Supplemental Digital Content is Available in the Text.
Key Words: ART adherence, Uganda, COVID, electronic health records, Africa, HIV
Introduction:
Recent studies project thousands of additional AIDS-related deaths because of COVID-19–related disruptions in HIV care. However, the extent to which disruptions in care have materialized since the start of the pandemic is not well understood.
Methods:
We use electronic health records to investigate how the pandemic has affected clinic visits, patients' antiretroviral therapy (ART) supply, and viral suppression for a cohort of 14,632 HIV clients from a large HIV clinic in Kampala, Uganda. We complement this with an analysis of electronically measured longitudinal ART adherence data from a subcohort of 324 clients.
Results:
Clinic visits decreased by more than 50% after a national lockdown started. The risk of patients running out of ART on a given day increased from 5% before the lockdown to 25% 3 months later (Relative Risk Ratio of 5.11, 95% confidence interval: 4.99 to 5.24) and remained higher than prelockdown 6 months later at 13% (Relative Risk Ratio of 2.60; 95% confidence interval: 2.52 to 2.70). There was no statistically significant change in electronically measured adherence or viral suppression.
Conclusion:
We document substantial gaps in HIV care after the start of the COVID-19 pandemic in Uganda. This suggests that measures to improve access should be explored as the pandemic persists. However, ART adherence was unaffected for the subcohort for whom we measured electronic adherence. This suggests that some clients may have stockpiles of ART tablets from previous prescriptions that allowed them to keep taking their medication even when they could not visit the clinic for ART refills.
INTRODUCTION
The COVID-19 pandemic creates several barriers to HIV care globally, which may result in increased AIDS-related deaths and greater spread of HIV.1–3 People living with HIV (PLWH) require daily doses of antiretroviral therapy (ART) to control their illness and reduce risk of forward transmission. Disruptions in care can hinder PLWH's ability to adhere to medication regimens.4 Barriers to HIV care and ART adherence during the pandemic may be exacerbated in poor communities with limited access to health facilities, such as those in sub-Saharan Africa where most PLWH reside.5–7 The World Health Organization (WHO) estimates that disruptions from the pandemic could cause up to half a million additional deaths from AIDS-related illnesses, mostly in sub-Saharan Africa.8 In addition, interruptions in ART access and daily pill taking among PLWH may lead to drug resistance and increased HIV viral loads, which in turn increase the risk of viral transmission.9,10 However, the extent to which care disruptions have materialized during the COVID-19 pandemic is not well understood.
The pandemic could reduce access to HIV care and hinder ART adherence for several reasons. First, many countries have implemented policies that require quarantining and social distancing, thus restricting transportation and limiting people's ability to travel to obtain their ART refills. In Uganda, the government implemented a national lockdown starting on March 25, 2020, that prohibited public transportation and limited private travel to 1 person per vehicle.11 Second, although Uganda eased transport restrictions after 2 months, PLWH may still avoid coming to the clinic because of fear of COVID-19 infection. A recent survey of PLWH in Uganda confirmed that 54% of respondents believed that coming to the clinic increased their risk of acquiring COVID-19.12 Third, the pandemic limits economic activity because of restrictions and reduced demand. This could increase food insecurity. Because most ART medication should be consumed with food to avoid unpleasant side effects, the increase in food insecurity may reduce ART adherence. Food insecurity could also affect adherence through other mechanisms such as depression and competing priorities. A recent study from Uganda, where food insecurity among PLWH was near 20% before the pandemic, found that lack of food is one of the most important barriers to ART adherence.13 Finally, the pandemic could disrupt daily pill-taking routines, which are important for consistent adherence, by changing the structure and schedule of daily life.12
Several recent studies have discussed or modeled the potential impacts of the COVID-19 pandemic on HIV-related outcomes.3,4,6,7,14,15 Others have asked PLWH about how they are faring during the pandemic through surveys or qualitative interviews.12,16–18 However, studies to date lack quantitative evidence on the extent to which the pandemic affects whether people have sufficient personal ART supply (ie, have medication on a given day), ART adherence, and clinical outcomes. In this observational cohort study, we used electronic health records (EHRs) from before and after the start of lockdown to investigate how the pandemic and lockdown affected HIV care disruptions (clinic attendance and personal ART supply) and viral suppression for a cohort of 14,632 HIV clients from Mildmay Uganda in Kampala, one of the largest HIV care providers in Uganda (henceforth the full Mildmay cohort). We complement this with the analysis of electronically measured, longitudinal ART adherence data from a subcohort of 324 clients enrolled in a study we conducted at Mildmay collected through electronic medication event monitoring system (MEMS) pill bottle caps (henceforth the MEMS cohort) and additional survey data to contextualize our findings with self-reported experiences during the pandemic.
METHODS
Study Design, Setting, and Participants
We use data from the EHR system of Mildmay Uganda. Mildmay specializes in the provision of comprehensive HIV and AIDS prevention, care, and treatment services through outpatient and inpatient services. The main facility has modern laboratory infrastructure with ability to do virology and other tests. Among the more than 15,000 patients served at the main facility in Kampala, 8% are children younger than 18 years, 64% are female, and 100% of clients receiving HIV care are on ART. Mildmay serves a large portion of the HIV-positive population in and around Kampala, and thus their clients represent a variety of different demographic groups. The average time to arrive to the clinic in our MEMS cohort is about 2 hours, which implies that clients come from all over the central region in Uganda, not just the urban areas near the clinic.
Mildmay is one of a growing number of facilities in sub-Saharan Africa with a well-established EHR system. We restrict our analysis to clients with at least 2 ART prescriptions in the 7 months leading up to the lockdown (14,632 clients) because these clients are likely to have been active Mildmay clients when the lockdown started on March 25, 2020. Prescriptions are usually for 30, 60, or 90 days, with 90 being most common (52% of all ART prescriptions).
As part of an ongoing study, Behavioral Economics Incentives to Support HIV Treatment Adherence (BEST, Clinical Trials Registration Number NCT03494777), we enrolled adult Mildmay clients to participate in a randomized controlled trial. These clients constitute our MEMS cohort and are a subset of the full Mildmay cohort.
The BEST study tests an intervention that promotes ART adherence through small rewards based on behavioral economics for high adherence, and is described in detail elsewhere.19 To recruit the BEST study participants, we used EHRs to identify patients who were aged 18 years or older, had been on ART at Mildmay for 2 years or longer, and had documented adherence problems in the 6 months preceding recruitment (defined as showing lack of viral suppression, being sent to adherence counseling, or showing disease stage 3 or 4 as per WHO guidelines).
Between March 2018 and August 2019, we recruited participants for the BEST study. As part of the BEST study protocol, clients received MEMS caps that recorded each time they opened their ART pill container. We excluded clients who opened their MEMS cap for less than 30% of their prescribed doses during the first month of the BEST study because this implies an inability to use the MEMS cap. Consistent use of the MEMS cap was a requirement for participating in the BEST study. Of the 376 clients who we recruited, 24 participants were excluded because they were not consistently using the MEMS cap. An additional 28 were lost to follow-up or excluded from the analysis because they did not meet the inclusion criteria for the EHR data extraction (ie, did not have at least 2 ART prescriptions between July 2019 and March 2020). We thus included 324 clients in our analysis; 215 were assigned to 1 of the 2 BEST intervention arms, and 109 were assigned to the control arm. The intervention did not moderate any of the results reported in this article (results available on request).
The BEST study was ongoing in its second year when the pandemic started to affect life in Uganda around March 2020.20 All intervention activities were paused when the pandemic began, but clients retained their MEMS caps and were instructed to continue using them. We used this cohort of 324 BEST participants to measure how ART adherence changed after the start of the pandemic. Most of the BEST participants had MEMS cap data available after the pandemic; 310 participants had a MEMS reading for the period up to June 2020 or later, and 293 participants had a MEMS reading in September 2020 or later.
The government implemented a national lockdown on March 25, 2020.20 Public transportation, taxis, and most businesses were required to close during this period, and citizens were told to stay in their homes aside from a few essential activities. Mildmay remained open during the lockdown. Although the lockdown officially ended on June 2, several transportation restrictions remained in effect by September 2020 (eg, use of motorcycle taxis or boda bodas, a common form of transportation in Uganda, remained restricted at the time of writing this article). Our study design uses longitudinal EHRs and adherence data to measure changes in outcomes after the start of the government-mandated lockdown.
We obtained ethics approval from the RAND Corporation's Human Subjects Protection Committee (#2016-0956), the Mildmay Uganda Research Ethics Committee Institutional Review Board (#02013-2018), and the Uganda National Council for Science and Technology (#2394). This study conforms to STROBE guidelines for observational studies (see Appendix, Supplemental Digital Content, http://links.lww.com/QAI/B728).
Data
Prescription Records
We extracted EHR data on ART prescriptions for all clients who met the eligibility criteria described above (n = 14,632). These data include the prescription date and days' supply of the prescription. We used this to assess the extent to which clients were likely to have run out of their medication, which implies that they missed a refill. We used the prescription duration to record the remaining days' supply on each day, assuming clients took their medication as prescribed (eg, if they get 90 days' supply on March 1, then they will have 89 remaining days' supply on March 2). We accounted for drug stockpiling by adding days' supply over time (eg, if they had 12 days' supply stockpiled when they get a new 90-day prescription, this would be coded as 102 days' supply). This approach is adapted from the “proportion of days covered” measure, which is a validated measure of medication adherence.21,22 Importantly, it is possible this measure underestimates remaining ART supply if clients take fewer pills than prescribed. This measure could also underestimate remaining ART supply if clients switched clinics and refilled their ART at the new location, in which case they would not have a prescription in the Mildmay EHR. To address this, we restricted the analysis to clients with at least 1 clinic visit between September 30, 2020, and August 6, 2021; that is, after our study period ended, they were observed at Mildmay and thus are unlikely to have moved or changed clinics during the pandemic. This excluded 1415 clients (9.6% of our sample; see Appendix Table S4, Supplemental Digital Content, http://links.lww.com/QAI/B728).
Mildmay allowed clients to refill their medication at external locations during the lockdown. Although the records team made an effort to add external refills to the EHR retrospectively through client reports, some external refills might be omitted from the EHR data. Only 7% of our MEMS cohort reported getting refills at different clinics on the phone survey (described below). To address this, we conducted sensitivity analyses where we excluded people who got external refills (see Appendix Figure S3, Supplemental Digital Content, http://links.lww.com/QAI/B728).
Clinic Visits and Viral Loads
We extracted data on clinic visits and HIV viral load measures for the same cohort of clients for whom we extracted prescription data. We used these data to create monthly totals of client visits and to estimate the share of Mildmay clients with a suppressed viral load in each month (below 200 copies/mL).23 Clients get routine viral load testing annually, which means monthly suppression numbers are based on different clients in different months.
Electronically Measured Adherence
All participants enrolled in the BEST study (intervention and control groups) received a MEMS cap that attached to their pill container on recruitment. MEMS caps house a microelectronic chip that records the date and time of each container opening, enabling a precise, objective assessment of the timing of each dose. Our study team extracted MEMS cap data using the PowerView software each time participants visited the clinic. We can only observe adherence data during the pandemic for individuals who visited the clinic after the pandemic started. We used the ART regimen in a client's medical record, which is composed of up to 3 different individual medications, to assess how many doses they were prescribed each day, which accounts for regimen changes. Clients with a once-a-day medication combined with a twice-a-day medication were classified as twice a day.
We used the MEMS cap event data to create a client day data set that records the client's adherence for each day that they had the device. We created a variable that captures the share of prescribed pills that were actually taken each day by dividing the number of bottle openings on each day (capped at the prescribed number of doses to prevent adherence measurements over 100%) by the number of doses prescribed (based on dosage information in the EHR).
We also assessed the degree to which clients' daily ART adherence routines were altered during the pandemic. We analyzed changes in the daily timing of pill container openings before and after the government-mandated lockdown began. We constructed a measure (2 measures for twice-a-day regimens) that indicated whether each opening was performed within a 2-hour window (±1 hour) from clients' typical pill-taking time based on the modal time over a 60-day window (±30 days). Most habitual behaviors are performed at approximately the same time each day.24,25 We hypothesized that the pandemic would disrupt pill-taking routines which could reduce ART adherence.
Surveys
Between March 2018 and August 2019, participants in the MEMS cohort completed a baseline survey on enrollment in the BEST study. The MEMS cohort also completed surveys at 6 months and 12 months after the start of the BEST study. We use the month 12 survey to assess changes in food security after the lockdown. Starting June 12, 2020, the team implementing the BEST study conducted phone surveys designed to understand clients' perceptions about the pandemic and how it affects their HIV care and adherence behavior. The survey collected quantitative data, which we report on in this article, and qualitative data, which has been reported elsewhere.12 The team called all 324 study participants and was able to implement the survey for 314 participants (10 clients could not be reached). During the call, the team also informed participants that the BEST study would continue after the lockdown ended and reminded them to continue using their MEMS caps.
Statistical Analysis
We analyzed ART adherence (percent of doses taken), client days without personal ART supply, number of clinic visits per month, and share of clients showing viral suppression from May 2018 to September 2020. We used linear regression models to compare these outcomes before the national lockdown and after the start of national lockdown. In addition, we used interrupted time series models to adjust for prelockdown trends in outcomes.26 We analyzed adherence and ART supply data at the client day level and viral suppression at the viral load test result level. We clustered standard errors by client using Huber–White cluster-robust standard errors to account for autocorrelation over time within client.27 We also conducted sensitivity analyses using mixed-effects models with random intercepts for each client (see Appendix Tables S3 and S5, Supplemental Digital Content, http://links.lww.com/QAI/B728). We do not have postlockdown MEMS cap readings for all study participants, which could introduce selection bias if the probability of coming to the clinic after the lockdown started is correlated with adherence. To address this, we split our MEMS cohort into different cohorts based on when the most recent MEMS cap data download occurred: (1) full sample (n = 324), (2) MEMS cap reading in June 2020 or later (n = 310), and (3) MEMS cap reading in September 2020 or later (n = 293). Options (2) and (3) have better internal validity because the same sample is used before and after the lockdown starts. We conducted our analysis separately for these 3 cohorts to assess whether changes in cohort composition over time affect our estimates. We conducted all analyses using Stata/SE 15.
Role of the Funding Source
The funder of the study had no role in study design, data collection, analysis, and interpretation or writing of the article. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
RESULTS
Table 1 shows demographics of the full Mildmay cohort and the MEMS cohort. The full Mildmay cohort was 39 years old on average, 34% male, had been taking ART for an average of 7.3 years, and 87.5% were virally suppressed in their most recent viral load test before the lockdown. The MEMS cohort was older (average aged 41 years), had been on ART for nearly 3 years longer on average than the full Mildmay cohort (9.8 years), and had a slightly lower proportion with a suppressed viral load. Table S1, Supplemental Digital Content, http://links.lww.com/QAI/B728, shows more detailed summary statistics about the MEMS cohort using data collected from the BEST study baseline survey.
TABLE 1.
Demographic and Clinical Characteristics of Full Mildmay Cohort and MEMS Cohort as of June 2019
| Full Mildmay Cohort | MEMS Cohort | |
| N | 14,308 | 324 |
| Age (yr) | 38.7 (0.116) | 41.1 (0.717) |
| Male (%) | 34.8 (0.398) | 36.4 (2.670) |
| Years at Mildmay | 8.1 (0.042) | 11.0 (0.212) |
| Years on ART | 7.4 (0.038) | 9.9 (0.198) |
| Viral load (copies/mL) | 4821 (1019) | 1850 (765) |
| Undetectable viral load (%) | 87.5 (0.276) | 86.7 (1.880) |
Data are from electronic health records as of June 2019. Viral load measures are based on the most recent viral load test. Standard errors in parentheses.
N, number.
Figure S1, Supplemental Digital Content, http://links.lww.com/QAI/B728, shows the number of recorded visits at Mildmay (that typically coincide with drug refills) in each month. In April 2018, there were 6054 client visits, and in April 2019, there were 7093. There was a stark drop in April 2020 after the onset of the lockdown, with only 3837 clients visiting the clinic (only 54% of total visits in April 2019). In May 2020, total visits were 45% of what they were in May 2019. Visits rebounded in June 2020 after the lockdown was partially lifted but remained substantially lower in July and August relative to previous years.
Figure 1 shows the share of days with personal ART supply for the full Mildmay cohort and our MEMS cohort in each month from May 2018 to September 2020. Mildmay clients would have run out of medication on about 5% of days (1.5 days) per month on average before the lockdown if they took all doses as prescribed. By June 2020, clients would have had no ART on 26% of days (7.8 days) on average. By September 2020 when the lockdown had been mostly lifted, the share of days without personal ART supply still remained higher than the prelockdown period at 14% of days (4.2 days). This suggests that clients were less likely to refill their medication on time after the start of the lockdown and continued to forgo refills for several months after the lockdown was mostly lifted. Results are similar but slightly less pronounced for the MEMS cohort (Fig. 1, dashed line).
FIGURE 1.
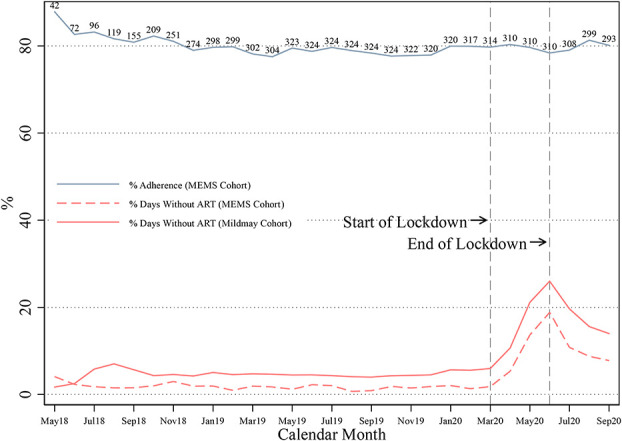
ART adherence and days without personal ART supply over time. Numbers above the adherence line represent sample sizes for each month for the MEMS cohort. % of days without ART reflects the share of client days in a given month where ART supply was 0. This measure is based on pharmacy refill records and assumes clients took their pills as prescribed. The full Mildmay cohort includes all clients with at least 2 ART prescriptions between July 2019 and March 2020. The MEMS cohort is the subset for which we have MEMS cap data. Although the “lockdown” in Kampala was eased in June 2020, several restrictions were still in place by September 2020.
Regression results in Table 2 show that the risk of having no personal ART supply on a given day increased by 0.21 by June 2020 compared with a prelockdown average of 0.05 [Relative Risk Ratio (RRR) of 5.29, 95% confidence interval (CI): 5.16 to 5.42] and remained 0.089 higher by September 2020 (RRR of 2.82; 95% CI: 2.72 to 2.92). After adjusting for the pre-existing trend (column 2 of Table 2), the risk of no personal ART supply was 0.20 higher in June (RRR of 5.11, 95% CI: 4.99 to 5.24) and 0.078 higher in September (RRR of 2.60; 95% CI: 2.52 to 2.70) compared with the prelockdown average. Results are similar when we use a mixed-effects model (see Appendix Table S3, Supplemental Digital Content, http://links.lww.com/QAI/B728) and when we restrict to clients with a visit after our study period ended (ie, clients who we are certain did not leave the clinic; see Table S4, Supplemental Digital Content, http://links.lww.com/QAI/B728).
TABLE 2.
Change in Personal ART Stockouts and ART Adherence After the Start of the Lockdown (Regression Results)
| Change in Risk of Personal ART Stockout on a Given Day (Full Mildmay Cohort) | Change in Risk of Personal ART Stockout on a Given Day (MEMS Cohort) | Change in % Adherence (MEMS Cohort) | ||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Unadjusted | Interrupted Time Series | Unadjusted | Interrupted Time Series | Unadjusted | Interrupted Time Series | |
| Prelockdown trend (d) | 2.27e-05*** (3.08e-06) | 1.50e-05 (1.17e-05) | −0.00418 (0.00309) | |||
| April 2020 | 0.0555*** (0.00203) | 0.0484*** (0.00179) | 0.0349*** (0.00970) | 0.0300*** (0.00885) | 1.032 (1.172) | 2.278* (1.172) |
| May 2020 | 0.161*** (0.00294) | 0.153*** (0.00280) | 0.118*** (0.0167) | 0.113*** (0.0158) | 0.329 (1.238) | 1.702 (1.267) |
| June 2020 | 0.209*** (0.00324) | 0.201*** (0.00312) | 0.170*** (0.0196) | 0.164*** (0.0189) | −0.927 (1.315) | 0.573 (1.405) |
| July 2020 | 0.146*** (0.00293) | 0.136*** (0.00277) | 0.0896*** (0.0155) | 0.0834*** (0.0146) | −0.279 (1.195) | 1.349 (1.383) |
| August 2020 | 0.105*** (0.00268) | 0.0951*** (0.00245) | 0.0691*** (0.0144) | 0.0624*** (0.0131) | 1.998 (1.244) | 3.755** (1.494) |
| September 2020 | 0.0888*** (0.00253) | 0.0783*** (0.00223) | 0.0592*** (0.0131) | 0.0521*** (0.0116) | 0.824 (1.289) | 2.709* (1.596) |
| Observations (client days) | 11,550,530 | 11,550,530 | 271,836 | 271,836 | 230,498 | 230,498 |
| R-squared | 0.047 | 0.047 | 0.049 | 0.049 | 0.000 | 0.000 |
| No. of clients | 14,632 | 14,632 | 324 | 324 | 324 | 324 |
| Average before lockdown | 0.0487 | 0.0487 | 0.0170 | 0.0170 | 79.37 | 79.37 |
Data were analyzed at the client day level. Columns (1) and (2) include all clients with at least 2 ART prescriptions between July 2019 and March 2020. Columns (3)–(6) include the sample for which we had MEMS cap adherence data. The stockout variable is set to 1 if the client did not have ART on a given day based on pharmacy refill records and assumes they took their pills as prescribed. Coefficients in columns (1) through (4) can be interpreted as the change in the risk of running out of ART on a given day in each month compared with before the pandemic (if pills were taken as prescribed). Adherence is the % of prescribed doses taken on a given day based on MEMS cap openings. Adherence coefficients in columns (5) and (6) can be interpreted as the percentage point change in ART adherence in each month compared with before the pandemic. Coefficients in columns (2), (4), and (6) adjust for the prelockdown trend in the outcome. The government-mandated lockdown started on March 25 and ended on June 2, 2020. There are more client day observations in columns (3) and (4) than in columns (5) and (6) because we have up-to-date pharmaceutical records for all 324 clients, but we are missing MEMS cap data for some clients in later months. See Figure 1 for sample sizes with adherence data in each month. Standard errors, which are clustered by individual, are in parentheses.
***P < 0.01, **P < 0.05, *P < 0.1.
Before March 2020, monthly adherence for our MEMS cohort was consistently around 80%, with a slight decline over time (Fig. 1). There was no change in adherence after the lockdown started or at any point during the pandemic. The effect of the lockdown on adherence looks similar when we restrict to those with a reading in June 2020 or later and September 2020 or later (see Figure S2, Supplemental Digital Content, http://links.lww.com/QAI/B728). Column 5 of Table 2 shows that MEMS cap measured adherence was not significantly different in any month after March 2020 compared with the prelockdown average. After adjusting for pre-existing trends, adherence was slightly higher in the postlockdown months and significantly higher in August 2020. Although there was no decrease in adherence after the lockdown, the MEMS cohort demonstrated a similar increase in the risk of running out of personal ART supply as the overall clinic population (columns 3 and 4 of Table 2).
We find that pill-taking routines may have been disrupted by the pandemic. Before the pandemic, participants were taking 68.9% of their daily pills consistently within a 2-hour time window, but this percentage was declining by roughly 0.3 percentage points per week of the pandemic. The government lockdown in April 2020 did not significantly affect the consistency of daily pill-taking timing, but the timing of pill taking became significantly less consistent during the later months of the pandemic (see Table S6, Supplemental Digital Content, http://links.lww.com/QAI/B728).
We do not find a reduction in viral suppression. Figure 2 plots the share of clients with a suppressed viral load in each month (of all clients who had a viral load test that month) for the full Mildmay cohort, and Table 3 shows regression results estimating the change in viral suppression after the start of the lockdown. Nearly 90% of clients had a suppressed viral load in each month, and this number went up slightly after the lockdown. Regression results show a modest but statistically significant increase in viral suppression after March 2020; between a 1.8 and 5.7 percentage point increase depending on the month. Although fewer clients had viral load tests during the lockdown (average of 325 in April and May 2020), the months after the lockdown eased had more viral load tests conducted than the average in the months before the lockdown (average of 1323 in June to September 2020 compared with an average of 1285 between May 2018 and March 2020). The risk of running out of ART before the lockdown was similar for clients with a viral load test after the lockdown (6.2% of client days) compared with those with no postlockdown viral load test (6.9% of client days). Results were similar when we restrict only to clients with a test both before and after the start of the lockdown (columns 3 and 4 of Table 3) and Table S2, Supplemental Digital Content, http://links.lww.com/QAI/B728, shows that these groups had similar characteristics.
FIGURE 2.
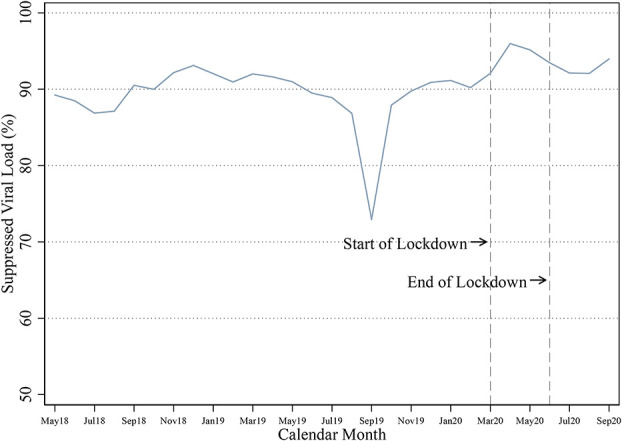
Share of clients with suppressed viral load by month. Data are from all viral load tests conducted for the full Mildmay cohort from May 2018 to September 2020 (36,356 tests for 14,632 unique clients). The full Mildmay cohort includes all clients with an ART prescription between July 2019 and March 2020. This figure plots the share of viral load tests in each month that recorded a suppressed viral load (<200 copies/mL). We are not sure why there is a dip in September 2019, but this could be because one of the viral load machines was down and the remaining machine could have had higher sensitivity. Although the “lockdown” in Kampala was eased in June 2020, several restrictions were still in place by September 2020.
TABLE 3.
Change in Share of Viral Load Tests That Show Viral Suppression After the Start of the Lockdown (Regression Results)
| Full Mildmay Cohort | Mildmay Cohort With a Viral Load Measure Before and After the Start of the Lockdown | |||
| (1) | (2) | (3) | (4) | |
| Unadjusted | Interrupted Time Series | Unadjusted | Interrupted Time Series | |
| Prelockdown trend (d) | 0.00106 (0.000844) | −0.0113*** (0.00165) | ||
| April 2020 | 5.683*** (1.190) | 5.307*** (1.232) | 7.198*** (1.236) | 11.75*** (1.450) |
| May 2020 | 4.616*** (1.142) | 4.207*** (1.190) | 6.770*** (1.159) | 11.68*** (1.403) |
| June 2020 | 3.172*** (0.820) | 2.731*** (0.888) | 4.970*** (0.858) | 10.22*** (1.185) |
| July 2020 | 1.755** (0.759) | 1.281 (0.837) | 3.003*** (0.806) | 8.597*** (1.155) |
| August 2020 | 1.798*** (0.688) | 1.292* (0.785) | 3.177*** (0.725) | 9.114*** (1.142) |
| September 2020 | 3.639*** (0.610) | 3.101*** (0.732) | 5.267*** (0.647) | 11.55*** (1.143) |
| Observations (number of tests) | 34,438 | 34,438 | 16,552 | 16,552 |
| R-squared | 0.002 | 0.002 | 0.006 | 0.009 |
| No. of clients | 14,199 | 14,199 | 5575 | 5575 |
| Average before lockdown | 90.37 | 90.37 | 89.06 | 89.06 |
Data were analyzed at the viral load test level. Columns (1) and (2) include all clients with a viral load test at Mildmay clinic as of May 2018. Columns (3) and (4) include only clients with at least 1 test before the lockdown on March 25, 2020, and 1 test after the lockdown. Viral suppression is set to 1 if viral load measure was <200 copies/mL. Coefficients in columns (2) and (4) adjust for the prelockdown trend in the viral suppression. The government-mandated lockdown started on March 25 and ended on June 2, 2020. Standard errors, which are clustered by individual, are in parentheses.
***P < 0.01, **P < 0.05, *P < 0.1.
Table 4 shows results from our phone survey. 41.8% of clients reported that the pandemic affects their ability to come to the clinic, but only 9.3% indicated they did not have enough ART at some point during the lockdown. Only 11.2% of respondents said that the pandemic decreases their ability to adhere to their medication, and only 8.3% reported worse adherence during the lockdown. Larger fractions of respondents reported an increased ability to adhere (12.5%) and better adherence (30.0%) during the lockdown. Finally, 23.9% of respondents reported high levels of food insecurity as measured by an adapted version of the Food Insecurity Experience Scale.28 This is a 19% increase in food insecurity levels compared with the month 12 survey which was conducted as part of the BEST study before the lockdown. Similarly, during the lockdown, 12.1% of respondents reported having missed a dose of ART in the past month because they did not have enough food compared with only 4.4% in the month 12 survey before the lockdown.
TABLE 4.
Survey Results for MEMS Cohort on Impacts of the Pandemic on Clinic Access, ART Adherence, and Food Security
| N = 314 N (%) |
|
| Covid-19 impacts ability to come to clinic | 131 (41.8%) |
| Not enough ART medication at any point since lockdown started | 29 (9.23%) |
| Pandemic impacts ability to adhere to medication | 76 (24.2%) |
| Increases ability | 38 (12.1%) |
| No change | |
| Decreases ability | 39 (12.4%) |
| Change in adherence during lockdown | 240 (76.3%) |
| Better adherence | 36 (11.1%) |
| No change | |
| Worse adherence | 94 (29.9%) |
| Food insecure | 194 (61.7%) |
| Missed dose of ART due to lack of food | 26 (8.28%) |
Data are from a phone survey conducted between June 12 and September 25, 2020. “Food Insecure” share is based on responses to 5 survey questions on access to food at the level of the household and the associated constraints on ability to obtain adequate quantity of food (adapted from the Food Insecurity Experience Scale). We defined the levels as low (raw score 0–3), and high (raw score 4–5) based on whether the respondent responded affirmatively to questions on cutting the size of meals or skipping a meal, gone a whole day without eating, been hungry but couldn't eat because they did not have money to buy food, not been sure where getting next meal, or felt worried or stressed about not having a reliable source of food. Ten of the 324 participants could not be reached by phone which is why the sample size is only 314.
N, number.
DISCUSSION
This study documents substantial disruptions in clinic attendance and personal ART supply after the COVID-19–induced lockdown in Uganda. This is despite the fact that Mildmay remained open for drug refills during the lockdown, had sufficient ART supply to fulfill all prescriptions, and allowed patients to get their refills from other clinics and community distribution points. Personal ART supply took several months to rebound after the lockdown was lifted and remained lower through the end of the observation period (September 2020). However, among the subsample with MEMS caps, we do not observe a substantive change in electronically measured adherence and we find an increase in self-reported adherence after the lockdown. Although we cannot exclude the possibility that this subsample behaved differently either because they were part of a study or because they had different demographic and clinical characteristics at baseline, but regardless, this suggests that some Mildmay clients had sufficient ART supply stockpiled to keep adhering for several months without needing to visit the clinic. As a result, most clients who received a viral load test after the lockdown started were able to maintain viral suppression and we do not observe a reduction in suppression. These results highlight the challenges PLWH face in accessing HIV care during a pandemic but call into question the notion that this will result in PLWH not adhering to their medication.3,4,8,15 However, the longer the pandemic and accompanying restrictions continue, the less likely personal stockpiles from previous prescriptions will work to maintain sufficient ART drug supply. Additional strategies specifically adapted to the pandemic may be required to assure sufficient drug supply for PLWH.
Stockpiling of medication is likely to occur for several reasons. First, people are scheduled for refills before their previous prescription runs out, and the duration of the prescription is not adjusted for this overlap. This means that the stockpile of tablets grows with each new prescription. While we account for this starting in May 2018, some clients had stockpiles built up before May 2018 that could have carried over to the lockdown period. Second, most people do not adhere to all of their medication, which means they have extra tablets in addition to the surplus from overlapping prescriptions. When we adjust our ART supply measure with the assumption of 80% adherence (rather than perfect adherence), we find that on average people have enough supply to last for more than 2 months on any given day compared with only 1 month with the assumption of perfect adherence. Moreover, there are very few client days without ART after the lockdown when we assume 80% adherence (see Appendix Figure S4, Supplemental Digital Content, http://links.lww.com/QAI/B728).
The subsample for which we measured adherence electronically may not be representative of the Mildmay clinic population, and it is possible this group's adherence was less affected by the lockdown than the general population. This group was older and had been on ART for longer (Table 1) and both of these factors are positively associated with adherence.29–31 Moreover, this group was enrolled in a study specifically focused on measuring ART adherence and had fewer days without ART pill supply before the lockdown (Fig. 1). Thus, it remains unclear whether ART adherence of the general Mildmay population was affected by the lockdown.
ART refills are not the only reason for visiting the clinic, and barriers to access could cause harm without affecting adherence. Clinic visits include monitoring of comorbidities, laboratory tests, support services such as adherence counseling and depression care, and monitoring of ART resistance. Thus, although we do not find that the pandemic substantively affected adherence (at least in our subsample provided with electronic pill caps) or viral suppression, it is possible that there were other harmful effects that are beyond the scope of this article, such as failure to detect opportunistic infections, failure to identify the need for a regimen change, failure to identify viral rebound, and generally missing opportunity to monitor health status.
One concerning finding from this study is increased levels of food insecurity compared with the BEST study survey conducted before the start of the pandemic. Previous work suggests that food availability is one the most important factors for adhering to ART regimens because most ART medications should be consumed with food to avoid side effects.13,32 Some other recent work from Africa found an increase in food insecurity during the pandemic.33,34 If food insecurity continues to increase, this could deter some people from taking their medication or result in other adherence barriers.
We also find that the pandemic has begun to disrupt pre-existing pill-taking routines (eg, always taking medication right after coming home from work), which raises additional concerns about the future rates of meditation adherence. Both food insecurity and disruptions in daily routines are likely to persist until the pandemic is under control, which suggests that ART adherence may be negatively affected as the pandemic drags on.
This study is the first we are aware of to examine electronically measured ART adherence data and HIV clinic records during the COVID-19 pandemic. However, in addition to the limitations mentioned above, this work should be interpreted in light of several other limitations. First, we do not know the extent to which study participants continued to use their MEMS caps after the lockdown started. At least 1 participant reported not putting the MEMS cap on a pill bottle that was refilled from an external clinic. External refills were rare, however, and results are similar when we exclude participants who reported external refills (see Appendix Figure S3, Supplemental Digital Content, http://links.lww.com/QAI/B728). Second, there may be selection bias in who received viral load tests after the lockdown. If healthier clients were more likely to come into the clinic after March, this could make viral suppression seem more common than it was in actuality. Third, we were unable to ask clients directly about stockpiling, which would have added validity to our theory for why the MEMS cohort was able to adhere without visiting the clinic. Fourth, we only have complete adherence data for a subset of the sample who visited the clinic after September 2020. Finally, as in any observational study, we do not have a control group to accurately benchmark what outcomes would look like in the absence of the pandemic.
This study documents reduced access to HIV care after the onset of the COVID-19 pandemic in Uganda. The EHR data show that the lockdown reduced access to vital ART medication. Although this does not seem to have affected electronically measured ART adherence for a small subsample, the pandemic does not have a clear end in sight in low-income and middle-income countries, and the well-being of PLWH around the world should continue to be monitored. Policy makers and health care providers must come up with creative ways to continue providing essential HIV care to avoid disease progression, increased transmission, and unnecessary mortality.
ACKNOWLEDGMENTS
The authors wish to thank the Mildmay clinic and the United States and Ugandan RAND research staff. The authors are particularly grateful to our excellent study team members: Peter Wabukala, Lillian Lunkuse, Philip Aroda, Stewart Walukaga, and Pius Kimuli. The authors also extend our gratitude to Mildmay's clients who so generously provided their time and insight to make this study possible.
Footnotes
Supported by the National Institute of Mental Health (Grant: R01MH110350, PI: Linnemayr). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Clinical trial registration: ClinicalTrials.gov NCT03494777.
The authors have no conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jaids.com).
REFERENCES
- 1.Pierre G, Uwineza A, Dzinamarira T. Attendance to HIV antiretroviral collection clinic appointments during COVID-19 lockdown. A single center study in Kigali, Rwanda. AIDS Behav. 2020;24:3299–3301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Corless IB, Hoyt AJ, Tyer-Viola L, et al. 90-90-90-Plus: maintaining adherence to antiretroviral therapies. AIDS Patient Care STDS. 2017;31:227–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hogan AB, Jewell BL, Sherrard-Smith E, et al. Potential impact of the COVID-19 pandemic on HIV, tuberculosis, and malaria in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8:e1132–e1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jiang H, Zhou Y, Tang W. Maintaining HIV care during the COVID-19 pandemic. Lancet HIV. 2020;7:e308–e309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Forsberg BC, Petzold MG, Tomson G, et al. Diarrhoea case management in low- and middle-income countries--an unfinished agenda. Bull World Health Organ. 2007;85:42–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El-Sadr WM, Justman J. Africa in the path of covid-19. N Engl J Med. 2020;383:e11. [DOI] [PubMed] [Google Scholar]
- 7.Nyoni T, Okumu M. COVID-19-Compliant strategies for supporting treatment adherence among people living with HIV in sub-saharan Africa. AIDS Behav. 2020;24:2473–2476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization. The Cost of Inaction: COVID-19-Related Service Disruptions Could Cause Hundreds of Thousands of Extra Deaths from HIV; 2020. Available at: https://www.who.int/news/item/11-05-2020-the-cost-of-inaction-covid-19-related-service-disruptions-could-cause-hundreds-of-thousands-of-extra-deaths-from-hiv. [Google Scholar]
- 9.Eisinger RW, Dieffenbach CW, Fauci AS. HIV viral load and transmissibility of HIV infection: undetectable equals untransmittable. JAMA. 2019;321:451–452. [DOI] [PubMed] [Google Scholar]
- 10.Fonsah JY, Njamnshi AK, Kouanfack C, et al. Adherence to antiretroviral therapy (ART) in Yaoundé-Cameroon: association with opportunistic infections, depression, ART regimen and side effects. PLoS One. 2017;12:e0170893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Museveni Y. Fourth address on COVID19; 2020. Available at: https://www.yowerikmuseveni.com/fourth-address-covid19. Accessed September 25, 2020.
- 12.Linnemayr S, Jennings Mayo-Wilson L, Saya U, et al. HIV care experiences during the COVID-19 pandemic: mixed-methods telephone interviews with clinic-enrolled HIV-infected adults in Uganda. AIDS Behav. 2021;25:28–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saya U, Wagner Z, Linnemayr S. The role of material deprivations in determining ART adherence: evidence from a discrete choice experiment among HIV-positive adults in Uganda. 9th Annual Conference of the American Society of Health Economists; June 8–9, 2020; ASHECON. [DOI] [PMC free article] [PubMed]
- 14.Drain PK, Garrett N. SARS-CoV-2 pandemic expanding in Sub-Saharan Africa: considerations for COVID-19 in people living with HIV. EClinicalMedicine. 2020;22:100342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jewell BL, Mudimu E, Stover J, et al. Potential effects of disruption to HIV programmes in sub-Saharan Africa caused by COVID-19: results from multiple mathematical models. Lancet HIV. 2020;7:e629–e640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sanchez TH, Zlotorzynska M, Rai M, et al. Characterizing the impact of COVID-19 on men who have sex with men across the United States in April, 2020. AIDS Behav. 2020;24:2024–2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rhodes SD, Mann-Jackson L, Alonzo J, et al. A rapid qualitative assessment of the impact of the COVID-19 pandemic on a racially/ethnically diverse sample of gay, bisexual, and other men who have sex with men living with HIV in the US south. AIDS Behav. 2021;25:58–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guo W, Weng HL, Bai H, et al. Quick community survey on the impact of COVID-19 outbreak for the healthcare of people living with HIV. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:662–666. [DOI] [PubMed] [Google Scholar]
- 19.Linnemayr S, Stecher C, Saya U, et al. Behavioral economics Incentives to support HIV treatment adherence (BEST): protocol for a randomized controlled trial in Uganda. Trials. 2020;21:9–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.COVID-19 Republic of Uganda Timeline [Internet]. 2021. Available at: https://covid19.gou.go.ug/timeline.html. Accessed August 13, 2021. [Google Scholar]
- 21.Byrd KK, Hou JG, Hazen R, et al. Antiretroviral adherence level necessary for HIV viral suppression using real-world data. J Acquir Immune Defic Syndr. 2019;82:245–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nau DP. Proportion of Days Covered (PDC) as a Preferred Method of Measuring Medication Adherence. Springfield, VA: Pharmacy Quality Alliance; 2012. [Google Scholar]
- 23.Hammer SM, Squires KE, Hughes MD, et al. A controlled trial of two nucleoside analogues plus indinavir in persons with human immunodeficiency virus infection and CD4 cell counts of 200 per cubic millimeter or less. AIDS Clinical Trials Group 320 Study Team. N Engl J Med. 1997;337:725–733. [DOI] [PubMed] [Google Scholar]
- 24.Wood W, Quinn JM. Habits and the Structure of Motivation in Everyday Life. Social Motivation: Conscious and Unconscious Processes. New York, NY: Cambridge University Press; 2005:55–70. [Google Scholar]
- 25.Wood W, Quinn JM, Kashy DA. Habits in everyday life: thought, emotion, and action. J Pers Soc Psychol. 2002;83:1281–1297. [PubMed] [Google Scholar]
- 26.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46:348–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Havlir DV, Balzer LB, Charlebois ED, et al. HIV testing and treatment with the use of a community health approach in rural Africa. N Engl J Med. 2019;381:219–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wambogo EA, Ghattas H, Leonard KL, et al. Validity of the food insecurity experience scale for use in sub-Saharan Africa and characteristics of food-Insecure individuals. Curr Dev Nutr. 2018;2:nzy062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Langebeek N, Gisolf EH, Reiss P, et al. Predictors and correlates of adherence to combination antiretroviral therapy (ART) for chronic HIV infection: a meta-analysis. BMC Med. 2014;12:142–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Teasdale CA, Wang C, Francois U, et al. Time to initiation of antiretroviral therapy among patients who are ART eligible in Rwanda: improvement over time. J Acquir Immune Defic Syndr. 2015;68:314–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Larsen A, Cheyip M, Tesfay A, et al. Timing and predictors of initiation on antiretroviral therapy among newly-diagnosed HIV-infected persons in South Africa. AIDS Behav. 2019;23:375–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leddy AM, Weiser SD, Palar K, et al. A conceptual model for understanding the rapid COVID-19–related increase in food insecurity and its impact on health and healthcare. Am J Clin Nutr. 2020;112:1162–1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dear N, Duff E, Esber A, et al. Transient reductions in HIV clinic attendance and food security during the COVID-19 pandemic for people living with HIV in four African countries. Clin Infect Dis. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McLinden T, Stover S, Hogg RS. HIV and food insecurity: a syndemic amid the COVID-19 pandemic. AIDS Behav. 2020;24:2766–2769. [DOI] [PMC free article] [PubMed] [Google Scholar]


