.8% vs. 8.1%, p < 0.001)
SOFA Lung Score can Predict the Prognosis of ACLF Patients with IPA
Respiratory injury and associated mortality were predominant in our ACLF patients with IPA. The SOFA lung score [21] is used to evaluate the severity of respiratory dysfunction or failure, and we hypothesized that it was applicable in ACLF patients with IPA. SOFA lung score > 1 strongly predicted the short-term outcomes of IPA patients (AuROC 0.770; Fig. 2e). Clinical manifestations in ACLF patients with SOFA lung score > 1 and those with SOFA lung score ≤ 1 are presented and compared in Table 3. Patients with IPA-associated death had a significantly worsened lung condition at the time of IPA diagnosis, as shown by higher SOFA lung scores (Fig. 2d). Our analysis showed that the 28-day mortality of patients with a SOFA lung score > 1 was significantly higher than that of patients with a score ≤ 1 (66.5% vs. 24.6%, p < 0.001; Fig. 2f). Similarly, the mortality caused by respiratory failure was significantly higher in the lung score > 1 group than in the lung score ≤ 1 group (45.8% vs. 8.1%, p < 0.001; Fig. 2g).
Table 3.
Clinical signs of IPA patients with CLIF lung score ≤ 1 or CLIF lung score > 1
| SOFA lung score ≤ 1 (n = 83) | SOFA lung score > 1 (n = 62) | p value | |
|---|---|---|---|
| Number | 83 | 62 | |
| Age in years, mean (SD) | 44.31 (11.69%) | 50.05 (13.38%) | 0.010 |
| Signs and symptoms | |||
| Refractory fever | 31 (37.3%) | 36 (58.1%) | 0.022 |
| Recrudescent fever | 17 (20.5%) | 19 (30.6%) | 0.182 |
| Pleuritic chest pain | 3 (3.6%) | 1 (1.6%) | 0.791 |
| Pleuritic rub | 5 (6.0%) | 10 (16.1%) | 0.057 |
| Dyspnea | 30 (36.1%) | 38 (61.3%) | 0.005* |
| Hemoptysis | 12 (14.5%) | 20 (32.3%) | 0.015* |
| Worsening respiratory insufficiency | 22 (26.5%) | 34 (54.8%) | 0.001* |
p value from Pearson’s v2 test or Fisher’s exact test in univariate analysis
BW body weight, HBV hepatitis B virus, EASL-CLIF European Association for the Study of the Liver- Chronic Liver Failure consortium, SOFA sequential organ failure assessment score, Refractory fever fever refractory to at least 3 d of appropriate antibiotic therapy, Recrudescent fever recrudescent fever after a period of defervescence of at least 48 h while still on antibiotics and without other apparent cause, Worsening respiratory insufficiency worsening respiratory insufficiency in spite of appropriate antibiotic therapy and ventilatory support
*p values are statistically significant
Antifungal Therapy
All but six probable IPA patients (139/145, 95.9%) received antifungal therapy. The vast majority of these ACLF patients (121/139, 87.1%) started antifungal therapy within 1 day of suspicion of IPA; i.e., there were no delays in antifungal treatment initiation in these patients.
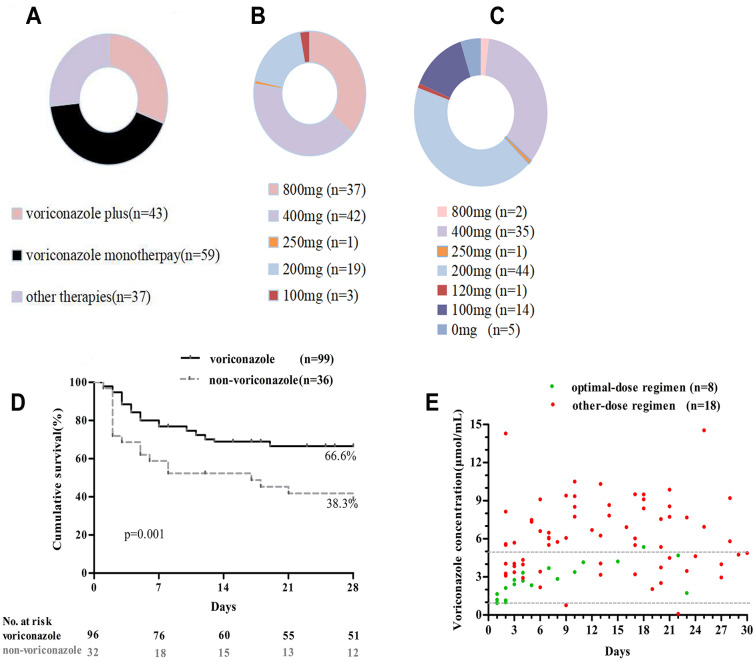
Therapeutic regimens consisting of voriconazole therapy were the most common (70.3%, n = 102; Fig. 3a). Among the voriconazole-based regimens, the loading dose of voriconazole ranged from 100 to 800 mg (Fig. 3b), and the maintenance dose ranged from 0 to 800 mg/day (Fig. 3c).
Fig. 3.
Antifungal therapy for IPA: a distribution of antifungal drugs prescribed in ACLF patients with probable IPA; b loading doses and c maintenance doses of voriconazole in ACLF patients; d cumulative 28-day mortality of patients treated with voriconazole therapy and non-voriconazole therapy (66.6% vs. 38.3%, p = 0.001). Log-rank test was performed; e trough voriconazole concentrations comparing patients treated with an optimal voriconazole regimen and those with other voriconazole regimens within 30 days
PSM was performed between IPA patients treated with voriconazole and those treated with other antifungal regimens. The clinical and laboratory data are shown in Supplementary Table 2. Patients treated with a voriconazole-based regimen had a lower 28-day mortality compared with those treated with a non-voriconazole antifungal regimen (66.6% vs. 38.3%, p = 0.001; Fig. 3d).
Based on the plasma voriconazole trough concentration measurement, we had established an optimal low-dose voriconazole regimen (loading dose, 0.2 g twice daily; maintenance dose, 0.1 g once daily) in pilot ACLF patients [14]. Plasma voriconazole concentration measurements were performed as therapeutic drug monitoring in 25.5% (26/102) of the patients from two centers. In eight patients, this low-dose regimen achieved a plasma voriconazole concentration of 1–5 μg/ml within 30 days. In the remaining 18 patients treated with other dosage regimens, the plasma voriconazole concentration exceeded 5 μg/ml as the treatment continued (Fig. 3e).
Discussion
This was a large and multicenter study to investigate short-term outcomes and antifungal options in ACLF patients with IPA. First, we described the detailed clinical features of IPA in ACLF patients and found that IPA increased the mortality risk attributed to respiratory failure in ACLF patients. Second, we demonstrated that a SOFA lung score > 1 was strongly associated with the short-term survival of ACLF patients with IPA. Finally, we suggested that an optimal voriconazole regimen achieved satisfactory antifungal responses and optimal drug concentrations ranging from 1 to 5 μg/ml.
Our previous investigation showed that probable IPA developed in approximately 5% of ACLF patients [14]. IPA was a fatal complication that dramatically increased mortality in ACLF patients and should not be missed. We demonstrated that the presence and severity of IPA-related respiratory dysfunction/failure at the time of IPA diagnosis is a major determinant of death in these patients. Respiratory failure was the dominant cause of death of ACLF patients with IPA.
Subsequently, we proved that SOFA lung score > 1 strongly predicted a worsened short-term outcome in ACLF patients with IPA, even if there was almost no delay of antifungal treatment after diagnosis. Patients with SOFA lung score ≤ 1 had good responses to antifungal treatments and low short-term mortality, which implied that patients may benefit from an early diagnosis and timely intervention prior to the development of impaired respiratory function. These findings suggest that prompt surveillance and early diagnosis of IPA in ACLF patients would be crucial to attenuate IPA-associated mortality. However, further studies are needed to determine the optimal surveillance strategy for invasive fungal diseases, including IPA in ACLF patients. Some promising strategies are sequential measurements of serum galactomannan antigen [22] or baseline chest computed tomography screening [23].
Treatment of IPA in patients with ACLF remains a challenge. Voriconazole is the first-line treatment for IPA, although it is associated with hepatotoxicity [10]. Caspofungin is used as rescue therapy, and it is well-tolerated in patients with hepatic dysfunction [10]. Other regimens for IPA including isavuconazole and l-AmB may be effective and tolerated in patients with ACLF, but were not well evaluated in the study. A recent study demonstrated the superiority of voriconazole as the first line of treatment for IA over caspofungin in patients with hematological malignancies [10]. In agreement with this finding, our preliminary analysis showed that a voriconazole-based regimen was better at improving survival in ACLF patients with IPA than a non-voriconazole-based regimen.
Voriconazole mainly carries out oxidative metabolism through the liver cytochrome P450 isoenzymes (including CYO2C19, CYP2C9, and CYP3A4). The pharmacokinetics of voriconazole vary greatly among individuals, and the influencing factors include age, liver function, drug interactions, and CYO2C19 gene polymorphism [24–26]. Notably, regarding the concern of hepatotoxicity, only a few patients were given the standard dose of voriconazole (loading dose 400 mg twice daily; maintenance dose 100 mg twice daily) [27], while the dosage in other patients was much lower than that recommended in patients without or with compensated liver diseases. However, we observed a similar treatment efficacy between patients who received the standard dosage and those who received a different dosage, possibly because of the delayed clearance of voriconazole in the context of ACLF.
The optimal blood concentration of voriconazole is between 1.0 and 5.0 µg/ml [27]. In our previous study [14], we suggested an optimal voriconazole regimen in ACLF patients using trough concentration monitoring methods. Our optimal voriconazole regimen could maintain stable and evidence-based therapeutic through concentrations between 1 and 5 µg/ml in our series of eight patients. The optimal voriconazole regimen is lower than the recommended dose for patients without liver disease or for Child–Pugh A/B/C cirrhosis [28–30], and the therapeutic effect was consistent with that in our previous study [14]. However, a large-sample, prospective study is warranted to validate the optimal voriconazole regimen for IPA in ACLF patients as the current investigation included a small number of patients for therapeutic drug monitoring.
The strength of this study lies in its relatively large cohort of ACLF patients with probable IPA derived from multiple centers and a matched cohort design. However, the retrospective study of IPA cases presents several limitations. First, there was the lack of systematic screening of IPA by chest computed tomography and galactomannan antigen detection in plasma, and the direct test for Aspergillus spp. in each patient may have underestimated the incidence of IPA in ACLF patients. The frequent use of broad-spectrum β-lactam antibiotics may be related to the false-positive detection of galactomannans. Second, given the presence of severe coagulopathy in ACLF patients, neither lung biopsy nor bronchoscopy with bronchoalveolar lavage were performed, which mitigates the evidence-based and hierarchical IPA diagnosis. Assessment of thromboelasticity may be a novel and feasible method to assess bleeding risk in ACLF patients. Finally, many hospitals had not carried out voriconazole concentration monitoring, so data on serum concentrations of voriconazole were not available for the majority of these patients.
Conclusion
ACLF patients with IPA have high mortality. The severity of respiratory dysfunction is a major determinant of the outcome, and the SOFA lung score can be used as a useful parameter to predict the prognosis of ACLF patients with IPA. Voriconazole can be used as the first choice of treatment for IPA, and the optimal voriconazole regimen was safe and effective in ACLF patients with IPA. Further prospective studies are warranted to optimize the surveillance strategy, improve the diagnosis of IPA under severe coagulopathy conditions, and validate the optimal voriconazole regimen in ACLF patients.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Funding
This work was supported by the National Science and Technology Major Project (2018ZX10723203, 2018ZX10302206), National Natural Science Foundation of China (82070650, 81270533, 81470038), National Key Research and Development Program of China (2017YFC0908100), Local Innovative and Research Teams Project of Guangdong Pearl River Talents Program(2017BT01S131), Key Scientific and Technological Program of Guangzhou City (201508020262), Department of Science and Technology of Guangdong Province (2014B020228003, 2015B020226004), Clinical Research Program of Nanfang Hospital, Southern Medical University (2018CR037), Clinical Research Startup Program of Southern Medical University by High-level University Construction Funding of Guangdong Provincial Department of Education(LC2019ZD006,LC2016PY005) and President Foundation of Nanfang Hospital, Southern Medical University(2019Z003). Prof. Yan Huang is supported by the National Science and Technology Major Project [2018ZX10722202] and National Key Research and Development Program of China [2017YFC0909104]. Dr. Jun Lv is supported by the National Science and Technology Major Project [2017ZX10302201-004-007] and National Natural Science Foundation of China [81902470]. Department of Science and Technology of Guangdong Province (2014B020228003) funded the journal’s Rapid Service Fee.
Medical Writing, Editorial, and Other Assistance
Editorial assistance for this manuscript was provided by Editage company and the source of funding for this assistance was Department of Science and Technology of Guangdong Province (2014B020228003).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Thanks to all authors for their contributions to this article. Jinjun Chen, Danli Chen, Yu Shi and Jinhua Hu conceived and designed the study. Danli Chen, Zhiping Qian, Haibin Su, Zhongji Meng, Jun Lv, Yan Huang, Yanhang Gao, Jingyuan Liu, Caiyan Zhao, Hongbo Gao, Yu Chen, Jie Xia, Liang Peng, Tao Han, Hai Li, Xin Zheng, Xianbo Wang, Xiaobo Lu and Yu Shi collected the data. Jinjun Chen, Danli Chen and Yu Shi contributed to data analysis and interpretation, and writing article; Jinjun Chen approved the study and this submission.
Disclosures
Danli Chen, Zhiping Qian, Haibin Su , Zhongji Meng, Jun Lv , Yan Huang, Yanhang Gao, Jingyuan Liu, Caiyan Zhao, Hongbo Gao, Yu Chen, Jie Xia, Liang Peng, Tao Han, Hai Li, Xin Zheng, Xianbo Wang, Xiaobo Lu , Yu Shi , Jinhua Hu and Jinjun Chen have nothing to disclose.
Compliance with Ethics Guidelines
The ethics committee of the Nanfang Hospital reviewed and approved this study. Written consent from patients or their authorized representatives was waived because of the retrospective nature of the study.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Danli Chen, Zhiping Qian and Haibin Su have contributed to this work equally.
Contributor Information
Xianbo Wang, Email: wangxianbo638@163.com.
Yu Shi, Email: zjushiyu@zju.edu.cn.
Jinhua Hu, Email: 139100020608@163.com.
Jinjun Chen, Email: chjj@smu.edu.cn.
References
- 1.Sarin SK, Kedarisetty CK, Abbas Z, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific Association for the Study of the Liver (APASL) 2014. Hepatol Int. 2014;8(4):453–471. doi: 10.1007/s12072-014-9580-2. [DOI] [PubMed] [Google Scholar]
- 2.Arroyo V, Moreau R, Kamath PS, et al. Acute-on-chronic liver failure in cirrhosis. Nat Rev Dis Prim. 2016;2:16041. doi: 10.1038/nrdp.2016.41. [DOI] [PubMed] [Google Scholar]
- 3.Albillos A, Lario M, Álvarez-Mon M. Cirrhosis-associated immune dysfunction: distinctive features and clinical relevance. J Hepatol. 2014;61(6):1385–1396. doi: 10.1016/j.jhep.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 4.Fernández J, Acevedo J, Wiest R, et al. Bacterial and fungal infections in acute-on-chronic liver failure: prevalence, characteristics and impact on prognosis. Gut. 2018;67(10):1870–1880. doi: 10.1136/gutjnl-2017-314240. [DOI] [PubMed] [Google Scholar]
- 5.Shi Y, Yang Y, Hu Y, et al. Acute-on-chronic liver failure precipitated by hepatic injury is distinct from that precipitated by extrahepatic insults. Hepatology. 2015;62(1):232–242. doi: 10.1002/hep.27795. [DOI] [PubMed] [Google Scholar]
- 6.Hu J, Zhao H, Lou D, et al. Human cytomegalovirus and Epstein-Barr virus infections, risk factors, and their influence on the liver function of patients with acute-on-chronic liver failure. BMC Infect Dis. 2018;18(1):577. doi: 10.1186/s12879-018-3488-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jalan R, Fernandez J, Wiest R, et al. Bacterial infections in cirrhosis: a position statement based on the EASL Special Conference 2013. J Hepatol. 2014;60(6):1310–1324. doi: 10.1016/j.jhep.2014.01.024. [DOI] [PubMed] [Google Scholar]
- 8.Blot SI, Taccone FS, Van den Abeele AM, et al. A clinical algorithm to diagnose invasive pulmonary aspergillosis in critically ill patients. Am J Respir Crit Care Med. 2012;186(1):56–64. doi: 10.1164/rccm.201111-1978OC. [DOI] [PubMed] [Google Scholar]
- 9.Husain S, Camargo JF. Invasive aspergillosis in solid-organ transplant recipients: guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33(9):e13544. doi: 10.1111/ctr.13544. [DOI] [PubMed] [Google Scholar]
- 10.De Pauw B, Walsh TJ, Donnelly JP, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46(12):1813–1821. doi: 10.1086/588660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arai M, Kanda T, Yasui S, et al. Opportunistic infection in patients with acute liver failure. Hepatol Int. 2014;8(2):233–239. doi: 10.1007/s12072-013-9514-4. [DOI] [PubMed] [Google Scholar]
- 12.Chen J, Yang Q, Huang J, Li L. Risk factors for invasive pulmonary aspergillosis and hospital mortality in acute-on-chronic liver failure patients: a retrospective-cohort study. Int J Med Sci. 2013;10(12):1625–1631. doi: 10.7150/ijms.6824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gustot T, Maillart E, Bocci M, et al. Invasive aspergillosis in patients with severe alcoholic hepatitis. J Hepatol. 2014;60(2):267–274. doi: 10.1016/j.jhep.2013.09.011. [DOI] [PubMed] [Google Scholar]
- 14.Gao J, Zhang Q, Wu Y, et al. Improving survival of acute-on-chronic liver failure patients complicated with invasive pulmonary aspergillosis. Sci Rep. 2018;8(1):876. doi: 10.1038/s41598-018-19320-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Verma N, Singh S, Taneja S, et al. Invasive fungal infections amongst patients with acute-on-chronic liver failure at high risk for fungal infections. Liver Int. 2019;39(3):503–513. doi: 10.1111/liv.13981. [DOI] [PubMed] [Google Scholar]
- 16.Miceli MH, Kauffman CA. Aspergillus galactomannan for diagnosing invasive aspergillosis. JAMA. 2017;318(12):1175–1176. doi: 10.1001/jama.2017.10661. [DOI] [PubMed] [Google Scholar]
- 17.Gu WY, Xu BY, Zheng X, et al. Acute-on-chronic liver failure in China: rationale for developing a patient registry and baseline characteristics. Am J Epidemiol. 2018;187(9):1829–1839. doi: 10.1093/aje/kwy083. [DOI] [PubMed] [Google Scholar]
- 18.Patterson TF, Thompson GR, 3rd, Denning DW, et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;63(4):e1–e60. doi: 10.1093/cid/ciw326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hou J, Wang G, Wang F, et al. Guideline of prevention and treatment for chronic hepatitis B (2015 update) J Clin Transl Hepatol. 2017;5(4):297–318. doi: 10.14218/JCTH.2016.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu YC, Mao YM, Chen CW, et al. CSH guidelines for the diagnosis and treatment of drug-induced liver injury. Hepatol Int. 2017;11(3):221–241. doi: 10.1007/s12072-017-9793-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moreau R, Jalan R, Gines P, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 2013;144(7):1426–1437.e14379. doi: 10.1053/j.gastro.2013.02.042. [DOI] [PubMed] [Google Scholar]
- 22.Nucci M, Nouér SA, Grazziutti M, Kumar NS, Barlogie B, Anaissie E. Probable invasive aspergillosis without prespecified radiologic findings: proposal for inclusion of a new category of aspergillosis and implications for studying novel therapies. Clin Infect Dis. 2010;51(11):1273–1280. doi: 10.1086/657065. [DOI] [PubMed] [Google Scholar]
- 23.Bitterman R, Hardak E, Raines M, et al. Baseline chest computed tomography for early diagnosis of invasive pulmonary aspergillosis in hemato-oncological patients: a prospective cohort study. Clin Infect Dis. 2019;69(10):1805–1808. doi: 10.1093/cid/ciz194. [DOI] [PubMed] [Google Scholar]
- 24.Wang T, Zhu H, Sun J, et al. Efficacy and safety of voriconazole and CYP2C19 polymorphism for optimised dosage regimens in patients with invasive fungal infections. Int J Antimicrob Agents. 2014;44(5):436–442. doi: 10.1016/j.ijantimicag.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 25.Seyedmousavi S, Mouton JW, Verweij PE, Brüggemann RJ. Therapeutic drug monitoring of voriconazole and posaconazole for invasive aspergillosis. Expert Rev Anti Infect Ther. 2013;11(9):931–941. doi: 10.1586/14787210.2013.826989. [DOI] [PubMed] [Google Scholar]
- 26.Li ZW, Peng FH, Yan M, et al. Impact of CYP2C19 genotype and liver function on voriconazole pharmacokinetics in renal transplant recipients. Ther Drug Monit. 2017;39(4):422–428. doi: 10.1097/FTD.0000000000000425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ashbee HR, Barnes RA, Johnson EM, Richardson MD, Gorton R, Hope WW. Therapeutic drug monitoring (TDM) of antifungal agents: guidelines from the British Society for Medical Mycology. J Antimicrob Chemother. 2014;69(5):1162–1176. doi: 10.1093/jac/dkt508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patterson TF, Thompson GR, 3rd, Denning DW, et al. Executive summary: practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;63(4):433–442. doi: 10.1093/cid/ciw444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dolton MJ, Ray JE, Chen SC, Ng K, Pont LG, McLachlan AJ. Multicenter study of voriconazole pharmacokinetics and therapeutic drug monitoring. Antimicrob Agents Chemother. 2012;56(9):4793–4799. doi: 10.1128/AAC.00626-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang T, Yan M, Tang D, et al. A retrospective, multicenter study of voriconazole trough concentrations and safety in patients with Child-Pugh class C cirrhosis. J Clin Pharm Ther. 2018;43(6):849–854. doi: 10.1111/jcpt.12724. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.