Summary
Background
We aimed to determine whether heart, stroke, and vascular disease (HSVD) prevalence and emergency primary evacuation (EPE), hospitalisation, and mortality differ by patient characteristics.
Methods
An Australian-wide incidence population based study, with prospective data collected form the 1 July 2019 to the 30 October 2020.
Findings
Indigenous Australians reported significantly higher prevalence of HSVD at 229.0 per-1000 as compared to 152.0 per-1000 non-Indigenous Australians: risk ratio 1.5 (95% CI 1.2-1.8). 583 remote patients received an EPE for HSVD, consisting of 388 (66.6%; 95% CI: 62.6-70.4) males and 195 (33.0%; 95% CI: 29.6-37.4) females. There were 289 (49.6%; 95% CI 45.4- 53.7) patients who identified as Indigenous, and 294 (50.4%; 95% CI 46.3- 54.6) as non-Indigenous. The mean Indigenous age during EPE was 48.0 (95% CI 45.9-50.1) years old, significantly lower than the non-Indigenous mean age of 55.6 (95% CI 53.8-57.4). Indigenous patients hospitalised for HSVD were younger, the majority younger than 65 years (n=21175; 73.7% 95% CI 73.2-74.2) as compared to non-Indigenous patients (n= 357654; 33.1% 95% CI 33.0-33.15). When adjusted for HSVD prevalence, remote Indigenous patients had a higher hospitalisation rate as compared to non-remote Indigenous patients (rate ratio: 1.6; 95% CI 1.3-2.0) and remote non-Indigenous patients (rate ratio: 1.2; 95% CI 1.0-1.5). More Indigenous patients died of HSVD before the age of 65 years (n=1875; 56.5% 95% CI 54.8-58.2) as compared to non-Indigenous patients (n= 16161; 10.6% 95% CI 10.45-10.8).
Interpretation
Indigenous Australians have a higher prevalence, and younger age during EPE, and hospitalisation for HSVD than non-Indigenous Australians.
Funding
This is a self/internally-funded study, with the lead organisation being the Royal Flying Doctor Service (RFDS) of Australia. For the duration of the study period, the RFDS provided in-kind support including one full-time equivalent (FTE) and resources (office space, computer, research software, and office equipment). There was no external funding source that had a role in study design or data analysis or interpretation.
Research in context.
Evidence before this study
While there has been research on heart, stroke, and vascular disease (HSVD) prevalence rates and associated disease risk factors such as diabetes mellitus, hypertension, and renal disease, it is unclear how disease prevalence impacts aeromedical retrieval, hospitalisation, and mortality.
Added value of this study
This incidence population based study found that hospitalisation for HSVD, even adjusted for HSVD prevalence, is highest amongst Australians who identify as both remote and Indigenous, with this group having higher rates of aeromedical retrieval and hospitalisation, coupled with a younger mortality age.
Implications of all the available evidence
Remote Indigenous Australians have a high hospitalisation rate for HSVD than either non-remote Indigenous Australian or non-Indigenous Australians. This is coupled with significantly worse outcomes. Equity interventions to improve HSVD outcomes may need to be different for remote compared to non-remote Indigenous Australians.
Alt-text: Unlabelled box
Introduction
Heart, stroke, and vascular disease (HSVD) is a leading cause of mortality and morbidity worldwide.1 Internationally Indigenous Peoples, all have higher prevalence of HSVD,2, 3, 4 with the Australian Aboriginal and Torres Strait Islander people, hereafter referred to as Indigenous Australians, having significantly higher rates of chronic disease compared to non-Indigenous Australians, coupled with disproportionate levels of social isolation, poverty, unemployment, lack of education, and inadequate access to health care.5,6 Together, these contribute to a significant, and unacceptable, gap in life expectancy between Indigenous and non-Indigenous Australians.7
In the year 2016, Indigenous Australians experienced a burden of disease that was 2.3 times the rate of non-Indigenous Australians.8 There were 284 years lost due to premature death per-1,000 Indigenous people in Australia, which was equivalent to 190,227 Disability Adjusted Life Years (DALYs).8 Chronic disease is the leading cause (64.0%) of total disease burden for Indigenous Australians,8 with ischaemic heart disease being their leading cause of death.9
Australian remote areas have the highest proportion of Indigenous people.10 These remote areas are often characterised as having low healthcare provision1,2,11 including low levels of culturally appropriate healthcare,13 with many Indigenous Australians in remote areas heavily reliant on visiting primary healthcare services and requiring aeromedical retrieval.14,15 The reasons for this disparity are complex, and are entrenched in a history of social inequality, disempowerment, poverty, dispossession and discrimination.7
Due to limitations in service accessibility and the tyranny of distance required to access metropolitan-based health services, visiting services have become an essential component of the remote landscape. Many of the visiting health services provided in remote and very remote Australia are conducted by aeromedical means and community-lead primary healthcare Aboriginal Health Services.16 While there has been research on HSVD prevalence rates and associated disease risk factors [1,6] such as diabetes mellitus, hypertension, and renal disease [12,17,18], it is unclear how disease prevalence impacts emergency primary evacuation (EPE) in remote Australia.
With a primary focus on remote Australia, we aimed to determine whether HSVD prevalence and subsequent emergency primary evacuation, hospitalisation, and mortality differ by Indigenous status and remoteness in Australia.
Methods
An incidence population based study, including Australians who completed the National Health Survey, and patients requiring EPE, hospital admission, and those with a HSVD cause of death.
Statement of ethics
This project was deemed a low-risk quality assurance project by the Australian Capital Territory Health Research Ethics Committee (number: 2020.LRE.00246), and as such the requirement to obtain formal approval was waived.
Patient consent was obtained by the Australian Bureau of Statistics, with the full methodology published online.19,20
This research project includes two Aboriginal clinical researchers as authors, who contributed to the study design.
Setting
In 2018 there were 24,194,495 (96.8%) non-Indigenous Australians, with the majority living in major cities (n= 17,013, 352; 70.3%) and the remainder in inner-regional, outer-regional, remote, and very remote areas (7,181,143; 29.7%). There were 798,365 (3.2% of the total Australian population) Indigenous Australians, with the majority (n= 499,934; 62.6%) of the Indigenous population residing in inner-regional (n= 189,414; 23.7%), outer-regional (n= 161,791; 20.3%), remote (n= 53,507; 6.7%), and very remote areas (n= 95,222; 11.9%). The remainder were residing in major city areas (n=298,431; 37.4%).10
The term ‘non-remote’ includes major cities, inner-regional, and outer-regional areas, whereas the term ‘remote’ includes remote and very remote areas.
The Australian Bureau of Statistics 2016 Census was used to estimate population rates by Indigenous status and remoteness area. Rates for subsequent years were calculated using the ABS population estimates and projections based on the 2016 Census.10
Self-reported long-term heart, stroke, and vascular disease prevalence
To determine Indigenous and non-Indigenous self-reported rates of HSVD, we used data from the Australian Bureau of Statistics (ABS) National Health Survey (NHS) and the National Aboriginal and Torres Strait Islander Health Survey (NATSIHS).19,20 Participant informed consent was obtained during the NHS and the NATSIHS.
The NHS was conducted throughout Australia from July 2017 to June 2018 (12 months) with the aim of obtaining national information on the health status of all Australians.23 The NHS collected self-reported respondent data on whether participants had 1 or more long-term health conditions (i.e. >6 months), including (although not limited to) heart, stroke, and vascular disease comprising of ischaemic heart diseases (angina, heart attack and other ischaemic heart diseases), cerebrovascular diseases (stroke and other cerebrovascular diseases), oedema, heart failure, and diseases of the arteries, arterioles and capillaries.
The NATSIHS was conducted between July 2018 and April 2019 (9-months), and was aimed at providing information on long-term health conditions, health risk factors, selected social and emotional wellbeing indicators, health measurements, and health-related actions for Aboriginal and Torres Strait Islander people.22 As per the NHS above, the NATSIHS collected self-reported respondent data on whether they had 1 or more long-term health conditions (i.e. >6 months), including heart, stroke, and vascular disease.23
Aeromedical retrieval population data
Aeromedical data was prospectively collected on individual patients at the time of retrieval, from 1 July 2019 and the 30 October 2020 (16 months) from service that provides aeromedical coverage throughout rural and remote Australia. Data collected included the transfer date, transfer location, patient record number, patient age, gender and Indigenous status, and in-flight working diagnosis. All in-flight diagnoses were coded to the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10).21,22 This study included patients with a primary in-flight diagnosis of ICD-10 Chapter IX ‘diseases of the circulatory system’, which is consistent with ‘heart, stroke, and vascular disease’ prevalence, hospital admission, and mortality data. Patient informed consent was obtained during retrieval, with Indigenous status self-reported.
Hospital admission data
Hospital admission data was provided by the National Indigenous Australians Agency (NIAA) and the Australian Institute of Health and Welfare (AIHW), and included hospitalisations by age groups, principal diagnosis chapter (defined using ICD-10) and Indigenous status, for the time period of July 2015 to June 2017 (2-years).23 Patient informed consent was obtained by the reporting jurisdiction. Indigenous status was self-reported by the patient at hospitalisation.
Data from the years 2015 until 2017 were grouped, due to the small numbers each year, by remoteness and Indigenous status. For rate calculations per-1000 population averaged per-year, the numerator was the average of the total number of hospitalisations and the denominator is the mid-point of the population for the time period.
Mortality data
Morbidity data was provided by the AIHW National Hospital Morbidity Database (NHMD), and included HSVD death (as the underlying cause of death), by remoteness and Indigenous status for the time period July 2014 to June 2018.
Data from the years 2014 until 2018 was grouped, due to the small numbers each year, by remoteness and Indigenous status. For rate calculations per-1000 population average per-year, the numerator was the average of the total number of deaths and the denominator was the mid-point of the population for the time period.
Statistical analysis
Categorical variables were summarised as counts and proportions. The comparison between the Indigenous and the non-Indigenous samples was made by estimating 95% confidence intervals for means and proportions of interest for the samples and examining whether the population values belonged within those confidence intervals. The population value outside of the sample 95% confidence interval can be interpreted as indicative of a statistically significant difference between the samples at the significance threshold of 0.05.
Rate ratios were calculated by determining the age-standardised rate for Indigenous Australians and then dividing by the age-standardised rate for non-Indigenous Australians.
Remoteness and non-remoteness statistical differences were calculated using a chi-square goodness of fit test, with significance determined at a threshold of 0.05.
Statistical analyses were performed using the statistical software package R version 3.5.1.
Role of funding source
This is a self/internally-funded study, with the lead organisation being the Royal Flying Doctor Service (RFDS) of Australia. For the duration of the study period, the RFDS provided in-kind support including one full-time equivalent (FTE) and resources (office space, computer, research software, and office equipment)
The RFDS provided internal governance approval, via their Clinical Health Research Ethics Committee (CHREC). The following employees and research partners had access to the research data used during analysis: FWG; PS; PW; and LC. There was no external funding source that had a role in study design or data analysis or interpretation.
Results
Heart, stroke, and vascular disease prevalence
The NHS and the NATSIHS consisted of 21315 and 10579 participants respectively (see Figure 1). Indigenous Australians reported higher proportion of HSVD (age-standardised) at 229.0 per-1000 as compared to 152.0 per-1000 non-Indigenous Australians, equalling a risk ratio of 1.5 (95% CI 1.2-1.8). When considering Indigenous population proportions of self-reported HSVD, age-standardised prevalence did not significantly increase (p= 0.16) with remoteness, ranging from 225.0 per-1000 in non-remote (i.e. major cities, inner-regional and outer regional areas) to 252.0 per-1000 Indigenous people in remote areas. Similarly, non-Indigenous age-standardised rates did not significantly decrease (p= 0.49) with remoteness, from 152.0 per-1000 in non-remote to 141.0 per-1000 in remote areas.
Figure 1.
Participants data sources by Indigenous and remoteness.
Heart, stroke, and vascular disease -related evacuations
There were 583 patients who received an EPE for HSVD over the 16 months’ timeframe, consisting of 388 (66.6%; 95% CI: 62.6-70.4) males and 195 (33.3%; 95% CI: 29.6-37.4) females. The mean overall age was 51.8 (SD 17.1; 95% CI: 50.4-53.2), with a similar mean age between males (52.2; SD 16.5; 95% CI: 50.55-53.8) and females (51.1; SD 18.3; 95% CI: 48.5-53.7).
There were 289 (49.6%; 95% CI 45.4- 53.7) EPE patients who identified as Indigenous, which was significantly (p<0.001) higher compared to the overall Indigenous population proportion for remote and very remote Australia (30.0%). There were 294 (50.4%; 95% CI 46.3- 54.6) patients who were non-Indigenous, which was significantly lower than the overall non-Indigenous population proportion for remote and very remote Australia (70.0%).
Indigenous gender distribution for EPE was even, as compared to the overall and non-Indigenous figures, with 154 (53.3%; 95% CI 47.3-59.1) males and 135 (46.7%; 95% CI 40.85-52.65) females. There were 234 (79.6%; 95% CI 74.5-84.05) non-Indigenous males and 60 (20.4%; 95% CI 15.95-25.5) non-Indigenous females. The mean Indigenous age was 48.0 (SD 17.9; 95% CI 45.9-50.1) years old, which was significantly (p<0.001) lower than the non-Indigenous mean age of 55.6 (SD 15.4; 95% CI 53.8-57.4).
The leading reasons for primary evacuation were acute myocardial infarction (n=129; 22.1%), angina pectoris (n=108; 18.5%), stroke (n=62; 10.6%), atrial fibrillation and flutter (n=48; 8.2%), heart failure (n= 39; 6.7%), and all other HSVD diagnoses (n=197; 33.8%). Indigenous patients were more likely to receive a primary evacuation for heart failure (n=29; 10.3% 95% CI 6.8-14.1) as compared to non-Indigenous patients (n= 10; 3.4% 95% CI 1.6-6.2). Non- Indigenous patients were more likely to receive a primary evacuation for atrial fibrillation and flutter (n=38; 12.9% 95% CI 9.3-17.3) as compared to Indigenous patients (n=10; 3.5% 95% CI 1.7- 6.3). There were 18 (6.2%) patients, all Indigenous, who received an EPE for rheumatic fever (95% CI 3.7-9.7). See Table 1 for information concerning the leading retrieval reasons by Indigenous status.
Table 1.
Aeromedical primary evacuation leading diagnosis by Indigenous status.
| Primary Evacuation Diagnosis | Overall total number (%) | Indigenous Total (%) | 95% CI | Non- Indigenous Total (%) | 95% CI |
|---|---|---|---|---|---|
| Acute myocardial infarction | 129 (22.1) | 71 (24.6) | 19.7-29.95 | 58 (19.7) | 15.3-24.7 |
| Angina pectoris | 108 (18.5) | 46 (15.9) | 11.9-20.65 | 62 (21.1) | 16.6-26.2 |
| Stroke, not specified as haemorrhage or infarction | 62 (10.6) | 31 (10.7) | 7.41-14.9 | 31 (10.5) | 7.3-14.6 |
| Atrial fibrillation and flutter | 48 (8.2) | 10 (3.5) | 1.7-6.3 | 38 (12.9) | 9.3-17.3 |
| Heart failure | 39 (6.7) | 29 (10.3) | 6.8-14.1 | 10 (3.4) | 1.6-6.2 |
| Other cardiac arrhythmias | 17 (2.9) | 9 (3.1) | 1.4-5.8 | 8 (2.7) | 1.2-5.3 |
| Other acute ischaemic heart diseases | 16 (2.7) | 9 (3.1) | 1.4-5.8 | 7 (2.3) | 0.1-4.8 |
| Other venous embolism and thrombosis | 15 (2.6) | 5 (1.7) | 0.6-4.0 | 10 (3.4) | 1.6-6.2 |
| Paroxysmal tachycardia | 14 (2.4) | 6 (2.1) | 0.8-4.5 | 8 (2.7) | 1.2-5.3 |
| Rheumatic fever without mention of heart involvement | 13 (2.2) | 13 (4.5) | 2.4-7.6 | 0 (0.0) | n.a |
| Essential (primary) hypertension | 10 (1.7) | 5 (1.7) | 0.6-4.0 | 5 (1.7) | 0.6-3.9 |
| Other diseases of pericardium | 9 (1.5) | 2 (0.7) | 0.08-2.5 | 7 (2.4) | 0.1-4.8 |
| Pulmonary embolism | 9 (1.5) | 5 (1.7) | 0.6-4.0 | 4 (1.4) | 0.4-3.45 |
| Other conduction disorders | 8 (1.4) | 2 (0.7) | 0.08-2.5 | 6 (2.0) | 0.75-4.4 |
| Phlebitis and thrombophlebitis | 7 (1.2) | 2 (0.7) | 0.08-2.5 | 5 (1.7) | 0.6-3.9 |
| Rheumatic fever with heart involvement | 5 (0.9) | 5 (1.7) | 0.6-4.0 | 0 (0.0) | n.a |
| Atrioventricular and left bundle-branch block | 5 (0.9) | 2 (0.7) | 0.08-2.5 | 3 (1.0) | 0.2-2.95 |
| Chronic ischaemic heart disease | 5 (0.9) | 2 (0.7) | 0.08-2.5 | 3 (1.0) | 0.2-2.95 |
| Intracerebral haemorrhage | 5 (0.9) | 1 (0.35) | 0.01-1.9 | 4 (1.4) | 0.4-3.45 |
| Hypotension | 5 (0.9) | 3 (1.0) | 0.2-3.0 | 2 (0.7) | 0.08-2.4 |
| All other | 54 (9.3) | 31 (10.7) | 7.4-14.9 | 23 (7.8) | 5.02-11.5 |
| Total | 583 (100.0) | 289 (49.6) | 45.4-53.7 | 294 (50.4) | 46.3-54.6 |
We observed 1.4 (95% CI 1.2-1.6) EPE events per-1000 Indigenous person-years, and, 0.6 (95% CI 0.5-0.7) EPE events per-1000 non-Indigenous person-years, resulting in an Indigenous to non-Indigenous rate ratio of 2.3 (95% CI 2.0-2.7). After adjusting the raw EPE rates for the reported HSVD prevalence, there was an EPE for HSVD rate of 7.5 per 1000 Indigenous person-with-HSVD-years and 5.7 per 1000 for non-Indigenous person-with-HSVD-years in remote Australia, resulting in a prevalence adjusted EPE Indigenous to non-Indigenous rate ratio of 1.31 (95% CI 0.4-3.9).
Heart, stroke, and vascular disease-related hospitalisations
There were 1,110,484 Australia-wide hospitalisations for HSVD between the time period of July 2015 to June 2017 (2-years), consisting of 28,729 (2.6%) Indigenous and 1,081,755 (97.4%) non-Indigenous patients. The average hospitalisation rate for Indigenous patients was numerically (p>0.05) higher at 32.0 per-1000 person-years as compared to non- Indigenous patients at 19.9 per-1000 person-years, giving an Indigenous to non-Indigenous rate ratio of 1.6 (95% CI 0.9-2.8). Similar to EPE, Indigenous patients were younger (p<0.001) with the majority hospitalised before the age of 65 years (n=21,175; 73.7% 95% CI 73.2-74.2) as compared to non-Indigenous patients (n= 357,654; 33.1% 95% CI 33.0-33.15).
The average Indigenous hospitalisation rate for HSVD was 30.0 per-1000-person-years in non-remote areas and 44.0 per-1000-person-years in remote areas, resulting in Indigenous remote-to-non-remote hospitalisation rate ratio of 1.5 (95% CI 0.9-2.4). The rate of non-Indigenous hospitalisations remained constant at 20.0 per-1000 person-years in non-remote and 20.1 per 1000 person-years in remote areas, resulting in a hospitalisation rate ratio of 1.0 (95% CI 0.5-1.9) for non-Indigenous population.
After adjusting the hospitalisation figures for the reported HSVD prevalence, Australia-wide Indigenous patients with HSVD were hospitalised at a rate of 139.7 per-1000 person-with-HSVD years, and non-Indigenous were hospitalised at a rate of 130.9 per-1000 person-with-HSVD-years, resulting in a rate ratio of 1.07 (95% CI 0.8-1.4) for Indigenous-to-non-Indigenous patients with HSVD. Remote Indigenous patients with HSVD had a hospitalisation rate of 175.0 per-1000 person-with-HSVD-years as compared to the hospitalisation rate of 110 per-1000 person-with-HSVD-years in non-remote Indigenous patients with HSVD, resulting in a rate ratio of 1.6 (95% CI 1.3-2.0). Remote non-Indigenous patients with HSVD had a hospitalisation rate of 142.0 per-1000 person-with-HSVD-years as compared to non-remote non-Indigenous rate of 128.0 per-1000 person-with-HSVD-years, resulting in a rate ratio of 1.11 (95% CI 0.9-1.4). When comparing the hospitalisations, remote Indigenous had a rate ratio of 1.2 (95% CI 1.0-1.5) as compared to remote non-Indigenous patients.
Heart, stroke, and vascular disease-related mortality
There were 156,731 reported cases with an underlying cause of death associated with HSVD between the time period of July 2014 to June 2018 (4-years), consisting of 3,319 (2.1%) Indigenous, 152,461 (97.3%) non-Indigenous patients, and 951 (0.6%) missing Indigenous status. Indigenous patients were younger with the majority of deaths occurring before the age of 65 years (n=1,875; 56.5%, 95% CI 54.8-58.2) as compared to non-Indigenous patients (n= 16,161; 10.6%, 95% CI 10.45-10.8).
The average death rate for Indigenous patients was 2.3 per 1000 person-years as compared to non- Indigenous patients at 1.6 per 1000 person-years, resulting in an Indigenous to non-Indigenous rate ratio of 1.4 (95% CI 0.2-10.5). The average Indigenous deaths rate was 3.3 per 1000 person-years in remote areas and 2.0 per 1000 person-years in non-remote areas, resulting in a rate ratio of 1.65 (95% CI 0.3-9.6). Non-Indigenous deaths rates were 1.5 per 1000 person-years in remote areas and 1.6 per 1000 person-years in non-remote areas, resulting in a rate ratio of 0.9 (95% CI 0.1-8.3).
After adjusting the mortality figures for the self-reported HSVD prevalence, Indigenous Australians with HSVD had a HSVD death rate at 10.0 per- 1000 person-with-HSVD-years as compared to non-Indigenous with a death rate at 10.5 per- 1000 person-with- HSVD-years, resulting in a mortality rate ratio between Indigenous to non-Indigenous Australians of 0.95 (95% CI 0.4-2.3). Remote Indigenous patients with HSVD had a death rate from HSVD at 13.1 per-1000 person years as compared to 8.9 per-1000 person years for non-remote Indigenous patients, resulting in a rate ratio of 1.5 (95% CI 0.6-3.5). Non-Indigenous patients with HSVD had a death rate of 10.6 per- person-with-HSVD-years in remote areas and 10.5 per-1000 person-with-HSVD-years in non-remote areas, resulting in a rate ratio of 1.0 (95% CI 0.4-2.3).
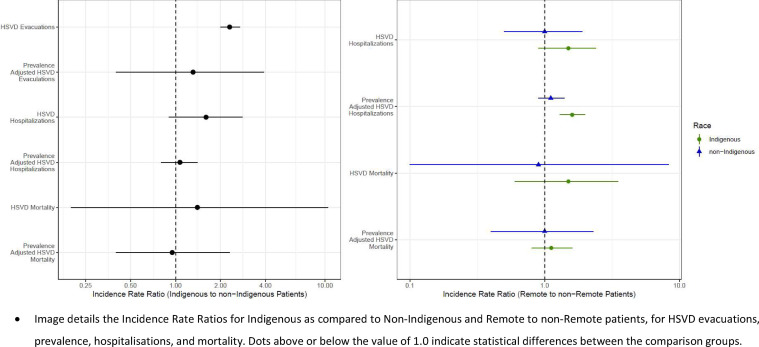
Please see Figure 2, Figure 3 for HSVD prevalence, and prevalence adjusted hospitalisation and mortality by Indigenous and remoteness.
Figure 2.
Incidence rate ratios for HSVD Evacuation, Hospitalization, and Mortality by Indigenous status and Remoteness. Image details the Incidence Rate Ratios for Indigenous as compared to Non-Indigenous and Remote to non-Remote patients, for HSVD evacuations, prevalence, hospitalisations, and mortality. Dots above or below the value of 1.0 indicate statistical differences between the comparison groups.
Figure 3.
Per-1000 population ratios for HSVD Evacuation, Hospitalization, and Mortality by Indigenous status and Remoteness.
Discussion
While Australia has made some progress in improving the health of Indigenous Australians between the years 2008 and 2018,7,24 major disparities persist and constitute a critical health challenge. From 2015 until 2017 the life expectancy for remote Indigenous males was still estimated to be 6.2 years lower than that of Indigenous males living in major cities (65.9 years compared with 72.1 years). For Indigenous females, the age gap was even wider at 6.9 years (69.6 years compared with 76.5 years).7 Consistent with these findings, we have demonstrated that the gap in healthcare for HSVD outcomes is unacceptably greater for Indigenous Australians living in remote Australia compared to their metropolitan counterparts. Reflecting these trends, we have also shown that Indigenous Australians in remote areas are retrieved, hospitalised and die at a younger age then their non-Indigenous counterparts. As such, any future “Closing the Gap” measures should heavily focus on the health inequalities in remote Australia. These measures should include Indigenous inclusion in the design and delivery of health care that is culturally safe and incorporates the needs of Indigenous Australians.
We found that Indigenous patients with HSVD were significantly younger than non-Indigenous patients during EPE, at hospital admission and at time of death. These findings reflect those of Brown (2010), who found that among 492 patients with acute coronary syndrome, Indigenous patients (n=214) were significantly younger with a mean age of 50.1 years as compared to non-Indigenous patients (n=278) with a mean age of 59.3 years old.25 Furthermore, in accord with our findings, just over half of the Indigenous group were male (57%), compared to almost 70.0% of the non-Indigenous group. Brown (2010) also found that Indigenous patients were significantly more likely to experience high risk acute coronary syndromes, similar to our observation that Indigenous patients were more likely to be suffering from heart failure.25 Others have shown that Indigenous heart failure hospitalisation rates are 11 times higher in men and 23 times higher in women aged 20-39 years of age,26 reflecting the high rates of diabetes, obesity, poor nutrition, hypertension, chronic kidney disease, tobacco smoking, and coronary artery disease in this population group.27 These well documented risk factors for heart failure are compounded by socio-economic disadvantage, inadequate infrastructure, service inaccessibility, and culturally unsafe health care and disease prevention programs for Indigenous Australians.
International findings suggest that low socio-economic population groups are likely to delay care due to factors associated with social determinants of health, such as poverty and high medical cost (direct and in-direct). This has been highlighted during the COVID-19 pandemic, with marginalised groups such as African and Native Americans, having a greater burden of disease, with COVID-19 exploiting social, economic, and health inequalities such as accessibility to affordable health insurance/ coverage.28 This “inverse care law” results in socially disadvantaged people receiving less, and lower-quality, health care despite having greater need.29
We found that, for Indigenous people living in remote Australia, the EPE, hospitalisation and mortality rates reflected the higher prevalence of HSVD in this population. However, our finding that non-remote Indigenous Australians with HSVD had lower hospital admission rates is intriguing. Others have shown that that Indigenous Australians are also less likely to receive a HSVD diagnostic procedure in hospital such as coronary angiography,30 thus limiting revascularisation (PCI or CABG) rates following angiography, potential leading to higher mortality rates for Indigenous Australians. However, similar findings in the Northern Territory of Australia,25 found that remote Indigenous Australians who did undergo angiography were subsequently prescribed evidence‐based therapies on discharge at comparable rates to non-Indigenous patients. This reflects similar findings in the United States where the greatest racial disparity was found to be in the referral for coronary angiography.31,32 Of interest, Aboriginal Australians with acute coronary syndromes have reported that negative hospital experiences, bias associated with complex comorbidities favouring conservative management, and patient choice may be responsible for lower angiography rates.33 Overall, it remains uncertain why Indigenous Australians present late for medical services, although cultural safety issues including discrimination and institutional racism most likely play a major role. Further research is urgently required to better understand the differences we have identified between remote and non-remote Indigenous people in the treatment and outcomes for HSVD.
In Australia, and other countries such as Canada that share a colonial history, health inequities arising from colonisation practices, have resulted in trauma and mistrust.34 As such, it is not enough to just provide additional services, they need to be culturally appropriate, and developed based on community need. This involves talking and engaging with communities. Indigenous patients value talk within healthcare communication, and is essential to their experience of care.35 Good talk and engagement (i.e. not talking down or being imposing) is an essential component to improve Indigenous engagement and accessibility to healthcare services.35 Historically this engagement has been poor, as indicated in the racial disparities in delivery of cardiac care in Australia.
This study included aeromedical data from a single service. This limitation was reduced by this service being the largest aeromedical provided in the world. A further potential limitation was the in-flight nature of the aeromedical diagnosis, which could differ to subsequent hospital discharge diagnosis. However, this limitation was reduced by grouping in-flight diagnosis into the high level diagnostic category of HSVD, which limited sub-diagnostic errors.
A limitation of this analysis was the self-reported disease prevalence data, and the risk for self-reporting bias, and the surveys being completed across different time points. Future surveys should validate disease prevalence via systems such as the Australian National Health Record. Furthermore, mortality data highlighting Indigenous status was provided from 5 out of 8 Australians jurisdictional areas. The capturing of this data is required to ensure culturally appropriate care and should be a policy priority for all jurisdictions.
Remote Australians were found to have higher prevalence of HSVD as compared to non-remote Australians, with Indigenous status and HSVD prevalence significantly influenced by remoteness. In line with this increase prevalence of HSVD, we found significantly more EPE for remote Indigenous Australians per-1000 population compared to non-Indigenous Australians, suggesting that the service is viewed as culturally accessible and safe. These Indigenous Australians were significantly younger and most frequently retrieved with acute coronary syndromes. This was also reflected in the higher hospitalisation rates at a younger age and younger age at death from HSVD for Indigenous Australians from remote areas as compared to non-Indigenous patients.
Data sharing statement
Population disease prevalence data can be accessed online via the Australian Bureau of Statistics website,19,20 or by emailing the corresponding author.
Please also contact the corresponding author for access to aeromedical primary evacuation, hospitalisation, and mortality data. Data provided to external sources requires approval by the Royal Flying Doctor Service's Clinical Health Research Ethics Committee, prior to release. Please contact the corresponding author for the relevant forms.
Declaration of Competing Interest
None.
Acknowledgments
Funding
This is a self/internally-funded study, with the lead organisation being the Royal Flying Doctor Service (RFDS) of Australia. For the duration of the study period, the RFDS provided in-kind support including one full-time equivalent (FTE) and resources (office space, computer, research software, and office equipment). There was no external funding source that had a role in study design or data analysis or interpretation.
Author contributions
FWG and PW formulated the research question and design and conducted the analysis and drafted the paper for submission. KR-B, ADS, GAD, SMD, PT, and FQ drafted the paper for submission. PS assisted with data analysis. LC conducted the statistical analysis and formulated the research design.
References
- 1.Calabria B., Korda R.J., Lovett R.W. Absolute cardiovascular disease risk and lipid-lowering therapy among Aboriginal and Torres Strait Islander Australians. Med J Aust. 2018;209(1):35–41. doi: 10.5694/mja17.00897. [DOI] [PubMed] [Google Scholar]
- 2.Rhoades D.A. Racial misclassification and disparities in cardiovascular disease among American Indians and Alaska Natives. Circulation. 2005;111(10):1250–1256. doi: 10.1161/01.CIR.0000157735.25005.3F. [DOI] [PubMed] [Google Scholar]
- 3.Smith E.R. The Canadian heart health strategy and action plan. The Canadian journal of cardiology. 2009;25(8):451. doi: 10.1016/s0828-282x(09)70116-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Atzema C.L., Khan S., Lu H. Cardiovascular disease rates, outcomes, and quality of care in Ontario Métis: a population-based cohort study. PLoS One. 2015;10(3) doi: 10.1371/journal.pone.0121779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhao Y., Vemuri S.R. Arya D. The economic benefits of eliminating Indigenous health inequality in the Northern Territory. Medical Journal of Australia. 2016;205(6):266–269. doi: 10.5694/mja16.00215. [DOI] [PubMed] [Google Scholar]
- 6.Al-Yaman F. The Australian Burden of Disease Study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people, 2011. Public Health Res Pract. 2017;27(4) doi: 10.17061/phrp2741732. [DOI] [PubMed] [Google Scholar]
- 7.Minister ADotP, Cabinet. Closing the Gap report 2020. 2020.
- 8.Health AIo, Welfare. Indigenous health and wellbeing. Canberra: AIHW;2020.
- 9.Australian Bureau of Statistics. 3303.0 - Causes of Death, Australia. Australian Bureau of Statistics. https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/3303.0∼2017∼Main%20Features ∼Australia's%20leading%20causes%20of%20death,%202017∼2. Published 2017. Accessed 1 December 2020.
- 10.Australian Bureau of Statistics. Estimates and Projections, Aboriginal and Torres Strait Islander Australians. Australian Bureau of Statistics. https://www.abs.gov.au/statistics/people/aboriginal-and-torres-strait-islander-peoples/estimates-and-projections-aboriginal-and-torres-strait-islander-australians/latest-release#data-download. Published 2019. Accessed 15 December 2020.
- 11.McGrail M.R., Humphreys J.S. Spatial access disparities to primary health care in rural and remote Australia. Geospat Health. 2015;10(2):358. doi: 10.4081/gh.2015.358. [DOI] [PubMed] [Google Scholar]
- 12.Gardiner F.W., Bishop L., Dos Santos A. Aeromedical retrieval for stroke in Australia. Cerebrovascular Diseases. 2020;49(3):334–340. doi: 10.1159/000508578. [DOI] [PubMed] [Google Scholar]
- 13.Liaw S.T., Lau P., Pyett P. Successful chronic disease care for Aboriginal Australians requires cultural competence. Australian and New Zealand journal of public health. 2011;35(3):238–248. doi: 10.1111/j.1753-6405.2011.00701.x. [DOI] [PubMed] [Google Scholar]
- 14.Jones R., Langford S. Australia's Royal Flying Doctor Service is the World's Largest Aeromedical Response Service.
- 15.Gardiner F., Coleman M. 2020. A letter from.. Western Australia. Lancet PsychiatryIn Press. [Google Scholar]
- 16.Gardiner F., Gale L., Ransom A., Laverty M. Looking Ahead: Country Australia's Health Service Needs in 2028. In: Royal Flying Doctor Service; 2018 [Google Scholar]
- 17.Gardiner F.W., Bishop L., Gale L. Poor access to kidney disease management services in susceptible patient populations in rural Australia is associated with increased aeromedical retrievals for acute renal care. Internal medicine journal. 2020;50(8):951–959. doi: 10.1111/imj.14716. [DOI] [PubMed] [Google Scholar]
- 18.Haynes A., Kalic R., Cooper M., Hewitt J.K., Davis E.A. Increasing incidence of type 2 diabetes in Indigenous and non-Indigenous children in Western Australia, 1990-2012. Med J Aust. 2016;204(8):303. doi: 10.5694/mja15.00958. [DOI] [PubMed] [Google Scholar]
- 19.Australian Bureau of Statistics. National Aboriginal and Torres Strait Islander Health Survey. Australian Bureau of Statistics. https://www.abs.gov.au/methodologies/national-aboriginal-and-torres-strait-islander-health-survey-methodology/2018-19. Published 2019. Accessed 08 December 2020.
- 20.Australian Bureau of Statistics. National Health Survey: methodology. Australian Bureau of Statistics. https://www.abs.gov.au/methodologies/national-health-survey-first-results-methodology/2017-18. Published 2018. Accessed 15 December, 2020.
- 21.Gardiner F.W., de Graaff B., Bishop L., Campbell J.A., Mealing S., Coleman M. Mental Health Crises in Rural and Remote Australia: An Assessment of Direct Medical Costs of Air Medical Retrievals and the Implications for the Societal Burden. Air medical journal. 2020;39(5):343–350. doi: 10.1016/j.amj.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brämer G.R. International statistical classification of diseases and related health problems. Tenth revision. World health statistics quarterly Rapport trimestriel de statistiques sanitaires mondiales. 1988;41(1):32–36. [PubMed] [Google Scholar]
- 23.National Indigenious Australians Agency. Access data. National Indigenious Australians Agency, https://www.indigenoushpf.gov.au/access-data. Published 2020. Accessed 12 December 2020.
- 24.Holland C. A ten-year review: the Closing the Gap strategy and recommendations for reset. [Australian Human Rights Commission], the Close the Gap Campaign Steering, 2018.
- 25.Brown A. Acute Coronary Syndromes in Indigenous Australians: Opportunities for Improving Outcomes Across the Continuum of Care. Heart, Lung and Circulation. 2010;19(5):325–336. doi: 10.1016/j.hlc.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 26.Teng T.-H.K., Katzenellenbogen J.M., Thompson S.C. Incidence of first heart failure hospitalisation and mortality in Aboriginal and non-Aboriginal patients in Western Australia, 2000–2009. International Journal of Cardiology. 2014;173(1):110–117. doi: 10.1016/j.ijcard.2014.02.020. [DOI] [PubMed] [Google Scholar]
- 27.Katzenellenbogen J.M., Sanfilippo F.M., Hobbs M.S. Aboriginal to non-Aboriginal differentials in 2-year outcomes following non-fatal first-ever acute MI persist after adjustment for comorbidity. European journal of preventive cardiology. 2012;19(5):983–990. doi: 10.1177/1741826711417925. [DOI] [PubMed] [Google Scholar]
- 28.Snowden L.R., Graaf G. COVID-19, Social Determinants Past, Present, and Future, and African Americans’ Health. Journal of Racial and Ethnic Health Disparities. 2021;8(1):12–20. doi: 10.1007/s40615-020-00923-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cookson R., Doran T., Asaria M., Gupta I., Mujica F.P. The inverse care law re-examined: a global perspective. The Lancet. 2021;397(10276):828–838. doi: 10.1016/S0140-6736(21)00243-9. [DOI] [PubMed] [Google Scholar]
- 30.Tavella R., McBride K., Keech W. Disparities in acute in-hospital cardiovascular care for Aboriginal and non-Aboriginal South Australians. Medical Journal of Australia. 2016;205(5):222–227. doi: 10.5694/mja16.00445. [DOI] [PubMed] [Google Scholar]
- 31.Schulman K.A., Berlin J.A., Harless W. The effect of race and sex on physicians' recommendations for cardiac catheterization. N Engl J Med. 1999;340(8):618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 32.Weintraub W.S., Vaccarino V. Explaining racial disparities in coronary outcomes in women. Circulation. 2003;108(9):1041–1043. doi: 10.1161/01.CIR.0000083529.48474.4F. [DOI] [PubMed] [Google Scholar]
- 33.Ilton M.K., Walsh W.F., Brown A.D., Tideman P.A., Zeitz C.J., Wilson J. A framework for overcoming disparities in management of acute coronary syndromes in the Australian Aboriginal and Torres Strait Islander population. A consensus statement from the National Heart Foundation of Australia. Med J Aust. 2014;200(11):639–643. doi: 10.5694/mja12.11175. [DOI] [PubMed] [Google Scholar]
- 34.Jacklin K.M., Henderson R.I., Green M.E., Walker L.M., Calam B., Crowshoe L.J. Health care experiences of Indigenous people living with type 2 diabetes in Canada. CMAJ. 2017;189(3) doi: 10.1503/cmaj.161098. E106-E112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jennings W., Bond C., Hill P.S. The power of talk and power in talk: a systematic review of Indigenous narratives of culturally safe healthcare communication. Aust J Prim Health. 2018;24(2):109–115. doi: 10.1071/PY17082. [DOI] [PubMed] [Google Scholar]