Abstract
Introduction
Smoking is associated with the occurrence and progression of cardiovascular diseases, inflammatory disorders and malignancies.
Objective
To study the platelet indices, neutrophil lymphocyte ratio (NLR) and platelet lymphocyte ratio (PLR) in smokers and their correlation with smoking pack-years.
Method
A total of 110 smokers and 110 non-smokers were included. The smokers were grouped into three groups: mild (<5 pack-years), moderate (5−10 pack-years) and heavy (>10 pack-years). The platelet count, plateletcrit (PCT), mean platelet volume (MPV) and platelet distribution width (PDW) were noted. The NLR and PLR were calculated and the statistical analysis was made using the Student’s T-test, Analysis of Variance (ANOVA) and Spearman’s correlation coefficient.
Results
The platelet count, PCT and PDW were significantly higher with mean values: 218.56 ± 121.31 vs 203.23 ± 80.35 (p-value = 0.038), 0.27 ± 0.10 vs 0.26 ± 0.10 (p-value = 0.041) and 12.54 ± 1.45 vs 11.99 ± 1.70 (p-value = 0.001) in smokers and non-smokers, respectively. The PLR differed significantly with mean values: 119.40 ± 84.81 in smokers and 181.99 ± 313.09 in non-smokers, with a p-value of 0.045. A significant positive correlation was found between pack-years of smoking and platelet count and PLR with the Pearson correlation coefficient of 0.250 and 0.198 and p-values, 0.008 and 0.037, respectively. The Platelet Count, PCT, MPV and PDW varied significantly between mild, moderate and heavy smoker groups, with p-values of 0.045, 0.010, 0.015 and 0.017, respectively.
Conclusion
The platelet indices and inflammatory markers NLR and PLR are derived from routine blood investigations, which are easily available and inexpensive. The monitoring of platelet indices, along with the PLR, can be used as early predictors of morbidity in smokers.
Keywords: NLR, PLR, Mean platelet volume, Platelet distribution width, Plateletcrit
Introduction
Smoking is considered a major risk factor for cardiovascular diseases, hypertension, inflammation, stroke, coagulopathy and respiratory diseases.1 Recently, the role of cigarette smoking in abnormalities in platelet activation and aggregation, along with other coagulation processing disruptions resulting in thrombotic formations, has been suggested.2 In smokers, the endothelial lining is damaged, which causes platelets to adhere to the subendothelial collagen and therefore, the number of platelets in circulation might vary. There have been conflicting results in previous studies on the effect of smoking on platelet counts.3 The platelet indices, such as the platelet distribution width (PDW), mean platelet volume (MPV) and plateletcrit (PCT), are the other biomarkers which can be altered in infections and respiratory and cardiovascular pathologies.4 The increased platelet activity, thrombus formation and thromboembolic diseases are among the major health hazards in developing countries. The MPV and PDW are indicators of platelet activation and are readily available in a routine hematology analyzer.5 The plateletcrit (PCT) may or may not be low in smokers. A low PCT value indicates platelet abnormality caused by the absence of a bone marrow response to the peripheral demand for platelets.6 The neutrophil lymphocyte ratio (NLR) and platelet lymphocyte ratio (PLR) are calculated from the complete blood count and are inexpensive and readily available. The combination of the NLR and PLR can be used as inflammation markers and can be considered as prognostic markers of systemic diseases.7 The NLR is used in the diagnosis and determination of cardiovascular diseases, pulmonary diseases, infections, endocrinological disorders and prognostic indicator in some malignancies.4 The PLR indicates increased platelet activation and has been observed as being associated with the onset and progression of atherosclerosis.1
There have been only a handful of studies on the effect of smoking on the platelet indices, PLR and NLR. The effect of smoking on platelets was studied by Anandalakshmi et al. in a trial which included only 50 subjects and 50 controls and found significantly increased MPV and PDW in smokers.5 Ghahremanfard et al. also compared the platelet indices between smokers and non-smokers.8 Similarly, according to Tulgar et al., the PDW was increased in smokers and there was also a positive correlation of PDW and NLR with packs/year.4 An increase in NLR and a decrease in PLR in smokers was found by Gumus et al.1
Therefore, in this study we aimed to compare the platelet indices, PLR and NLR among the smokers and non-smoker groups and also analyze if there could be a significant correlation of the above-mentioned parameters with the pack-years of smoking.
Method
The study was conducted in a tertiary care hospital in the department of Pathology within a period of two months (July 2019–August 2019). The patients were selected from those attending the outpatient department for routine checkup and referred to the laboratory for routine blood investigations. There was a total of 220 cases, 110 smokers and 110 non-smoker controls. The smokers were divided into three groups: mild (<5 pack-years), moderate smokers (5−10 pack-years) and heavy smokers (>10 pack-years).
Individuals with associated comorbid illnesses, such as diabetes mellitus, hypothyroidism, hyperthyroidism, renal failure, malignancy, pregnancy, upper respiratory tract infection, pulmonary hypertension, chronic liver disease, hematological disorder, leukocytosis, leukopenia, anemia and family history of lipid disorders or those taking steroids or anticoagulants, such as aspirin, were excluded from the study.
Under aseptic conditions, a 3 mL venous sample was collected in an EDTA vial. The platelet indices of all the individuals included in the study were noted and the PLR and NLR were calculated using the complete blood count. A comparison was made among the smokers and non-smokers and the correlation of pack-years of smoking with the above-mentioned parameters was studied.
Statistical analysis
The variables were tested for normality using the Kolmogorov–Smirnov Test and represented a normal distribution. The comparison between cases and controls was done using the T-test. The one-way ANOVA test was used for the intergroup comparison between the mild, moderate and heavy smoker groups. The Pearson correlation test was used to analyze the correlation of pack-years of smoking with the parameters. A p-value <.05 was considered significant.
A written informed consent was obtained from each patient.
Observation and result
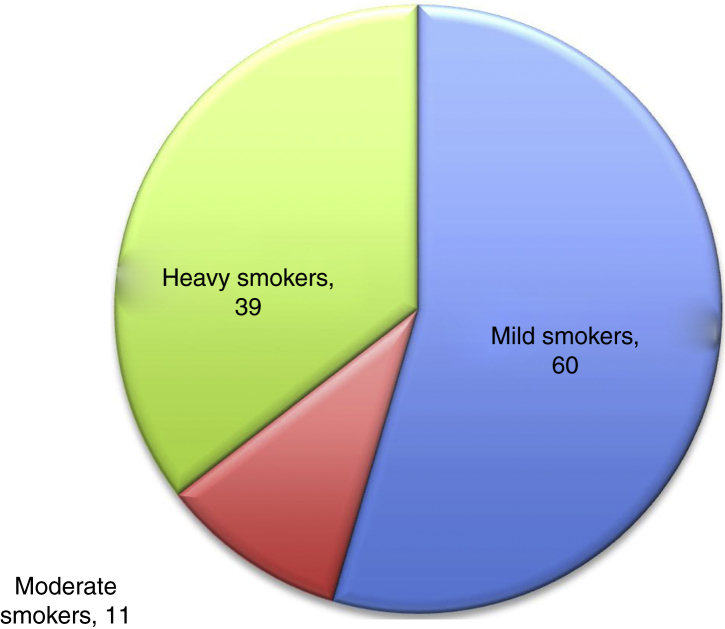
The average age of the 110 subjects was 47.42 ± 13.45 and 110 controls was 49.21 ± 15.29. There were 101 Males and 9 females in the smoker group (Table 1; Figure 1).
Table 1.
Subjects included.
| Smokers (n = 110) | Non-smokers (n = 110) | p-Value | |
|---|---|---|---|
| Age | 47.42 ± 13.45 | 49.21 ± 15.29 | 0.357 |
| Gender | 0.808 | ||
| Males | 101 | 97 | |
| Females | 9 | 13 |
Figure 1.
Smokers by group.
The platelet count was significantly elevated in the smokers, with a mean value of 18.56 ± 121.31 in smokers and 203.23 ± 80.35 in non-smokers and a p-value of 0.038 (Table 2). The platelet count in this study was mildly reduced in the moderate smokers, with a mean value 188.58 ± 73.79, compared to 205.82 ± 74.94 in mild smokers; however, the heavy smoker group had a much higher platelet count, with a mean of 264.41 ± 190.78 and thus, the platelet count was found to differ significantly among the smoker groups (p = 0.045) (Table 3).
Table 2.
Comparison of parameters between smokers and non-smokers.
| Parameter | Smokers (n = 110) | Non-smokers (n = 110) | p-Value |
|---|---|---|---|
| Platelet count (103/uL) | 218.56 ± 121.31 | 203.23 ± 80.35 | 0.038* |
| MPV (fL) | 17.79 ± 4.20 | 16.48 ± 4.33 | 0.367 |
| PCT (%) | 0.27 ± 0.10 | 0.26 ± 0.10 | 0.041* |
| PDW (fL) | 12.54 ± 1.45 | 11.99 ± 1.70 | 0.001* |
| (NLR) (%) | 2.61 ± 1.99 | 2.48 ± 2.30 | 0.526 |
| (PLR)(%) | 119.40 ± 84.81 | 181.99 ± 313.09 | 0.045* |
p-Values; student t-test, statistically significant (*p < .05).
MPV: mean platelet volume; PCT: plateletcrit; PDW: platelet distribution width; NLR: neutrophil lymphocyte ratio; PLR: platelet lymphocyte ratio.
Table 3.
Comparison of parameters between smoker groups.
| Parameter | Mild smokers (<5 pack-years) | Moderate smokers (5−10 pack-years) | Heavy smokers (>10 pack-years) | p-Value |
|---|---|---|---|---|
| N = 60 | N = 11 | N = 39 | ||
| Platelet count (103/uL) | 205.82 ± 74.94 | 188.58 ± 73.79 | 264.41 ± 190.78 | 0.045* |
| PCT (%) | 0.27 ± 0.06 | 0.23 ± 0.10 | 0.33 ± 0.16 | 0.010* |
| MPV (fL) | 10.85 ± 1.73 | 12.08 ± 1.51 | 12.42 ± 1.55 | 0.017* |
| PDW (fL) | 14.09 ± 4.12 | 16.11 ± 3.79 | 17.49 ± 4.21 | 0.015* |
| NLR (%) | 2.47 ± 2.14 | 3.54 ± 4.13 | 2.78 ± 1.37 | 0.226 |
| PLR (%) | 108.69 ± 54.54 | 105.10 ± 83.49 | 139.39 ± 114.32 | 0.19 |
p Values; one-way ANOVA, statistically significant (*p < .05).
MPV: mean platelet volume; PCT: plateletcrit; PDW: platelet distribution width; NLR: neutrophil lymphocyte ratio; PLR: platelet lymphocyte ratio.
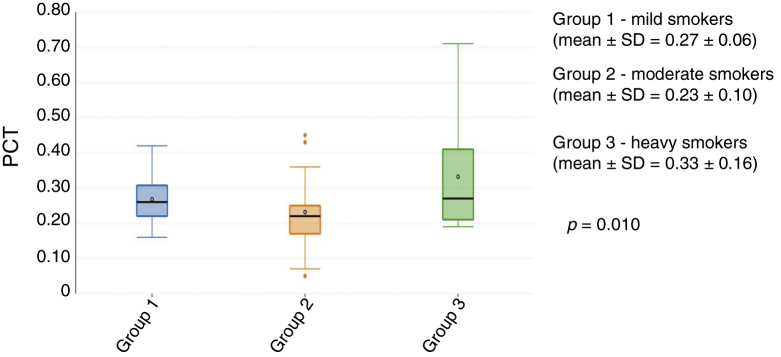
The plateletcrit was also found to be significantly elevated in the smokers, having mean values of 0.27 ± 0.10 in smokers and 0.26 ± 0.10 in non-smokers, with a p-value <0.05. (Table 2). The PCT among the smoker groups showed similar findings as to the platelet count. The Mean ± SD value of the PCT in mild smokers was 0.27 ± 0.06, 0.23 ± 0.10 in moderate smokers and 0.33 ± 0.16 in heavy smokers, with p = 0.041, which was statistically significant (Table 3, Figure 2).
Figure 2.
Graphical representation of PCT % in mild, moderate and heavy smokers.
(PCT: plateletcrit).
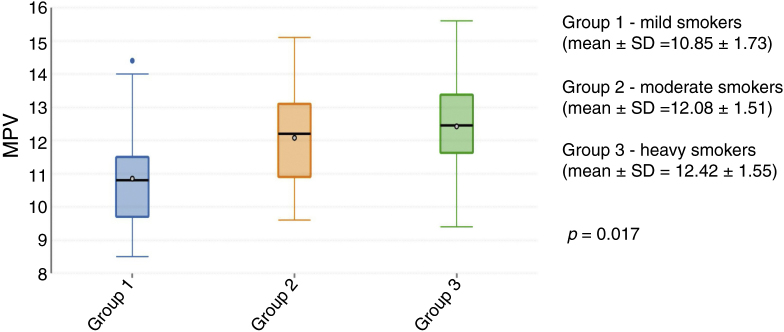
The MPV values did not show a significant difference in smokers vs non-smokers; however, the MPV increased significantly from 10.85 ± 1.73 in mild smokers to 12.08 ± 1.51 in moderate smokers and 12.42 ± 1.55 in heavy smokers. (p = 0.017) (Table 3, Figure 3).
Figure 3.
Graphical representation of MPV (fL) in mild, moderate and heavy smokers.
(MPV: mean platelet volume).
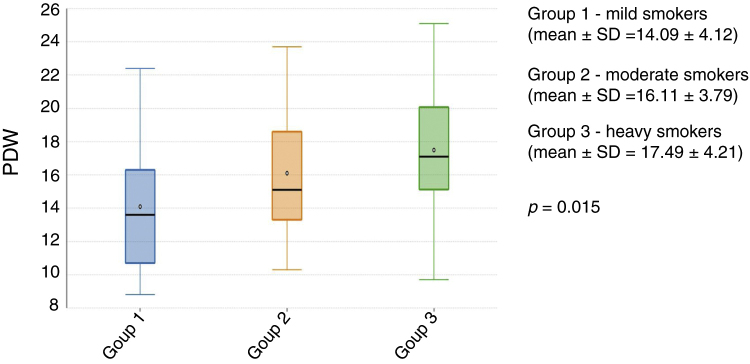
A significant difference in PDW values was found between smokers (12.54 ± 1.45) and non-smokers (11.99 ± 1.70), with a p-value of 0.001 (Table 2), and the PDW also differed significantly in mild smokers (14.09 ± 4.12), moderate smokers (16.11 ± 3.79) and in heavy smokers (17.49 ± 4.21), with the p-value of 0.015 (Table 3, Figure 4).
Figure 4.
Graphical representation of PDW (fL) in mild, moderate and heavy smokers.
(PDW: platelet distribution width).
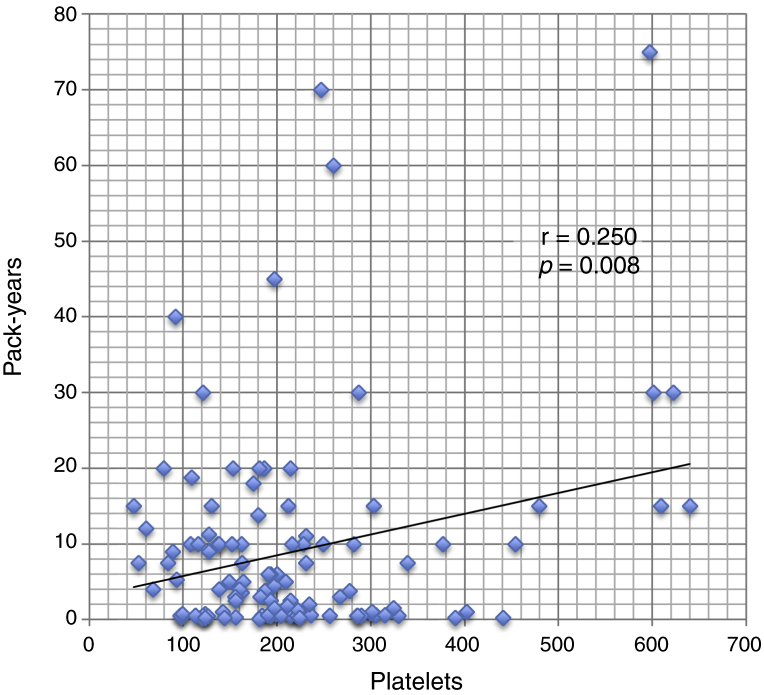
A positive correlation of the platelet count with increasing pack-years, with a correlation coefficient ‘r’ of 0.250 and a p-value of 0.008 (Table 4, Figure 5), was found. However, no statistically significant correlation of smoking pack-years was found with other platelet parameters.
Table 4.
Correlation of parameters with pack-years of smoking.
| Parameter | Correlation coefficient ‘r’ | p-Value |
|---|---|---|
| Platelet count (103/uL) | 0.250* | 0.008* |
| PCT (%) | 0.015 | 0.891 |
| MPV (fL) | 0.050 | 0.643 |
| PDW (fL) | 0.074 | 0.500 |
| Neutrophil lymphocyte ratio (NLR) (%) | 0.064 | 0.179 |
| Platelet lymphocyte ratio (PLR) (%) | 0.198 | 0.037* |
p-Values; Spearman’s correlation coefficient, statistically significant (*p < .05).
MPV: mean platelet volume; PCT: plateletcrit; PDW: platelet distribution width; NLR: neutrophil lymphocyte ratio; PLR: platelet lymphocyte ratio.
Figure 5.
Correlation between pack-years of smoking and platelet count.
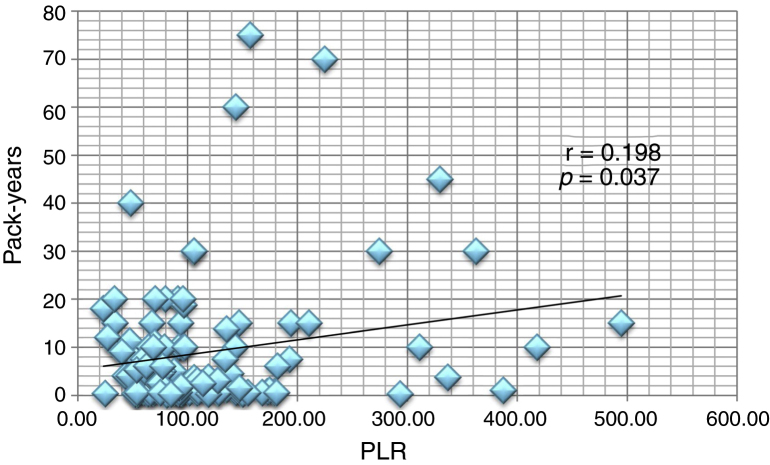
There was no significant difference in the NLR among the smokers and non-smokers; the PLR, on the other hand, showed a significant difference with lower values in the smoker group (119.40 ± 84.81 vs 181.99 ± 313.09; p-value = 0.045) (Table 2). The PLR values did not differ significantly among the three smoker groups, but there was a positive significant linear correlation of pack-years of smoking, with the PLR detected with the correlation coefficient r = 0.198 and p-value = 0.037, which was statistically significant (Table 4, Figure 6).
Figure 6.
Correlation between pack-years and platelet lymphocyte ratio (PLR).
Discussion
Smoking induces oxidative stress leading to increased platelet activation and aggregation and endothelium injury caused by nicotine.9 The role of cigarette smoking in the disruption of platelet activation, aggregation and coagulation leading to thrombosis has been suggested.5
The 3 groups of biomarkers may be involved in arterial thrombosis due to cigarette smoking, namely biomarkers for inflammation, biomarkers for oxidative stress and biomarkers for platelet activation. The first group of biomarkers, the highly sensitive-C reactive protein, fibrinogen and Von Willebrand factor levels have been found to be increased in smokers. Smokers also had increased prostaglandin F (PGF) 2alpha formation, enhanced COX-mediated inflammation and elevated cytokines and isoprostanes.8
There have been conflicting results in the previous studies on the effect of smoking on platelet counts. Some studies indicate that the platelet count increased with smoking,3 while some studies claim that the platelet count decreases in chronic smokers and that an increase in the duration of smoking was associated with a significant reduction in the platelet counts.9 It has been demonstrated that the levels of thrombopoietin were increased in smokers, when compared with nonsmokers, thereby inducing the production of platelets, leading to increased platelet counts.10 The increase in the mean platelet count in smokers, also reported by Ghahremanfard et al., is consistent with our findings.8 Tulgar et al.4 found no significant difference in the platelet count and PCT between smokers and non-smokers. Another study reported a significant increase in the platelet count and decreased PCT in the male smokers.8 In our study, an increased platelet count, along with an increased PCT and a significant correlation between the platelet count and pack-years, was found in the platelet count, with the coefficient ‘r’ of 0.250 and p-value of 0.008. The correlation of these indices with pack-years was significant, but weak. In addition, the platelet count and PCT varied significantly between the three smoker groups, with a p-value <.05, the highest values being among the heavy smoker groups, though the values corresponding to the moderate smoker group (5−10 pack-years) were slightly lower than those of the mild smokers (<5 pack years).
The MPV can be used as a marker of platelet activation and the platelet size correlates with the activity of the platelets, the larger ones being more active.1 In our study, though we did not find a significant difference between the smokers and non-smokers, but a significant difference with the increasing values of MPV in the mild, moderate and heavy smoker groups was found. Gumus et al.1 and Anandalakshmi et al.5 reported significantly higher MPV values in the smokers. Anandalakshmi et al. also reported increasing values of MPV among mild (10–14 pack-years), moderate (15–19 pack-years) and heavy (>20 pack-years), with a significant difference among the three groups.5 Tulgar et al.4 and Butkiewicz et al.12 reported no significant impact of smoking on the MPV. Cho et al. reported that the patients who stopped smoking had lower MPV levels.11 Another study reported higher MPV levels in smokers and these were significantly lower after 3 months of smoking cessation.12
The PDW is another marker of platelet activation which corresponds to the variation in size of the platelets.1 Anandhalakshmi et al. reported that the PDW was significantly increased in the smoker group and also increased significantly with the intensity of smoking,5 which is consistent with our findings. Similarly, Tulgar et al. also reported increased PDW values in smokers, in addition to a significant positive correlation with pack-years, which differed from our study, in which we could establish no such correlation.4
The NLR and PLR have been used as an indicator of inflammation and have been associated with diabetes mellitus, chronic obstructive pulmonary disease (COPD), malignancies and systemic inflammatory response in rheumatic disease. They can be derived from routine blood investigations without any additional cost.1 We found that the NLR, though increased in the smokers, did not show a significant difference between smokers and non-smokers. The PLR, on the other hand, was significantly elevated in the smokers and also a significant positive, though weak, correlation was also seen with increasing pack-years of smoking, with a p-value <.05. Gumus et al. reported an increase in the NLR and a decrease in PLR in the smoker group.1 Tulgar et al. reported a positive correlation of the NLR with increasing pack years, however, no significant differences in the PLR values were reported in smokers vs non-smokers, nor was there any significant correlation of pack-years of smoking with the PLR values observed by them.4 No significant difference in the NLR and PLR values among the mild, moderate and heavy smoker groups was found in our study, consistent with the Gumus et al. study, in which the three smoker groups were also divided on the basis of the number of cigarettes smoked per day (1–10/day, 11–20/day and >20/day).1
There is a paucity of literature on the effect of smoking on the platelet indices and the systemic inflammatory markers NLR and PLR, which are inexpensive to measure, easily available and can be used for predicting the risk of thromboembolic disorders in the smokers.
Limitations
The limitations in our study were the relatively small sample size and the fact that most of the subjects included in our study were males (M – 97, F – 13). The studies have suggested that physical inactivity may contribute to a proinflammatory burden and thus, may affect the inflammatory biomarkers.13 In addition, the exposure to environmental pollution may also effect these biomarkers.13 In the present study, the participants were not asked about the physical inactivity, nor was the environmental pollution taken into account.
Conclusion
The platelet count, PCT and PDW were increased significantly in smokers, in addition to a positive correlation of platelet count and PLR with pack-years. The platelet count, PCT, PDW and MPV also differed significantly among the mild (<5 pack-years), moderate (5−10 pack-years) and heavy (>10 pack-years) smokers. No significant difference in the NLR was noted between smokers and non-smokers. The platelet indices and PLR, which are derived from routine blood investigations and are thus cost effective, can be used for predicting the risk of morbidities like cardiovascular events and thromboembolism in smokers.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Gumus F., Solak I., Eryilmaz M.A. The effects of smoking on neutrophil/lymphocyte, platelet/ /lymphocyte ratios. Bratisl Med J. 2018;119(2):116–119. doi: 10.4149/BLL_2018_023. [DOI] [PubMed] [Google Scholar]
- 2.Ghahremanfard F., Semnani V., Ghorbani R., Malek F., Behzadfar A., Zahmatkesh M. Effects of cigarette smoking on morphological features of platelets in healthy men. Saudi Med J. 2015;36(7):847–850. doi: 10.15537/smj.2015.7.11026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Misra J., Venkatesh K. Comparison of platelet count in smokers versus non-smokers. J Evid Based Med Healthc. 2018;5(19):1522–1528. [Google Scholar]
- 4.Tulgar Y.K., Cakar S., Tulgar S., Dalkilic O., Cakiroglu B., Uyanik B.S. The effect of smoking on neutrophil/lymphocyte and platelet/lymphocyte ratio and platelet ındices: a retrospective study. Eur Rev Med Pharmacol Sci. 2016;20(14):3112–3118. [PubMed] [Google Scholar]
- 5.Swaminathan Anandhalakshmi, Amitkumar Kalaivani, Ganapathy Shivasekar, Ayyavoo Saravanan. Evaluation of the impact of cigarette smoking on platelet parameters. Natl J Physiol Pharm Pharmacol. 2015;5(5):426–430. [Google Scholar]
- 6.Asif M., Karim S., Umar Z., Malik A., Ismail T., Chaudhary A. Effect of cigarette smoking based on hematological parameters: comparison between male smokers and non-smokers. Turk J Biochem. 2013;38(1):75–80. [Google Scholar]
- 7.Acharya A.B., Shetty I.P., Jain S., Padakannaya I., Acharya S., Shettar L. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in chronic periodontitis before and after nonsurgical therapy. J Indian Soc Periodontol. 2019;23:419–423. doi: 10.4103/jisp.jisp_622_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ghahremanfard F., Semnani V., Ghorbani R., Malek F., Behzadfar A., Zahmatkesh M. Effects of cigarette smoking on morphological features of platelets in healthy men. Saudi Med J. 2015;36(7):847–850. doi: 10.15537/smj.2015.7.11026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sandhya M., Satyanarayana U., Mohanty S., Basalingappa D.R. Impact of chronic cigarette smoking on platelet aggregation and coagulation profile in apparently healthy male smokers. Int J Clin Exp Physiol. 2015;2(2):128–133. [Google Scholar]
- 10.Lupia E., Bosco O., Montrucchio G. Thrombopoietin contributes to enhanced platelet activation in cigarette smokers. Atherosclerosis. 2010:314–319. doi: 10.1016/j.atherosclerosis.2009.11.019. [DOI] [PubMed] [Google Scholar]
- 11.Cho SY, You E., Lee H.J., Lee W.I., Park T.S. Smoking cession decreases mean platelet volume in healthy Korean populations. Clin Lab. 2014;60:1413–1416. doi: 10.7754/clin.lab.2013.130901. [DOI] [PubMed] [Google Scholar]
- 12.Butkiewicz A.M., Kemona-Chetnik I., Dymicka-Piekarska V., Matowicka- Karna J., Kemona H. Does smoking affect thrombocytopoiesis and platelet activation in women and men? Adv Med Sci. 2006;51:123–126. [PubMed] [Google Scholar]
- 13.Çekici Y., Yılmaz M., Seçen Ö. New inflammatory indicators: association of high eosinophil-to-lymphocyte ratio and low lymphocyte-to-monocyte ratio with smoking. J Int Med Res. 2019;47(9):4292–4303. doi: 10.1177/0300060519862077. [DOI] [PMC free article] [PubMed] [Google Scholar]