Abstract
Objective
To describe the characteristics of contacts of patients with COVID-19 case in terms of time, place and person, to calculate the secondary attack rate (SAR) and factors associated with COVID-19 infection among contacts.
Design
A retrospective cohort study
Setting and participants
Contacts of cases identified by the health department from 14 March 2020to 30 May 2020, in 9 of 38 administrative districts of Tamil Nadu. Significant proportion of cases attended a religious congregation.
Outcome measure
Attack rate among the contacts and factors associated with COVID-19 positivity.
Results
We listed 15 702 contacts of 931 primary cases. Of the contacts, 89% (n: 14 002) were tested for COVID-19. The overall SAR was 4% (599/14 002), with higher among the household contacts (13%) than the community contacts (1%). SAR among the contacts of primary cases with congregation exposure were 5 times higher than the contacts of non-congregation primary cases (10% vs 2%). Being a household contact of a primary case with congregation exposure had a fourfold increased risk of getting COVID-19 (relative risk (RR): 16.4; 95% CI: 13 to 20) than contact of primary case without congregation exposure. Among the symptomatic primary cases, household contacts of congregation primaries had higher RR than household contacts of other cases ((RR: 25.3; 95% CI: 10.2 to 63) vs (RR: 14.6; 95% CI: 5.7 to 37.7)). Among asymptomatic primary case, RR was increased among household contacts (RR: 16.5; 95% CI: 13.2 to 20.7) of congregation primaries compared with others.
Conclusion
Our study showed an increase in disease transmission among household contacts than community contacts. Also, symptomatic primary cases and primary cases with exposure to the congregation had more secondary cases than others.
Keywords: COVID-19, epidemiology, infection control, public health
Strengths and limitations of this study.
We documented the secondary attack rate (SAR) of COVID-19 in a large cohort of more than 15 000 contacts in India.
All the contacts were tested with RT-PCR; therefore, the estimates of SAR were reliable.
The state updated the testing policy in the early phase of this pandemic based on the findings from this study.
We did not have confirmation of the COVID-19 status of 11% of the contacts.
Contact tracing was prioritised for household contacts during lockdown as the community interactions were limited.
Background
The novel coronavirus outbreak due to SARS-CoV-2 infection reported from China in December 2019 was declared a Public Health Emergency of International Concern by WHO on 30 January 2020.1 At the early stages of COVID-19, international travel was the most common exposure. Subsequently, clusters emerged in various settings, including community gatherings, hospital settings and commercial gatherings. Investigating such clusters provided clues for disease transmission and guided intervention strategies for pandemic response.2 Contact tracing is one of the key strategies to interrupt the chain of transmission of SARS-CoV-2. The aim of the contact tracing strategy is to reduce secondary cases of COVID-19. In this context, the secondary attack rate (SAR) of SARS-CoV-2 denotes the probability that infection occurs among susceptible contacts within a reasonable incubation period following contact with the infectious person(s) or that of the source3 and represents infectiousness of the agent. The SAR among contacts, thus, is a useful indicator to track the viral transmission potential4 and thereby guides control strategies. The SAR of SARS-CoV-2 differs from the nature of the setting and that of the symptomatic status of the primary cases.5–8 Understanding the dynamics of transmission of COVID-19 for specific settings will help in preventing the spread of the infection.9
India reported the first laboratory-confirmed case on 30 January 2020, from a southern state, Kerala. In early March, most reported cases had a history of international travel or contact with the traveller.10 Tamil Nadu, the southern state of India, reported the first case of COVID-19 on 18 March 2020.11 At the initial stages, COVID-19 cases were reported among international travellers and subsequently among travellers from other states. On 13 March, the media reported a cluster of cases linked to a religious congregation in New Delhi.12 13 According to the reports, the event started on 9 February 2020, with more than 4000 participants from various Indian states and abroad gathered in groups to attend the meeting.14 As the participants returned to their respective states, clusters emerged in several states.15 People from Tamil Nadu also participated in the meeting, predominantly during 21–23 March 2020.16 After returning from the event, attendees travelled to many parts of the State. Public health authorities initiated a massive search for potential cases and their contact in various districts.
From February 2020, the health department of Tamil Nadu state practised testing and quarantine of international travellers and enhanced the voluntary testing of symptomatic individuals with history of travel or hostory of contact with a traveller. When the congregation cluster was reported, all the persons who attended the congregation were traced, quarantined and tested. The persons tested for COVID-19 were isolated and treated. The persons who tested negative were quarantined for 14 days. Also, the COVID-19 test was repeated after fifth day of the first testing. The household members of the attendees were immediately tested for COVID-19, if any person is tested positive.
After the information of COVID-19 outbreak in the Delhi congregation setting, Government of Tamil Nadu collected the line list of participants from the appropriate authority involved in the outbreak control in the congregation. The district collected additional information from the local leaders.
At the time this investigation was undertaken, there was no widespread community transmission. Most of the infection was among travellers and healthcare workers, and they did not mingle with the community due to restrictions. Unlike international travellers, congregation participants travelled with other local travellers and after attending the congregation, all resumed social and work-related activities after arrival. Therefore, they are more likely to transmit to the community.
Due to the novelty of the pandemic, the transmission dynamics of the diseases were not fully understood. In the early phase, knowledge on the spread of the disease in various settings and in different geographical was not known. Also, the contribution of the congregation cluster in driving the pandemic is not known. Knowing this information was crucial in preventing the disease’s spread from the primary case to the contacts. In this context, we conducted a study to estimate the SAR in terms of time, place and person and determined risk factors for COVID-19 infection among contacts during March–May 2020 in Tamil Nadu, India.
Methods
Study design
We conducted a retrospective cohort study of all contacts of COVID-19 cases between 14 March 2020 to 30 May 2020 of Tamil Nadu, the Southern state of India.
Study setting and the COVID-19 context
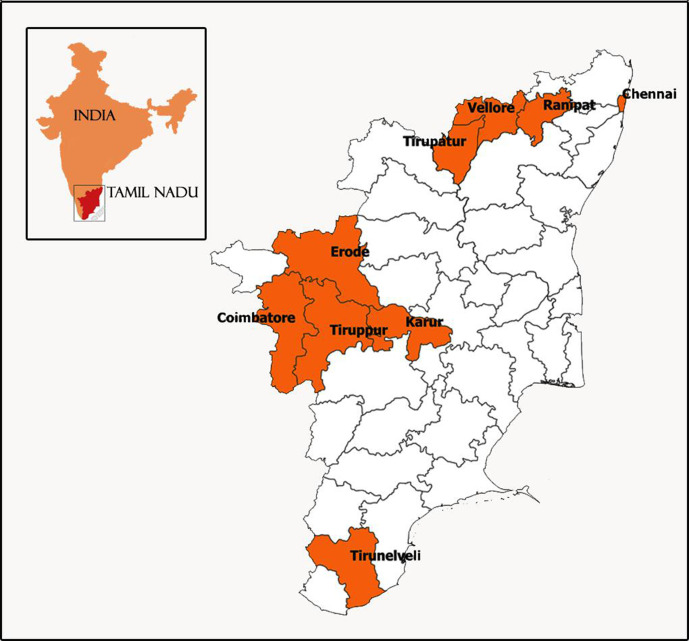
We studied 9 of 38 administrative districts reporting maximum cases during the study period (figure 1). These nine districts reported higher number of cases during the study period. The study districts varied in a population density ranging from 28 553 persons/km2 in the State’s capital city of Chennai to 367 in Erode district, located southwest of Chennai. The average family size was similar (3.5–4.3 persons per family) across these study districts.
Figure 1.
Map of Tamil Nadu included in the epidemiological study of COVID-19.
The COVID-19 response strategies implemented by the State included surveillance for case identification, confirmation with reverse transcriptase PCR (RT-PCR) test for COVID-19, contact tracing, isolation and quarantine, in addition to community-based interventions. The confirmation with RT-PCR was done by identifying two or more target genes (E/RdRp/ORF1ab/N/S) using multiplex PCR kits. The district officials hospitalised the patients with COVID-19, and quarantined COVID-19 tested negatives at home or facility. By contact tracing, the officials identified the household and the community contacts and tested them for COVID-19. We included all COVID-19 confirmed cases in the study period from these districts.
Sampling and sample size
We listed all the identified confirmed COVID-19 cases in the study districts from 1 March 2020 to 30 May 2020. We included all the contacts of the individuals identified as COVID-19 positive.
Operational definitions
Primary case: any individual with a laboratory-confirmed COVID-19 case with no reported history of contact with COVID-19 case
Symptomatic cases: any individual with h/o fever, cough, sore throat or breathlessness from 5 days before the date of testing.
Confirmed case: any individual who is tested positive for COVID-19 using RT-PCR
Contact: any individual comes in proximity with individuals positive for COVID-19.17 High-risk contacts is defined as any person who was in proximity with individuals positive for COVID-19 within 2 m of proximity for 15 min. Low-risk contact is defined as any person who was in proximity with individuals positive for COVID-19 and sharing same environment but not having high exposure.
Household contact: any individual living in the same household and comes in proximity with the individual with COVID-19 confirmed.
Community contact: any individual other than living in the same household and comes in proximity with the individual with COVID-19 confirmed.
Cluster: an unusual aggregation of two are more COVID-19 cases grouped in time and space and reported to a health agency.18
Congregation exposure: individual who have attended the religious congregation event held during February and March 2020 (newspaper reference).
SAR: the SAR is the proportion of individuals positive for COVID-19 among the tested contacts.
Data collection and analysis
We collected data from district surveillance records and classified the contacts as household and community contacts. We abstracted the information on sociodemographic characteristics, residence location, symptom status and congregation exposure of the primary case from the district surveillance records.
The analysis is based on the information from nine identified districts. We described the total number of contacts and the median number of contacts per case by the district. We calculated the overall SAR for COVID-19 and by age, gender, symptom status and congregation exposure of the primary case. We estimated the SAR by symptom status and congregation exposure of the primary case in two subgroups, namely, household and community contacts. We determined the risk factors associated with COVID-19 infection among contacts based on the household versus community exposure, congregation versus non-congregation exposure of primary case and symptom status of the primary case. We estimated the unadjusted and age/sex-adjusted relative risk (RR) and 95% CIs for the four categories of contacts. The community contacts of the non-congregation primary case were the reference category. The other categories were community contacts of congregation primary, household contacts of non-congregation and household contacts of congregation primary cases. We also estimated the unadjusted and age/sex-adjusted RR and 95% CI after stratifying the four categories by symptom status of the primary case.
Human participation protection
No primary information was collected from the participants. We maintained complete confidentiality and anonymity of the participants during data abstraction.
Patient and public Involvement in research
Patients and/or the public were not involved in the conduct of research.
Results
Description of the cases and contacts
We identified 931 COVID-19 primary cases and 15 702 contacts during the study period. The median number of contacts identified per COVID-19 case was 17 (IQR: 9–18) in the selected nine districts. Around 11% (n: 102) of the cases did not have household contacts. The duration from the reporting of the first COVID-19 case to the time of data abstraction ranged from 51 days for Chennai and 15 days for Karur district (table 1). This is because the reporting of the first case varies across the districts and the data collection was done in the same period across these districts and hence the duration of the data collection period varies.
Table 1.
Frequency of contacts traced per COVID-19 primary case by district, Tamil Nadu, India, March–May 2020
| District | Days since reporting of the first case in the district | # primary cases | Frequency of contacts | Number of contacts tested | Number of contacts tested positive | Secondary attack rate | |||
| # contacts identified | Household contacts | Community contacts | Median (range) contacts per primary case | ||||||
| Chennai | 51 | 530 | 9731 | 1795 | 7936 | 18 (1–151) | 9724 | 261 | 3 (2.4–3.0) |
| Coimbatore | 33 | 151 | 3257 | 570 | 2687 | 22 (1–274) | 1585 | 151 | 10 (8.2–11.1) |
| Erode | 46 | 56 | 1032 | 246 | 786 | 18 (3–141) | 1032 | 38 | 4 (2.7–5.0) |
| Karur | 15 | 42 | 416 | 271 | 145 | 10 (1–86) | 416 | 18 | 4 (2.8–6.7) |
| Ranipet | 25 | 29 | 273 | 153 | 120 | 9 (1–68) | 273 | 11 | 4 (2.3–7.1) |
| Tirunelveli | 23 | 35 | 166 | 157 | 9 | 5 (1–21) | 145 | 20 | 14 (9.1–20.0) |
| Tirupathur | 20 | 12 | 312 | 61 | 251 | 26 (1–100) | 312 | 5 | 2 (0.7–3.7) |
| Tiruppur | 24 | 66 | 279 | 241 | 38 | 5 (1–10) | 279 | 80 | 29 (23.7–34.0) |
| Vellore | 23 | 10 | 236 | 51 | 185 | 24 (6–79) | 236 | 15 | 6 (3.9–10.0) |
| Overall | 931 | 15 702 | 3545 | 12 157 | 17 (5–26) | 14 002 | 599 | 4 (4.0–4.6) | |
Of the identified 15 702 contacts, 14 002 (89%) contacts were tested for COVID-19. Apart from household contacts, most community contacts (98%) were cab drivers, vegetable sellers, co-workers or co-passengers in public transport. The majority of the household contacts (99%) were tested. There is no difference between tested and not-tested by age and gender (data not shown).
Information on age was available for 99.7% (13 969/14 002) of the contacts (table 2). The contacts were predominantly aged 21–40 years (41%) and 41–59 years (27%). Over half of the contacts were males (53%). About one-fourth (28%) of the contacts were traced from primary cases with congregation exposure, and 25% of the contacts had household COVID-19 exposure. Healthcare providers contributed to less than 1% of the contacts identified for the primary cases.
Table 2.
Secondary attack rate (%) by selected characteristics among the contacts traced per COVID-19 primary case, Tamil Nadu, India, March–May 2020
| Selected characteristics | Number of contacts (%) | # COVID-19 positive | Secondary attack rate (%) (95% CI) | |
| Overall | 14 002 (100%) | 599 | 4 (4.0 to 4.6) | |
| Age in years (N=13 379) | ≤20 | 3203 (24%) | 138 | 4 (3.7 to 5.1) |
| 21–40 | 5511 (41%) | 237 | 4 (3.8 to 4.9) | |
| 41–59 | 3364 (25%) | 155 | 5 (4.0 to 5.4) | |
| 60+ | 1301 (10%) | 65 | 5 (4.0 to 6.4) | |
| Gender (N=13 969) | Male | 7443 (53%) | 280 | 4 (3.4 to 4.2) |
| Female | 6526 (47%) | 318 | 5 (4.4 to 5.4) | |
| Congregation exposure of primary case (N=14 002) | Yes | 3884 (28%) | 377 | 10 (8.8 to 10.7) |
| No | 10 118 (72%) | 222 | 2 (1.9 to 2.5) | |
| Contact type (N=14 002) | Household | 3474 (25%) | 464 | 13 (12.3 to 14.5) |
| Community | 10 417 (74%) | 135 | 1 (1.0 to 1.5) | |
| Healthcare personnel | 111 (1%) | 0 | 0 | |
| Symptom status of primary case (N=13 338) | Symptomatic | 607 (5%) | 37 | 6 (4.5 to 8.3) |
| Asymptomatic | 12 731 (95%) | 464 | 4 (3.3 to 4.0) | |
SAR by selected characteristics
Among tested contacts (N: 14 002), 599 (4.3%) tested positive for COVID-19 based on RT-PCR. The overall SAR was 4% (599 of 14 002). The SAR was similar across the age groups and gender, ranging from 4% to 5%. The SAR among the contacts of primary cases with congregation exposure was 5 times higher (10%) than contacts of non-congregation primary cases (2%). Of the 599 contacts who tested positive, more than three-fourths (78%) were household contacts.
The overall SAR was 4%, with 13% among the household contacts compared with 1% among the community contacts. The secondary attack among household contacts of primary cases with exposure to congregation was higher (21%) than the contacts of primary cases without congregation exposure (6%) (table 3). The primary cases’ symptomatic status was available for 95% (13 338) of the tested contacts. The overall secondary attack among contacts of the primary cases with COVID-19 symptoms was 6% compared with 4% among the contacts of asymptomatic cases. The household contacts exposed to the symptomatic primary case had two times higher attack rate as compared with contacts of asymptomatic primary cases (25% vs 12%). Secondary attack among the community contacts was similar irrespective of the symptomatic status of the primary case.
Table 3.
Secondary attack rate among household and non-household contacts of individuals with COVID-19 by type of exposure and symptom status of primary cases, Tamil Nadu, March–May 2020 (N=14 002)
| Type of exposure or symptom status of the primary case | The secondary attack rate (%) (95% CI) (# cases/# contacts of the case) | ||
| Household | Community contacts | Overall | |
| N=14 002 | |||
| Congregation | 21 (19.0 to 22.9) (352/1686) |
1 (0.6 to 1.5) (25/2198) |
10 (8.8 to 10.7) (377/3884) |
| No congregation | 6 (5.2 to 7.5) (112/1788) |
1 (1.0 to 1.6) (110/8330) |
2 (1.9 to 2.5) (222/10118) |
| N=13 338 | |||
| Symptomatic | 25 (17.6 to 34.1) (26/104) |
2 (1.2 to 3.9) (11/503) |
6 (4.5 to 8.3) (37/607) |
| Asymptomatic | 12 (10.5 to 12.9) (341/2930) |
1 (1.0 to 1.5) (123/9801) |
4 (3.3 to 4) (464/12 731) |
Risk factors for secondary cases
We estimated the risk of acquiring infection for contacts by type of contact and congregation participation of the primary cases. There was no significant risk among the community contacts of the primary cases irrespective of the participation in the congregation. The RR of household contacts of primary cases with congregation participation was 4 times higher (RR: 16.4; 95% CI: 13.3 to 20.2) in getting COVID-19 compared with household contacts of other primary cases (RR: 4.9; 95% CI: 3.81 to 6.38). The association did not change even after adjusting for age and gender (table 4).
Table 4.
Factors associated with COVID-19 among the contacts of Tamil Nadu, India, March–May 2020
| Risk factors | Crude RR (95% CI) | RR with age-adjusted (95% CI) | RR with age and sex adjusted (95% CI) |
| Community contacts of non-congregation primary cases | Ref. | Ref. | Ref. |
| Community contact of congregation primary cases | 1.0 (0.7 to 1.5) | 0.9 (0.6 to 1.4) | 0.9 (0.6 to 1.4) |
| Household contacts of non-congregation primary cases | 4.9 (3.8 to 6.4) | 4.7 (3.7 to 6.2) | 4.7 (36.4 to 6.1) |
| Household contacts of congregation primary cases | 16.4 (13.3 to 20.2) | 16.2 (13.1 to 20.0) | 16.1 (13.0 to 20.0) |
RR, relative risk.
We estimated the RR stratified by the symptomatic status of the primary cases. In the strata where the primary case was symptomatic, there was an eightfold increase in RR for household contacts of congregation participants when compared with the household contacts of other cases (RR: 25.3, 95% CI: 10.2 to 63) vs RR: 14.6, 95% CI: 5.7 to 37.7)). If the primary case was asymptomatic, there was no increase in RR for community contacts of congregation participants, but RR was increased among household contacts of primary cases with congregation exposure. The change in RR among household contacts of the symptomatic primary case was several folds higher as compared with household contacts of the asymptomatic primary case (table 5).
Table 5.
Factors associated with COVID-19 among the contacts stratified by the symptomatic status of the primary cases of Tamil Nadu, India, March–May 2020
| Symptomatic primary | Type of contacts | Crude RR (95% CI) | Adjusted RR with age and sex (95% CI) |
| Yes | Community contacts of non-congregation primary cases | Ref. | Ref. |
| Community contact of congregation primary cases | 10.5 (6.0 to 33.0) | 8.6 (2.6 to 29.1) | |
| Household contacts of non-congregation primary cases | 15.5 (6.0 to 39.8) | 14.6 (5.7 to 37.7) | |
| Household contacts of congregation primary cases | 26.7 (10.8 to 65.9) | 25.3 (10.2 to 63.0) | |
| No | Community contacts of non-congregation primary cases | Ref. | Ref. |
| Community contact of congregation primary cases | 0.9 (0.6 to 1.4) | 0.9 (0.5 to 1.3) | |
| Household contacts of non-congregation primary cases | 4.6 (3.5 to 6.0) | 4.4 (3.4 to 5. 8) | |
| Household contacts of congregation Primary cases | 16.48 (13.17 to 20.63) | 16.52 (13.16 to 20.74) |
RR, relative risk.
Discussion
Our study showed an increase in disease transmission among household contacts than community contacts. The transmission was further accentuated if the primary case had symptoms or exposure to a congregation. The high risk of infection among family members was consistent with the pooled analysis of 43 studies, which estimated an SAR of 18% among household contacts.19 Other systematic reviews demonstrated an SAR of 16.6%20 and 27%21 compared with our study. This may probably be due to the timeline of our study in early part of the pandemic. We also observed very low SAR (1%) among non-household contacts, possibly due to the State’s lockdown situation during the study period. Contact tracing is one of the core public health strategies for COVID-19 control, and our study assessed if districts implemented this strategy. Although the median number of contacts per case was 17, there was a high variation between districts due to limiting the contact tracing to only household contacts in several cases. A study in the UK measuring the efficacy of contact tracing for COVID-19 suggested an average of 36 contacts must be traced per case.22 Another study in the Republic of Korea shows a range of 15–649 contacts traced per case.23 Once the number of cases increases, extensive contact tracing may not be feasible unless we deploy dedicated human resources and train the contact tracers. There was a limited capacity in the initial phase of the epidemic; however, the public health department added human resources, especially in the capital city of Chennai, to sustain the contact tracing as cases started increasing.
Initially, testing was done among the individuals reported with symptoms. But due to the clustering of cases among the congregation attendees, all the congregation attendees were tested irrespective of symptom status, as there was lot of panic in the initial phase of the pandemic. It posed high risk of big outbreak. Similarly, all international travellers were tested irrespective of the symptom status. We observed a higher attack rate among household contacts (25%) of symptomatic primary cases when compared with asymptomatic. Our observations were similar to a pooled analysis of three studies from Wei et al,24 Park et al25 and Chaw et al,26 which reported 20% SAR among household contacts of symptomatic primary cases.27 This observation guided the testing policy in the context of limited resources at the peak of the pandemic. We prioritised the testing of household contacts of symptomatic primary cases in the subsequent phases of pandemic at times of resource constraints. Although the attack rate was lower among contacts of asymptomatic primary, the transmission did take place especially in the household setting. Our findings support the rationale of isolation of all cases irrespective of the symptoms and testing of all household contacts to break the chain of transmission.28
At the time when this investigation was undertaken, there was no widespread community transmission. Most of the infection was among international travellers and healthcare workers, and they were separated from the community, due to isolation and quarantine protocols. Unlike international travellers, congregation participants travelled with local people. After attending the congregation, all resumed their routine work and social activities after arrival. This posed threat to transmit to diseases in the community, as the congregation occurred before the lockdown.
The congregation clusters were one of the sources, which led to COVID-19 transmission in various communities.29 Similar to our setting, many countries experienced clusters emerging from congregation settings. In South Korea, an explosive outbreak happened following a social event held at a church and is attributable to 84% of the total confirmed cases of South Korea reported till mid-March.30 Another study in Jordan among the wedding attendees reported a higher attack rate of 22%.31 Similar clusters had been reported in different parts of South Korea,32 and in the USA, a secondary attack of 53.3% was estimated among one such event attendees.33 In addition to the effect of disease spread within the cluster, the attendees returned from the congregation involved themselves in the routine duties and social activities, which led to further spread of the disease in the community. Avoiding any type of gathering is one of the essential mitigation measures to be followed strictly. Ban on mass gatherings by the health department are one of the important intervention in addition to good diagnostic facilities and remotely accesses health advice, together with specialised treatment for people with severe disease.34
Our study has several limitations. We did not have confirmation of the COVID-19 status of 11% of the contacts, who were mostly community contacts. Hence, this may have overestimated the overall SAR by 0.3%. Contact tracing was prioritised for household contacts due to restricted mobility and limited interactions at the community level. Therefore, secondary attack among non-household contacts may not reflect the real transmission potential. Information regarding symptoms was retrieved from district surveillance records. The symptom status was collected at the time of diagnosis. We could not verify if the primary case developed symptoms later in the course of illness. Hence, there was a chance of misclassification of symptom status. We abstracted the information from the records of the district surveillance units. The information on the date of exposure and the date of sample taken are not available for all the contacts. Hence, we could not calculate the time taken for the contacts to be tested from the date of contact.
We conclude that COVID-19 transmission was higher among household contacts, contacts of symptomatic primary case and contacts of primary cases exposed to the congregation. Based on the findings, we informed the testing policy and contact tracing strategy in the early stages of the COVID-19 epidemic in Tamil Nadu. We recommend testing all household contacts irrespective of the symptoms and extensive contact tracing and testing in case of super spreader events. In resource-constrained settings, all contacts of symptomatic primary cases should be prioritised for testing. The gatherings should be restricted to prevent significant clusters.
Supplementary Material
Footnotes
Twitter: @drrubesh, @drKumaravel
Contributors: KK, MRaju, MP and PK designed the study, supervised fieldwork, did primary data collection, planned data analysis and wrote the first draft of the manuscript. VV, PR, MSakthivel, PS, PG and SKM did primary data collection and did data analysis. MSendhilkumar, VV, IS and KI supervised fieldwork and data management. JM, RG, SS, SR, KSTS, MV, MT, KJ, VG and SK supervised fieldwork and supported data collection. PV, YN, SP, TSS, MReddy, BR and MVM conceptualised the study and gave critical comments in finalising the manuscript. All authors approved the final manuscript. MRaju takes responsibility for the integrity of the data and the accuracy of the data analysis. MRaju is responsible for the overall content as guarantor.
Funding: This work was supported by ICMR-National Institute of Chennai intramural funds.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Institutional Ethics Committee of ICMR-National Institute of Epidemiology, Chennai, approved the study. Written consent was not required for this study.
References
- 1.World Health Organization . Statement on the second meeting of the International health regulations (2005) emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV), 2020. Available: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
- 2.WHO . Coronavirus disease (COVID-19): contact tracing, 2020. Available: https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-contact-tracing
- 3.Halloran ME. Secondary attack rate. In: Peter A, Theodore C, eds. Encyclopedia of biostatistics. New York: John Wiley & Sons Ltd, 2005. [Google Scholar]
- 4.Li W, Zhang B, Lu J, et al. Characteristics of household transmission of COVID-19. Clin Infect Dis 2020;71:1943–6. 10.1093/cid/ciaa450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu Y, Eggo RM, Kucharski AJ. Secondary attack rate and superspreading events for SARS-CoV-2. Lancet 2020;395:e47. 10.1016/S0140-6736(20)30462-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luo L, Liu D, Liao X, et al. Contact settings and risk for transmission in 3410 close contacts of patients with COVID-19 in Guangzhou, China : A prospective cohort study. Ann Intern Med 2020;173:879–87. 10.7326/M20-2671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis 2020;94:91–5. 10.1016/j.ijid.2020.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng HY, Jian SW, Liu DP. High transmissibility of COVID-19 near symptom onset. medRxiv 2020. [Google Scholar]
- 9.Wilder-Smith A, Chiew CJ, Lee VJ. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect Dis 2020;20:e102–7. 10.1016/S1473-3099(20)30129-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jahan N, Rubeshkumar P, Karuppiah M, et al. Entry and initial spread of COVID-19 in India: epidemiological analysis of media surveillance data, India, 2020. Clin Epidemiol Glob Health 2021;9:347–54. 10.1016/j.cegh.2020.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.State Control Room, Directorate of Public Health and Preventive Medicine Health and Family Welfare Department, Government of Tamil Nadu . Available: https://stopcorona.tn.gov.in/wp-content/uploads/files/MediaBulletin180320COVID19.pdf
- 12.Ali A. Coronavirus was a test of secular nationalism. Then Tablighi Jamaat became the scapegoat. The Print., 2020. Available: https://theprint.in/opinion/coronavirus‐test‐of‐secular‐nationalism‐tablighi‐jamaat‐became‐scapegoat/392764/
- 13.The Hindu . Gathering at Nizamuddin a highly Irresponsible act, says Kejriwal, 2020. Available: https://www.thehindu.com/news/cities/Delhi/gathering‐at‐nizamuddin‐a‐highly‐irresponsible‐act‐says‐kejriwal/article31221982.ece
- 14.Chandna H. 30% of India’s Covid‐19 positive caseload linked to Tablighi Jamaat meet, says govt. The Print, 2020. Available: https://theprint.in/health/30‐of‐indias‐covid‐19‐positive‐caseload‐linked‐to‐tablighi‐jamaat‐meet‐says‐govt/404426/
- 15.India Today . Of 14,378 total Covid‐19 cases in India, 4,291 linked to Delhi’s Markaz event: Health ministry, 2020. Available: https://www.indiatoday.in/india/story/coronavirus‐india‐total‐cases‐linked‐tablighi‐jamaat‐markaz‐nizamuddin‐event‐health‐ministry‐1668456‐2020‐04‐18
- 16.NDTV . 1,023 COVID-19 cases linked to Mosque event, Tamil Nadu leads: 10 points: NDTV. Available: https://www.ndtv.com/india-news/coronavirus-tablighi-jamaat-1-023-of-2-902-covid-19-cases-linked-to-mosque-event-tamil-nadu-leads-2206193
- 17.National Centre for Disease Control Directorate General of Health Services MoH . FW, GOI, New Delhi The updated case definitions and contact-categorisation. Available: https://nirth.res.in/virology/Revised_case_definitions_for_COVID_19.pdf
- 18.Guidelines for investigating clusters of health events. MMWR Recomm Rep 1990;39:1–23. [PubMed] [Google Scholar]
- 19.Koh WC, Naing L, Chaw L, et al. What do we know about SARS-CoV-2 transmission? A systematic review and meta-analysis of the secondary attack rate and associated risk factors. PLoS One 2020;15:e0240205. 10.1371/journal.pone.0240205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Madewell ZJ, Yang Y, Longini IM, et al. Household transmission of SARS-CoV-2: a systematic review and meta-analysis. JAMA Netw Open 2020;3:e2031756. 10.1001/jamanetworkopen.2020.31756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lei H, Xu X, Xiao S, et al. Household transmission of COVID-19-a systematic review and meta-analysis. J Infect 2020;81:979–97. 10.1016/j.jinf.2020.08.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keeling MJ, Hollingsworth TD, Read JM. The efficacy of contact tracing for the containment of the 2019 novel coronavirus (COVID-19). MedRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.COVID-19 National Emergency Response Center, Epidemiology and Case Management Team, Korea Centers for Disease Control and Prevention . Coronavirus Disease-19: summary of 2,370 contact investigations of the first 30 cases in the Republic of Korea. Osong Public Health Res Perspect 2020;11:81–4. 10.24171/j.phrp.2020.11.2.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wei L, Lv Q, Wen Y. Household transmission of COVID-19, Shenzhen, January-February 2020. medRxiv 2020. [Google Scholar]
- 25.Park SY, Kim Y-M, Yi S, et al. Coronavirus disease outbreak in call center, South Korea. Emerg Infect Dis 2020;26:1666–70. 10.3201/eid2608.201274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chaw L, Koh WC, Jamaludin SA, et al. Analysis of SARS-CoV-2 transmission in different settings, Brunei. Emerg Infect Dis 2020;26:2598–606. 10.3201/eid2611.202263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Koh WC, Naing L, Chaw L, et al. What do we know about SARS-CoV-2 transmission? A systematic review and meta-analysis of the secondary attack rate and associated risk factors. PLoS One 2020;15:e0240205. 10.1371/journal.pone.0240205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.MOHFW . Revised guidelines for home isolation of very mild/pre-symptomatic/asymptomatic COVID-19 cases 2020.
- 29.Quadri SA. COVID-19 and religious congregations: implications for spread of novel pathogens. Int J Infect Dis 2020;96:219–21. 10.1016/j.ijid.2020.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Choi JY. COVID-19 in South Korea. Postgrad Med J 2020;96:399–402. 10.1136/postgradmedj-2020-137738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yusef D, Hayajneh W, Awad S, et al. Large outbreak of coronavirus disease among wedding attendees, Jordan. Emerg Infect Dis 2020;26:2165–7. 10.3201/eid2609.201469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shim E, Tariq A, Choi W, et al. Transmission potential and severity of COVID-19 in South Korea. Int J Infect Dis 2020;93:339–44. 10.1016/j.ijid.2020.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hamner L, Dubbel P, Capron I, et al. High SARS-CoV-2 Attack Rate Following Exposure at a Choir Practice - Skagit County, Washington, March 2020. MMWR Morb Mortal Wkly Rep 2020;69:606–10. 10.15585/mmwr.mm6919e6 [DOI] [PubMed] [Google Scholar]
- 34.The times of India; avoid mass gatherings, says govt as corona cases hit 31. Available: http://timesofindia.indiatimes.com/articleshow/74520610.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request.