Abstract
Purpose:
Surgeons now have a variety of treatment options for Dupuytren’s contracture including traditional partial fasciectomy (PF), percutaneous needle aponeurotomy (PNA), and collagenase Clostridium histolyticum (CCH) injection. An important factor in clinical decision making is the cost-effectiveness of the various modalities, as will be discussed in this article.
Methods:
A literature search was performed by 2 independent reviewers. A total of 14 articles and 3 abstracts met inclusion criteria. Papers were excluded for non-English language, insufficient breakdown of costs by treatment type, promotional materials, or works-in-progress. Cost data were extracted and subsequently converted to US dollars. Weighted means were used to objectively pool data that were sufficiently similar in methodology and population.
Results:
Seven observational cohort studies were pooled and found to have a weighted mean cost in favour of PNA at US$3335 per patient as compared to CCH at US$3673.14 and PF at US$4734.14. Two expected-value decision analysis models were in agreement that PF is not cost-effective, but they differed on whether PNA or CCH was the most cost-effective strategy. Two cost minimization studies agreed that CCH was less costly than PF by US$486. One cost–benefit analysis found no significant cost benefit to CCH or PF, but found significant indirect benefit to CCH. Overall 10 of 17 studies found CCH to be superior with respect to direct cost, indirect cost, or both. Only 2 of the 17 studies found PF to be the most cost-effective method. Of the 7 studies that considered PNA, 4 found it to be lowest cost.
Conclusion:
The vast majority of studies found PF to be the most costly treatment modality; however, it is still the treatment of choice in certain clinical scenarios. It is difficult to compare CCH to PNA, as many studies did not consider PNA. More studies, especially considering indirect costs, are required to be able to accurately determine which method is most cost-effective.
Keywords: Dupuytren’s contracture, economic analysis, fasciectomy, percutaneous needle aponeurotomy, collagenase Clostridium histolyticum
Abstract
Objectif :
Les chirurgiens possèdent désormais diverses options pour traiter la maladie de Dupuytren, y compris la fasciectomie partielle (FP) classique, l’aponévrotomie percutanée à l’aiguille (APA) et l’injection de collagénase issue du Clostridium histolyticum (CCH). Le rapport coût-efficacité des diverses modalités est un facteur important de la prise de décision clinique, comme on le verra dans le présent article.
Méthodologie :
Deux analystes indépendants ont procédé à une analyse bibliographique. Au total, 14 articles et trois résumés respectaient les critères d’inclusion. Les articles qui n’étaient pas rédigés en anglais, dont la ventilation des coûts par type de traitement était insuffisante, qui contenaient du matériel promotionnel ou qui rendaient compte de travaux en cours étaient exclus. Les chercheurs ont extrait les données sur les coûts et les ont converties en dollars américains. Ils ont utilisé les moyennes pondérées pour regrouper objectivement les données dont la méthodologie et la population étaient suffisamment semblables.
Résultats :
Les chercheurs ont regroupé quatre études de cohorte observationnelles et ont constaté que le coût moyen pondéré de l’APA, à 3 335 $ par patient, était plus favorable que celui de la CCH, à 3 673,14 $ et de la FP, à 4 734,14 $. Trois modèles d’analyse décisionnelle de la valeur attendue concluaient que la FP n’était pas rentable, mais divergeaient sur le coût de l’APA et de la CCH. Deux études de minimisation des coûts ont convenu que la CCH coûtait 486 $ de moins que la FP. Une analyse coût-bénéfice n’a pas établi de coûts-avantages significatifs pour la CCH ou la FP, mais a constaté des avantages indirects significatifs pour la CCH. Bref, selon 11 des 17 études, la CCH était supérieure sur le plan des coûts directs, des coûts indirects ou de ces deux coûts. Seulement deux des 17 études ont indiqué que la FP était la plus rentable. Sur les sept études qui évaluaient l’APA, quatre ont indiqué qu’il s’agissait de la moins coûteuse.
Conclusion :
La grande majorité des études ont établi que la FP était le traitement le plus coûteux, mais elle demeure à privilégier dans certains scénarios cliniques. Il est difficile de comparer la CCH à l’APA, car de nombreuses études n’évaluaient pas l’APA. Il faudra mener plus d’études, notamment sur les coûts indirects, pour déterminer la méthode qui est vraiment la plus rentable.
Introduction
Dupuytren’s contracture is a progressive disease of the palmar fascia causing debilitating flexion contractures at the metacarpophalangeal and interphalangeal joints. 1 Surgical management of this entity has been the mainstay of treatment for many years, including open fasciotomy, partial (or limited) fasciectomy (PF), radical fasciectomy, and dermofasciectomy with or without skin grafting. 1 Recently there has been an emergence of less invasive options. Three of the most commonly used procedures today are traditional PF, percutaneous needle aponeurotomy (PNA), and collagenase Clostridium histolyticum (CCH) injection. 2 There is emerging data and ongoing trials comparing safety and efficacy of these treatment options. Another important factor in clinical decision making is the cost-effectiveness of the various modalities. This article will review the available literature comparing costs of PF, PNA, and CCH. A secondary objective is to explore the patient and disease characteristics that are more amenable to each therapeutic procedure.
Methods
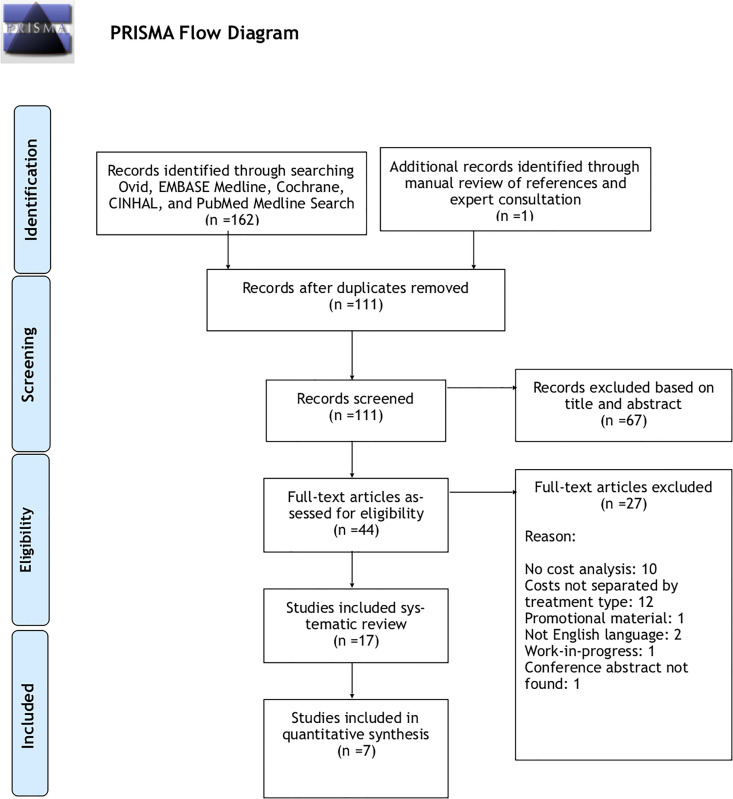
This study was registered with PROSPERO (review protocol available at http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42014015190). PRISMA guidelines were utilized and adhered to throughout the study. A literature search was performed, by 2 independent reviewers, using Cochrane, OVID Medline, EMBASE, CINAHL, and PubMed databases, as well as a manual review of references. The time frame chosen was 2000 until present, given the more recent reintroduction of PNA and development of CCH. See Table 1 for a sample search strategy. A total of 14 articles and 3 abstracts met inclusion criteria, from an initial 162. Papers were excluded for non-English transcript, absent or insufficient breakdown of costs by treatment type, promotional materials, or work-in-progress. See Figure 1 for search strategy flow diagram and full inclusion and exclusion criteria. Kappa value of 0.94 was achieved, indicating excellent agreement between reviewers. Discrepancies were resolved by discussion with senior authors. Each paper was scored using the MINORS criteria for non-randomized studies, with an average score of 17.6 (1.2) of a possible 24. 3 Cost data were extracted and subsequently converted to US Dollars (USD) to allow for direct comparisons and pooling of data. Daily exchange rates were extracted from Bloomberg financial news and data source. The conversion rate chosen was determined by the date the manuscript was received by the publishing journal. This date was selected in order to have the most accurate temporally related conversion rate to the time the costs were actually collected. A weighted mean was used to objectively pool data that were sufficiently similar in methodology and population. Standard deviations were reported where possible.
Table 1.
Sample Search Strategy for OVID Medline.
|
Figure 1.
PRISMA flow diagram. From: Moher D, et al. 15
Results
A summary of the characteristics and findings of all studies in this review can be found in Table 2. Pooled data from each subset of study design will be analysed in further detail below.
Table 2.
Summary of Results of Systematic Review.
| n | Design | MINORS score | Currency | Cost types | PF cost (USD) | CCH cost (USD) | PNA cost (USD) | Patient population | Cost description | Additional information | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mehta & Belcher (2014) 6 | 40 | Prospective cohort | 19 | Great British Pounds | Direct | 11 361 | 3370 | N/A | Average age 69; Single digit affected, 29 male, 11 female | Initial consult, 60 minutes OR time, day surgery unit, no overnight stay, 1 surgeon FU, 1 PT FU | No PT or FU for CCH patients therefore may have overestimated the cost savings of CCH. |
| Atroshi et al (2014) 7 | 32 | Retrospective cohort | 18 | Swedish Kronor | Direct | 2103 | 1675 | N/A | Age > 65 years and retired | Initial consult, day surgery OR, GA, or axillary block, same day surgery, 2+ nurse FU visits, 1+ hand therapist FU, 1 surgeon FU | CCH costs assuming 20% of patients required 2 injections. All costs calculated based on average salary of care providers. |
| Cervero et al (2013) 8 | 91 | Retrospective observational | 17 | Euros | Direct | 2183 | 1258 | N/A | Average age 65, primarily male, 1 or 2 digits affected | Initial consult, preoperative workup if age > 60, preanaesthesia visit, minor or major ambulatory surgery, 9 overnight admissions, surgeon FU, rehab | Significant learning curve of the CCH injections. Values estimated from bar chart using average of highest and lowest costs. |
| Herrera et al (2013) 9 | 48 | Retrospective observational | 19 | US Dollars | Direct | 11 240 | N/A | 4658 | PF: mean 60 years, multiple digits, primarily male. CCH: mean 65 years, primarily male | Initial consults, surgical fees, anaesthesia, facility fees, but no PT costs considered | Highest treatment costs for all interventions, likely due to local health-care costs. No PT costs considered. |
| Gerber et al (2011) 10 | 64506 | Retrospective observational | 18 | Great British Pounds | Direct | 4717 | N/A | 1982 | Average age 65, primarily male | Admission and day surgery costs only. No outpatient, FU or PT costs captured. | “Division of palmar fascia” included as PNA cost. No outpatient costs for any treatment. |
| Baltzer & Binhammer (2013) 13 | N/A | Expected value decision analysis model | N/A | Canadian dollars | Direct and indirect | 7998 | 6461 | 4002 | Assumed age of presentation 63 years with 15 year time horizon, single digit treated | Facility, anaesthetic, FU, allied health, PT, equipment, treatment of potential complications, lost productivity, parking, lost income | Direct and indirect costs from societal perspective. CCH most cost effective if drug costs drop to 470. |
| Chen et al (2011) 12 | N/A | Expected value decision analysis model | N/A | US Dollars | Direct | 820 114 | 51 431 | 96 474 | Assumed age of presentation 63 years with 20 year time horizon | Surgical, facility, splinting, rehab (36 visits) | Complications included in model. Included OR/anaesthesia costs for PNA. No PT included for CCH. |
| De Salsa-Cansado et al (2013) 14 | N/A | Cost minimization analysis | N/A | Euros | Direct | 2163 | 1550 | N/A | Not specified | Initial consult, surgery, 72% inpatient stay (mean 1.5 day), investigations (mean 4.9), FU visits (mean 4.9), rehab (27% had an average of 6.6 sessions) | Costs obtained from combination of 123 patient retrospective observational study and from the literature of typical CCH use and efficacy. Sponsored by Pfizer. |
| Inês et al (2011) 15 | N/A | Cost minimization analysis | N/A | Euros | Direct | 3181 | 2822 | N/A | Not specified | Surgery, inpatient stay, outpatient FU, PT. Indirect costs estimated by human capital method. | Conference abstract—no additional data available. |
| Brazzelli et al (2015) 18 | N/A | Markov decision analysis | N/A | Great British Pounds | Direct | 3702 | 8207 | 1862 | Average age 63, 84% male, moderate to severe disease. 37 year time horizon. | Surgery, inpatient stay, anaesthetic, FU, PT, splints, complications, treatment in case of recurrence. | PNA least costly, but PF most cost-effective. CCH less effective and more costly. |
| Malone & Armstrong (2012) 17 | N/A | Markov decision analysis | N/A | US Dollars | Direct | 18 345 | 4489 | 14 970 | Not specified. 30 year time horizon | Not described | Conference abstract—no additional data available. |
| Sau et al (2011) 19 | N/A | Markov decision analysis | N/A | US Dollars | Direct | x | x+1844 | x+247 | Not Specified. 10 year time horizon | Not described | Conference abstract—no additional data available. |
| Syed et al (2014) 5 | 56 | Prospective Cohort | 16 | Great British Pounds | Direct | 5177 | 2167.00 | N/A | Average age 65, primarily male, baseline contracture 41.8° | Based on UK’s National Health Services’ Payment by Results | Assumes equal recurrence rate in cost calculations (savings greater if CCH more effective). |
| Donga et al (2015) 4 | PF = 1264, CCH = 309 | Retrospective Cohort | 16 | US Dollars | Direct | 5408 | 4844.00 | N/A | Average age CCH = 64.28, Average age PF = 61.50, both groups primarily male | Lab/pathology tests, surgery and anaesthesia, ancillary services (PT/OT), pharmacy | Smaller CCH population was possible due to recent adoption of CCH in United States. CCH patients were significantly older. |
| Wagner et al (2014) 16 | N/A | Markov Decision Analysis | N/A | Canadian Dollars | Direct and Indirect | direct: 2842-2972; indirect: 2328 | direct: 1104-3311; indirect: 155 | N/A | Not specified. 5 year time horizon. | Direct treatment, complications and work days lost | Savings of US$3035 to US$3119 direct and US$535 to US$931 indirect with CCH compared to PF. Price ranges are based on number of joints affected, between 1and 3. |
| Leskela et al (2016) 20 | N/a | Cost–benefit analysis | N/A | Euros | Direct and indirect | 2641-3246 | 2450-3375 | N/A | Not specified | Based on EMR and OR management systems from 7 Finnish hospitals. Includes pre/post visits, procedure, physical therapy, medications. Indirect consideration of time for surgeon, nurse and PT. | Accounts for reinjection consults and visits with CCH. Finds no significant direct cost benefit, but a significant indirect benefit of less than half the time for CCH (5:56-8:00 minutes for CCH vs 16:52-19:22 minutes for PF). |
| Povlsen et al (2014) 11 | 20 | Prospective cohort | 18 | N/A | Indirect | N/A | N/A | N/A | Average age 65, primarily male | Time of preoperative preparation, anaesthesia, theatre, recovery, and postoperative ward in minutes. Total time in minutes was 194.3 for CCH and 1009.2 for PF. | Found CCH significantly better in time in theatre, follow-up, healing, and return to normal activities. |
Abbreviations: CCH, Clostridium histolyticum; EMR, electronic medical record; FU, follow-up; GA, general anesthetic; N/A, not applicable; OT, occupational therapy; OR, operating room; PF, partial fasciectomy; PNA, percutaneous needle aponeurotomy; PT, physiotherapy; rehab, rehabilitation.
Observational Cohort
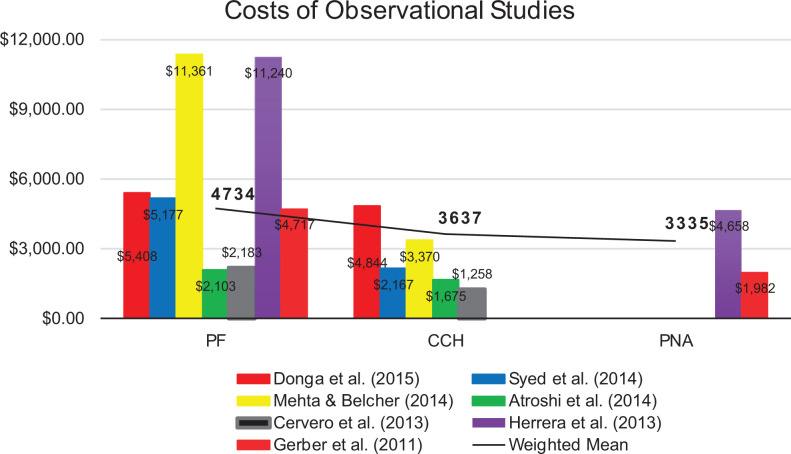
Seven observational cohort studies were pooled and found to have a weighted mean cost in favour of PNA and CCH over PF by approximately US$1400 and US$1100 respectively. (Figure 2). 4 -10 Unfortunately, only 2 of these studies considered PNA, so a robust comparison cannot be made between PNA and CCH. 9,10 In a sensitivity analysis by Atroshi et al, it is worth noting that, if 50% of patients require more than one injection, then the costs tip in favour of PF. 7
Figure 2.
Costs of observational studies.
There was an eighth observational study by Povlsen et al, 11 which was not included in the quantitative analysis because it considered indirect costs only. Of note, this study found CCH to require significantly less time in the operating room and follow-up, and to result in significantly earlier healing and return to daily activities. 11
Expected-Value Decision Analysis
Two expected-value decision analysis models were in agreement that PF is not cost-effective, but they differed on whether PNA or CCH was the most cost-effective strategy. Chen et al found CCH to be most cost-effective, but did not meet the generally accepted willingness to pay cut-off of US$50 000/quality-adjusted life-year (QALY). 12 In the sensitivity analysis, they did determine that CCH would meet this cut-off if the price dropped to US$945. A potential biasing factor was that CCH did not include splinting and hand therapy afterward, whereas PF and PNA were estimated to need 36 visits. Additionally, anaesthesia and OR costs were included for PNA, however PNA is often performed in the office setting, thus likely overestimating the costs. 12
Baltzer and Binhammer take into account both direct and indirect costs. 13 Percutaneous needle aponeurotomy was found to be most cost-effective at US$3990 per patient. Clostridium histolyticum was found to be second most effective at US$6442, but the sensitivity analysis did show that if the market value of collagenase dropped to US$470 (from estimate of US$3000 at the time) that it then would become the most cost-effective treatment option. Further, at US$875 per round of treatment, CCH met the generally accepted willingness to pay cut-off of US$50 000/QALY. 13
Cost Minimization Study
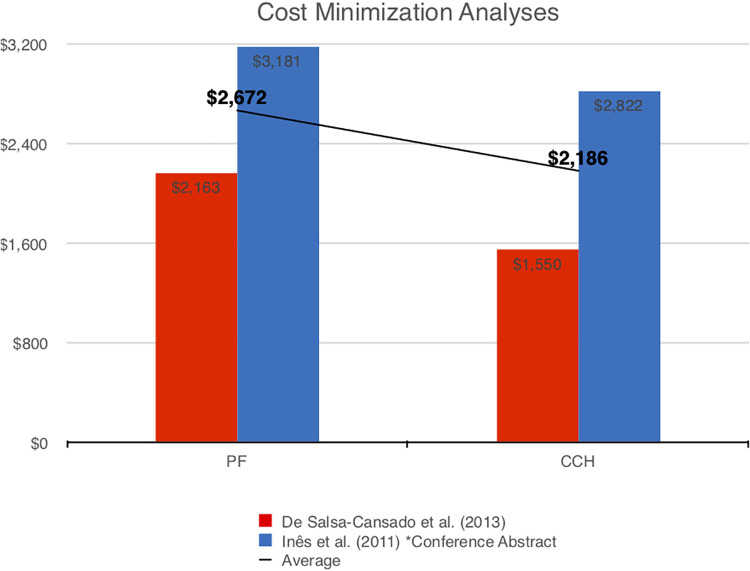
Two cost minimization studies agreed that CCH was less costly than PF by US$486 (Figure 3). De Salsa-Cansado et al stated that PNA would be the least expensive option but that it wasn’t included in the analysis as it is not the gold standard for treatment and not widely used in Spain. 14 Inês et al also included an indirect cost analysis which demonstrated increased savings of CCH from US$359 to US$1892. This was a conference abstract, therefore a critical appraisal of the study was not possible. 16
Figure 3.
Comparison of means of minimization studies.
Markov Decision Analysis
Wagner et al is the only study in this series to consider direct cost of treatment as well as indirect cost of complications and work days lost. 17 Clostridium histolyticum was found to be superior to PF with direct savings of US$3035 to US$3119 and indirect savings of US$535 to US$931. 17
Malone and Armstrong found CCH significantly more cost-effective than PF or PNA. 18 This study reported data per QALY, and of note, all of the treatment options were significantly below the US$50 000 willingness-to-pay cut-off. 18 Brazzelli et al similarly measured cost per QALY, but found that while PNA was the least costly treatment modality, PF was more cost-effective due to greater interventional success. Interestingly, this study found CCH to be least cost-effective. 19 Sau et al also found PF to be the most cost-effective. 20 No specific value was reported; instead CCH and PNA were reported as incremental costs above PF. This outlier could either represent a publication bias against PF or issues with the methodology of the study preventing final publication. Since a full text article is unavailable for review, it is impossible to determine which is the case. 20
Cost–Benefit Analysis
Leskela et al considered both direct and indirect costs in their cost–benefit analysis. 21 At US$2641 to US$3246 for PF and US$2450 to US$3375 for CCH, there was no significant financial benefit to either treatment. However, CCH was found to be of greater benefit overall, as it required less than half the time investment of PF (5:56-8:00 minutes vs 16:52-19:22 minutes). 21
Discussion
The study objective, to determine the most cost-effective treatment for Dupuytren’s, was limited by the literature available for review. The majority of papers were small, retrospective observational studies. Additionally, the heterogeneity of study design and nature of costs captured limited the quantitative pooling and comparison of data. Finally, few of the papers (7 of 17) included PNA as a treatment option. This makes direct comparison between PNA and CCH very difficult.
Despite these limitations, there are a number of insights to be gained. The majority of studies (14 of 17) found PF to be the most costly procedure. Only 2 studies reported PF as the most cost-effective method using a Markov decision analysis design. 19,20 There is significant evidence that PF is not the most cost-effective strategy for uncomplicated, first presentation, single digit disease. However, there are still a number of patient and disease factors in which PF is still widely considered the first-line treatment. For example, advanced presentation, recurrent disease with multiple previous operative procedures, multiple digits affected simultaneously, or anticipated requirement for access to the volar plate, may all benefit from open operative management.
This leaves minimally invasive approaches as the most cost-efficient first-line treatment. However, given the results of this study, it is still unclear whether PNA or CCH is the most cost-effective modality. As mentioned above, many of the studies did not include PNA as a treatment option. Overall, 10 of 17 studies found CCH to be least costly. However, of the studies considering PNA, 4 of 7 found PNA to be lowest cost or cost-effective. These finding should be interpreted with caution due to the inherent biases applied to observational designs. Although a definitive comparison between the 2 cannot be made, many of the studies’ sensitivity analyses agree that for CCH to be cost-effective, the drug price would need to decrease.
This review provides insight into the economic considerations of various treatment options for Dupuytren’s contracture, however, more studies are required to definitively determine which method is most cost-effective. In particular, studies that consider indirect costs, while comparing PNA and CCH, will add value to the current body of literature. There are a variety of ongoing studies investigating safety and efficacy of CCH; ideally these will include a cost-effectiveness component in the analysis.
Footnotes
Authors’ Note: This project did not require ethics approval as it does not involve patient contact. No consent was obtained or required. This project has not been previously presented or published.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Maleka Ramji, MD https://orcid.org/0000-0001-9033-4132
References
- 1. Rayan GM. Dupuytren disease: anatomy, pathology, presentation, and treatment. J Bone Joint Surg. 2007;89(1):189–198. [DOI] [PubMed] [Google Scholar]
- 2. Desai SS, Hentz VR. The treatment of Dupuytren disease. J Hand Surg. 2011;36(5):936–942. [DOI] [PubMed] [Google Scholar]
- 3. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 4. Donga P, DeKoven M, Kaplan FT, Tursi JP, Lee EC. Costs of collagenase Clostridium histolyticum and fasciectomy for Dupuytren’s contracture. Am J Pharm Ben. 2015;7(1):24–31. [Google Scholar]
- 5. Syed AM, Mcfarlane J, Chester T, Powers D, Sibly F, Talbot-Smith A. Clinical efficacy and cost-effectiveness of Clostridium histolyticum collagenase injections in a subpopulation of Dupuytren’s contracture patients. Eur Orthop Traumatol. 2014;5:311–316. [Google Scholar]
- 6. Mehta S, Belcher H. A single-centre cost comparison analysis of collagenase injection versus surgical fasciectomy for Dupuytren’s contracture of the hand. J Plast Reconstr Aesthet Surg. 2014;67(3):368–372. [DOI] [PubMed] [Google Scholar]
- 7. Atroshi I, Strandberg E, Lauritzson A, Ahlgren E, Waldén M. Costs for collagenase injections compared with fasciectomy in the treatment of Dupuytren’s contracture: a retrospective cohort study. BMJ Open. 2014;4(1):e004166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cerveró RS, Ferrando NF, Jornet JP. Use of resources and costs associated with the treatment of Dupuytren’s contracture at an orthopedics and traumatology surgery department in Denia (Spain): collagenase Clostridium hystolyticum versus subtotal fasciectomy. BMC Musculoskelet Disord. 2013;14(1):293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Herrera FA, Benhaim P, Suliman A, Roostaeian J, Azari K, Mitchell S. Cost comparison of open fasciectomy versus percutaneous needle aponeurotomy for treatment of Dupuytren contracture. Ann Plast Surg. 2013;70(4):454–456. [DOI] [PubMed] [Google Scholar]
- 10. Gerber RA, Perry R, Thompson R, Bainbridge C. Dupuytren’s contracture: a retrospective database analysis to assess clinical management and costs in England. BMC Musculoskelet Disord. 2011;12(1):73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Povlsen B, Shields AM, Bhabra GS. Resource utilisation associated with single digit Dupuytren’s contracture treated with either surgery or injection of collagenase Clostridium histolyticum. Hand Surg. 2014;19(2):205–209. [DOI] [PubMed] [Google Scholar]
- 12. Chen NC, Shauver MJ, Chung KC. Cost-effectiveness of open partial fasciectomy, needle aponeurotomy, and collagenase injection for Dupuytren contracture. J Hand Surg. 2011;36(11):1826–1834. [DOI] [PubMed] [Google Scholar]
- 13. Baltzer H, Binhammer PA. Cost-effectiveness in the management of Dupuytren’s contracture. A Canadian cost-utility analysis of current and future management strategies. Bone Joint J. 2013;95(8):1094–1100. [DOI] [PubMed] [Google Scholar]
- 14. De Salas-Cansado M, Cuadros M, Del Cerro M, Arandes JM. Budget impact analysis in Spanish patients with Dupuytren’s contracture: fasciectomy vs. collagenase Clostridium histolyticum. Chir Main. 2013;32(2):68–73. [DOI] [PubMed] [Google Scholar]
- 15. Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group . Preferred Reporting Items for Systematic Reviews and Meta-Analysis: The PRISMA Statement. PLoS Med. (2009);6(6):e1000097. doi:10.1371/journal.pmed1000097. [PMC free article] [PubMed] [Google Scholar]
- 16. Ines M, Silverio NM, Erdogan-Ciftci E. PMS43 Cost-minimization analysis of collagenase Clostridium histolyticum compared with fasciectomy in patients with Dupuytren’s contracture in Portugal. Value Health. 2011;14(7): A310. [Google Scholar]
- 17. Wagner M, Lavoie L, Hensen M, Postema R, Welner S. Economic evaluation of collagenase Clostridium histolyticum injection for the treatment of Dupuytren’s contracture in Canada. J Popul There Clin Pharmacol. 2014;1(1):e126. [Google Scholar]
- 18. Malone DC, Armstrong EP. PMS29 Cost-effectiveness of collagenase Clostridium histolyticum, limited fasciectomy, and percutaneous needle fasciotomy in the treatment of Dupuytren’s contracture. Value Health. 2012;15(4):A38–A39. [Google Scholar]
- 19. Brazzelli M, Cruickshank M, Tassie E, et al. Collagenase Clostridium histolyticum for the treatment of Dupuytren’s contracture: systematic review and economic evaluation. Health Technol Assess. 2015;19(90):1–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sau C, Bounthavong M, Tran JN, Wilson RL. PMS29 Cost-utility analysis of collagenase Clostridium histolyticum, limited fasciectomy, and percutaneous needle fasciotomy in Dupuytren’s contracture. Value Health. 2011;14(3):A128. [Google Scholar]
- 21. Leskela RL, Herse F, Torkki P, Laine J, Vilkuna T, Raatikainen T. Analysis of the adoption of new health technology: the case of Dupuytren’s disease. Int J Healthc Technol Manag. 2016;15(3):210–227. [Google Scholar]