Abstract
We report a case series of biopsy-proven reactive axillary lymph nodes, which were avid on FDG PET/CT in breast cancer patients post COVID-19 vaccination. With 4 cases presenting in a consecutive 10-day period, it became apparent that metabolically active axillary lymphadenopathy is an adverse effect of COVID-19 vaccines, currently being deployed worldwide. This may lead to patients undergoing unnecessary biopsy. We have started taking a COVID-19 vaccine status history before PET/CT. If enlarged/metabolically active axillary nodes are identified in the ipsilateral vaccinated arm, then axillary ultrasound at 4 weeks is suggested.
Key Words: COVID-19, vaccine, FDG, PET/CT, breast cancer, lymphadenopathy
FIGURE 1.
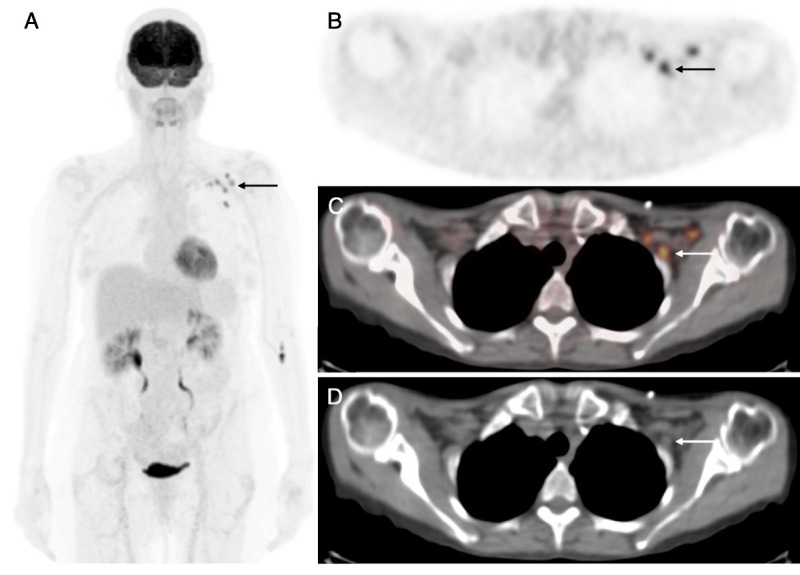
A 67-year-old woman with a history of metastatic right-sided breast cancer diagnosed 2 years previously presents for a restaging scan. 18F-FDG PET/CT images (A, MIP; B, axial PET; C, axial fused PET/CT; D, axial CT) demonstrated intense uptake in nonenlarged left axillary and subpectoral lymph nodes (A–D, arrow). The patient received the COVID-19 vaccine in the left arm 2 weeks earlier. An ultrasound-guided biopsy of the lymph node was undertaken, and histological analysis revealed benign reactive change only. The role of PET/CT in breast cancer staging and the pitfalls in interpretation is ever increasingly recognized,1–11 and in this new era of mass COVID-19 vaccination, care must be taken to interpret findings in relation to vaccine timing to avoid drawing inaccurate conclusions.12–14
FIGURE 2.
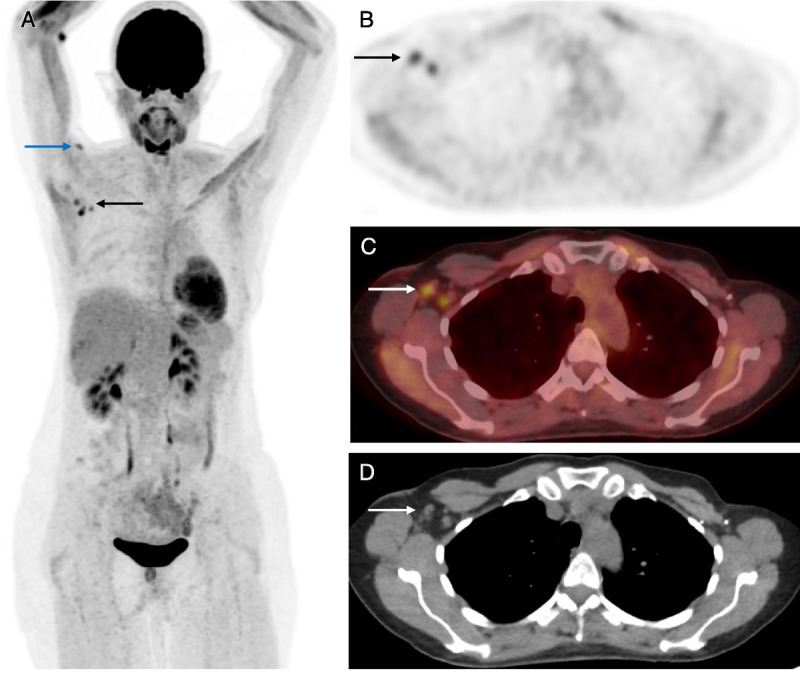
A 48-year-old woman with a history of primary left-sided breast cancer diagnosed 7 years previously and treated with left mastectomy and axillary node clearance plus risk-reducing right mastectomy and bilateral reconstruction presents for restaging scan. 18F-FDG PET/CT images (A, MIP; B, axial PET; C, axial fused PET/CT; D, axial CT) demonstrated intense uptake in nonenlarged right axillary lymph nodes (A–D, black and white arrows). The patient received the COVID-19 vaccine in the right arm 3 weeks earlier. There is a small focus of FDG avidity in the deltoid muscle in the right upper arm at the known injection site (blue arrow). This patient also underwent ultrasound-guided biopsy of the lymph node, which was shown to be reactive with no evidence of malignancy. At this time, the UK vaccination program was ahead of most other countries in the world, having offered the first dose of the vaccine to all over 70s by mid-February 2021. Being largely similar in age demographic, it became apparent that we would be seeing an increasing number of recently vaccinated patients presenting for surveillance cancer imaging. A new approach was needed to prevent unnecessary interventions, and our institution began to collect information about vaccination such as date, type, first/second dose, and arm vaccinated before PET/CT studies to avoid this pitfall in future patients.
FIGURE 3.
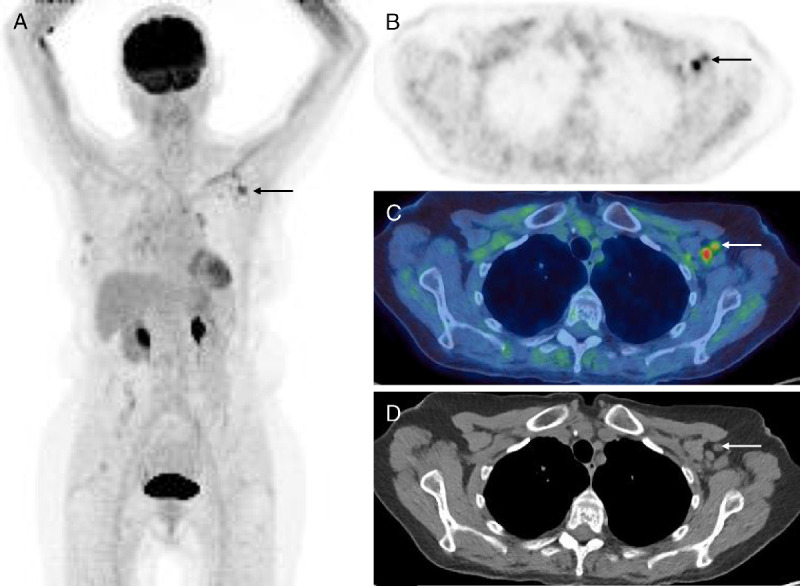
An 83-year-old woman with primary right-sided breast cancer on hormonal treatment and chemotherapy underwent routine 3-monthly follow-up 18F-FDG PET/CT. The patient had been given the COVID-19 vaccine in the left arm 2 weeks before the examination. 18F-FDG PET/CT images (A, MIP; B, axial PET; C, axial fused PET/CT; D, axial CT) demonstrated intense uptake in nonenlarged left axillary and subpectoral lymph nodes (A–D, arrow). There was unchanged intense uptake in 2 stable right breast nodules (not shown). This was yet another case of axillary lymph node avidity contralateral to the known breast cancer but ipsilateral to the recently vaccinated arm. On this occasion, however, a conservative approach was taken, and as the lymph nodes were of normal size on CT, the patient was scheduled for a follow-up ultrasound 4 weeks later. It is important to stress that if the avid lymph nodes are ipsilateral to the breast cancer, or enlarged on CT, emergent further workup with ultrasound ± biopsy is warranted.
FIGURE 4.
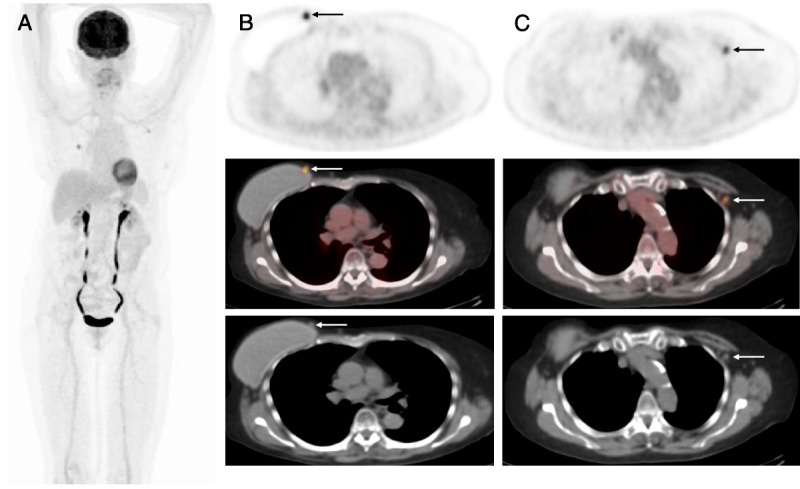
A 66-year-old woman with a history of primary right-sided breast cancer treated with right mastectomy and implant reconstruction presents for routine follow-up imaging. 18F-FDG PET/CT images (A, MIP; B and C, axial PET, fused PET/CT, and CT) demonstrated focal intense uptake in the medial aspect of the right breast adjacent to the implant in keeping with disease recurrence (B, arrow). There was also intense uptake in a nonenlarged left subpectoral lymph node (C, arrow). Further questioning revealed the patient had received the COVID-19 vaccine in the left arm less than 3 weeks earlier. Further research on clarifying the expected time course of axillary lymph node FDG avidity and associated SUV values on PET/CT is needed, especially as new COVID-19 vaccinations to target emerging variants may be introduced in the future. This will also ensure these patients are appropriately managed going forward.
Footnotes
Conflicts of interest and sources of funding: This project was supported by the NIHR UCLH Biomedical Research Centre. None declared to all authors.
Contributor Information
Sweni Shah, Email: sweni.shah@nhs.net.
Ashley M. Groves, Email: ashleygroves@nhs.net.
Simon Wan, Email: mwan@nhs.net.
Anmol Malhotra, Email: anmolmalhotra@nhs.net.
REFERENCES
- 1.Groves AM Shastry M Ben-Haim S, et al. Defining the role of PET-CT in staging early breast cancer. Oncologist. 2012;17:613–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vatsa R Singh SS Ashwathanarayana AG, et al. Breast cancer imaging with PET based radiopharmaceuticals other than 18F-FDG. Clin Nucl Med. 2020;45:e72–e76. [DOI] [PubMed] [Google Scholar]
- 3.Dong A Wang Y Lu J, et al. Spectrum of the breast lesions with increased 18F-FDG uptake on PET/CT. Clin Nucl Med. 2016;41:543–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nursal GN Nursal TZ Aytac HO, et al. Is PET/CT necessary in the management of early breast cancer? Clin Nucl Med. 2016;41:362–365. [DOI] [PubMed] [Google Scholar]
- 5.Bakheet SM Powe J Kandil A, et al. F-18 FDG uptake in breast infection and inflammation. Clin Nucl Med. 2000;25:100–103. [DOI] [PubMed] [Google Scholar]
- 6.Nishimura S Koizumi M Kawakami J, et al. Contralateral axillary node metastasis from recurrence after conservative breast cancer surgery. Clin Nucl Med. 2014;39:181–183. [DOI] [PubMed] [Google Scholar]
- 7.Bhargava P, Glass E, Ghesani M. Inflammatory F-18 FDG uptake secondary to ruptured breast prosthesis. Clin Nucl Med. 2006;31:227–228. [DOI] [PubMed] [Google Scholar]
- 8.Hurwitz R. F-18 FDG positron emission tomographic imaging in a case of ruptured breast implant: inflammation or recurrent tumor? Clin Nucl Med. 2003;28:755–756. [DOI] [PubMed] [Google Scholar]
- 9.Johnson DS, Wong JT, Coel MN. False-positive positron emission tomographic scan for recurrent breast cancer resulting from a bee sting. Clin Nucl Med. 1999;24:702–703. [DOI] [PubMed] [Google Scholar]
- 10.Bhargava P Zhuang H Kumar R, et al. Iatrogenic artifacts on whole-body F-18 FDG PET imaging. Clin Nucl Med. 2004;29:429–439. [DOI] [PubMed] [Google Scholar]
- 11.Park J Byun BH Noh WC, et al. Lymph node to primary tumor SUV ratio by 18F-FDG PET/CT and the prediction of axillary lymph node metastases in breast cancer. Clin Nucl Med. 2014;39:e249–e253. [DOI] [PubMed] [Google Scholar]
- 12.Doss M Nakhoda SK Li Y, et al. COVID-19 vaccine-related local FDG uptake. Clin Nucl Med. 2021. [DOI] [PubMed] [Google Scholar]
- 13.Xu G, Lu Y. COVID-19 mRNA vaccination–induced lymphadenopathy mimics lymphoma progression on FDG PET/CT. Clin Nucl Med. 2021;46:353–354. [DOI] [PubMed] [Google Scholar]
- 14.Ahmed N Muzaffar S Binns C, et al. COVID-19 vaccination manifesting as incidental lymph nodal uptake on 18F-FDG PET/CT. Clin Nucl Med. 2021. [DOI] [PubMed] [Google Scholar]


