Supplemental Digital Content is available in the text.
Keywords: candidate gene approach, coronavirus disease 2019, gene polymorphisms, severe acute respiratory syndrome coronavirus 2, severity
IMPORTANCE:
The pathology caused by the coronavirus disease 2019 is mediated by host-mediated lung inflammation, driving severity, and mortality. Polymorphisms in genes encoding host inflammation and immune-related molecules may be associated with the development of serious pathologies, and identifying such gene polymorphisms may lead to the identification of therapeutic targets.
OBJECTIVES:
We attempted to identify aggravation-predicting gene polymorphisms.
DESIGN:
We use a candidate gene approach associated with multiple phase pathogenesis in coronavirus disease 2019 patients among a cohort in Hiroshima, a city with a population of 1 million, in Japan. DNA samples from the study populations were genotyped for 34 functional polymorphisms from 14 distinct candidate genes, which encode proteins related to viral cell entry, regulation of viral replication, innate immune modulators, regulatory cytokines, and effector cytokines.
SETTING AND PARTICIPANTS:
Three core hospitals providing different services for patients with coronavirus disease 2019 under administrative control. A total of 230 patients with coronavirus disease 2019 were recruited from March 1, 2020, to March 31, 2021.
MAIN RESULTS AND MEASUREMENTS:
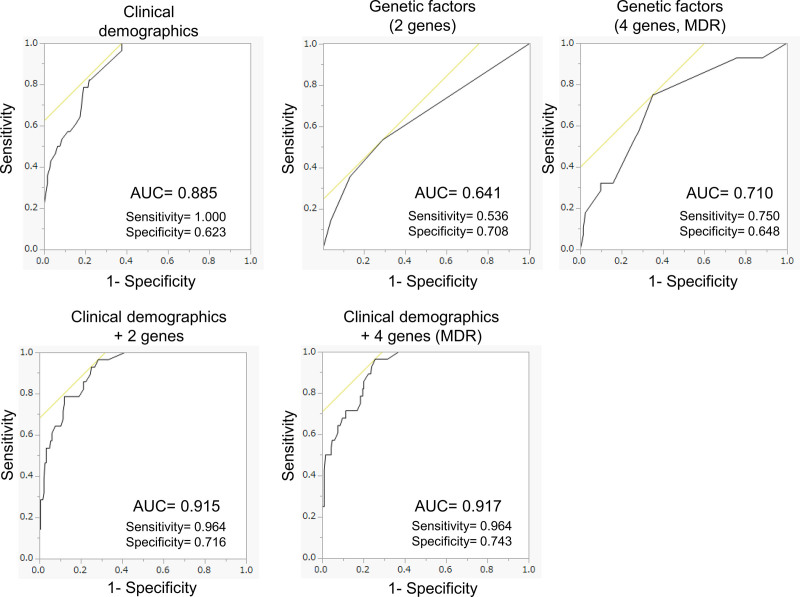
Among the 14 genes, we found rs1131454 in OAS1 and rs1143627 in IL1B genes as independent genetic factors associated with disease severity (adjusted odds ratio = 7.1 and 4.6 in the dominant model, respectively). Furthermore, we investigated the effect of multiple phase pathogenesis of coronavirus disease 2019 with unbiased multifactor dimensionality reduction analysis and identified a four-gene model with rs1131454 (OAS1), rs1143627 (IL1B), rs2074192 (ACE2), and rs11003125 (MBL). By combining these polygenetic factors with polyclinical factors, including age, sex, higher body mass index, and the presence of diabetes and hypertension, we proposed a composite risk model with a high area under the curve, sensitivity, and probability (0.917, 96.4%, and 74.3%, respectively) in the receiver operating characteristic curve analysis.
CONCLUSIONS AND RELEVANCE:
We successfully identified significant genetic factors in OAS1 and IL1B genes using a candidate gene approach study as valuable information for further mechanistic investigation and predictive model building.
The coronavirus disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has resulted in a global and local health crisis. The transmission capacity of SARS-CoV-2 exceeds expectations, and the outbreak puts our medical systems at a risk of collapse. Patients with COVID-19 show a broad spectrum of disease progression. The identification of risk factors for severe COVID-19 is desperately needed to distinguish patients who are at increased risk and to treat them more aggressively with limited social resources. Clinical studies on COVID-19 have revealed the clinical risk factors for severe diseases, such as age, sex, obesity, and comorbidities (1–6). The pathogenesis of severe COVID-19 and the associated respiratory failure has been extensively investigated, revealing the mechanism of viral entry, life cycle, and the host immune system that sometimes responds excessively, resulting in unfavorable outcomes, such as cytokine storms and acute respiratory distress syndrome (7–10). Our understanding of the pathogenesis of COVID-19 suggests that the clinical severity could be determined by the host response against SARS-CoV-2 in multiple pathogenetic phases.
Gene polymorphism could be one of the determinants of individual responses against viruses, including SARS-CoV-2. The candidate gene approach is a useful technique for identifying genetic risk factors for complex disorders, such as severe COVID-19 (11). Candidates having a plausible physiologic role in a major pathway implicated in the pathogenesis of COVID-19 should be tested for the effects of the genetic variants of potentially contributing genes.
Here, we used the candidate gene approach study to delineate the host genetic factors contributing to severe COVID-19 with respiratory failure. Furthermore, we investigated the interaction of multiple phase pathogenesis with unbiased and model-free statistical methods, multifactor dimensionality reduction (MDR) analysis, and estimated the genetic factors as predictors of severe COVID-19.
MATERIALS AND METHODS
Study Participants
We recruited a total of 230 patients with COVID-19, which was confirmed by SARS-CoV-2 viral RNA polymerase chain reaction (PCR) test using nasopharyngeal swabs or other relevant biological fluids. Patients were recruited from three hospitals: Funairi Citizens Hospital, Hiroshima Prefectural Hospital, and Hiroshima University Hospital in Hiroshima, Japan, from March 1, 2020, to March 31, 2021 (initial phase of the pandemic). Priority vaccination for the elderly began in Hiroshima Prefecture on April 12, 2021. Therefore, the cohort in this study consisted of unvaccinated patients. These three hospitals provided different services for patients with COVID-19 under administrative control. The judgment to admission was pretty depend on the pandemic situation. At the time of initial emerging phase, the judgment was strictly made even for asymptomatic patients to isolate them. Funairi Citizens Hospital treated mainly mild cases (participants, n = 162/526), and Hiroshima Prefectural Hospital treated mild to moderate II and some severe cases (n = 46/354). If the patients’ condition became severe, Hiroshima University Hospital treated them in the ICU (n = 22/26). This study was approved by the Ethical Committee for Human Genome Research of Hiroshima University (Hi-258). Written informed consent was obtained from all the participants.
Disease severity was classified according to the National Institutes of Health guideline, Version October 22 (Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases), based on the use of oxygen supplementation or mechanical ventilation (12). Severity was graded according to the maximum respiratory support received at any point during hospitalization (mild, no oxygen supplementation; moderate I, supplemental oxygen therapy only; moderate II, noninvasive ventilatory support [nasal high flow]; and severe, invasive ventilatory support including extracorporeal membrane oxygenation). Other data collection was performed by physicians from local medical records using an electronic data form. The data were gathered from the Hiroshima University Hospital for analyses. Comorbidities, such as diabetes mellitus (DM), hypertension (HT), chronic respiratory disease, chronic renal disease, cancer, and steroid use, were defined upon receiving the prescription. Symptoms, laboratory data, were collected from the date of the initial assessment after admission (Supplemental Table 1, http://links.lww.com/CCX/A839). Missing data were happened at random on the observed variables only among nonsevere patients (body mass index [BMI], n = 17; comorbidities, n = 2; and smoking history, n = 11, respectively).
Candidate Gene Polymorphism
DNA samples from the study populations were genotyped for 34 functional polymorphisms from 14 distinct candidate genes. These gene polymorphisms in genes encoding viral cell entry, regulation of viral replication, innate immune modulators, regulatory cytokines, and effector cytokines were selected based on the best evidence from studies published under the key words “sepsis,” “respiratory infection,” “pneumonia,” “inflammation,” and “SARS.” If there were more than four candidate polymorphisms for a gene, the selection was based on the number of publications in single nucleotide polymorphism (SNP) database of National Center for Biotechnology information (13–38). Given the possibility of genetic diversity between the Japanese and East Asian populations (39), we performed the analysis even through the selected SNPs had low minor allele frequencies in database. The descriptions of the polymorphisms and minor allele frequencies for each marker are shown in Supplemental Table 2 (http://links.lww.com/CCX/A840).
Genotyping
Blood samples of the study population were collected by EDTA containing tubes with blinded unique identification number. Peripheral blood mononuclear cells (PBMCs) were isolated from the blood draw. Genomic DNA was extracted from PBMCs or whole blood using a QIAcube (QIAGEN, Hilden, Germany). Then, most SNP genotyping was carried out using TaqMan SNP genotyping assays (Thermo Fisher Scientific, MA) according to the manufacturer’s protocol. In brief, two allele-specific TaqMan probes containing distinct fluorescent dyes and a PCR primer pair were used to detect specific SNP targets. Quantitative PCR, as a readout, was performed with Roter-GeneQ (QIAGEN). We describe the zygosity of A>G SNP as AA or GG, and AG in the case of homozygosity and heterozygosity, respectively.
Zygosity for the deletion (D)–insertion (I) polymorphism of the ACE gene was determined using an assay to distinguish D and I alleles based on PCR and visualization by electrophoresis (190bp and 490bp amplicon, respectively) (40). Samples classified as the deletion-homozygotic (DD) genotype were subjected to PCR again to eliminate DD mistyping by detecting a 319bp amplicon implied I allele (13).
Statistical Analysis
All statistical analyses were performed as complete-case analysis using the JMP Pro statistical software package 15.0.0 (SAS Institute, Cary, NC) and the Java software MDR v.3.0.2 (investigated by Jason Moore, available at www.sourceforge.net). The Pearson chi-square test was used to test for differences in distribution between nonsevere and severe patients. Logistic regression analysis was used to estimate the associations between genotypes and risk of severe disease by computing the odds ratios (ORs) and 95% CIs from multivariate logistic regression analyses (adjusting for age > 65 yr, sex, BMI > 25, presence of diabetes, and hypertension, n = 211). The impact of polymorphism was tested in additive, dominant, and recessive models.
We employed the multifactor dimensionality reduction (MDR) analysis, a nonparametric and model-free method developed by Ritchie et al (41), and detected and characterized high-dimensional gene-gene interactions in studies with relatively small sample sizes (n = 230). MDR analysis identified nonhypothetical genotype combinations (or possible interactions) associated with disease severity. In brief, the dataset was divided into a model building set and a model testing set to evaluate the accuracy rate. The model with maximum cross-validation (CV) consistency (CVC) and balanced testing accuracy (TA) was selected as the best model. In this study, the MDR analysis was conducted using the dichotomous groupings of the polymorphisms selected by the candidate gene approach, and we used a 10-fold CV to calculate the mean CVC and balanced TA. The best models with the maximum TA and CVC were identified. The MDR results were considered statistically significant at the level of 0.05. The predictive models are created by a logistic regression model based on the forward-backward selection according to the mentioned clinical and genetic candidate factors (n = 211). Then, the accuracy of the severity risk model was assessed using the area under the curve (AUC).
RESULTS
Clinical Characteristics of the Study Population
Twenty-eight of the 230 patients (12.2%) with COVID-19 infection were categorized as having severe infection, which required mechanical ventilation during hospitalization (severe group). Ninety-eight (70 nonsevere and 28 severe) and six patients were received corticosteroid therapy and anti-interleukin (IL)-6 antibody therapy for COVID-19 infection, respectively (Supplemental Table 1, http://links.lww.com/CCX/A839). There was no patient who was received anti-IL-1 antibody or anti-tumor necrosis factor alpha antibody therapy. Seven patients in the severe group (25.0%) died due to COVID-19 infection, but no mortality was observed in those with mild to moderate COVID-19 infection (nonsevere group). Consistent with previous reports, the severe group was older (age mean ± sd, 64.2 ± 13.3 vs 48.5 ± 16.7), more likely to be male (82.1% vs 55.0%), and had higher BMI (27.6 ± 4.8 vs 23.7 ± 3.9) and comorbidities (82.1% vs 49.0%) compared with the nonsevere group (Table 1). Diabetes and hypertension were more frequent in the severe group than in the nonsevere group (50.0% vs 11.4%, and 71.4% vs 18.3%, respectively). There was no difference in the periods in which patients were admitted to the hospital after the start of symptoms between the severe and nonsevere groups. In our cohort, history of smoking was not associated with the severity of infection; however, the current smoking status seems to be a beneficial factor associated with the severity, contrary to the expectation that smoking exacerbated COVID-19 infection. We observed that younger patients who were associated with a lower risk of severe disease were more frequently current smokers, resulting in a conflicting association. Based on these observations, we set five clinical covariates (age ≥ 65 yr, sex, BMI ≥ 25, diabetes, and hypertension) for covariate adjustment of the genetic analyses.
TABLE 1.
Characteristics of the Study Population
| Demographics/Comorbidities | Nonsevere (n = 202) | Severea (n = 28) | Nonsevere vs Severe pb | ||
|---|---|---|---|---|---|
| Milda (n = 163) | Moderate Ia (n = 36) | Moderate IIa (n = 3) | |||
| Severity at admission (mild/moderate I/II/ severe), n | 163/0/0/0 | 15/21/0/0 | 3/0/0/0 | 4/12/3/9 | |
| Number of death (mortality), n (%) | 0 | 0 | 0 | 7 (25.0) | |
| Age, mean ± sd | 53.1 ± 16.3 | 59.7 ± 12.7 | 67.7 ± 13.3 | 64.2 ± 13.3 | < 0.0001 |
| Age < 65/ ≥ 65c, n | 147/16 | 25/11 | 2/1 | 12/16 | < 0.0001 |
| Gender (male/female)c, n | 85/78 | 24/12 | 2/1 | 23/5 | 0.004 |
| BMI, mean ± sd | 23.4 ± 3.5 | 25.2 ± 5.3 | 23.5 ± 1.0 | 27.6 ± 4.9 | < 0.0001 |
| BMI < 25/ ≥ 25c,d, n | 104/42 | 22/14 | 2/1 | 10/18 | 0.0006 |
| Days from initial symptoms to admission, mean ± sd | 4.4 ± 4.2 | 5.9 ± 4.1 | 3.0 ± 1.8 | 4.5 ± 3.1 | 0.776 |
| Current smoking, n (%) | 43 (26.4) | 3 (8.3) | 0 | 0 | 0.002 |
| History of smokingd, n (%) | 84 (51.5) | 19 (52.8) | 1 (33.3) | 12 (42.9) | 0.536 |
| Diabetesc,d, n (%) | 16 (9.8) | 7 (19.4) | 0 | 14 (50.0) | < 0.0001 |
| Hypertensionc,d, n (%) | 23 (14.1) | 12 (33.3) | 2 (66.7) | 20 (71.4) | < 0.0001 |
| Chronic respiratory diseased, n (%) | 9 (5.5) | 0 | 0 | 1 (3.6) | 0.813 |
| Chronic renal diseased, n (%) | 0 | 1 (2.8) | 0 | 2 (7.1) | 0.026 |
| Cancerd, n (%) | 3 (1.8) | 0 | 0 | 0 | 0.373 |
| Steroid userd, n (%) | 0 | 1 | 0 | 1 (3.6) | 0.192 |
| Cardiovascular infarctiond, n (%) | 4 (2.5) | 0 | 0 | 4 (14) | 0.008 |
| Cardiac failured, n (%) | 1 (0.6) | 0 | 0 | 1 (3.6) | 0.192 |
| Brain infarctiond, n (%) | 1 (0.6) | 0 | 0 | 2 (7.1) | 0.026 |
| Organ transplantationd, n (%) | 1 (0.6) | 1 | 0 | 0 | 0.468 |
BMI = body mass index.
aDefinition of severity classified according to National Institutes of Health guideline version October 22: mild, no oxygen supplementation; moderate I, supplemental oxygen therapy only; moderate II, noninvasive ventilatory support; and severe, invasive ventilatory support.
bUnivariate statistic (Wilcoxon signed rank test/χ2 test).
cSet up as adjusting covariates for genetic analysis.
dMissing data: BMI (n = 17), comorbidities (n = 2), and history of smoking (n = 11).
Candidate Gene Approach Identified Independent Risk Genotypes for Severe COVID-19
The SNP descriptions are listed in Supplemental Table 2 (http://links.lww.com/CCX/A840). Two of the final set of 34 SNPs in the 14 genes investigated were found to be significantly associated with the severe group. The SNPs rs1131454 (OAS1 gene, GG genotype) and rs1143627 (IL1B gene, GG genotype) had an increased risk of severe disease at approximately seven-fold and four-fold (adjusted OR [aOR], 7.1; 95% CI, 1.8–27.6 and aOR, 4.6; 95% CI, 1.3–17.0), respectively, in the dominant model (Table 2). The additive effect, which included a baseline risk (absence of the risk allele), a medium risk (heterozygosity for the risk allele), and a high risk (homozygosity for the risk allele), was not observed in these two SNPs for severity of COVID-19 infection. Additionally, the two SNP statuses were not associated with the five clinical covariates for adjustments.
TABLE 2.
Genetic Risk Factors for Severe Coronavirus Disease 2019
| Gene | Additive Model Adjusted ORa | p | Recessive Model Adjusted OR | p | Dominant Model Adjusted OR | p |
|---|---|---|---|---|---|---|
| OAS-1 (rs1131454) | ||||||
| AA (n = 82) | Reference | 7.1 (1.8–27.6) | 0.0048 | 2.1 (0.63–6.8) | 0.225 | |
| AG (n = 96) | 1.1 (0.3–4/3) | 0.913 | ||||
| GG (n = 33) | 7.4 (1.6–34.6) | 0.0112 | ||||
| IL1B (rs1143627) | ||||||
| AA (n = 61) | Reference | 4.6 (1.3–17.0) | 0.0207 | 2.23 (0.57–8.64) | 0.244 | |
| AG (n = 103) | 1.5 (0.3–6.4) | 0.608 | ||||
| GG (n = 47) | 6.1 (1.1–33.3) | 0.0372 | ||||
OR = odds ratio.
We describe the zygosity of A>G SNP as AA or GG, and AG in the case of homozygosity and heterozygosity, respectively.
aAdjusted with age > 65, gender, body mass index > 25, diabetes, and hypertension.
Collectively, we identified independent genetic risk factors, homozygotes with the minor allele of rs1131454 in the OAS1 gene and rs1143627 in IL1B, as predictors of severe COVID-19 infection.
Multiple Phase Model in MDR Analysis
We further investigated the gene-gene interactions and/or multiple phase effects of gene polymorphisms with MDR analyses. We obtained no consistent model in the two- or three-way gene interaction analyses. However, the four-way gene interaction analysis revealed a significant association between rs1131454 (OAS1), rs1143627 (IL1B), rs2074192 (ACE2), and rs11003125 (MBL) (CVC, 0.9; TA, 0.74; p < 0.0001; Table 3).
TABLE 3.
Interaction Gene Models for Severe Coronavirus Disease 2019 by Multifactor Dimensional Reduction Assay
| No. of Gene | Best Interaction Model | Testing Accuracy | Cross-Validation Consistency | p | |||
|---|---|---|---|---|---|---|---|
| 1 | OAS1 rs1131454 | 0.61 | 9/10 | 0.0018 | |||
| 2 | OAS1 rs1131454 | Chemokine ligand 5 rs2280788 | 0.64 | 4/10 | 0.0102 | ||
| 3 | OAS1 rs1131454 | IL1B rs1143627 | ACEI Alu repeat zygosity for the insertion-deletion polymorphism | 0.68 | 3/10 | 0.0007 | |
| 4 | OAS1 rs1131454 | IL1B rs1143627 | ACE2 rs2074192 | MBL rs11003125 | 0.73 | 8/10 | < 0.0001 |
Predictive Model for Severe COVID-19 Infection
We evaluated whether the use of polygenetic risk factors improved the prediction of severe disease once the individual was infected with COVID-19. We performed an receiver operating characteristic (ROC) curve analysis with the risk score calculated by a multivariable model using forward-backward stepwise binary logistic regression analysis. ROC curve analyses revealed that a higher AUC was found for the combination of five clinical factors and two gene factors compared among those with only two genetic factors that were identified as independent risk, four genetic factors by MDR analysis, and clinical factors (AUC = 0.915 vs 0.640, 0.709, and 0.885, respectively; Fig. 1). The genetic factors identified in the MDR analysis also slightly improved the AUC in the ROC analysis combined with clinical factors (AUC = 0.917). The final model (clinical and MDR genes) equation was: Predictive score (P) = 1/(1 + e–x)
Figure 1.
Receiver operating characteristic (ROC) analysis of predictive models for severe coronavirus disease 2019 infection. ROC curve analysis were performed with indicated clinical or genetic covariates to calculate the predictive value, area under the curve (AUC), sensitivity, and specificity. Clinical demographics and two genes indicated age greater than 65, gender, body mass index greater than 25, the presence of diabetes and hypertension, and rs1131454 (OAS1) and rs1143627 (IL1B), respectively. Four genes additionally indicated rs2074192 (ACE2) and rs11003125 (MBL) identified in multifactor dimensionality reduction (MDR) analysis.
x = –1.12 + 0.767 × (–1 if yr ≤ 64 1 if yr ≥ 65) + 0.577 × (–1 if female 1 if male) + 0.549 × (–1 if BMI < 25 1 if BMI ≥ 25) + 0.757 × (–1 if DM negative 1 if DM positive) + 0.998 × (–1 if HT negative 1 if HT positive) + 0.882 × (–1 if rs1131454 others 1 if rs1131454 GG) + 0.480 × (–1 if rs1143627 others 1 if rs1143627 GG) + 0.574 × (–1 if rs11003125 CC 1 if rs11003125 others).
The composite risk score including polygenetic and polyclinical factors showed a high sensitivity and specificity (96.4% and 74.3%, respectively) to effectively predict the population that may be associated with severe disease after COVID-19 infection.
DISCUSSION
The pathogenesis of COVID-19 infection is complex and involves a series of reactions in the host’s body. Gene polymorphisms have been reported to be associated with these reactions against viral infections, including previous coronavirus infections such as SARS and Middle East respiratory syndrome, through multiple mechanisms (19, 22–24). Several genome-wide association studies (GWASs) have been conducted in Europe to identify unbiased targets for risk diagnosis and the therapeutic design for COVID-19 infection. The first report on GWAS of severe COVID-19 detected two genetic susceptibility loci, at Chr3p21.31 and Chr9q34.2, using a meta-analysis of two case/control panels of a thousand people from Italy and Spain (42). The gene cluster around the Chr3p21.31 locus, reported as a Neanderthal genetic variant, has been reproducibly associated with severe COVID-19 by at least three GWASs, indicating a common genetic mechanism underlying severe COVID-19 (42–44). Although genetic risk analysis is helpful to identify the natural risk of the population and even of individuals as well, it is sometimes difficult to conduct a study with a sufficient number of participants to identify unbiased targets, such as GWAS. The gene candidate strategy focuses on selected target genes and can reduce the required number of participants based on the information provided in previous reports. Using the candidate gene approach, we identified independent genetic factors, rs1131454 (OAS1 gene) and rs1143627 (IL1B gene), which are associated with severe disease in the Japanese population. Both pathways identified in our cohort, OAS1 and IL-1b, have convincing points of action, such as regulating viral replication and promoting an excessive immune response, respectively. The OAS1 pathway, which activates RNase L to cleave the RNA virus genome, has also been identified as a candidate genetic mechanism in a European cohort by a GWAS using different SNPs (rs4767027 as a protein quantitative trait loci) (45). We investigated SNPs (rs2660 and rs10774671), which have high linkage disequilibrium with rs4767027, and both SNPs showed no significant impact on severe disease in our cohort. One of the previous reports revealed that the Neanderthal risk haplotype, which includes the OAS1 rs47767027, is almost absent in East Asian populations, such as in the Japanese, owing to its geographical distribution (44). However, the finding that a pathway involves disease severity with the same gene through different polymorphisms in different races could be interpreted to enhance the biological significance of the OAS1 pathway in COVID-19 infection. It is likely that a genetic predisposition in the OAS1 pathway may contribute to the dysregulation of the innate antiviral immune system in COVID-19 patients. Similarly, IL-1 signaling has been reported as the most important pathway for the severity of COVID-19 patients in another GWAS (46). Together with these findings, further investigation of the mechanisms underlying the pathogenesis of COVID-19 through the pathways, OAS1 and IL-1b, would be potential opportunities to develop new prevention and treatment strategies.
Previous investigators have developed risk scoring systems to identify severe or fatal disease outcomes based on clinical findings after infection, such as laboratory tests or CT findings with demographic characteristics, to guide clinical decisions (47–50). A representative study in the United Kingdom has worked on nearly 20 million primary care records to identify the factors associated with COVID-19–related death by creating a new health analytics platform and building a predictive model with a high C-statistic (0.93) (1). Owing to these valuable efforts (1–6), several demographics, such as age, sex, obesity, and comorbidities, are well-established risk factors for severe infection. Our independent genetic predictors for severe COVID-19 infection improved the predictive model with a combination of demographic characteristics (Fig. 1). The prediction of the aggravation in COVID-19 patients by clinical demographics was superior in sensitivity but not in specificity. On the other hand, that by genetic factors was superior in specificity but not in sensitivity. The predictive model by combining both factors and complemented each other resulted in a high in AUC. A model created through MDR analysis that originally investigated gene-gene interaction by unbiased computational model building can be interpreted as a model with multiple phase effects in different pathogenesis stages in COVID-19 infection. The model using four genes listed by MDR analysis provided a slight but further improvement for the prediction of severe COVID-19 infection before the individuals were infected. Under the current COVID-19 pandemic, a better predictive model can provide valuable information for selecting potentially risky individuals to set up focused prophylaxis such as prior vaccination or develop strategies for the management of hospitalization or priority treatment in the limited social resources. However, the clinical significance of the slight improvement in AUC by adding genetic factors from two to four would be a subject for future research.
The limitation of this study is the sample size, which could provide only limited power. We believe this illustrates that using the proper methodology, such as the candidate gene approach, the genetic effects can be revealed even with a modest sample size. However, we cannot exclude the possibility that our findings may be due to chance and should be interpreted with caution. Further studies with large participants are required to validate our findings.
CONCLUSIONS
In conclusion, a candidate gene approach to investigate gene polymorphism for severe COVID-19 infection successfully identified independent genetic factors, OAS1 and IL-1B. This is valuable information for further mechanistic investigations and predictive model building.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
Supported, in part, by grant from the Government Academia Collaboration of Hiroshima Prefecture. Funding was also provided by Japan Agency for Medical Research and Development under Grant Number JP20he0722005 and JP20fk0108453.
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020; 584:430–436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect. 2020; 81:e16–e25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Richardson S, Hirsch JS, Narasimhan M, et al. ; the Northwell COVID-19 Research Consortium. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020; 323:2052–2059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ioannou GN, Locke E, Green P, et al. Risk factors for hospitalization, mechanical ventilation, or death among 10 131 US Veterans with SARS-CoV-2 infection. JAMA Netw Open. 2020; 3:e2022310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu Y, Sun J, Dai Z, et al. Prevalence and severity of corona virus disease 2019 (COVID-19): A systematic review and meta-analysis. J Clin Virol. 2020; 127:104371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fried MW, Crawford JM, Mospan AR, et al. Patient characteristics and outcomes of 11 721 patients with coronavirus disease 2019 (COVID-19) hospitalized across the United States. Clin Infect Dis. 2021; 72:e558–e565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giamarellos-Bourboulis EJ, Netea MG, Rovina N, et al. Complex immune dysregulation in COVID-19 patients with severe respiratory failure. Cell Host Microbe. 2020; 27:992–1000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou Z, Ren L, Zhang L, et al. Heightened innate immune responses in the respiratory tract of COVID-19 patients. Cell Host Microbe. 2020; 27:883–890. e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fauci AS, Lane HC, Redfield RR. Covid-19 - navigating the uncharted. N Engl J Med. 2020; 382:1268–1269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cyranoski D. Profile of a killer: The complex biology powering the coronavirus pandemic. Nature. 2020; 581:22–26 [DOI] [PubMed] [Google Scholar]
- 11.Dryja TP. Human genetics. Deficiencies in sight with the candidate gene approach. Nature. 1990; 347:614. [DOI] [PubMed] [Google Scholar]
- 12.Gulick RM, Lane HC, Masur H, et al. COVID-19 Treatment Guidelines. 2020. Available at: www.covid19treatmentguidelines.nih.gov. Accessed October 25, 2020
- 13.Lindpaintner K, Pfeffer MA, Kreutz R, et al. A prospective evaluation of an angiotensin-converting-enzyme gene polymorphism and the risk of ischemic heart disease. N Engl J Med. 1995; 332:706–711 [DOI] [PubMed] [Google Scholar]
- 14.Bosso M, Thanaraj TA, Abu-Farha M, et al. The two faces of ACE2: The role of ACE2 receptor and its polymorphisms in hypertension and COVID-19. Mol Ther Methods Clin Dev. 2020; 18:321–327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asselta R, Paraboschi EM, Mantovani A, et al. ACE2 and TMPRSS2 variants and expression as candidates to sex and country differences in COVID-19 severity in Italy. Aging (Albany NY). 2020; 12:10087–10098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Madsen HO, Garred P, Kurtzhals JA, et al. A new frequent allele is the missing link in the structural polymorphism of the human mannan-binding protein. Immunogenetics. 1994; 40:37–44 [DOI] [PubMed] [Google Scholar]
- 17.Koch A, Melbye M, Sørensen P, et al. Acute respiratory tract infections and mannose-binding lectin insufficiency during early childhood. JAMA. 2001; 285:1316–1321 [DOI] [PubMed] [Google Scholar]
- 18.Hamano E, Hijikata M, Itoyama S, et al. Polymorphisms of interferon-inducible genes OAS-1 and MxA associated with SARS in the Vietnamese population. Biochem Biophys Res Commun. 2005; 329:1234–1239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonnevie-Nielsen V, Field LL, Lu S, et al. Variation in antiviral 2’,5’-oligoadenylate synthetase (2’5’AS) enzyme activity is controlled by a single-nucleotide polymorphism at a splice-acceptor site in the OAS1 gene. Am J Hum Genet. 2005; 76:623–633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu X, Xing H, Gao W, et al. A functional variant in the OAS1 gene is associated with Sjögren’s syndrome complicated with HBV infection. Sci Rep. 2017; 7:17571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ching JC, Chan KY, Lee EH, et al. Significance of the myxovirus resistance A (MxA) gene -123C>a single-nucleotide polymorphism in suppressed interferon beta induction of severe acute respiratory syndrome coronavirus infection. J Infect Dis. 2010; 201:1899–1908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhu X, Wang Y, Zhang H, et al. Genetic variation of the human α-2-Heremans-Schmid glycoprotein (AHSG) gene associated with the risk of SARS-CoV infection. PLoS One. 2011; 6:e23730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chan KY, Xu MS, Ching JC, et al. CD209 (DC-SIGN) -336A>G promoter polymorphism and severe acute respiratory syndrome in Hong Kong Chinese. Hum Immunol. 2010; 71:702–707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ng MW, Zhou G, Chong WP, et al. The association of RANTES polymorphism with severe acute respiratory syndrome in Hong Kong and Beijing Chinese. BMC Infect Dis. 2007; 7:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qiu P, Wang L, Ni J, et al. Associations between HMGB1 gene polymorphisms and susceptibility and clinical outcomes in Chinese Han sepsis patients. Gene. 2019; 687:23–29 [DOI] [PubMed] [Google Scholar]
- 26.Lee K, Chang Y, Song K, et al. Associations between single nucleotide polymorphisms of high mobility group box 1 protein and clinical outcomes in Korean sepsis patients. Yonsei Med J. 2016; 57:111–117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Song W, Tan H, Wang S, et al. Association of high mobility group box protein B1 gene polymorphisms with pneumonia susceptibility and severity. Genet Test Mol Biomarkers. 2019; 23:3–11 [DOI] [PubMed] [Google Scholar]
- 28.Gallagher PM, Lowe G, Fitzgerald T, et al. Association of IL-10 polymorphism with severity of illness in community acquired pneumonia. Thorax. 2003; 58:154–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chong WP, Ip WK, Tso GH, et al. The interferon gamma gene polymorphism +874 A/T is associated with severe acute respiratory syndrome. BMC Infect Dis. 2006; 6:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang H, Wang M, Shi T, et al. TNF rs1799964 as a predictive factor of acute toxicities in Chinese rectal cancer patients treated with chemoradiotherapy. Medicine (Baltimore). 2015; 94:e1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang J, Chi H, Xiao H, et al. Interleukin 6 (IL-6) and tumor necrosis factor α (TNF-α) single nucleotide polymorphisms (SNPs), inflammation and metabolism in gestational diabetes mellitus in Inner Mongolia. Med Sci Monit. 2017; 23:4149–4157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saleh A, Sultan A, Elashry MA, et al. Association of TNF-alpha G-308 a promoter polymorphism with the course and outcome of COVID-19 patients. Immunol Invest. 2020. Nov 23. [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mahto H, Tripathy R, Meher BR, et al. TNF-α promoter polymorphisms (G-238A and G-308A) are associated with susceptibility to systemic lupus erythematosus (SLE) and P. falciparum malaria: A study in malaria endemic area. Sci Rep. 2019; 9:11752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hu P, Chen Y, Pang J, et al. Association between IL-6 polymorphisms and sepsis. Innate Immun. 2019; 25:465–472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ambrocio-Ortiz E, Pérez-Rubio G, Abarca-Rojano E, et al. Influence of proinflammatory cytokine gene polymorphisms on the risk of COPD and the levels of plasma protein. Cytokine. 2018; 111:364–370 [DOI] [PubMed] [Google Scholar]
- 36.Zhang N, Xu Y, Zhang B, et al. Analysis of interleukin-8 gene variants reveals their relative importance as genetic susceptibility factors for chronic periodontitis in the Han population. PLoS One. 2014; 9:e104436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Montoya-Ruiz C, Jaimes FA, Rugeles MT, et al. Variants in LTA, TNF, IL1B and IL10 genes associated with the clinical course of sepsis. Immunol Res. 2016; 64:1168–1178 [DOI] [PubMed] [Google Scholar]
- 38.Fu LY, Qiu X, Deng QL, et al. The IL-1B gene polymorphisms rs16944 and rs1143627 contribute to an increased risk of coronary artery lesions in Southern Chinese children with Kawasaki disease. J Immunol Res. 2019; 2019:4730507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang Y, Lu D, Chung YJ, et al. Genetic structure, divergence and admixture of Han Chinese, Japanese and Korean populations. Hereditas. 2018; 155:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rigat B, Hubert C, Corvol P, et al. PCR detection of the insertion/deletion polymorphism of the human angiotensin converting enzyme gene (DCP1) (dipeptidyl carboxypeptidase 1). Nucleic Acids Res. 1992; 20:1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ritchie MD, Hahn LW, Moore JH. Power of multifactor dimensionality reduction for detecting gene-gene interactions in the presence of genotyping error, missing data, phenocopy, and genetic heterogeneity. Genet Epidemiol. 2003; 24:150–157 [DOI] [PubMed] [Google Scholar]
- 42.Ellinghaus D, Degenhardt F, Bujanda L, et al. ; Severe Covid-19 GWAS Group. Genomewide association study of severe Covid-19 with respiratory failure. N Engl J Med. 2020; 383:1522–1534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pairo-Castineira E, Clohisey S, Klaric L, et al. ; GenOMICC Investigators; ISARIC4C Investigators; COVID-19 Human Genetics Initiative; 23andMe Investigators; BRACOVID Investigators; Gen-COVID Investigators. Genetic mechanisms of critical illness in COVID-19. Nature. 2021; 591:92–98 [DOI] [PubMed] [Google Scholar]
- 44.Zeberg H, Pääbo S. The major genetic risk factor for severe COVID-19 is inherited from Neanderthals. Nature. 2020; 587:610–612 [DOI] [PubMed] [Google Scholar]
- 45.Zhou S, Butler-Laporte G, Nakanishi T, et al. A Neanderthal OAS1 isoform protects individuals of European ancestry against COVID-19 susceptibility and severity. Nat Med. 2021; 27:659–667 [DOI] [PubMed] [Google Scholar]
- 46.Wang F, Huang S, Gao R, et al. Initial whole-genome sequencing and analysis of the host genetic contribution to COVID-19 severity and susceptibility. Cell Discov. 2020; 6:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liang W, Liang H, Ou L, et al. ; China Medical Treatment Expert Group for COVID-19. Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19. JAMA Intern Med. 2020; 180:1081–1089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Galloway JB, Norton S, Barker RD, et al. A clinical risk score to identify patients with COVID-19 at high risk of critical care admission or death: An observational cohort study. J Infect. 2020; 81:282–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Feng Z, Yu Q, Yao S, et al. Early prediction of disease progression in COVID-19 pneumonia patients with chest CT and clinical characteristics. Nat Commun. 2020; 11:4968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang C, Qin L, Li K, et al. A novel scoring system for prediction of disease severity in COVID-19. Front Cell Infect Microbiol. 2020; 10:318. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.