Abstract
Objectives:
To compare inpatient compliance with venous thromboembolism prophylaxis regimens.
Design:
A secondary analysis of patients enrolled in the ADAPT (A Different Approach to Preventing Thrombosis) randomized controlled trial.
Setting:
Level I trauma center.
Patients/Participants:
Patients with operative extremity or any pelvic or acetabular fracture requiring venous thromboembolism prophylaxis.
Intervention:
We compared patients randomized to receive either low molecular weight heparin (LMWH) 30 mg or aspirin 81 mg BID during their inpatient admission.
Main Outcome Measurements:
The primary outcome measure was the number of doses missed compared with prescribed number of doses.
Results:
A total of 329 patients were randomized to receive either LMWH 30 mg BID (164 patients) or aspirin 81 mg BID (165 patients). No differences observed in percentage of patients who missed a dose (aspirin: 41.2% vs LMWH: 43.3%, P = .7) or mean number of missed doses (0.6 vs 0.7 doses, P = .4). The majority of patients (57.8%, n = 190) did not miss any doses. Missed doses were often associated with an operation.
Conclusions:
These data should reassure clinicians that inpatient compliance is similar for low molecular weight heparin and aspirin regimens.
Keywords: aspirin, low molecular weight heparin, trauma, venous thromboembolism prophylaxis
1. Introduction
Pulmonary embolism (PE) is one of the most common causes of death in trauma patients who survive beyond the first 24 hours after injury.[1–4] Orthopaedic trauma patients, in particular, are at extremely high risk for venous thromboembolism (VTE).[2,5–9] Fortunately, VTE chemoprophylaxis can significantly reduce VTE risk in these patients; however, guidelines on which prophylaxis regimen is best for this population are ambiguous due to limited quality evidence. Treatment courses with LMWH and aspirin are 2 of the most commonly prescribed regimens.[9–14]
The Eastern Association for the Surgery of Trauma (EAST) and the American College of Chest Physicians (ACCP) recommend LMWH for VTE prophylaxis in trauma patients. However, many orthopaedic surgeons prefer an aspirin regimen based on studies performed mostly in the arthroplasty literature that have found aspirin could be equally effective at VTE prevention with reduced risk of wound and bleeding complications.[12,15–21] As a result, aspirin is now included in the ACCP guidelines as an option for chemoprophylaxis after high-risk orthopaedic surgery.[14] Data specific to orthopaedic trauma patients is limited. As a result, the Orthopaedic Trauma Association Evidence-Based Quality Value and Safety Committee reported there exists wide variability in prescribed regimens and emphasized the need for standardized guidelines to improve care.[22]
Since trauma patients likely have even higher VTE and bleeding risk, there is a need to evaluate effectiveness and complication rates associated with these 2 regimens in this population. Regimen compliance is critical to preventing VTE events and should be considered when creating guidelines. Unfortunately, few studies have evaluated compliance with these specific regimens in orthopaedic trauma patients during the index admission and, to our knowledge, there has been no direct comparison of inpatient compliance with aspirin to LMWH for VTE prophylaxis in orthopaedic trauma patients.
Given the lack of clear guidelines, known difficulties with compliance, and large differences in baseline characteristics of the medications used for prophylaxis, an in-depth comparison of compliance with these medications is needed. This comparison will be helpful for clinicians to understand barriers to treatment and for researchers who take an explanatory approach to comparing the effectiveness of these medications in the future. The objective of this study was to compare overall compliance with our institution's inpatient VTE prophylaxis guidelines for aspirin versus LMWH VTE prophylaxis regimens in orthopaedic trauma patients. The secondary objective was to identify factors associated with missed VTE prophylaxis doses and the discontinuance of VTE prophylaxis in this patient population including factors related to patient compliance as well as barriers to provider or system compliance with guidelines. We hypothesized that VTE prophylaxis compliance would be lower in the LMWH group than in the aspirin group.
2. Materials and methods
This study was conducted as a secondary analysis of patients enrolled in the ADAPT (A Different Approach to Preventing Thrombosis) randomized controlled trial as registered on clinicaltrials.gov (Identifier: NCT02774265).[23] All adult (age ≥18 years) trauma patients presenting to the R Adams Cowley Shock Trauma Center from January 19, 2016 to October 31, 2016 with an operative extremity fracture proximal to the metatarsals/carpals or any pelvic or acetabular fracture requiring VTE prophylaxis were included in the trial. Prisoners, pregnant patients, non-English-speaking patients, and patients on pre-existing anticoagulation (not including antiplatelet agents), with an indication for therapeutic anticoagulation or aspirin dose greater than 81 mg daily, or with a contraindication to either prophylaxis regimen were excluded. Eligible patients were approached on admission and before the third dose of prophylaxis. Informed consent was obtained as required for all enrolled patients. This study was approved by our Institutional Review Board (IRB).
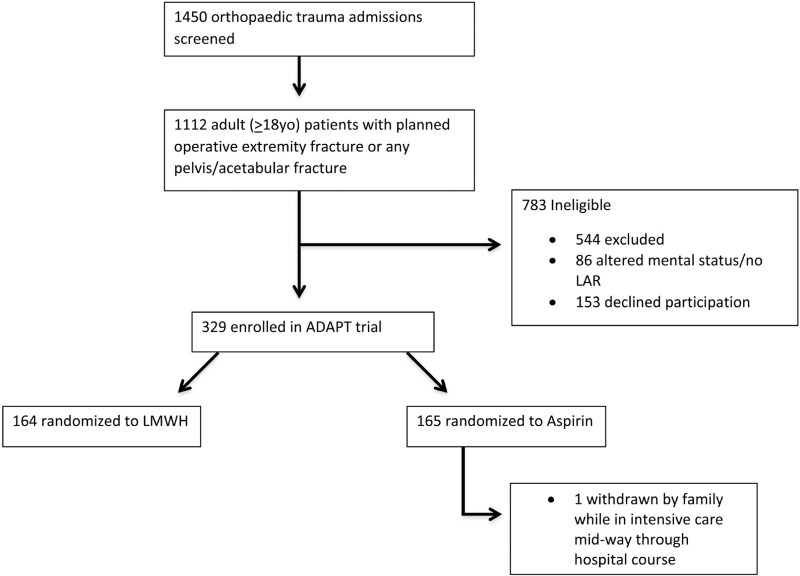
Enrolled patients were randomized to receive either LMWH 30 mg BID (with allowance for dose adjustment according to body mass index) or aspirin 81 mg BID for the remainder of their VTE prophylaxis course. BID dosing is administered at 10 am and 10 pm typically at our institution. However, for patients who have a dose of medication automatically held in a procedure, a provider can reschedule the dose to occur before or after the procedure if noticed and desired. Of note, aspirin is not considered a standard of care treatment regimen at this time in polytrauma patients and the off-label use of 81 mg aspirin for the indication of VTE prophylaxis was approved by the IRB of record. Randomization was carried out in the study's REDCap database at the time of consent with 1:1 allocation ratio and block sizes of 6. After randomization, the study team notified the clinical team of the patient's enrollment status and treatment arm. The clinical team was responsible for ordering the chemoprophylaxis for study patients. The study team, clinical team, and patients were not blinded to their treatment arm. Of 482 patients who met the eligibility criteria, 329 (68.3%) patients consented to enroll in study: 164 randomized to LMWH and 165 to aspirin (Fig. 1).
Figure 1.
CONSORT diagram.
The timing of initiation and duration of prophylaxis was determined by the treating physician as indicated by the patient's injuries and clinical course. Enrolled patients were followed prospectively during their inpatient admission. A general surgery resident with experience rotating on the trauma service performed, at a minimum, once daily checks of patient orders and the medication administration record. The timing of prophylaxis initiation, number of missed doses, reasons for missed doses, and reasons for discontinuation, delay, or physician holding of prophylaxis were recorded. In addition, data on the doses of nonallocated medications with the reason for administration were collected. Any time an ordered dose is missed, the study center's medication administration record requires the nurse enter a reason the dose was held. This documented reason was used to determine why the dose was missed. Cases with an uncertain reason for missed prophylaxis or administration of nonallocated prophylaxis were discussed on a daily basis with the primary clinical team and nursing staff.
Our primary outcome measure was the number of doses missed compared with the number of prescribed doses. Intention-to-treat analysis was performed. Patient demographics, clinical characteristics, and compliance were compared by intention-to-treat regimen group using Student t tests for normally distributed continuous variables and Wilcoxon rank-sum tests for nonparametric continuous variables. Fisher exact tests and Chi-squared tests were used to compare nominal data.
3. Results
Three hundred twenty-nine patients were enrolled (164 LMWH, 165 aspirin) (Fig. 1). The majority of participants were male (n = 223, 67.8%) with a mean age of 46.7 years (range 18–93, SD 19.5), mean Injury Severity Score (ISS) 11.0 (range 1–41, SD 6.2), and a median Trauma and Injury Severity Score (TRISS) of 0.99 (range 0–0.996). Overall, 26.5% had multiextremity orthopaedic trauma. The baseline characteristics were similar between the 2 treatment groups, with the exception of patient sex (P = .06) and the proportion of patients with peptic ulcers (P = .02) (Table 1). Patients were inpatients for a median of 9 days (range 0–43, mean 9.6 days), with no difference between the treatment groups (LMWH, 9.8 days ± 7.3; aspirin 9.6 days ± 7.3, P = .86).
Table 1.
Baseline characteristics
| Aspirin(n = 165) | LMWH(n = 164) | Total(n = 329) | |
|---|---|---|---|
| Age (years) | 48.0 (18.6) | 45.4 (20.4) | 46.7 (19.5) |
| Sex | |||
| Male | 104 (63.0) | 119 (72.6) | 223 (67.8) |
| Female | 61 (37.0) | 45 (27.4) | 106 (32.2) |
| Race | |||
| White | 106 (64.2) | 97 (59.5) | 203 (61.9) |
| Black | 45 (27.3) | 53 (3.3) | 98 (29.9) |
| Hispanic | 5 (3.0) | 2 (1.2) | 7 (2.1) |
| Mixed | 3 (1.8) | 6 (3.7) | 9 (2.7) |
| Other | 6 (3.6) | 5 (3.1) | 11 (3.3) |
| Current smoker | 65 (39.3) | 62 (38.3) | 127 (38.8) |
| History of VTE | 8 (4.8) | 7 (4.3) | 15 (4.6) |
| Comorbidities | |||
| Peptic ulcer | 12 (7.2) | 3 (1.8) | 15 (4.6) |
| Diabetes | 17 (10.3) | 16 (9.8) | 33 (10.0) |
| Active cancer | 5 (3.0) | 2 (1.2) | 7 (2.1) |
| Immunosuppressed | 8 (4.8) | 9 (5.5) | 17 (5.2) |
| Additional medications | |||
| Aspirin, daily preinjury | 22 (13.3) | 23 (14.0) | 45 (13.7) |
| Plavix, preinjury | 1 (0.6) | 2 (1.2) | 3 (0.9) |
| OCP/estrogen | 3 (1.8) | 3 (1.8) | 6 (1.8) |
| BMI | |||
| Underweight (<18.5) | 6 (3.7) | 4 (2.5) | 10 (3.1) |
| Normal weight (18.5–24.9) | 57 (35.0) | 57 (35.0) | 114 (65.0) |
| Overweight (25.0–-29.9) | 47 (28.8) | 53 (32.5) | 100 (30.7) |
| Obese (≥30.0) | 53 (32.5) | 49 (30.1) | 102 (31.3) |
| ISS | 11.0 (6.6) | 11.0 (5.7) | 11.0 (6.2) |
| Mechanism of injury | |||
| Blunt | 148 (97.4) | 147 (94.2) | 295 (95.8) |
| Penetrating | 2 (1.3) | 7 (4.5) | 9 (2.9) |
| Other | 2 (1.3) | 2 (1.3) | 4 (1.3) |
| Open fracture | 37 (22.4) | 39 (23.4) | 76 (23.1) |
| Fracture location | |||
| Upper extremity | 42 (25.5) | 41 (25.0) | 83 (25.2) |
| Lower extremity and pelvis/acetabular | 154 (93.3) | 149 (90.9) | 303 (92.1) |
| Multi-limb | 43 (26.1) | 44 (27.0) | 87 (26.5) |
| Nonorthopaedic injury (AIS ≥2) | |||
| Abdomen | 17 (10.3) | 14 (8.5) | 31 (9.4) |
| Head | 35 (21.2) | 36 (22.0) | 71 (21.6) |
| Chest | 39 (23.6) | 43 (26.2) | 82 (24.9) |
VTE prophylaxis was initiated on average within the first 48 hours in the hospital course, and slightly faster for the LMWH group (LMWH: 0.9 days vs. aspirin: 1.2 days, P = .01) (Table 2). Overall, patients were on inpatient VTE prophylaxis for 9.7 days (SD 7.3), with no difference between the treatment groups (P = .86). Overall, patients missed less than 1 dose (mean 0.6, SD 0.9), with no observed difference between the LMWH group (mean 0.7, SD 1.0) or aspirin group (mean 0.6, SD 0.8, P = .45). Of total number of prescribed inpatient doses, 3.9% were missed with no difference between the groups (LMWH 4.3% vs. aspirin 3.5%, P = .30).
Table 2.
VTE prophylaxis dosing characteristics
| Dosing characteristic | All(n = 29) | Aspirin(n = 165) | LMWH(n = 164) | P value |
|---|---|---|---|---|
| Days from admission to allocated prophylaxis administration, mean (SD) | 1.0 (0.8) | 1.2 (0.8) | 0.9 (0.8) | .01 |
| Total number of inpatient days on prophylaxis, mean (SD) | 9.7 (7.3) | 9.6 (7.3) | 9.8 (7.3) | .86 |
| Number of missed inpatient doses, mean (SD) | 0.6 (0.9) | 0.6 (0.8) | 0.7 (1.0) | .45 |
| Proportion of inpatient doses missed, mean % (SD) | 3.9 (7.2) | 3.5 (6.5) | 4.3 (7.9) | .30 |
The most common reason for missed inpatient VTE prophylaxis was perioperative holding of prophylaxis (n = 136, 66.0%) (Table 3). Of note, typical practice at the study institution is to not hold aspirin doses preoperatively since the half-life is long enough that holding 1 dose would not have an effect. For LWMH, the decision to hold a perioperative dose is at the discretion of the clinical treating team and depends on the planned operation. The inability to administer enteral medication was an issue specific to patients on aspirin VTE prophylaxis (aspirin: 15.5% vs. LMWH: 0%, P < .01). The most common reason for the inability to administer enteric aspirin was physician ordering error in which the wrong form or route of the drug was ordered (eg, oral administration in a patient who is intubated with no feeding tube instead of per rectum).
Table 3.
Most common reasons for missed inpatient VTE prophylaxis doses
| Reasons for missed doses | AllMissed doses(n = 206) | AspirinMissed doses(n = 97) | LMWHMissed doses(n = 109) | P value |
|---|---|---|---|---|
| In a procedure or awaiting a procedure that requires prophylaxis to be held, n (%) | 136 (66.0) | 57 (58.8) | 79 (72.5) | .05 |
| Systematic issue, n (%) | 30 (14.6) | 16 (16.5) | 14 (12.8) | .58 |
| Patient refused dose, n (%) | 25 (12.1) | 9 (9.3) | 16 (14.7) | .33 |
| Inability to administer enteral medication, n (%) | 15 (7.3) | 15 (15.5) | 0 (0) | <.01 |
Only 6.1% (n = 20) of patients had their assigned prophylaxis stopped during their inpatient course with no significant difference between treatment arms (P = .1). The most common reason for stopping prophylaxis was a new indication for therapeutic anticoagulation (60.0%) (Table 4).
Table 4.
Reasons for stopping inpatient VTE prophylaxis by treatment arm
| Reasons for stopping allocated regimen | All(n = 20) | Aspirin(n = 6) | LMWH(n = 14) | P value |
|---|---|---|---|---|
| New indication for therapeutic anticoagulation, n (%) | 12 (60.0) | 4 (66.7) | 8 (57.1) | .19 |
| Patient refusal of further injections, n (%) | 2 (10.0) | 0 (0) | 2 (14.3) | .25 |
| Accidental prescription of non-allocated prophylaxis, n (%) | 2 (10.0) | 0 (0) | 2 (14.4) | .25 |
| Acute kidney injury, n (%) | 1 (5.0) | 0 (0) | 1 (7.1) | .50 |
| Change in regimen by attending surgeon for sterile wound drainage, n (%) | 1 (5.0) | 0 (0) | 1 (7.1) | .50 |
| Gastrointestinal bleed, n (%) | 1 (5.0) | 1 (16.7) | 0 (0) | .50 |
| Study withdrawal due to family concerns about medication efficacy, n (%) | 1 (5.0) | 1 (16.7) | 0 (0) | .50 |
Finally, 10.6% of patients (n = 35) received at least 1 dose of the nonassigned prophylaxis regimen postrandomization without a medical indication for the change in prophylaxis. However, no significant difference was observed in inpatient crossover rates between treatment arms (P = .6).
4. Discussion
Poor medication adherence is a well-described problem resulting in billions of dollars per year in excess health care costs, and care in the trauma patient population is notorious for low compliance.[24–26] Lack of compliance with VTE prophylaxis can have particularly concerning consequences including fatal PE. In the ongoing debate on what is the best VTE prophylaxis regimen in the orthopaedic trauma population, it is important to consider compliance in addition to efficacy. To our knowledge, this is the first study to directly compare inpatient compliance with 2 of the most commonly prescribed VTE chemoprophylaxis regimens (twice daily LMWH and twice daily aspirin) in the orthopaedic trauma population.
Previous studies have reported low overall compliance rates with ACCP guidelines with the majority of at-risk patients who subsequently develop a VTE failing to receive appropriate ACCP-recommended prophylaxis during their index admission.[27–32] In the outpatient setting, studies in orthopaedic patients have demonstrated varying nonadherence rates to LMWH (up to 40%) with patients missing up to 50% of their doses.[32–36] Compliance in our study was higher than previously reported. VTE chemoprophylaxis was initiated early in the hospital course, and missed doses were uncommon. Doses of nonallocated prophylaxis without a clinical indication for the change in prophylaxis were also relatively low at just below 11% of patients receiving a dose of nonallocated VTE prophylaxis. The higher compliance seen in our study could be a result of Hawthorne effect because of the prospective study design. As part of the study protocol, rounding lists for the trauma teams were updated to include assigned VTE prophylaxis, and daily checks of patient orders and medication administration records were performed. When prophylaxis initiation was delayed, doses were missed, or orders were discontinued for unclear reasons the clinical team was contacted to provide a reason. This notification could alert a team of potential noncompliance on a daily basis allowing for the team to correct any errors in medication orders. Clinicians could consider integrating similar measures into daily care outside of this study to improve compliance and ultimately reduce VTE event rates since delays in chemoprophylaxis initiation and missed doses are associated with increased VTE events.[29,30,37] Alternatively, the greater percentage of missed doses reported in previous studies could be because some of those studies retrospectively reviewed charts of patients who developed VTE. Since missed doses are associated with increased VTE event rates, compliance is likely lower in that population.
We did not observe a significant difference in compliance between regimens. LMWH chemoprophylaxis was initiated slightly earlier than aspirin chemoprophylaxis, but there was no difference in duration of chemoprophylaxis or number of missed doses during the index admission. The small difference in timing of initiation might be because LMWH was our center's standard of care choice of prophylaxis before study initiation. Chemoprophylaxis doses were most commonly missed in the perioperative period either because a nurse decided to hold the prophylaxis dose before surgery or because the patient was in the operating room at the time the dose was due. The independent decision to hold prophylaxis by a nurse could actually cause harm by withholding the medication when the patient needs it most and is an area for potential education to improve compliance and VTE outcomes. Patient refusal, conversely, was a much less common reason for missed doses than that reported in the literature. Shermock et al[27] reported that almost half of all missed prophylaxis doses were a result of patient refusal. This discrepancy could be due to selection bias in which patients who are more likely to refuse chemoprophylaxis might have refused to participate in the study. Alternatively, the informed consent process can lead to a Hawthorne effect where patients are less inclined to refuse chemoprophylaxis after receiving education on the reason for prophylaxis including prevention of fatal PE. If this is the case, interventions to provide patient education and medication awareness on admission could be another mechanism to improve inpatient compliance.
Reasons for missed doses did not differ between regimens, except only patients on the aspirin regimen missed doses because of an inability for enteric administration usually caused by a physician ordering the incorrect form or route of the dose. The study allowed for any available route of administration including oral, crushed through a feeding tube and rectal. This barrier is one that would need to be addressed in future studies on efficacy and in practice with provider education if the aspirin regimen is used. A nonsignificant trend toward the LMWH group having more perioperative missed doses was also observed.
Surprisingly, no differences in refusal rates between regimens were observed in our study. Previous studies have documented a strong patient preference for medications with oral administration over subcutaneous injection, raising the question of whether administration route might contribute to poor adherence.[29,38–40] However, existing studies comparing adherence patterns with oral vs. injected chemoprophylaxis regimens are few with mixed results. Berggvist et al found that injection was not a barrier to good compliance, whereas Peidro-Garcés et al found patients on an oral regimen were more compliant.[35,36] We found that patients on the aspirin regimen refused medication doses just as frequently as patients randomized to the LMWH regimen. The lack of association of route with refusal rates in our study might again be caused by a combination of selection bias and patient education during the informed consent process. A previous study at our center found that patients were quick to change their medication route preference for only a small reduction in risk of fatal PE.[40] Perhaps educating patients on the risk of fatal PE without chemoprophylaxis negates any pre-existing medication route preference.
As part of a pragmatic trial, our study did not include a built-in protocol for when patients refused a dose. Typically at our institution, the nurse will go to administer the medication and if a patient refuses the nurse will document the refusal. The nurse may choose to notify the resident or midlevel provider of the refusal but there is no guarantee that this happens each time a dose is refused. Once a provider is notified, he or she may discuss risks and benefits of such refusal with a patient, but again this is at the discretion of the individual provider. One limitation of this pragmatic study was that we were unable to track the response to refusal patterns.
Strengths of this study include the prospective randomized design and the large sample size in this complex patient population. Our study was limited by its single-center design. It was conducted at a high-volume academic level I trauma center and might not be generalizable to other health care systems or different patient populations. As mentioned earlier, compliance rates in the study could also be falsely elevated as a result of selection bias and Hawthorne effect from study interventions. However, any improvement in compliance caused by these factors would most likely affect compliance rates with both regimens equally. Finally, this study was a secondary analysis of the ADAPT randomized control trial and might be underpowered for some results and was not powered to determine effect of noncompliance on VTE event rates. However, previously published studies[30,31] have shown a direct correlation between missed doses and VTE events so although we did not power our study to evaluate for this outcome, we would expect noncompliance to affect VTE event rates. Despite these limitations, our study addresses an important question that could affect the efficacy of chemoprophylaxis and the results should be considered when creating guidelines for this patient population.
5. Conclusion
In conclusion, inpatient VTE prophylaxis compliance was similar for aspirin and LMWH in this randomized trial. Missed doses were most often associated with an operative procedure; however, patient refusal and inability to give enteric medications also contributed. Percent of patients receiving nonallocated chemoprophylaxis was relatively low at around 11%. These data should help reassure clinicians that these medicines likely have similar inpatient compliance and also prove crucial to investigators designing larger trials to explore the efficacy of these medicines.
Acknowledgments
The ADAPT investigators:R Adams Cowley Shock Trauma Center, University of Maryland School of Medicine, Baltimore, Maryland, USA: Bryce E. Haac, Nathan N. O’Hara, Gerard P. Slobogean, Robert V. O’Toole, Richard Van Besien, Dimitrius Marinos, Yasmin Degani, Peter Z. Berger, George B. Reahl, Daniel Mascarenhas, Daniel Connelly, Thomas M. Scalea, Deborah M. Stein, Theodore T. Manson
McMaster University, Hamilton, Ontario: Herman Johal
References
- 1.Shackford SR, Moser KM. Deep venous thrombosis and pulmonary embolism in trauma patients. J Intensive Care Med. 1988;3:87–98. [Google Scholar]
- 2.Geerts WH, Code KI, Jay RM, et al. A prospective study of venous thromboembolism after major trauma. N Engl J Med. 1994;331:1601–1606. [DOI] [PubMed] [Google Scholar]
- 3.O’Malley KF, Ross SE. Pulmonary embolism in major trauma patients. J Trauma. 1990;30:748–750. [DOI] [PubMed] [Google Scholar]
- 4.Sevitt S, Gallagher N. Venous thrombosis and pulmonary embolism. A clinico-pathological study in injured and burned patients. Br J Surg. 1961;48:475–489. [DOI] [PubMed] [Google Scholar]
- 5.Shackford SR, Davis JW, Hollingsworth-Fridlund P, et al. Venous thromboembolism in patients with major trauma. Am J Surg. 1990;159:365–369. [DOI] [PubMed] [Google Scholar]
- 6.Abelseth G, Buckley RE, Pineo GE, et al. Incidence of deep-vein thrombosis in patients with fractures of the lower extremity distal to the hip. J Orthop Trauma. 1996;10:230–235. [DOI] [PubMed] [Google Scholar]
- 7.Rogers FB. Venous thromboembolism in trauma patients: a review. Surgery. 2001;130:1–12. [DOI] [PubMed] [Google Scholar]
- 8.Hak DJ. Prevention of venous thromboembolism in trauma and long bone fractures. Curr Opin Pulm Med. 2001;7:338–343. [DOI] [PubMed] [Google Scholar]
- 9.Hill J, Treasure T. National Clinical Guideline Centre for Acute and Chronic Conditions. Reducing the risk of venous thromboembolism in patients admitted to hospital: summary of NICE guidance. BMJ. 2010;340:c95. [DOI] [PubMed] [Google Scholar]
- 10.Drescher FS, Sirovich BE, Lee A, et al. Aspirin versus anticoagulation for prevention of venous thromboembolism major lower extremity orthopedic surgery: a systematic review and meta-analysis. J Hosp Med. 2014;9:579–585. [DOI] [PubMed] [Google Scholar]
- 11.Mont MA, Jacobs JJ. Preventing venous thromboembolic disease in patients undergoing elective hip and knee arthroplasty. J Am Acad Orthop Surg. 2011;19:768–776. [DOI] [PubMed] [Google Scholar]
- 12.Anderson DR, Dunbar MJ, Bohm ER, et al. Aspirin versus low-molecular-weight heparin for extended venous thromboembolism prophylaxis after total hip arthroplasty: a randomized trial. Ann Intern Med. 2013;158:800–806. [DOI] [PubMed] [Google Scholar]
- 13.Sahebally SM, Healy D, Walsh SR. Aspirin in the primary prophylaxis of venous thromboembolism in surgical patients. Surgeon. 2015;13:348–358. [DOI] [PubMed] [Google Scholar]
- 14.Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopaedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141 (2 suppl):e278S–325S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rogers FB, Cipolle MD, Velmahos G, et al. Practice management guidelines for the prevention of venous thromboembolism in trauma patients: the EAST practice management guidelines work group. J Trauma. 2002;53:142–164. [DOI] [PubMed] [Google Scholar]
- 16.Collaborative overview of randomised trials of antiplatelet therapy—III: Reduction in venous thrombosis and pulmonary embolism by antiplatelet prophylaxis among surgical and medical patients. BMJ. 1994;308:235–246. [PMC free article] [PubMed] [Google Scholar]
- 17.Group PEPPTC. Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: pulmonary embolism prevention (PEP) trial. Lancet. 2000;355:1295–1302. [PubMed] [Google Scholar]
- 18.Bozic KJ, Vail TP, Pekow PS, et al. Does aspirin have a role in venous thromboembolism prophylaxis in total knee arthroplasty patients? J Arthroplasty. 2010;25:1053–1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vulcano E, Gesell M, Esposito A, et al. Aspirin for elective hip and knee arthroplasty: a multimodal thromboprophylaxis protocol. Int Orthop. 2012;36:1995–2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raphael IJ, Tischler EH, Huang R, et al. Aspirin: an alternative for pulmonary embolism prophylaxis after arthroplasty? Clin Orthop Relat Res. 2013;472:482–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gehling H, Giannadakis K, Lefering R, et al. [Prospective randomized pilot study of ambulatory prevention of thromboembolism. 2 times 500 mg aspirin (ASS) vs. clivarin 1750 (NMH)]. Unfallchirurg. 1998;101:42–49. [DOI] [PubMed] [Google Scholar]
- 22.Sagi HC, Ahn J, Ciesla D, et al. Venous thromboembolism prophylaxis in orthopaedic trauma patients: a survey of OTA member practice patterns and OTA expert panel recommendations. J Orthop Trauma. 2015;29:e355–e362. [DOI] [PubMed] [Google Scholar]
- 23. US National Institute of Health. ClinicalTrials.gov Registry. Available at: https://clinicaltrials.gov/ct2/show/NCT02774265. Accessed June 29, 2017. [Google Scholar]
- 24.Kripalani S, Yao X, Haynes B. Interventions to enhance medication adherence in chronic medical conditions. Arch Intern Med. 2007;167:540–549. [DOI] [PubMed] [Google Scholar]
- 25.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. [DOI] [PubMed] [Google Scholar]
- 26.Rayan N, Barnes S, Fleming N, et al. Barriers to compliance with evidence-based care in trauma. J Trauma Acute Care Surg. 2012;72:585–592. [DOI] [PubMed] [Google Scholar]
- 27.Shermock KM, Lau BD, Haut ER, et al. Patterns of non-administration of ordered doses of venous thromboembolism prophylaxis: implications for novel intervention strategies. PLoS One. 2013;8:e66311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haut ET, Lau BD, Kraus PS, et al. Preventability of hospital-acquired venous thromboembolism. JAMA Surg. 2015;150:912–915. [DOI] [PubMed] [Google Scholar]
- 29.Louis SG, Sato M, Geraci T, et al. Correlation of missed doses of enoxaparin with increased incidence of deep vein thrombosis in trauma and general surgery patients. JAMA Surg. 2014;149:365–370. [DOI] [PubMed] [Google Scholar]
- 30.Wiseman DN, Harrison J. A retrospective review of the use of thrombopropylaxis in patients who subsequently developed a venous thromboembolism after discharge from hospital. N Z Med J. 2010;123:37–49. [PubMed] [Google Scholar]
- 31.Yu HT, Dylan ML, Lin J, et al. Hospitals’ compliance with prophylaxis guidelines for venous thromboembolism. Am J Health Syst Pharm. 2007;64:69–76. [DOI] [PubMed] [Google Scholar]
- 32.Colwell CW, Jr, Pulido P, Hardwick ME, et al. Patient compliance with outpatient prophylaxis: an observational study. Orthopedics. 2005;28:143–147. [DOI] [PubMed] [Google Scholar]
- 33.Wilke T, Moock J, Muller S, et al. Nonadherence in outpatient thrombosis prophylaxis with low molecular weight heparins after major orthopedic surgery. Clin Orthop Relat Res. 2010;468:2437–2453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Karlinski M, Stolarczyk A, Siuda M, et al. Compliance with low molecular weight heparin in ambulatory orthopedic patients. Ortop Traumatol Rehabil. 2006;8:633–638. [PubMed] [Google Scholar]
- 35.Piedro-Garces L, Otero-Fernandez R, Lozano-Lizarraga L. Adherence to and satisfaction with oral outpatient thrombosmbolism prophylaxis compared to parenteral: SALTO study. Rev Esp Cir Ortop Traumatol. 2013;57:53–60. [DOI] [PubMed] [Google Scholar]
- 36.Bergqvist D, Arcelus JI, Felicissimo P, et al. Post-discharge compliance to venous thromboembolism prophylaxis in high-risk orthopaedic surgery: results from the ETHOS registry. Thromb Haemost. 2012;107:280–287. [DOI] [PubMed] [Google Scholar]
- 37.Byrne JP, Manson SA, Gomez D, et al. Timing of pharmacologic venous theromboembolism prophylaxis in severe traumatic brain injury: a propensity-matched cohort study. J Am Coll Surg. 2016;223: 621–631.e5. [DOI] [PubMed] [Google Scholar]
- 38.Wong A, Kraus PS, Lau BD, et al. Patient preferences regarding pharmacologic venous thromboembolism prophylaxis. J Hosp Med. 2015;10:108–111. [DOI] [PubMed] [Google Scholar]
- 39.Jin J, Sklar GE, Min Sen Oh V, et al. Factors affecting therapeutic compliance: a review from the patient's perspective. Ther Clin Risk Manag. 2008;4:269–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Haac BE, O’Hara NN, Mullins CD, et al. Patient preferences for venous thromboembolism prophylaxis after injury: a discrete choice experiment. BMJ Open. 2017;7:e016676. [DOI] [PMC free article] [PubMed] [Google Scholar]