A year and a half after the onset of the coronavirus disease 2019 (COVID-19) pandemic, there are few published data about the long-term renal prognosis of infected critical patients admitted to intensive care units (ICUs) who develop acute kidney injury (AKI) requiring continuous renal replacement therapies (CRRTs) [1, 2]. We performed a retrospective observational study in which we analysed the renal long-term clinical course and outcomes of 53 critical patients infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) who developed acute respiratory failure and AKI requiring CRRT.
Baseline characteristics are shown in Table 1. Regarding long-term renal function, the surviving patients did not receive any additional dialysis; however, at discharge, the decrease in estimated glomerular filtration rate (eGFR) was 31.7 ± 21.8 and 29.8 ± 18.4 mL/min/1.73 m2 at 6 months and 1 year, respectively (P < 0.001) (Figure 1). At admission, 22 patients had albuminuria and 29 had microhaematuria. After 6 months, only 2 patients of 14 survivors maintained these alterations.
Table 1.
Clinical and demographic characteristics of 53 critically ill COVID-19 patients who developed AKI requiring CRRT
| Clinical and demographic characteristics | Values |
|---|---|
| Sex (male/female), n/n | 42/11 |
| Age (years), median (IQR) | 63 (31–78) |
| Baseline serum creatinine (mg/dL), mean ± SD | 1.23 ± 0.93 |
| Baseline eGFR (mL/min/1.73 m2), mean ± SD | 73.1 ± 26.7 |
| Diabetes, n (%) | 12 (23) |
| Hypertension, n (%) | 40 (75) |
| Obesity, n (%) | 20 (38) |
| CRRT prescription, % |
|
| Time on CRRT (days), median (IQR) | 18 (1–176) |
| Mortality, n (%) | 39 (73.5) |
CVVHD, continuous venovenous haemodialysis; CVVH, continuous veno-venous haemofiltration; IQR, interquartile range; SD, standard deviation.
FIGURE 1:
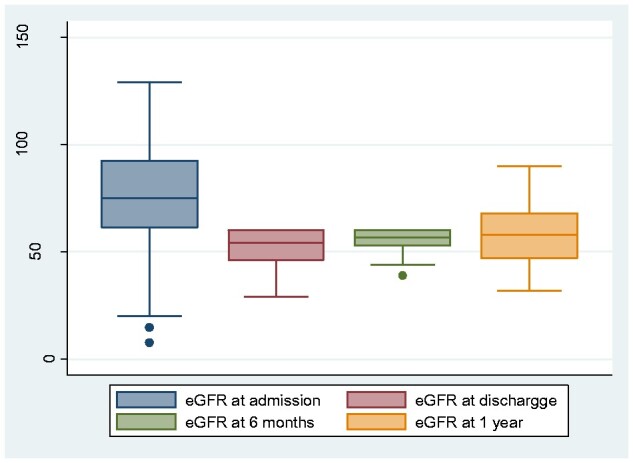
eGFR (ml/min/1.73 m2) 6 months and 1 year after SARS-CoV-2 infection (n = 14 survivors)
Ng et al. [3] recently published the outcomes among patients hospitalized with COVID-19 and AKI. Among those with AKI Stage 3 who survived, 30.6% remained on dialysis at discharge, and pre-hospitalization chronic kidney disease (CKD) was the only independent risk factor associated with needing dialysis at discharge. It is unclear how many of these patients may subsequently experience recovery of kidney function, although it should be noted that more than half of them had pre-existing advanced CKD. In contrast, in our data series, only patients with previous normal baseline kidney function were included in the analysis. A meta-analysis [4] showed a high prevalence of abnormal urinalysis and kidney dysfunction in COVID-19 patients (3.7%). Fifty-seven percent of patients during hospitalization present proteinuria, but no data about long-term renal outcomes have been described in these patients. The long-term health consequences of patients with COVID-19 who have been discharged from hospital have been recently published in a Chinese cohort [5]. Thirteen percent of the patients without AKI and with normal eGFR at the acute phase had decreased eGFR at the 6-month follow-up. Therefore the decrease of kidney function is important after COVID-19 infection even in patients who do not develop AKI.
Our results offer important messages: survivor patients who develop AKI requiring CRRT in the ICU do not require long-term dialysis if they have normal baseline renal function; 1 year after discharge, no patients have recovered their renal function and have lost half of kidney function after SARS-CoV-2 infection; by 1 year, most of the urinary sediment alterations have disappeared and, lastly, these results support that these patients require post-discharge nephrologist care.
ACKNOWLEDGEMENTS
This research was conducted in accordance with the World Medical Association Declaration of Helsinki. Ethical approval was waived by the local Ethics Committee of Hospital General Universitario Gregorio Marañón.
FUNDING
This study was funded by Red de Investigación Renal, ISCIII RETIC REDINREN RD016/009 (FEDER funds).
AUTHORS’ CONTRIBUTIONS
R.M., A.M. and M.G. conceived and designed the study, had full access to data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. R.M. and M.G. acquired, analysed or interpreted the data. All of the authors revised and drafted the manuscript.
CONFLICT OF INTEREST STATEMENT
P.R.B. has received fees for conference from Baxter. The other authors declare no conflicts of interest.
Contributor Information
Rosa Melero, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Antonia Mijaylova, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Patrocinio Rodriguez-Benitez, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Nicolas Macías, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Ines Aragoncillo, Instituto de Investigación Sanitaria Gregorio Marañón, Madrid, Spain; Red de Investigación Renal, ISCIII RETIC REDINREN RD016/009 (FEDER funds), Madrid, Spain.
Maria Luisa Rodriguez-Ferrero, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Ana Garcia-Prieto, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Arturo Bascuñana, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Adriana Acosta, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Angela Gonzalez-Rojas, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Alejandra Muñoz de Morales, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Javier Carbayo, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Luis Sanchez-Cámara, Instituto de Investigación Sanitaria Gregorio Marañón, Madrid, Spain.
Ursula Verdalles, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Soraya Abad, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Almudena Vega, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Eduardo Verde, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
David Arroyo, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Ana Perez de Jose, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Patricia Piñero, Servicio de Anestesiología y Reanimación, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Jamil Cedeño, Servicio de Medicina Intensiva, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Fernando Anaya, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Manuel Antonio Rengel, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Daniel Barraca, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
María Olmedo, Servicio de Microbiología y Enfermedades Infecciosas, Hospital General Universitario Gregorio Marañón, Madrid, Spain.
Marian Goicoechea, Servicio de Nefrología, Hospital General Universitario Gregorio Marañón, Madrid, Spain; Red de Investigación Renal, ISCIII RETIC REDINREN RD016/009 (FEDER funds), Madrid, Spain.
REFERENCES
- 1. Cummings MJ, Baldwin MR, Abrams Det al. Epidemiology, clinical course and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet 2020; 395: 1763–1770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gabarre P, Dumas G, Dupont Tet al. Acute kidney injury in critically ill patients with COVID-19. Intensive Care Med 2020; 46: 1339–1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ng J, Hirsch JS, Hazzan Aet al. Outcomes among patients hospitalized with COVID-19 and acute kidney injury. Am J Kidney Dis 2021; 77: 204–215.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yang X, Jin Y, Li Ret al. Prevalence, and impact of acute renal impairment on COVID-19: a systematic review and meta-analysis. Crit Care 2020; 18: 356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Huang C, Huang L, Wang Yet al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 2021; 397: 220–232 [DOI] [PMC free article] [PubMed] [Google Scholar]


