Abstract
Study Objectives
High rates of sleep and mental health problems have been reported during the COVID-19 pandemic, but most of the evidence is retrospective without pre-pandemic data. This study documented rates of prevalent, incident, and persistent insomnia and psychological symptoms during the COVID-19 pandemic (2020) compared to pre-pandemic data (2018).
Methods
Data were derived from a longitudinal, population-based study of insomnia in Canada. When the first lockdown started in the province of Quebec, a subsample of participants who had completed the latest 2018 follow-up were surveyed (April to May 2020) about their sleep, insomnia, and psychological symptoms since the beginning of the pandemic. Prevalence, incidence, and persistence rates of insomnia, and severity of stress, anxiety, and depressive symptoms were estimated, as well as their associations with confinement, loneliness, social support, use of electronics, and other lifestyle changes occurring during the pandemic. A sleep/health survey and validated questionnaires of insomnia, sleep quality, stress, fatigue, anxiety, and depression were administered at both assessments.
Results
The sample consisted of 594 adults (mean age: 48.3 ± 13.1 years; 64.0% women). Prevalence of insomnia increased from 25.4% to 32.2% (symptoms) and from 16.8% to 19% (syndrome) from 2018 to 2020, for an overall 26.7% increase in insomnia rates. Of those classified as good sleepers in 2018 (n = 343), 32.6% (n = 112) had developed new insomnia during the COVID-19 pandemic. Among participants who had insomnia in 2018, the persistence rate was 76.5% 2 years later. There was a significant worsening of sleep quality, fatigue, anxiety, and depression (all ps < .005) during the COVID-19 pandemic compared to 2018. Significant associations were found between sleep and psychological symptoms and with living alone and being in confinement, lower social support, increased time using electronic devices, reduced physical exercise, and higher financial stress.
Conclusions
The COVID-19 pandemic is associated with significant increases in insomnia and psychological symptoms compared to the pre-pandemic period. Large scale public sleep and mental health intervention programs should be prioritized during and after a pandemic such as the COVID-19.
Keywords: insomnia, sleep, psychological symptoms, confinement, COVID-19, pandemic
Statement of Significance.
Question. What are the prevalence, incidence, and persistence rates of insomnia and severity of psychological symptoms during COVID-19 relative to pre-pandemic data, and how are those symptoms related to confinement, social isolation, and changes in lifestyles during the pandemic?
Findings. This cohort study revealed very high rates of prevalent (52.9%), incident (32.5%), and persistent insomnia (76.5%) during the first wave of the COVID-19 pandemic, with decreased sleep quality and increased psychological symptoms relative to pre-pandemic data. Severity of insomnia was associated with higher stress and psychological symptoms, and with being in confinement, living alone, and increased usage of electronics.
Meaning. Large scale public sleep health education is needed to minimize occurrence of insomnia and mental health problems during and after a pandemic such as COVID-19 to prevent long-term adverse outcomes.
Introduction
The COVID-19 pandemic has produced unprecedented changes in many aspects of our lives, including changes in health behaviors (sleep, diet, exercise), social relationships, as well as in our work schedule and environment. Surveys conducted in various countries have reported very high rates of sleep (insomnia) and psychological (e.g. anxiety and depression) problems, as well as changes in sleep scheduling factors both among healthcare workers [1, 2] and in the general population [3–6]. Those problems have been attributed to such factors as confinement, loneliness and social isolation, reduced daylight exposure, and the stress and worries associated with the fear of infection, financial problems, and uncertainty about the outcome of COVID-19. While there is little doubt that sleep and mental health problems have increased since the beginning of the pandemic, the accuracy of the various estimates reported so far is questionable given the use of volunteers completing web-based surveys and the lack of pre-pandemic baseline data from the same sample. Nearly all published studies were cross-sectional surveys with convenience samples, some asking participants to make comparisons with their own situations before the pandemic, raising the issue as to whether data derived with such a methodology represent reliable and valid estimates of insomnia and psychological symptoms in the general population.
The present study capitalized on an ongoing longitudinal, population-based study of the natural history of insomnia in a Canadian cohort of adults who had completed their last follow-up assessment in 2018 and were then solicited during the first wave of COVID-19 (April to May 2020). The objective was to document prevalent, incident, and persistent cases of insomnia, along with perceived stress and psychological symptoms. We were also interested in documenting the associations of those symptoms with social confinement, loneliness, and changes in various lifestyles during the COVID-19 pandemic (e.g. electronic use, physical activity).
Methods
Study context and participants
Data for this cohort study were derived from a 10-year population-based longitudinal study on the natural course of insomnia among adults living in Canada [7, 8]. Shortly after the beginning of the pandemic in Canada, French-speaking participants (mostly from the Province of Quebec) who had completed the latest 2018 follow-up assessment were contacted to survey their sleep and insomnia, perceived stress, and psychological symptoms during the pandemic. The Province of Quebec was at that time the epicenter of the pandemic in Canada and residents of the province were in confinement under strict government health measures. Of the 1434 French-speaking participants who completed the 2018 survey (in May/June 2017 and January/February 2018), 1253 (87.4%) were reached by email (n = 922) or telephone (n = 331) in 2020 and 611 (48.8%) adults completed the survey in April and May of 2020. The median duration of follow-up was 28 months (range 24 to 37 months). A total of 594 (97.2%) who completed at least the COVID-19 and sleep/insomnia questions were included in the present analyses. The study was approved by the Research Ethics Committee of Université Laval and participants provided consent.
Sleep status groups
At each assessment in 2018 and 2020, participants were classified into one of three groups (i.e. good sleepers, subsyndromal insomnia, and insomnia syndrome) based on standard algorithms used in our longitudinal study [7–9], which combine criteria from the Diagnostic and Statistical Manual for Mental Disorders (4th edition) [10], the International Classification of Sleep Disorders (3rd edition) [11] and self-reported use of sleep medication. Responses from the Insomnia Severity Index (ISI; scores range from 0 to 28, with higher scores indicating greater severity of insomnia) [12] and the Pittsburgh Sleep Quality Index (PSQI; scores range from 0 to 21, with higher scores indicating poorer sleep quality) [13] were used to classify participants in one of the groups. The reference period for these questionnaires was the past month.
Good sleepers
Participants classified as good sleepers were satisfied with their sleep, did not report insomnia symptoms, and did not use prescribed or over-the-counter sleep medications.
Subsyndromal insomnia
Participants classified in that group reported insomnia symptoms at least three nights/week, but did not meet all criteria for an insomnia syndrome/disorder (i.e. did not report distress, daytime impairment or dissatisfaction with sleep, and sleep problems lasted < 1 month). Participants who were dissatisfied with their sleep, but did not exhibit insomnia symptoms, and those using prescribed or over-the-counter sleep medication at least one night, but less than three nights/week were also classified in this group.
Insomnia syndrome
Participants in this group met diagnostic criteria for an insomnia disorder. They were dissatisfied with their sleep (score of 3 or 4 on that ISI item) and had symptoms of initial (sleep onset latency > 30 min), middle (wake time after sleep onset > 30 min), or late insomnia (last awakening > 30 min before desired wake time) at least three nights/week for at least 1 month. They also reported significant distress or daytime impairment associated with insomnia (ISI score of 3 or 4 for one of those items). Participants who reported using prescribed sleep medication three or more nights/week were classified in this group.
Measures
Insomnia and sleep habits were measured using a sleep/health survey (including questions about the COVID-19 pandemic infection designed by our team, the ISI [12], the PSQI [13], and the Multidimensional Fatigue Inventory (MFI) [14]. Stress, anxiety, and depression were measured using the Perceived Stress Scale (Cohen, 1983), State-Trait Anxiety Inventory (STAI-State) [15], and the Beck Depression Inventory (BDI) [16], respectively, and selected questions from the survey. Several questions were asked about whether participants’ sleep schedules (bedtime, arising time, naps) had changed since the beginning of the pandemic; whether the amount of time they spent since the beginning of the pandemic had increased, decreased, or stayed the same for the several activities: time working from home, time spent on electronic devices (e.g. computers, laptops, cellular phones), time spent in physical activity, time spent outside the house, time spent in the bedroom; whether they had been in confinement at home because of government regulations since the beginning of the pandemic; and their degree of concern about their financial situation.
Statistical analyses
To determine incidence and persistence rates of insomnia and describe sleep schedules during the COVID-19 pandemic, linear (normal data) and generalized (binary data) mixed model analyses were computed. All inferential analyses were weighted according to normalized post-stratification sampling weights estimated to correct differential response rates according to the joint distribution of sex and age groups for the population of the Province of Quebec (2006 Canadian Census). Statistical significance was set at a standard bilateral alpha level of 0.05 and all analyses were performed using SAS, version 9.4 (SAS Institute, Cary, NC).
Results
Participants
The sample consisted of 594 adults (mean age: 48.3 ± 13.1 years; range: 18–83 years; 64.0% women) with complete data at both assessments. Participants were predominantly married or living with a partner (62.4%), working full time (50.3%) or retired (43.9%), and had a college degree (44.8%). There were 76% of the participants who reported at least one medical diagnosis (e.g. hypertension) and 18.3% reported at least one psychiatric diagnosis (e.g. anxiety). Only eight participants thought they had been infected with COVID-19.
Comparisons of data collected in 2018 from responders and those who declined to participate in the current survey revealed no differences on most demographic variables (e.g. sex, age, marital status, or occupation); the only exception was for education, with more completers having university degree relative to non-completers (46% vs. 35.4%, p < .001). Insomnia and sleep-related symptoms were slightly more severe in nonresponders relative to responders: ISI (M = 7.5 vs. 6.7, p = .008), PSQI (M = 5.9 vs. 5.5, p = .02), Epworth (M = 20.8 vs. 19.3, p < .001) and MFI fatigue scale (M = 45.9 vs. 43.4, p= .001). Those differences reflected on small effect sizes (ranging from Cohen’s d = 0.12 to 0.19). Nonresponders reported higher anxiety (STAI-state M = 30.7 vs. 29.3, p = .008) and depressive symptoms (BDI M = 6.7 vs. 5.8, p = .008) compared to responders, although effect sizes associated with those differences were small (0.12 to 0.14).
Prevalence, incidence, and persistence of insomnia
Table 1 shows changes in sleep/insomnia status from 2018 to 2020. In 2018, 59.5% (weighted percentage, n = 343) of the sample were classified as good sleepers, 25.1% (n = 151), had subsyndromal insomnia, and 15.5% (n = 100) presented an insomnia syndrome. During the COVID-19 pandemic in 2020, 50.7% (n = 290) were classified as good sleepers, 31.6% (n = 191) had subsyndromal insomnia, and 17.7% (n = 113) met criteria for an insomnia syndrome (see Table 1). Thus, overall prevalence rates for insomnia symptoms and syndrome increased from 42.3% in 2018 to 51.2% in 2020, for an absolute 21% increase during that interval.
Table 1.
Changes in sleep status from before to during the COVID-19 pandemic (n = 594).
| Time 2 (May 2020) | |||
|---|---|---|---|
| Time 1 (2018) | Good sleepers (n = 290) | Subsyndromal insomnia (n = 191) | Insomnia syndrome (n = 113) |
| Good sleepers (n = 343) | 231 (68.5%) | 87 (25.6%) | 25 (5.9%) |
| Subsyndromal insomnia (n = 151) | 46 (31.3%) | 81 (51.4%) | 24 (17.3%) |
| Insomnia syndrome (n = 100) | 13 (12.4%) | 23 (22.4%) | 64 (65.2%) |
Percentages are adjusted values.
Among participants classified as good sleepers in 2018 (n = 343), 25.6% (n = 87) developed insomnia symptoms and 5.9% (n = 25) developed an insomnia syndrome in 2020, for an overall 32.6% (n = 112) incidence of new cases of insomnia over a 2-year period. Among the participants who had insomnia in 2018, the overall persistence rate was 76.5% 2 years later. And of those with insomnia symptoms or syndrome in 2018, 23.5% went in remission in 2020.
Changes in insomnia severity, sleep quality, psychological symptoms, and medication use
For the total sample (regardless of sleep status), there was a significant worsening of sleep quality (PSQI; p = .001), but a decrease in insomnia severity (ISI; p = .029) in 2020 compared to 2018 (see Table 2). Fatigue (p = .001), anxiety (STAI-State) (p = .001) and depression (BDI) (p = .003) were significantly higher during the COVID-19 pandemic compared to baseline status in 2018 (depression was no longer significantly higher when the sleep item was removed from the BDI, p = .068). Proportions of sleep medication users (i.e. at least one night per week) did not change significantly from 2018 to 2020 for prescribed (M = 13.5% vs. 15.1%) and over-the-counter (3.6% vs. 5.4%) medication, natural products (M = 13.8% vs. 10.3%), and alcohol use as a sleep aid (M = 4.6% vs. 4.1%) (all ps > .10).
Table 2.
Changes in insomnia, sleep quality, and psychological symptoms from pre- to during the COVID-19 pandemic (n = 594)
| Mean ± standard error | |||
|---|---|---|---|
| Measure | Time 1 (2018) | Time 2 (2020) | P |
| Insomnia severity (ISI) | 6.7 ± 0.2 | 6.3 ± 0.2 | .0287 |
| Sleep quality (PSQI) | 5.5 ± 0.1 | 6.0 ± 0.1 | .0001 |
| Stress (PSS) | 19.3 ± 0.3 | 19.4 ± 0.3 | .762 |
| Fatigue (MFI) | 43.4 ± 0.6 | 46.3 ± 0.6 | <.0001 |
| Anxiety (STAI-State) | 29.3 ± 0.4 | 30.6 ± 0.4 | .0008 |
| Depression (BDI) | 6.4 ± 0.3 | 7.2 ± 0.3 | .0025 |
| Depression (BDI without the sleep item) | 5.8 ± 0.3 | 6.2 ± 0.3 | .0608 |
ISI, Insomnia Severity Index; PSQI, Pittsburgh Sleep Quality Index; MFI, Multidimensional Fatigue Inventory; STAI, State-Trait Anxiety Inventory; BDI, Beck Depression Inventory.
Changes in sleep schedules during the COVID-19 pandemic
Examination of sleep schedules on the PSQI revealed that participants reported going to bed later (22:50 vs. 22:38) and arising later (7:16 vs. 6:58) during the COVID-19 compared to their 2018 data (see Table 3), but there was no significant change in nocturnal sleep duration. Nonetheless, sleep efficiency was significantly lower and participants reported a significant increase in the frequency of naps; almost twice as many in 2020 compared to 2018.
Table 3.
Changes in sleep habits from pre- to during the COVID-19 pandemic (n = 594)
| Mean ± standard error | |||
|---|---|---|---|
| Variable | Time 1 (2018) | Time 2 (May 2020) | P |
| Bedtime | 22:38 ± 0.1 | 22:50 ± 0.1 | <.0001 |
| Arising time | 6:58 ± 0.1 | 7:16 ± 0.1 | <.0001 |
| Sleep duration (hours) | 7:18 ± 0.1 | 7:19 ± 0.1 | .8404 |
| Sleep efficiency (%) | 88.2 ± 0.7 | 81.9 ± 0.7 | <.0001 |
| Naps (frequency) | 1.2 ± 0.1 | 2.1 ± 0.1 | <.0001 |
| Use of sleep medication (%) | 13.5 ± 0.0 | 15.2 ± 0.0 | .0983 |
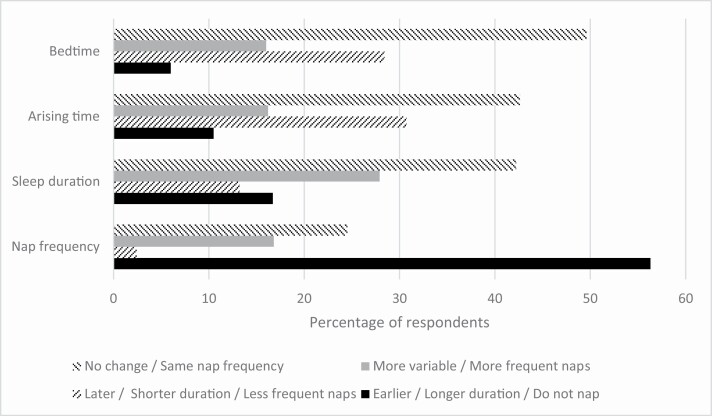
Figure 1 shows whether respondents reported that their sleep schedules, sleep duration, and naps changed during the pandemic compared to their pre-pandemic situation. While the majority reported no change in their sleep schedule, there were significantly more people reporting going to bed later and arising later than those reporting earlier sleep schedules (29% vs. 6% for bedtime and 31% vs. 11% for arising time). Likewise, most respondents reported no change in their overall sleep duration, but there were more people who mentioned sleeping longer than people who reported sleeping less before the pandemic (17% vs. 13%) and more people who mentioned increasing their daytime naps compared to those who said they decreased them (17% vs. 2%).
Figure 1.
Changes in sleep habits since the beginning of the COVID-19 pandemic (n = 594).
Associations between confinement, loneliness, social support, and changes in lifestyles during COVID-19 and insomnia and sleep quality
From April to May 2020, 74.8% of the sample (n = 443) were confined at home under strict government health emergency measures. Compared to those not in confinement (mostly essential workers), individuals living in confinement reported significantly higher scores on measures of stress, fatigue, and anxiety (all ps < .05). Individuals in confinement and living alone (n = 130) reported more severe depressive (p = .03) and fatigue symptoms (p = .002) than those in confinement but living with at least one other person (n = 311) and those not in confinement (n = 149). Lower social support (measured by the number of persons one can confide in) was significantly associated with more severe insomnia, poorer sleep, and more stress, anxiety, and depression symptoms (all Pearson rs significant at ps < .01).
About 63.5% of the sample reported increased time using electronic devices during the pandemic, and this increase was significantly associated with more severe insomnia (M ISI = 6.92 vs. 5.29, p = .0001) and lower sleep quality (M PSQI = 6.19 vs. 5.65, p = .05). The subgroup of 11.5% of the sample who reported spending more time in their bedroom during the pandemic experienced significantly higher insomnia severity (M ISI = 7.95 vs. 6.06, p = .004) and poorer sleep quality (M PSQI = 6.36 vs. 5.86, p = .04) compared to those who decreased or did not change the amount of time spent in their bedroom. Participants who decreased their physical activity during confinement (31.4%) reported significantly higher insomnia severity (M ISI = 7.35) compared to those who did not report any change (46.8%; M = 5.88) or those who increased their physical activity (21.8%; M = 5.71, p = .002). No group difference was found on sleep quality as measured by PSQI (p = .32). Finally, being more concerned about one’s financial situation was significantly associated with higher insomnia severity (r = 0.27, p < .001) and poorer sleep quality (r = 0.21, p < .001).
Discussion
The present findings indicate very high prevalence and incidence rates of insomnia during the early months of the COVID-19 pandemic compared to pre-pandemic rates in 2018. The overall prevalence of insomnia, for both symptoms and syndrome combined, increased from 42.3% to 51.2%, for an absolute 21% increase. The 32.7% incidence rate of new cases of insomnia was about four times higher than that reported previously for a similar 2-year interval in the pre-pandemic period [8]. Likewise, the rate of persistent insomnia over a 2-year interval was 76.5%, also much higher than previously reported (55%) for a similar interval. The severity of some psychological symptoms (anxiety, depression, fatigue) was also significantly higher during the pandemic, although the proportion of individuals exceeding clinical threshold remained low.
These longitudinal findings build on evidence derived from cross-sectional studies and provide more accurate estimates of prevalent, incident, and persistent insomnia in relation to the COVID-19 pandemic, and the extent to which insomnia is related or was exacerbated by psychological symptoms and lifestyle changes during the pandemic [3–5]. While several potential contributing factors have been proposed to account for the high rates of sleep and mental health problems during the pandemic, the present study provides new and stronger evidence that social confinement, combined with living alone, and lower social support and increase the use of electronic devices were all associated with both insomnia and psychological symptoms.
Interestingly, a slight shift in sleep scheduling was observed during the pandemic, with both bedtimes and arising times being pushed later by 12 and 18 min, respectively. While the global estimates of sleep duration did not seem to change with this shift, there were nonetheless more people who reported that their sleep duration had increased than people who stated it had decreased. Likewise, there were more people who increased the frequency of daytime napping than people who decreased that practice. Thus, it could be that some people, perhaps those who had accumulated a sleep debt before the pandemic took this opportunity to catch up on their sleep. The current data add to previous similar findings [17].
The availability of baseline data was an important strength of the current study compared to most previous studies which asked participants to compare their sleep patterns during and before the pandemic, a method that is subject to important recall bias and that precludes establishing reliable estimates of prevalent and incident cases of insomnia. Despite this strength of having pre-pandemic data, this study has some limitations which limit the generalizability of the findings. Although more than 1200 potential participants were solicited for the current study, only about half of them actually provided enough data to be included in the analyses. It is important to note, however, that nonresponders reported more severe insomnia and psychological symptoms compared to responders, which would argue for some degree of generalizability. Also related to this issue was the fact that our sample was restricted to a subgroup of the original sample, namely French-Canadian adults living in the Province of Quebec, a decision made for logistic and time constraints. With regard to this last point, the Province of Quebec was the epicenter of the pandemic in Canada at the time of the survey, with the highest infection and death rates relative to other provinces, which may have contributed to higher prevalence and incidence rates of insomnia.
While the present data indicate very significant increase in insomnia during the early wave of the pandemic, it is important to note that the original study, although population-based, was not designed to recruit a random and representative sample of the entire population; rather, it was interested in documenting the course of insomnia over time in a representative sample of individuals with insomnia. Thus, one might expect that individuals with insomnia are more likely to volunteer for such study. Nonetheless, the absolute increase of 21% is very substantial. Also, while the 32.7% incidence rate over a 2-year interval may seem very high, a previous study by Perlis et al. [18] reported a 1-year incidence rate of acute insomnia at 27%. While the two studies were different in their method used to evaluate insomnia (one used daily sleep diaries and focused on acute insomnia and the current study focused on chronic insomnia and used annual evaluation with the past month as reference). Because the current methodology may have missed on intermittent cases that emerged and resolved during the 2-year interval, we are confident that the current incidence rates are fairly conservative. Given the periodic nature of insomnia for many individuals, the same limitation could be raised about the interpretation of the rates of persistent/remitted insomnia (76.5%/23.5%).
The increased prevalence of insomnia during the pandemic along with a decrease of insomnia severity may seem counterintuitive. However, data from Table 1 suggest that the higher prevalence in 2020 was likely driven by increases in sub-syndromal insomnia (25% to 32%) while prevalence of syndrome increased only from 16.8% to 19%. Thus, the pandemic did not so much affect those who already had an insomnia disorder/syndrome, but rather it increased the number of good sleepers that developed sub-syndromal insomnia, which likely brought down the overall ISI average. It is also important to note that despite the statistical significance of the overall reduction in insomnia severity (total ISI score decreased from 6.7 to 6.3), the effect size was very small (0.8) and probably of no clinical significance
The main implication of the current findings is that public health education and clinical resources need to be dedicated for individuals at risk for sleep and psychological problems. Early intervention is important given the evidence that persistence of insomnia over time may increase the risk of or exacerbated existing psychological problems such as anxiety and depression. Public sleep health education initiatives are particularly timely and relevant during a pandemic such as COVID-19, and they would also be highly relevant at times of other major life events (e.g. natural disasters) [19].
In summary, the COVID-19 pandemic was associated with significant adverse outcomes on both sleep and mental health, highlighting the urgent need for broad public sleep and mental health programs. Prevention of insomnia and promotion of mental health, in particular through the promotion of sleep health behaviors, should be prioritized during and after a pandemic such as COVID-19.
Funding
This research was supported by the Canadian Institutes of Health Research grants to the first author (#42504; #353509).
Disclosure Statement
Charles Morin has received research support from Idorsia, Canopy Health, Eisai, Lallemand and served as consultant on advisory boards with Eisai, Merck, Pear Therapeutics, Sunovion and Weight Watchers. None of those were related to the present paper. All other authors reported no conflict.
References
- 1. Pappa S, et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sanghera J, et al. The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting—a systematic review. J Occup Health. 2020;62(1):e12175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kokou-Kpolou CK, et al. Insomnia during COVID-19 pandemic and lockdown: prevalence, severity, and associated risk factors in French population. Psychiatry Res. 2020;290:113128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Casagrande M, et al. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yu BY, et al. Prevalence of sleep disturbances during COVID-19 outbreak in an urban Chinese population: a cross-sectional study. Sleep Med. 2020;74:18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Partinen M, et al. ; ICOSS-Collaboration Group. Sleep and circadian problems during the coronavirus disease 2019 (COVID-19) pandemic: the International COVID-19 Sleep Study (ICOSS). J Sleep Res. 2021;30(1):e13206. [DOI] [PubMed] [Google Scholar]
- 7. Morin CM, et al. The natural history of insomnia: a population-based 3-year longitudinal study. Arch Intern Med. 2009;169(5):447–453. [DOI] [PubMed] [Google Scholar]
- 8. Morin CM, et al. Incidence, persistence, and remission rates of insomnia over 5 years. JAMA Netw Open. 2020;3(11):e2018782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. LeBlanc M, et al. Incidence and risk factors of insomnia in a population-based sample. Sleep. 2009;32(8):1027–1037. doi: 10.1093/sleep/32.8.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. American Psychiatric Association. Diagnostic and Statistical Manual for Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 11. American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 12. Morin CM, et al. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Buysse DJ, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 14. Smets EM, et al. The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res. 1995;39(3):315–325. [DOI] [PubMed] [Google Scholar]
- 15. Spielberger CD. Manual for the State-Trait Anxiety Inventory (STAI). Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 16. Beck AT, et al. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8(1):77–100. [Google Scholar]
- 17. Cellini N, et al. Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: age, gender and working status as modulating factors. Sleep Med. 2021;77:112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Perlis ML, et al. The natural history of insomnia: the incidence of acute insomnia and subsequent progression to chronic insomnia or recovery in good sleeper subjects. Sleep. 2020;43(6). doi: 10.1093/sleep/zsz299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Belleville G, et al. Post-traumatic stress among evacuees from the 2016 Fort McMurray Wildfires: Exploration of psychological and sleep symptoms three months after the evacuation. Int J Environ Res Public Health. 2019;16(9). [DOI] [PMC free article] [PubMed] [Google Scholar]