Abstract
The geographical overlaps of malaria parasites and Salmonella spp. can lead to co-infection of these two pathogens, especially in the tropics where malaria is endemic. Moreover, few literatures suggested that malaria infection was associated with Salmonella bacteremia. Therefore, this study quantified pooled prevalence of typhoidal/non-typhoidal Salmonella (NTS) and probability of typhoidal/NTS and malaria co-infection among febrile patients. The systematic review protocol was registered at PROSPERO (CRD42021252322). Studies on co-infection of typhoidal/NTS and malaria were searched in PubMed, Scopus, and Web of Science. The risk of bias of the included studies was assessed using the checklist for analytical cross-sectional studies developed by the Joanna Briggs Institute. Meta-analyses on the following criteria were performed: (1) pooled prevalence of typhoidal/NTS and malaria co-infection among febrile patients, (2) pooled prevalence of typhoidal/NTS among malaria patients, (3) pooled prevalence of malaria infections among patients with Salmonella spp. infection, and (4) probability of typhoidal/NTS and malaria co-infection among febrile patients. Additionally, the case fatality rate and mean difference of malarial parasitemia between typhoidal/NTS and malaria co-infection and Plasmodium monoinfection were also determined. The subgroup analyses of typhoidal/NTS, regions (Africa and Asia), countries, time (publication year), characteristics of participants, and diagnostic tests for identifying Salmonella spp. were also conducted. A sensitivity test was performed to determine the robustness of the study outcomes. Publication bias among the included studies was evaluated using the funnel plot and Egger’s test. All analyses were performed using Stata version 15 (StataCorp LLC, Texas, USA) with a p-value < 0.05 indicating statistical significance. Eighty-one studies that met the eligibility criteria were included in the analyses. Of the 73,775 study participants, 4523 had typhoidal/NTS and malaria co-infections. The pooled prevalence rates of typhoidal/NTS and malaria co-infection among febrile patients were 14% (95% confidence interval [CI], 9–19%; I2, 99.4%; 2971/17,720 cases) and 1% (95% CI 1–1%; I2, 89.9%; 252/29,081 cases) using the Widal test and culture methods for identifying Salmonella spp., respectively. The pooled prevalence rates of typhoidal/NTS infection among patients with malaria were 31% (95% CI 23–39%; I2, 99.5%; 3202/19,208 cases) and 3% (95% CI 2–3%; I2, 86.8%; 407/40,426 cases) using the Widal test and culture methods for identifying Salmonella spp., respectively. The pooled prevalence rates of malaria infection among patients with typhoidal/NTS were 17% (95% CI 6–29%; I2, 33.3%; 13/75 cases) and 43% (95% CI 32–53%; I2, 89.1%; 287/736 cases), respectively. Malaria infection was associated with typhoidal/NTS in children aged < 15 years (p < 0.0001; odds ratio, 0.36; 95% CI 0.23–0.58; I2, 73.9%; 3188/43,212 cases). The case fatality rate in patients with malaria and NTS co-infections was 16% (95% CI 9–24%; I2, 89.1%; 18/103 cases). From the view of the present study, the inappropriate use of the Widal test for Salmonella spp. diagnosis can overestimate the prevalence of typhoidal/NTS and malaria co-infections. Malaria infection associated with typhoidal/NTS in children and the high case fatality rates among few patients with co-infections were highlighted. Future prospective longitudinal studies using the appropriate and confirmatory dsiagnosis for Salmonella spp. infections are highly recommended to ensure the real prevalence of co-infection and highlight the outcome of co-infection for providing adequate treatment in febrile patients who live in areas where malaria is endemic, such as tropical Africa and India.
Subject terms: Epidemiology, Infectious diseases
Introduction
Malaria is a major public health problem in tropical and subtropical countries. The World Health Organization (WHO) reported 229 million cases of malaria and 409,000 deaths in 20191. Most of these cases (51% globally) were found in Nigeria (27%), the Democratic Republic of the Congo (12%), Uganda (5%), Mozambique (4%), and Niger (3%), whereas 51% of malaria deaths occurred in Nigeria (23%), the Democratic Republic of the Congo (11%), the United Republic of Tanzania (5%), Mozambique (4%), Niger (4%), and Burkina Faso (4%)1. Although the incidence of malaria declined from 2000 to 2019, its diagnosis among febrile patients in malaria-endemic settings remains challenging; malaria and typhoid and non-typhoid fever are co-endemic and have similar clinical signs and symptoms.
Salmonella species are Gram-negative bacilli members of Enterobacteriaceae and associated with human infection2,3. Salmonella is comprised of two major species, namely, Salmonella enterica and Salmonella bongori. S. enterica are classified into six serotypes, which are differentiated based on their antigenicity3. Several Salmonella enterica serotypes cause typhoid fever. S. typhi and S. paratyphi, collectively referred to as typhoidal Salmonella, are the most common species that cause enteric fever (typhoid fever and paratyphoid fever). While both fevers share clinical symptoms, paratyphoid fever tends to be more benign4,5. Paratyphoid fever is most commonly acquired by ingesting contaminated food or water5. Humans are key reservoir hosts for typhoidal Salmonella and contribute to disease transmission and dissemination5. Typhoid fever is characterized by gastroenteritis and presents with nonspecific clinical symptoms, such as high fever, fatigue, headache, malaise, abdominal pain, nausea, vomiting, constipation, and diarrhea5,6. These symptoms are indistinguishable from other causes of fever, such as malaria5. The complications of typhoid fever include septicemia, meningitidis, and immunological symptoms7. Typhoid fever may be mild or severe, and complications may contribute to typhoid-related deaths7,8. Non-typhoid fever is a febrile illness caused by non-typhoidal Salmonella (NTS), including S. enteritidis and S. typhimurium9. NTS infections most often cause mild gastroenteritis, which is usually self-limiting7. Recently, NTS infections have been associated with septicemia and high mortality rates in immunocompromised patients in sub-Saharan Africa10.
The Salmonella infection rate is high in low- and middle-income countries with > 100 per 100,000 infected people annually11,12. Typhoid fever is an important cause of morbidity and mortality worldwide, with an estimated 16–33 million cases and 500,000 to 600,000 deaths annually13. Typhoid is endemic in developing countries, especially Africa, whereas developed countries have a much lower incidence. The majority of patients in developed countries are travelers returning from endemic areas14. In developing countries, especially in Southeast Asia and Africa, NTS is endemic and is a global burden, contrary to typhoidal Salmonella12,14. Poor water quality, poor handwashing habits, and consumption of untreated drinking water or unsafe food are the main causes of typhoid fever15. Therefore, people with low socioeconomic status and poor or improper hygiene have high risk of fecal–oral enteric infections, including typhoidal and NTS. The most recent meta-analysis revealed that household behaviors, including poor hygiene and consumption of unsafe food and untreated water, increase the risk of typhoid transmission16. Among children in Africa, NTS is a leading cause of bacteremia, whereas typhoid fever has a relatively low burden17–19. Another study demonstrated that typhoid fever is more common in older children with a period of fever, whereas non-typhoidal bacteremia frequently develops in younger children of poorly educated women or women with low socioeconomic status20.
For the diagnosis of typhoidal Salmonella infection, especially from blood, bacteriological culture is the gold standard21. The sensitivity of the culture method depends on the blood volume, antibiotic treatment, affected individual, disease duration, and presence of bacteremia22. Blood cultures have a sensitivity of 40–80%9,23. Moreover, they are most sensitive in the first week of infection as circulating bacterial concentrations peak at that time23. Stool and rectal swab cultures have lower sensitivity than blood cultures24. However, sensitivity can be enhanced by culturing from three specimens or performing multiple cultures from a single stool specimen24. Culture methods are less frequently employed in developing countries because of the high cost and requirements for good laboratory facilities and highly trained professionals7,25. Serological diagnoses of infections are conducted using the Widal test. This test measures the antibody titers specific for Salmonella O (somatic) and H (flagella) antigens7. The Widal test is widely used in numerous countries where trained technicians and laboratory facilities are limited7,25. Other useful methods for the diagnosis of Salmonella infection include enzyme-linked immunosorbent assay (ELISA), which detect IgM and IgG antibodies against Salmonella surface molecules, and molecular methods, such as nested multiplex polymerase chain reaction (PCR) and real-time PCR, which target Salmonella virulence genes. The real-time PCR test is highly specific and sensitive and has faster turnaround times than culture methods7,26.
The geographical overlaps of malarial parasites and typhoidal/NTS can lead to co-infection of these two pathogens, especially in the tropics where malaria is endemic. The overlap in the clinical symptoms of malaria and non-malaria febrile illness or co-infection of these two pathogens may lead to the misdiagnosis of one disease. Previous studies conducted in Africa demonstrated that bacteremia caused by NTS was associated with malaria parasitemia17,27,28, recent malaria29, anemia29, severe malarial anemia30, jaundice, and hypoglycemia20. Previous studies also demonstrated that NTS infection is associated with more severe anemia and malaria compared with typhoidal Salmonella or other bacteremia infections17,29,31. Another study demonstrated that NTS infections were associated with previous antimalarial treatment and malarial complications (severe anemia, jaundice, and hypoglycemia). Furthermore, a systematic review demonstrated a higher case fatality rate in children who were co-infected with NTS compared with those infected with malaria alone; however, the study had limitations on high heterogeneity between studies, inclusion of recent malaria infection, use of antigen-based rapid diagnostic tests (RDTs), study design, quality of microbiological data, and publication bias, making the meta-analysis potentially misleading32. To the best of our knowledge, meta-analyses determining the association between malaria and typhoid/non-typhoid fever have not been well conducted, and information is not updated. Therefore, the present study aimed to quantify the pooled prevalence, probability, and outcome of typhoidal/NTS and malaria co-infection among febrile patients who were suspected of having these two diseases.
Methods
Protocol and registration
The protocol of systematic review was registered at PROSPERO (CRD42021252322) and conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement33.
Search strategy
Potentially relevant articles in PubMed, Web of Science, and Scopus were searched using the combined search terms presented in Supplementary Table S1. The relevant search terms were retrieved from Medical Subject Headings to ensure the inclusion of all relevant studies. The searches were conducted from inception to April 27, 2021. Searches were limited to the English language, but the year of publication was not limited. Additional searches were performed by reviewing the reference lists of the included studies and Google Scholar to ensure that all potentially relevant studies were included in the meta-analysis.
Eligibility criteria
Observational studies in the English language that reported concurrent malaria and typhoidal/NTS infection were included in the study. Studies reporting data that could not be extracted, case–control studies, experimental studies, animal studies, case reports, and case series were excluded.
Study selection and data extraction
Potentially relevant articles were selected by two authors (MK, WM) using the eligibility criteria. First, the duplicates from the three databases were removed. Second, the remaining studies were screened for titles and abstracts, and any non-related studies were excluded. Third, the full texts of the remaining studies were examined, and any non-related studies were excluded with reasons. Then, the remaining studies were included in the systematic review and meta-analysis. Any disagreement on the study selection between the two authors was resolved by reaching a consensus after the discussion. Data extraction was performed by two authors (MK, WM) using the pilot standardized datasheets. The following information was obtained from each study: first author names, publication year, study sites (country and region), year the study was conducted, study design, characteristics of participants including age and sex, number of co-infections, number of malaria cases, number of typhoid/non-typhoid cases, number of case fatality in co-infection and Plasmodium monoinfection, diagnostic test for malaria, and diagnostic test for typhoid (best diagnostic test). Any disagreement on data extraction between the two authors was resolved by a third author (PW) for the final decision.
Risk of bias
The risk of bias of the included studies was evaluated using the checklist for analytical cross-sectional studies developed by the Joanna Briggs Institute34. The checklist is comprised of eight categories (yes/no/unclear/not applicable answers) based on the design, conduct, and analysis. Studies with yes answers in all eight categories were considered to have low risk of bias (high quality), whereas those that complied with four to six categories were considered to have a moderate risk of bias (moderate quality). Any study that complied with less than four categories was considered to have a high risk of bias (low quality) and thus excluded from the present study. The risk of bias was evaluated by two authors (MK, WM). If the two authors disagreed on the risk of bias assessment, a third author (PW) was responsible for the final decision.
Outcomes
The outcomes of this study were as follows: (1) pooled prevalence of typhoidal/NTS and malaria co-infection among febrile patients, (2) pooled prevalence of typhoidal/NTS infection among patients with malaria, (3) pooled prevalence of malaria infection among patients with Salmonella spp. infection, (4) comparison of typhoidal/NTS infection among patients with severe and non-severe malaria, (5) association between malaria and typhoidal/NTS infections, (6) case fatality rate among patients with typhoidal/NTS and malaria co-infection, and (7) difference in mean parasitemia level between patients with typhoidal/NTS and malaria co-infection and those with Plasmodium spp. monoinfection.
Data synthesis
The pooled prevalence rate of typhoidal/NTS and malaria co-infection among febrile patients, typhoidal/NTS infection rate among patients with malaria, malaria infection rate among patients with Salmonella spp. infection, case fatality rate among patients with typhoidal/NTS and malaria co-infection, and comparison of typhoidal/NTS infection rates among patients with severe and non-severe malaria were estimated using random-effect models, assuming heterogeneity of the included studies. The results of the individual studies are presented in the forest plots as the point estimates (prevalence in percentage) and 95% confidence interval (CI). The association between Plasmodium spp. and Salmonella spp. infections was determined using the random-effects model and expressed as odds ratio with 95% CI. The difference in mean parasitemia level between patients with typhoidal/NTS and malaria co-infection and Plasmodium spp. monoinfection was estimated using the random-effects model and expressed as weighted mean difference (WMD) with 95% CI. The heterogeneity among the included studies was assessed using Cochran’s Q and I2 statistics. Cochran’s Q < 0.05 or I2 > 50% indicated substantial heterogeneity among the included studies. If no substantial heterogeneity existed, the fixed-effects model was employed to estimate the effect size (pooled prevalence or pooled odds ratio). The subgroup analysis of typhoidal/NTS, regions (Africa and Asia), countries, time (publication year), characteristics of participants, and diagnostic tests for identifying Salmonella spp. were conducted to explore the source(s) of heterogeneity among the overall effect estimate. Sensitivity analyses of the probability of Plasmodium spp. and Salmonella spp. co-infection were performed using the random- and fixed-effects models after excluding outliers.
Publication bias
Publication bias among the included studies was evaluated using a funnel plot between the effect size (ES) and standard error of the ES (seES). A funnel plot with asymmetrical distribution indicated publication bias. Egger’s test was employed if the funnel plot asymmetry was caused by the small study effect. A contour-enhanced funnel plot was also utilized to find the possible causes of funnel plot asymmetry among the included studies. The significance of contour-enhanced funnel plots (p < 0.01) indicated that the cause of funnel plot asymmetry might be more likely other factors such as heterogeneity, selection bias, and quality of the included studies than publication bias.
Results
Search results
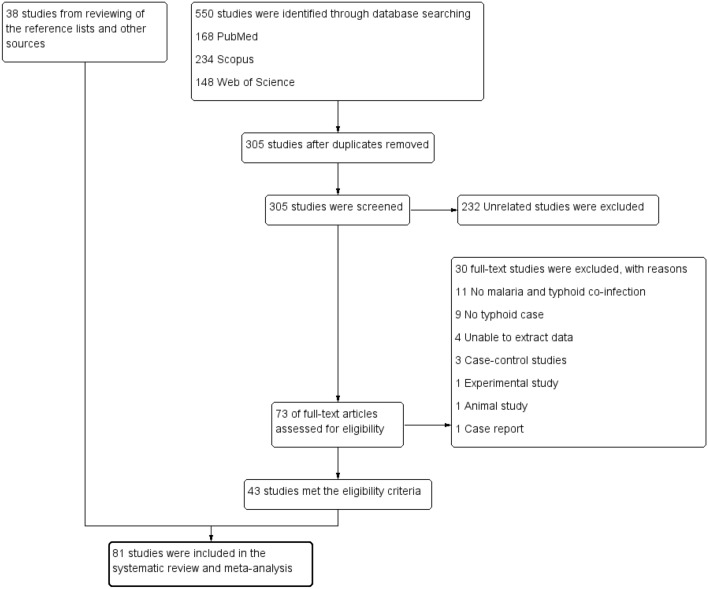
A total of 550 studies were retrieved from the three databases (168 from PubMed, 234 from Scopus, and 148 from Web of Science). After removal of 245 duplicated studies, the titles and abstracts of 305 studies were screened. After excluding 232 unrelated studies, 73 were retained for full-text examination. A total of 30 studies were excluded for the following reasons: 11 studies had no malaria and typhoid co-infection cases, 9 studies had no typhoid cases, data could not be extracted from 4 studies, 3 were case–control studies, 1 was an experimental study, 1 was an animal study, and 1 study was a case report. Finally, 43 studies17,20,30,35–74 were included. Thirty-eight studies27–29,31,75–108 from additional searches of reference lists and Google Scholar were included. Thus, 81 studies met the eligibility criteria and thus included in the qualitative and quantitative analyses (Fig. 1).
Figure 1.
Study flow diagram.
Characteristics and quality of the included studies
The characteristics of the included studies are presented in Table 1. A total of 76 studies were cross-sectional or retrospective studies, whereas 5 were prospective studies. All studies were published between 1987 and 2021. In Africa, 61 studies (75.3%) were conducted; in Asia, 19 studies (23.4%); and in Europe, 1 study. The African studies were conducted in Nigeria (30/61, 49.2%)36–38,42,47,48,50,51,57,59,61,64,75,77,82–84,89–91,94–101,103,107, Cameroon (5/61, 8.2%)35,40,73,92,93, Ghana (5/61, 8.2%)41,53,56,76,85, Kenya (5/61, 6.2%)28,29,60,72,80, Tanzania (4/61, 6.56%)20,39,44,46, Malawi17,27,30, Burkina Faso54,86, Mozambique79, Sierra Leone87, the Democratic Republic of the Congo49, Ethiopia45, Gabon55, and Gambia31, and one study was conducted in Burkina Faso, Ethiopia, Ghana, Guinea-Bissau, Kenya, Madagascar, Senegal, South Africa, Sudan, and Tanzania62. The Asian studies were conducted in India (12/19, 63.2%)43,66–68,71,74,81,88,104–106,108, Pakistan (4/19, 21.1%)52,65,70,102, Myanmar58,78, and Vietnam63. One study was conducted in Sweden69.
Table 1.
Characteristics of the included studies.
| Author | Study site | Year conducted | Study design | Participants | Age | Sex (M:F) | All co-infection | Salmonella spp. with typhoid | Salmonella spp. with non-typhoid | All malaria cases | Malaria without typhoid | Typhoid without malaria | Test for malaria | Test for typhoid |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abah et al. (2019)75 | Nigeria | 2016 | Cross-sectional study | 500 Febrile patients | 1–60 years | 244:256 | 115 | 115 | 0 | 278 | 163 | 85 | Microscopy | Widal test |
| Achonduh-Atijegbe et al. (2016)35 | Cameroon | 2014 | Cross-sectional study | 315 Febrile children (6 months–15 years) | 5.8 years (± 3.8) | 157:158 | 14 | 14 | 193 | 179 |
S. typhi and S. paratyphi (14) |
Microscopy, RDT, PCR | Rapid diagnostic test | |
| Afoakwah et al. (2011)76 | Ghana | NS | Cross-sectional study | 129 Patients clinically diagnosed as having malaria | 5–83 years | 0.58125 | 6 | 6 | 24 | 18 | 26 | RDT | Widal test | |
| Agwu et al. (2009)36 | Nigeria | 2003–2004 | Cross-sectional study | 560 Febrile known HIV/AIDS (239 male and 321 female) patients | < 10 years (30), 11–20 (86), 21–30 (252), 31–40 (183), 41–50 (7), > 50 (2) | 239:321 | 117 | 117 | 418 | P. falciparum (301) | S. typhi (73) | Microscopy | Widal test | |
| Akinyemi et al. (2007)37 | Nigeria | 2004–2005 | Cross-sectional study | 235 Febrile patients | 0–5 years (29), 6–15 (31), 16–30 (22), 31–45 (15), > 46 (10) | 16 | 16 | 0 | 107 | 91 | 26 | Microscopy | Blood culture | |
| Akinyemi et al. (2015)38 | Nigeria | 2010–2011 | Cross-sectional study | 135 Febrile patients | NS | NS | 4 | 4 | 9 | 5 |
S. typhi (22), S. paratyphi (7) |
Microscopy | Blood culture | |
| Alhassan et al. (2012)77 | Nigeria | NS | Cross-sectional study | 300 Febrile patients | 0 to > 60 years | 143:157 | 4 | 4 | 51 | 47 | NS | Microscopy | Blood culture | |
| Ali et al. (2020)39 | Tanzania | 2015 | Cross-sectional study | 149 Febrile patients | Mean, 22 years; range, 1–70 | 62:87 | 1 | 1 | 7 | 6 | 0 | Molecular method | Molecular method | |
| Ammah et al. (1999)40 | Cameroon | 1997–1998 | Cross-sectional study | 200 Febrile patients | Mean, 28 years (± 20.1); range, 4–75 | 88:112 | 103 | 38 | 65 | 115 | 12 |
S. typhi (10), S. paratyphi (5), S. typhimurium (4) |
Microscopy | Widal test |
| Anabire et al. (2018)41 | Ghana | 2015 | Cross-sectional study | 150 Febrile children | Median, 3 years (IQR, 2–8 years) | 77:73 | 9 | 9 | 85 | 76; median age, 4.0 (2.0–8.0); anemia (55/76); thrombocytopenia (47/76); leukopenia (2/76); CBC | S. typhi (20): median age, 6.5 (3.0–11.0); anemia (12/20); thrombocytopenia (2/20); leukopenia (0); CBC | Microscopy, RDT | Widal test | |
| Anjorin et al. (2020)42 | Nigeria | 2016–2018 | Cross-sectional study | 182 Pregnant women having influenza-like illness | Mean, 29.3 years; range, 18–45 | 34 | 34 | 34 | NS | Rapid diagnostic test | ||||
| Aung et al. (2018)78 | Myanmar | 2016–2017 | Prospective study | 20 Patients with P. falciparum | > 16 years | 19:01 | 1 | 1 | 20 | 19 | NS | Microscopy, RDT | Blood culture | |
| Bassat et al. (2009)79 | Mozambique | 2003–2007 | Retrospective study | 1404 Children with severe malaria | < 5 years | NS | 12 | 0 | 12 | 1404 | 1382 | NS | Microscopy | Blood culture |
| Berkley et al. (1999)80 | Kenya | 1993–1996 | Prospective study | 783 Children with severe malaria | NS | 396:387 | 6 | 0 | 6 | 783 | 777 | NS | Microscopy | Blood culture |
| Bhalla et al. (2019)43 | India | 2018 | Cross-sectional study | 607 Patients with dengue, malaria, leptospirosis, typhoid, and rickettsia diseases | NS | Positive cases (male, 383:224) | 1 | 1 | 372 | 371 | 45 | Microscopy | Widal test | |
| Bhattacharya et al. (2013)81 | India | 2004 | Prospective study | 3371 Febrile patients | Mean, 24.7 years | 1730 :1641 | 2 | 2 | 0 | 93 | 91 | 159 | Microscopy | Blood culture |
| Biggs et al. (2014)44 | Tanzania | 2006–2007 | Cross-sectional study | 3639 Febrile children | Median 1.57 years (0.2–13.0) | 1970: 1669 | 53 | 53 | 2195 | 2142 | S. typhi (11), non-typhoidal Salmonella (109) | Microscopy, RDT | Blood culture | |
| Birhanie et al. (2014)45 | Ethiopia | 2013 |
Cross-sectional Study |
200 Febrile patients | 24.24 ± 13.4, range 2 to > 46 | 120:80 | 13 | 13 | 73 | 60 | 25 | Microscopy | Widal test | |
| Brent et al. (2006)29 | Kenya | 1998–2002 | Prospective study | 166 Non-typhoidal Salmonella | Median 15 months (8–27) | 54 | 0 | 54 | 54 | 0 | 112 | ELISA | Blood culture | |
| Bronzan et al. (2007)30 | Malawi | 1996–2005 | Cross-sectional study | 1388 Severe malaria with bacteriamia | Children > 6 months | 37 | 37 | 1388 | 1351 | NS | Microscopy | Blood culture | ||
| Chipwaza et al. (2015)46 | Tanzania | 2013 | Cross-sectional study | 370 Febrile patients | 2–13 years | 189:181 | 13 | 13 | 98 | 85 | 38 | Microscopy | Widal test | |
| Chukwuma et al. (2014)82 | Nigeria | 2012–2013 | Cross-sectional study | 350 Pregnant women | 5 | 5 | 0 | 10 | 5 | 1 | Microscopy | Stool culture | ||
| Edet et al. (2016)83 | Nigeria | 2014–2015 | Cross-sectional study | 100 Febrile patients | 10–80 years | 43:57:00 | 11 | 11 | 0 | 41 | 30 | 0 | Microscopy | Blood culture |
| Ekesiobi et al. (2017)84 | Nigeria | NS | Cross-sectional study | 256 Febrile patients | 1 to > 35 years | 128:128 | 29 | 25 | 4 | 202 | 173 | 9 | Microscopy | Stool culture |
| Enabulele et al. (2016)47 | Nigeria | NS | Cross-sectional study | 271 Febrile patients | > 18 years | NS | 5 | 5 | 193 | 188 | 24 | Microscopy | Widal test | |
| Evans et al. (2004)85 | Ghana | NS | Cross-sectional study | 23 Children with severe malaria | NS | NS | 10 | 0 | 10 | 23 | 13 | 19 | Microscopy | Blood culture |
| Eze et al. (2011)48 | Nigeria | NS | Cross-sectional study | 25 Malaria cases | NS | NS | 3 | 3 | 25 | 22 | 0 | NS |
Widal tes t |
|
| Falay et al. (2016)49 | Democratic Republic of the Congo | 2012 | Cross-sectional study | 16 S. typhi positive, 107 Non-typhoidal Salmonella | S. typhi positive (median 96 (48–123) months), non-typhoidal Salmonella (median 24 (12–36)) | S. typhi positive (7:9), non-typhoidal Salmonella (63:45) | 63 | 5 | 58 | 0 | S. typhi positive (11), non-typhoidal Salmonella (59) | Microscopy, RDT | Blood culture | |
| Graham et al. (2000)17 | Malawi | 1996–1998 | Cross-sectional study | 219 Non-typhoidal Salmonella | > 6 months | NS | 82 | 82 | 0 | 144 | Microscopy | Blood culture | ||
| Ibrahim et al. (2019)86 | Burkina Faso | 2014 | Cross-sectional study | 283 Malaria cases | Median 18 (0–85 years) | 140:143 | 91 | 91 | 0 | 283 | 192 | NS | Microscopy | Widal test |
| Igbeneghu et al. (2009)50 | Nigeria | NS | Cross-sectional study | 258 Febrile Patients | NS | NS | 1 | 1 | 161 | 160 | 1 | Microscopy | Blood culture | |
| Igharo et al. (2012)51 | Nigeria | NS | Cross-sectional study | 234 Febrile patients | NS | 113:121 | 43 | 43 | 88 | 45 | 130 | Microscopy | Widal test | |
| Jalani et al. (2019)52 | Pakistan | 2017 | Cross-sectional study | 144 Febrile patients | 1–10 (75), 11–20 (35), > 20 (34) | 74:70 | 9 | 9 | 20 | 11 | 86 | Microscopy | Widal test | |
| Kargbo et al. (2014)87 | Sierra Leone | 2013–2014 | Cross-sectional study | 11,069 Febrile patients | 5–70 years |
5245: 5824 |
2101 | 2101 | 0 | 8849 | 6748 | 554 | Microscopy | Widal test |
| Katiyar et al. (2020)88 | India | 2018 | Cross-sectional study | 780 Malaria cases | 0–80 years | 425:355 | 122 | 122 | 0 | 780 | 658 | NS | Microscopy, RDT | Widal test |
| Krumkamp et al. (2016)53 | Ghana | 2007–2012 | Cross-sectional study | 6746 Febrile patients | < 15 years | 33 | 33 | 2563 | 2530 | Non-typhoidal Salmonella (160), S. typhi (93) | Microscopy | Blood culture | ||
| Mabey et al. (1987)31 | Gambia | 1979–1984 | Cross-sectional study | 116 Patients with typhoidal/non-typhoidal Samonella | 35 | 5 | 30 | 35 | NS | 81 | Microscopy | Blood culture | ||
| Maltha el al. (2014)54 | Burkina Faso | 2012–2013 | Cross-sectional study | 711 Severe malaria | Median 19 (10–36) | 393:318 | 33 | 12 | 21 | 711 | 678 | 0 | Microscopy, RDT | Blood culture |
| Mbuh et al. (2003)89 | Nigeria | 1996 | Cross-sectional study | 218 Febrile patients | 2–59 years | 118:100 | 1 | 1 | 0 | 60 | 59 | 0 | Microscopy | Blood culture |
| Mike et al. (2017)90 | Nigeria | 2015 | Retrospective study | 627 Febrile patients | 1–75 years | 375:252 | 136 | 136 | 0 | 233 | 97 | 49 | Microscopy | Widal test |
| Mohammed et al. (2020)91 | Nigeria | 2020 | Cross-sectional study | 429 Pregnant women | 21–30 years | 429 | 12 | 12 | 0 | 123 | 111 | 33 | Microscopy, RDT | Rapid diagnostic test |
| Mourembou et al. (2016)55 | Gabon | NS | Cross-sectional study | 410 Febrile patients | < 16 years | 212:198 | 3 | 323 | 320 | 0 | Molecular method | Molecular method | ||
| Mtove et al. (2010)20 | Tanzania | 2008–2009 | Cross-sectional study | 156 Children with pathogenic bacteriamia | 2 months to 14 years | 34 | 3 | 31 | 0 | S. typhi (11), non-S. Typhi (14) | Microscopy, RDT | Blood culture | ||
| Ndip et al. (2015)92 | Cameroon | 2010 | Cross-sectional study | 206 Febrile patients | 4–80 years | 12 | 12 | 0 | 186 | 174 | 14 | Microscopy | Stool culture | |
| Nielsen et al. (2015)56 | Ghana | 2007–2011 | Cross-sectional study | 771 Malaria cases | < 15 years | 1049:866 | 21 | 21 | 771 | 750 | 0 | Microscopy | Blood culture | |
| Njolle et al. (2020)93 | Cameroon | 2015 | Cross-sectional study | 160 Febrile patients | 18 months–60 years | 81:79 | 12 | 9 | 3 | 31 | 19 | Typhoid (55), non-typhoidal Salmonella (24) | Microscopy | Stool culture |
| Nwabueze et al. (2013)94 | Nigeria | NS | Cross-sectional study | 700 Pregnant women | NS | NS | 236 | 236 | 0 | 512 | 276 | NS | Microscopy | Widal test |
| Nwuzo et al. (2009)57 | Nigeria | 2007 | Cross-sectional study | 250 Febrile patients | 0–70 years | 123:127 | 14 | 14 | 33 | 19 | S. typhi (39) | RDT | Blood culture | |
| Nyein et al. (2016)58 | Myanmar | 2014–2015 | Cross-sectional study | 67 Adults with P. falciparum | Adults | NS | 4 | 3 | 1 | 67 | 63 | 0 | Microscopy, RDT | Blood culture |
| Odikamnoro et al. (2018)59 | Nigeria | NS | Cross-sectional study | 350 Febrile patients | All age groups | 164:186 | 127 | 127 | 190 | 63 | 46 | Microscopy | Widal test | |
| Ohanu et al. (2003)95 | Nigeria | 1997–1998 | Cross-sectional study | 270 Febrile patients | 15–59 years | 130:140 | 16 | 16 | 0 | 60 | 44 | 22 | Microscopy | Blood and stool culture |
| Omoya et al. (2017)96 | Nigeria | 2015 | Cross-sectional study | 170 Pregnant women | 16–45 years | 170 | 79 | 79 | 0 | 112 | 33 | 35 | Microscopy | Widal test |
| Onyido et al. (2014)97 | Nigeria | 2012 | Cross-sectional study | 200 Healthy individuals | 1–80 years | 52:148 | 10 | 10 | 0 | 50 | 40 | 11 | Microscopy | Widal test |
| Orok et al. (2016)98 | Nigeria | 2015 | Cross-sectional study | 250 Febrile patients | 1–75 years | 113:137 | 2 | 2 | 0 | 202 | 200 | NS | Microscopy | Blood culture |
| Oshiokhayamhe et al. (2021)99 | Nigeria | NS | Cross-sectional study | 200 Students | 18–30 years | 100:100 | 5 | 5 | 0 | 10 | 5 | 25 | Microscopy | Widal test |
| Oundo et al. (2002)60 | Kenya | 1997–2001 | Cross-sectional study | 9147 Children with severe malaria | Mean 22.28 months (25.3) | 101 | 101 | 9248 | 9147 | Non-typhoidal Salmonella (352) | Microscopy | Blood culture | ||
| Ozumba et al. (2020)100 | Nigeria | 2015 | Cross-sectional study | 200 Pregnant women | < 20 to 60 years | 200 | 8 | 8 | 0 | 16 | 8 | 78 | Microscopy | Widal test |
| Pam et al. (2015)101 | Nigeria | 2015 | Cross-sectional study | 250 Pregnant women | < 20 to 60 years | 250 | 9 | 9 | 0 | 16 | 7 | 68 | RDT | Widal test |
| Pam et al. (2018)61 | Nigeria | 2015 | Cross-sectional study | 200 Pregnant women | < 20 (6), 21–30 (110), 31–40 (72), 41–50 (10), 51–60 (2) | All were females | 9 | 9 | 25 | 16 | 86 | Microscopy, RDT | Widal test | |
| Park et al. (2016)62 | Burkina Faso, Ethiopia, Ghana, Guinea-Bissau, Kenya, Madagascar, Senegal, South Africa, Sudan, and Tanzania | 2010–2014 | Cross-sectional study | 497 Febrile patients | All age groups | NS | 24 | 9 | 15 | 0 | 473 | Microscopy, RDT | Blood culture | |
| Phu et al. (2020)63 | Vietnam | 1991–2003 | Cross-sectional study | 845 Adult patients admitted with severe falciparum malaria | > 14 years | NS | 4 | 3 | 1 | 840 | 836, mean age 31 years, range 15–79 years, median parasite count 81,766/μL (12,811 to 316,512/μL) | 0 | Microscopy | Blood culture |
| Popoola et al. (2019)64 | Nigeria | 2017 | Cross-sectional study | 682 Febrile patients | < 1 (7), 1–5 (217), 6–12 (189), 13–17 (61), 18–59 (198), ≥ 60 (10) | 332:350 | 7 | 6 | 1 | 171 | 164 | S. typhi (21), non-typhoidal Salmonella (5) | Microscopy | Molecular method |
| Qureshi et al. (2019)65 | Pakistan | 2012–2013 | Cross-sectional study | 1889 Febrile patients | All age groups | Infected cases 164:147 | 11 | 11 | 128 | 117 age 1–12 (67), 13–60 (50) | 183, age 1–12 (110), 13–60 (73) | Microscopy | Rapid diagnostic test | |
| Raja et al. (2016)66 | India | 2013–2014 | Cross-sectional study | 100 Febrile patients | NS | NS | 2 | 2 | 10 | 8 | 6 | Microscopy, RDT | Blood culture | |
| Ramya et al. (2017)67 | India | 2010–2012 | Cross-sectional study | 824 Malaria, typhoid, dengue cases | NS | NS | 55 | 55 | NS | NS | RDT | Widal test | ||
| Sajid et al. (2017)102 | Pakistan | NS | Cross-sectional study | 300 Febrile patients | 1 to > 46 years | 150:150 | 21 | 21 | 65 | 44 | 16 | Microscopy | Widal test | |
| Sale et al. (2020)103 | Nigeria | NS | Cross-sectional study | 200 Febrile patients | ≤ 10 to > 30 years | 96:104 | 45 | 45 | 0 | 111 | 66 | 33 | Microscopy, RDT | Widal test |
| Samatha et al. (2015)68 | India | 2014–2015 | Cross-sectional study | 582 Febrile patients | NS | NS | 4 | 4 | 306 | 302 | Widal test 132, culture 7 | Microscopy | Blood culture | |
| Sandlund et al. (2012)69 | Sweden | 1995–2009 | Cross-sectional study | 755 Malaria patients | Mean 33.6 (15.2 years), range 1–79 years (13.68 years), range 18–77 years | 01:01.0 | 4 | 4 | 755 | 751 | 0 |
Microscopy, RDT, molecular Method |
Blood culture | |
| Shaikh et al. (2018)70 | Pakistan | 2017–2018 | Cross-sectional study | 985 Febrile patients | Malaria positive: mean 38.63 | Malaria positive: 209:181 | 52 | 52 | 442 | 390 | 250 | NS | Widal test | |
| Sharma et al. (2016)104 | India | 2014–2016 | Cross-sectional study | 3010 Febrile patients | Children and adults | 2260:750 | 48 | 48 | 0 | 210 | 162 | 12 | Microscopy, RDT | Blood culture |
| Singh et al. (2014)71 | India | 2013 | Cross-sectional study | 1141 Febrile patients | ≥ 12 years | 618:523 | 1 | 1 | 147 | 146 | 92 | Microscopy, RDT | Blood culture | |
| Snehanshu et al. (2014)105 | India | 2012–2013 | Cross-sectional study | 200 Febrile patients | 0 to > 60 years | 88:112 | 5 | 5 | 0 | 36 | 31 | NS | Microscopy | Blood culture |
| Sur et al. (2006)106 | India | 2004 | Prospective study | 3371 Febrile patients | 0 to > 70 years | NS | 3 | 3 | 0 | 93 | 90 | 92 | Microscopy | Blood culture |
| Tabu et al. (2012)72 | Kenya | 2006–2009 | Cross-sectional study | 3578 Febrile (60 non-typhoidal Salmonella investigated for malaria) | NS | NS | 12 | 12 | NS | NS | Non-typhoidal Salmonella (48) | Microscopy | Blood culture | |
| Tchuandom et al. (2018)73 | Cameroon | 2016–2017 | Cross-sectional study | 961 Febrile patients | ≤ 15 years, mean 7.1 (2.9 years) | 495:466 | 6 | 6 | 396 | 390 | 22 | RDT | RDT | |
| Ukaegbu et al. (2014)107 | Nigeria | NS | Cross-sectional study | 300 Febrile patients | 0 to > 60 years | 117:183 | 9 | 9 | 0 | 162 | 153 | NS | Microscopy | Stool culture |
| Vats et al. (2018)108 | India | NS | Cross-sectional study | 300 Febrile patients | 1–60 years | 206:94 | 3 | 3 | 0 | 31 | 28 | 9 | Microscopy | Blood culture |
| Verma et al. (2014)74 | India | 2012 | Cross-sectional study | 800 Febrile patients | NS | NS | 9 | 9 | NS | NS | NS | Microscopy, RDT | Blood culture | |
| Walsh et al. (2000)27 | Malawi | 1996–1997 | Cross-sectional study | 128 Non-typhoidal Salmonella | 0–13 years | NS | 32 | 0 | 32 | 32 | NS | 96 | Microscopy | Blood culture |
| Were et al. (2011)28 | Kenya | 2004–2006 | Cross-sectional study | 585 Children with P. falciparum | 1–36 months | 295:290 | 24 | 0 | 24 | 585 | 561 | NS | Microscopy | Blood culture |
ELISA enzyme-linked immunosorbent assay, NS not specified, RDT rapid diagnostic test.
Among the 81 studies included in the analysis, 49 studies (60.5%) enrolled febrile patients35–41,43–47,50–53,55,57,59,62,64–68,70–77,81,83,84,87,89,90,92,93,95,98,102–108, 8 studies enrolled pregnant women42,61,82,91,94,96,100,101, 6 studies enrolled patients with severe malaria30,54,63,79,80,85, 9 studies enrolled malaria positive patients28,48,56,58,60,69,78,86,88, 5 studies enrolled typhoid/non-typhoid-positive patients17,27,29,31,49, and one study enrolled children with pathogenic bacteremia20. Co-infections with malaria and typhoidal/NTS were reported in 4,523 cases from 73,775 total patients enrolled in the 81 included studies. Co-infections with malaria and typhoidal Salmonella spp., including S. typhi and S. paratyphi, were reported in 3813 cases from 56 studies31,36,38,39,41–43,45–48,50–52,57,59,61,65–68,70,71,73–78,81–84,86–108. Co-infections with malaria and NTS, such as S. typhimurium, were reported in 707 cases from 18 studies17,27–31,44,53,56,60,62,69,72,79,80,84,85,93. Co-infections with malaria and both typhoidal and NTS spp. were reported in 13 studies20,31,35,37,40,49,54,55,58,63,64,84,93.
Salmonella spp. infection was identified using blood cultures (39/81, 48.1%)17,20,27–31,37,38,44,47,49,50,53,54,56–58,60,62,63,66,68,69,71,72,74,77–81,83,85,89,98,104–106,108, Widal test (27/81, 33.3%)36,40,41,43,45,46,48,51,52,59,61,67,70,75,86–88,90,94,96,97,99–103, stool cultures (5/81, 6.17%)82,84,92,93,107, RDTs (4/81, 4.94%)35,42,73,91, and molecular methods (3/43, 6.98%)39,55,64. One study95 employed both blood and stool cultures. Some studies used combinations of methods to identify Salmonella spp. infection. However, only a definitive method was demonstrated in this qualitative synthesis. For the identification of malaria, Plasmodium spp. infections were identified via microscopy alone (52/81, 64.2%)17,27,28,30,31,36–38,40,43,45–47,50–53,56,59,60,63–65,68,72,75,77,79–87,89,90,92–100,102,105–108, microscopy/RDT (16/81, 19.8%)20,41,44,49,54,58,61,66,69,71,74,78,88,91,103,104, RDT alone (5/81, 6.17%)57,67,73,76,101, molecular method39,55, microscopy/RDT/molecular method35,69, not specified42,48,70, and ELISA29.
Among the 81 studies included in the present study, 30 (37%) were rated as low risk of bias, whereas 51 studies had a moderate risk of bias (51/81, 63%). Studies with a high risk of bias were removed during the study selection (Supplementary Table S2).
Prevalence of typhoidal and NTS and malaria co-infections among febrile patients
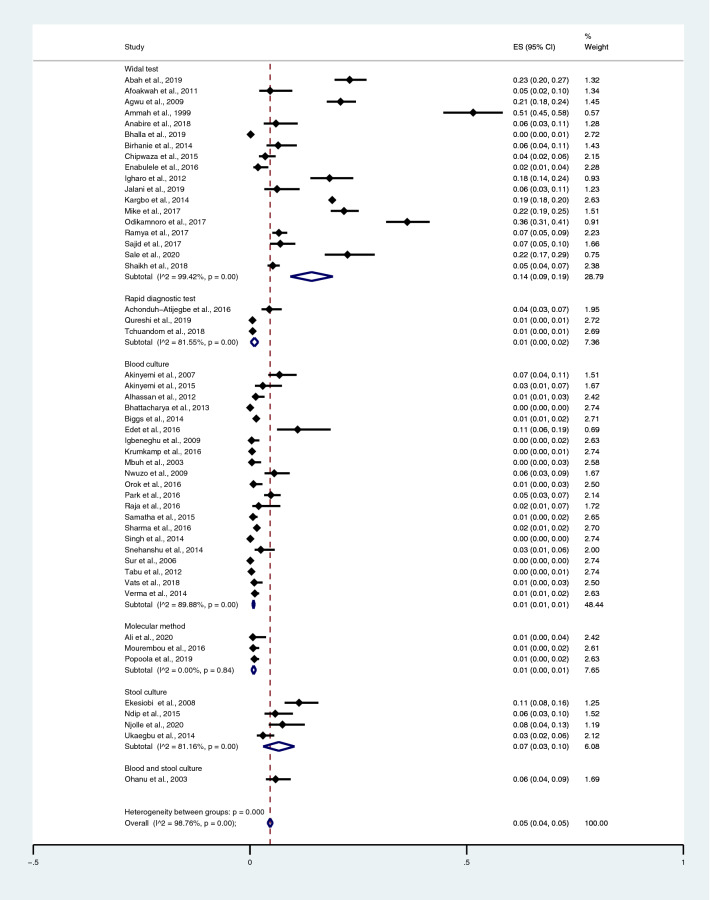
The pooled prevalence rate of typhoidal/NTS and malaria co-infections among febrile patients was estimated from 50 studies35–41,43–47,50–53,55,57,59,62,64–68,70–77,81,83,84,87,89,90,92,93,95,98,102–108. The studies were divided into four groups based on diagnostic tests for Salmonella spp. The results indicated that the pooled prevalence rates of typhoidal/NTS and malaria co-infections among febrile patients were 14% (95% CI 9–19%; I2, 99.4%) using the Widal test, 1% (95% CI 1–1%; I2, 89.9%) using blood culture, 1% (95% CI 0–2%; I2, 81.6%) using RDTs, 1% (95% CI 0–1%; I2, 0%) using a molecular method, 7% (95% CI 3–10%; I2, 81.2%) using stool cultures, and 6% (95% CI 4–9%) using a combination of blood and stool cultures (Fig. 2).
Figure 2.
The pooled prevalence of typhoidal/NTS and malaria co-infection among febrile patients detected using diagnostic tests for Salmonella spp. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval.
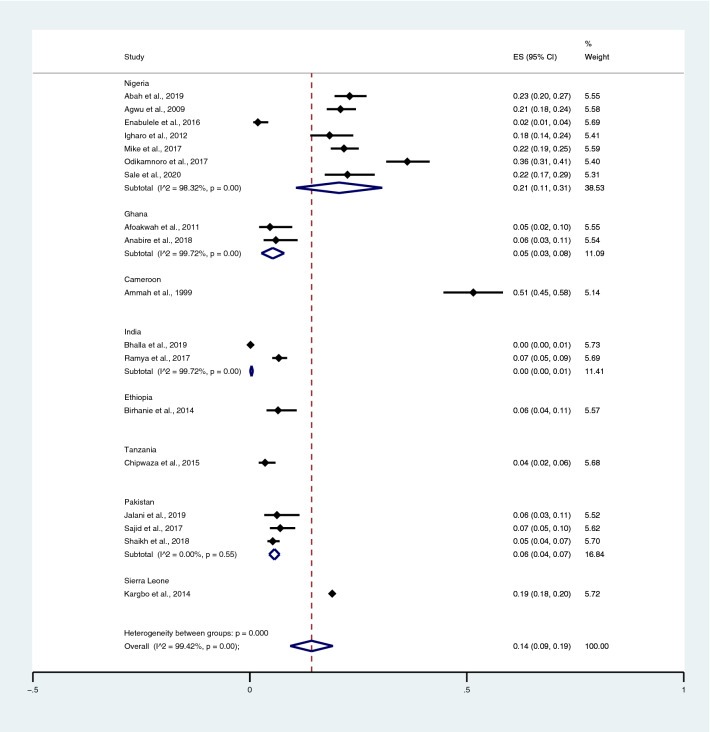
When Salmonella spp. infections were detected using the Widal test, the highest prevalence rate of co-infections was noted in Cameroon (51%; 95% CI 45–58%) and Nigeria (21%; 95% CI 11–31%; I2, 98.3%), whereas lower prevalence rates were detected in Sierra Leone (19%; 95% CI 18–20%), Ethiopia (6%; 95% CI 4–11%), Pakistan (6%; 95% CI 4–7%; I2, 0%), Ghana (5%; 95% CI 3–8%; I2, 99.7%), India (0%; 95% CI 0–1%; I2, 99.7%), and Tanzania (4%; 95% CI 2–6%) (Fig. 3).
Figure 3.
Pooled prevalence of typhoidal/NTS and malaria co-infection using the Widal test for the identification of Salmonella spp. infection stratified by countries. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval.
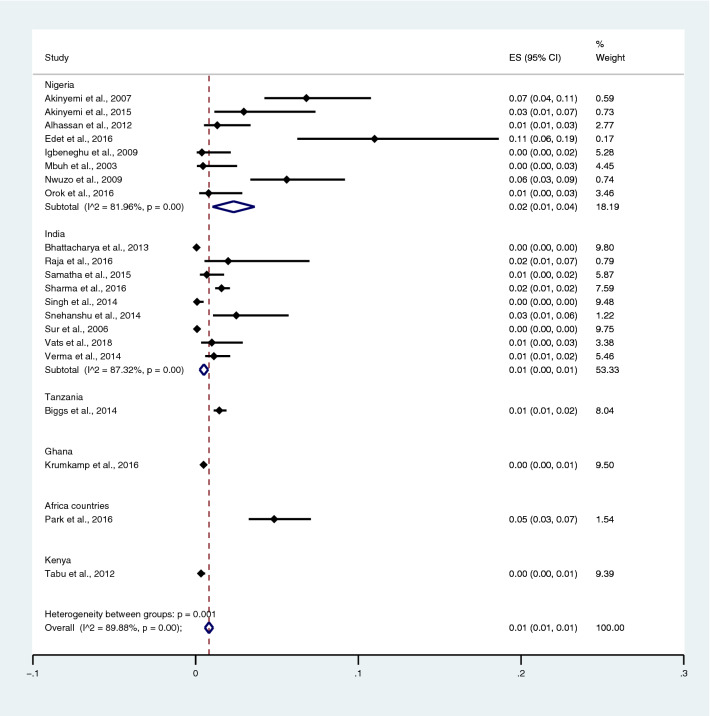
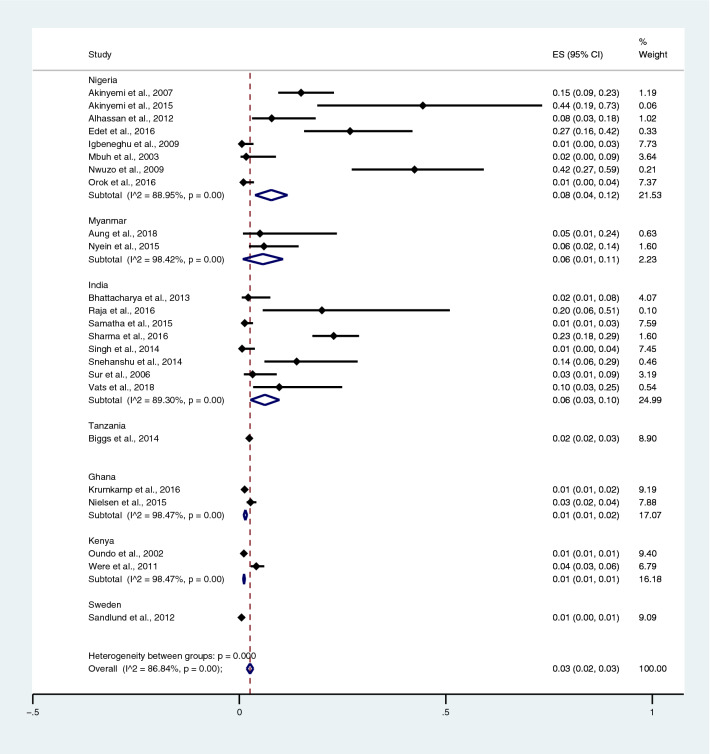
Among the studies using blood culture for the identification of Salmonella spp. infections, the highest prevalence of co-infection was reported in Burkina Faso, Ethiopia, Ghana, Guinea-Bissau, Kenya, Madagascar, Senegal, South Africa, Sudan, and Tanzania (5%; 95% CI 3–7%). Contrarily, lower prevalence was reported in Nigeria (2%; 95% CI 1–4%; I2, 82%), India (1%; 95% CI 0–1%; I2, 87.3%), Tanzania (1%; 95% CI 1–2%), Ghana (0%; 95% CI 0–1%), and Kenya (0%; 95% CI 0–1%) (Fig. 4).
Figure 4.
Pooled prevalence of typhoidal/NTS and malaria co-infection using blood cultures for the identification of Salmonella spp. infection stratified by countries. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval, NS not specified.
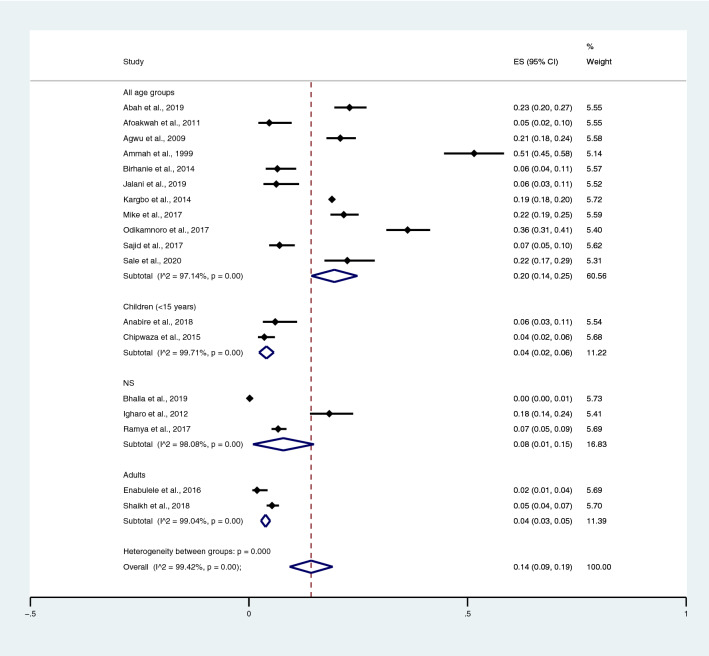
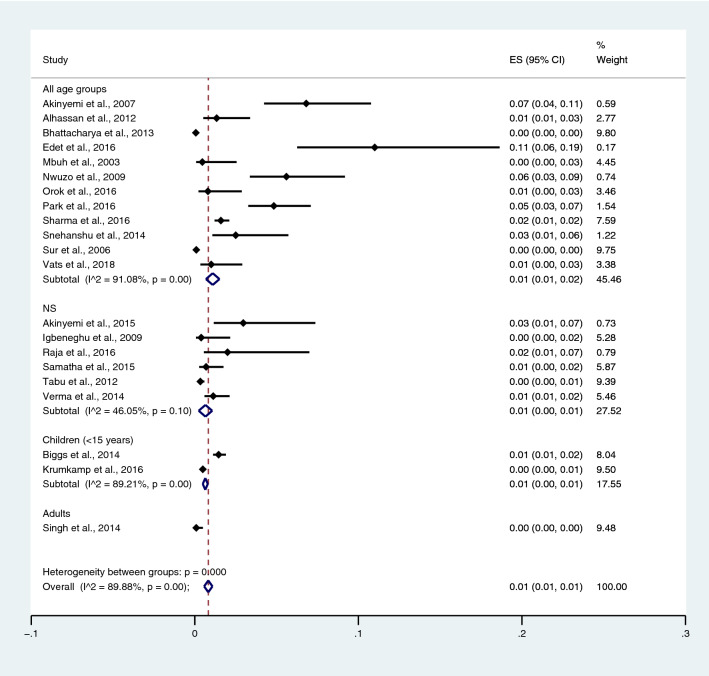
Among the studies using the Widal test for the identification of Salmonella spp. infections, the highest prevalence of co-infections was noted in the studies that enrolled participants in all age groups (95% CI 20%; 95% CI 14–25%; I2, 97.1%). The prevalence of co-infections was 4% in children (95% CI 2–6%; I2, 99.7%), 8% in the not specified (NS) age group (95% CI 1–15%), and 4% in adults (95% CI 3–5%; I2, 99%) (Fig. 5) when Salmonella spp. infections were detected using the Widal test. Among the studies using blood cultures for the identification of Salmonella spp. infections, the prevalence of co-infections was 1% in all age groups (95% CI 1–2%; I2, 91.1%), 1% in the NS group (95% CI 0–1%; I2, 46.1%), and 1% in children (95% CI 0–1%; I2, 89.2%) (Fig. 6).
Figure 5.
Pooled prevalence of typhoidal/NTS and malaria co-infection using the Widal test for the identification of Salmonella spp. infection stratified by age groups. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval.
Figure 6.
Pooled prevalence of typhoidal/NTS and malaria co-infection using blood cultures for the identification of Salmonella spp. infection stratified by age groups. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval, NS not specified.
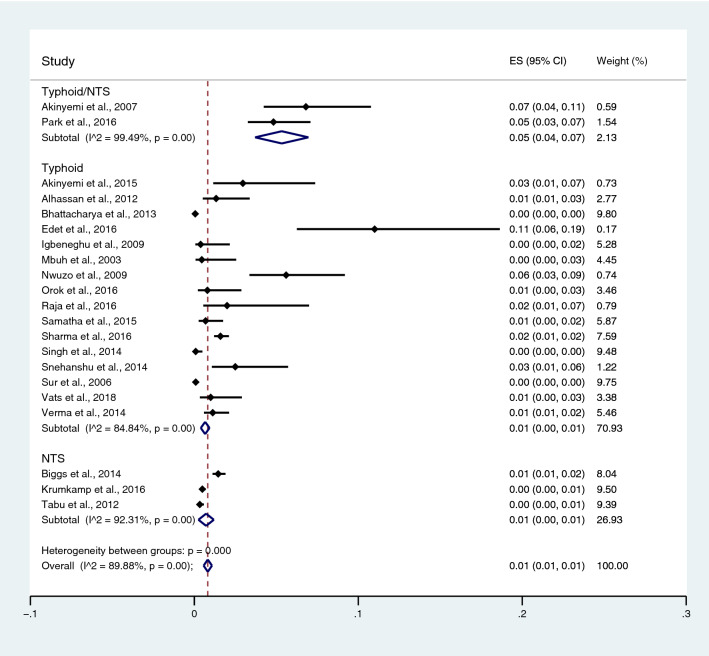
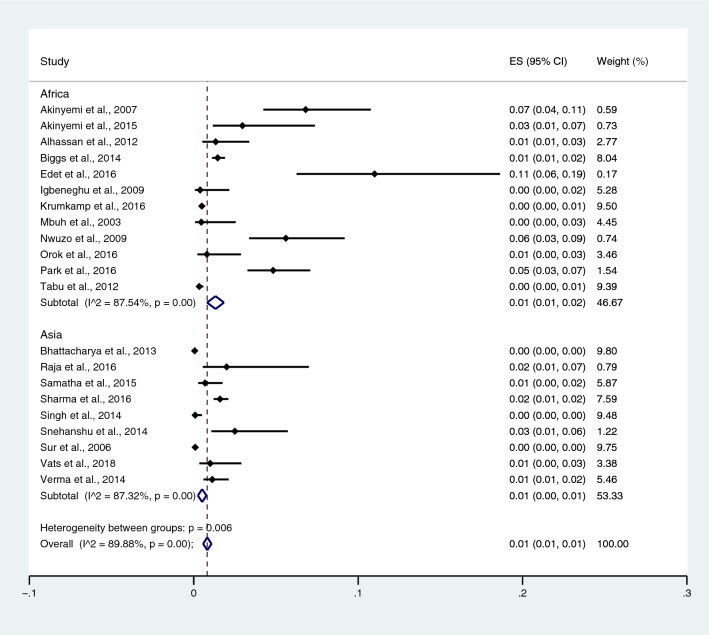
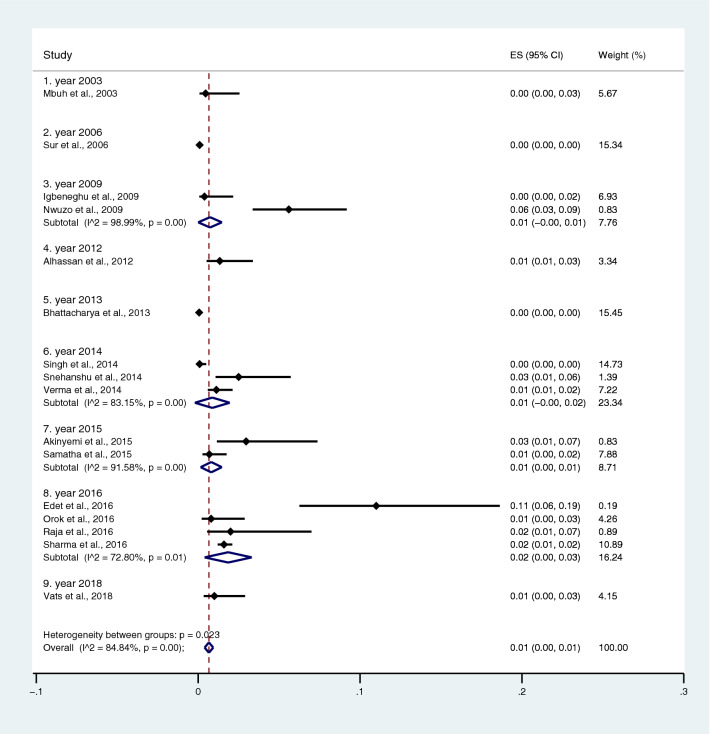
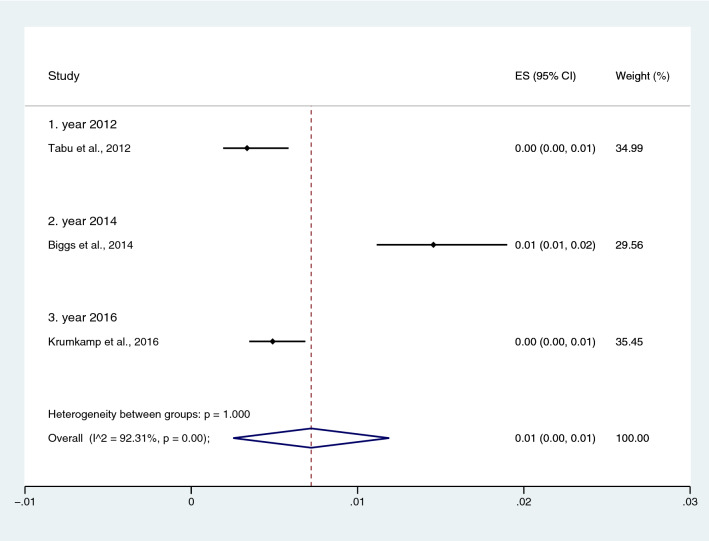
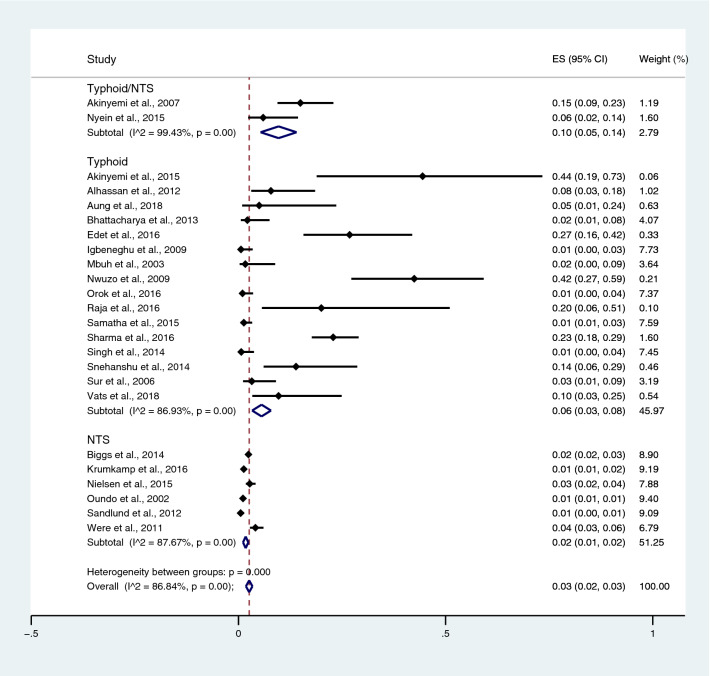
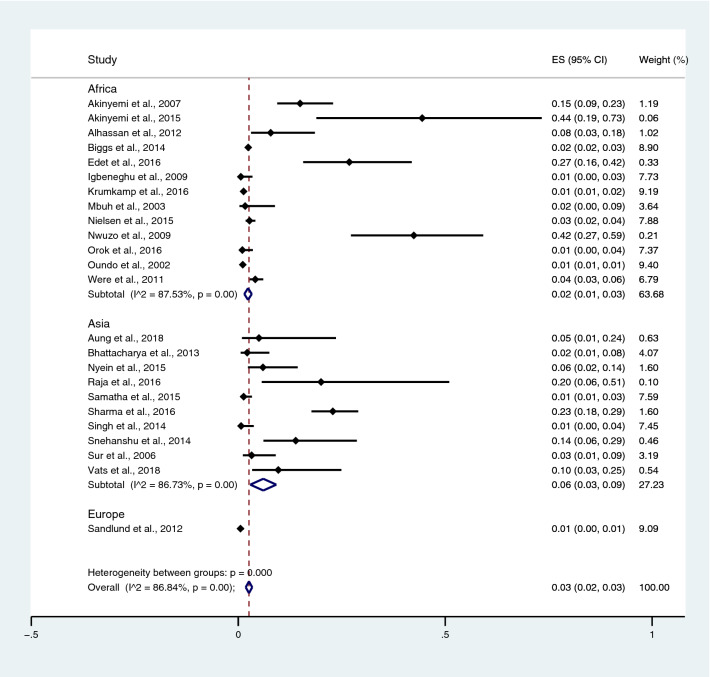
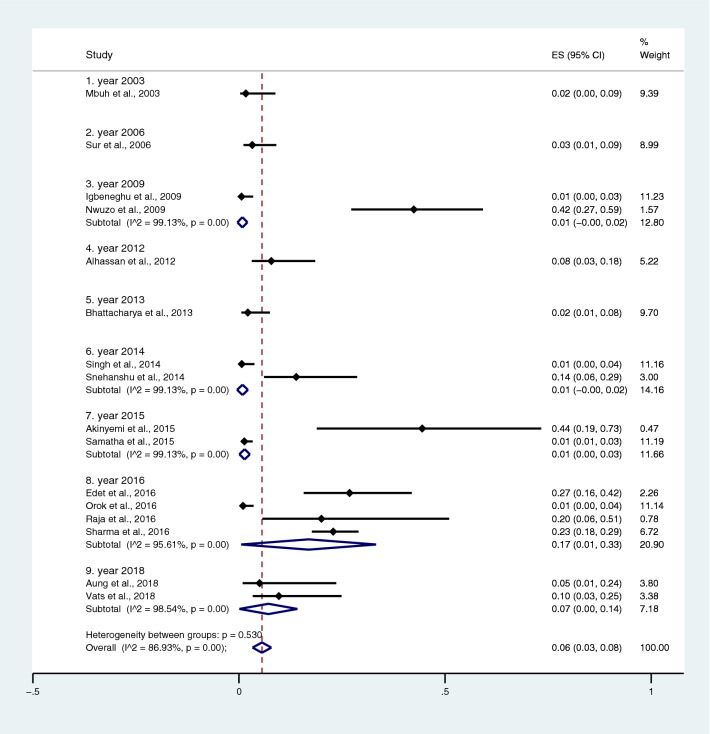
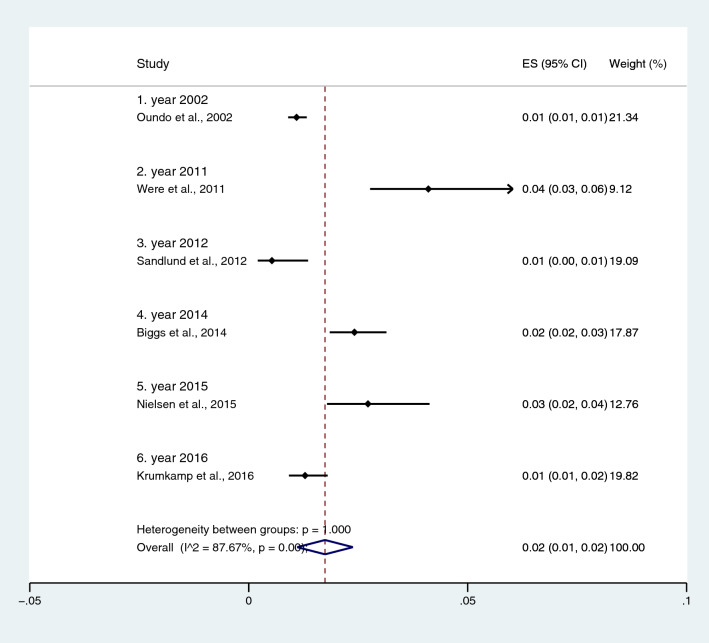
Subgroup analysis of typhoidal/NTS infection, regions (Africa and Asia), and time (publication year) was performed using the data from studies using blood culture for typhoidal/NTS identification37,38,44,50,53,57,62,66,68,71,72,74,77,81,83,89,98,104–106,108. Results showed that the prevalence rates of malaria and typhoid co-infections and malaria and NTS co-infections were 1% (95% CI 0–1%; I2, 84.8%) and 1% (95% CI 0–1%; I2, 92.3%) (Fig. 7). Subgroup analysis of regions showed that the prevalence rates of malaria and typhoidal/NTS co-infections were 1% in Africa (95% CI 1–2%; I2, 87.5%) and 1% in Asia (95% CI 0–1%; I2, 87.3%) (Fig. 8). Subgroup analysis of time showed that the prevalence rate of malaria and typhoid co-infections was highest (2%) in 2016 (95% CI 0–1%; I2, 72.8%) and 1% in 2009, 2012, 2014, and 2015 and 0% in 2003, 2006, 2013, and 2018 (Fig. 9). Subgroup analysis of time showed that the prevalence rate of malaria and NTS co-infections was highest (1%) in 2014 and 0% in 2012 and 2016 (Fig. 10).
Figure 7.
Pooled prevalence of typhoidal/NTS and malaria co-infection using blood cultures for the identification of Salmonella spp. infection stratified by typhoidal/NTS infection. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval, NS not specified.
Figure 8.
Pooled prevalence of typhoidal/NTS and malaria co-infection using blood cultures for the identification of Salmonella spp. infection stratified by regions. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval, NS not specified.
Figure 9.
Pooled prevalence of typhoidal and malaria co-infection using blood cultures for the identification of Salmonella spp. infection stratified by time (publication year). ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval, NS not specified.
Figure 10.
Pooled prevalence of NTS and malaria co-infection using blood cultures for the identification of Salmonella spp. infection stratified by time (publication year). ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval, NS not specified.
Prevalence of typhoidal/NTS infections among patients with malaria
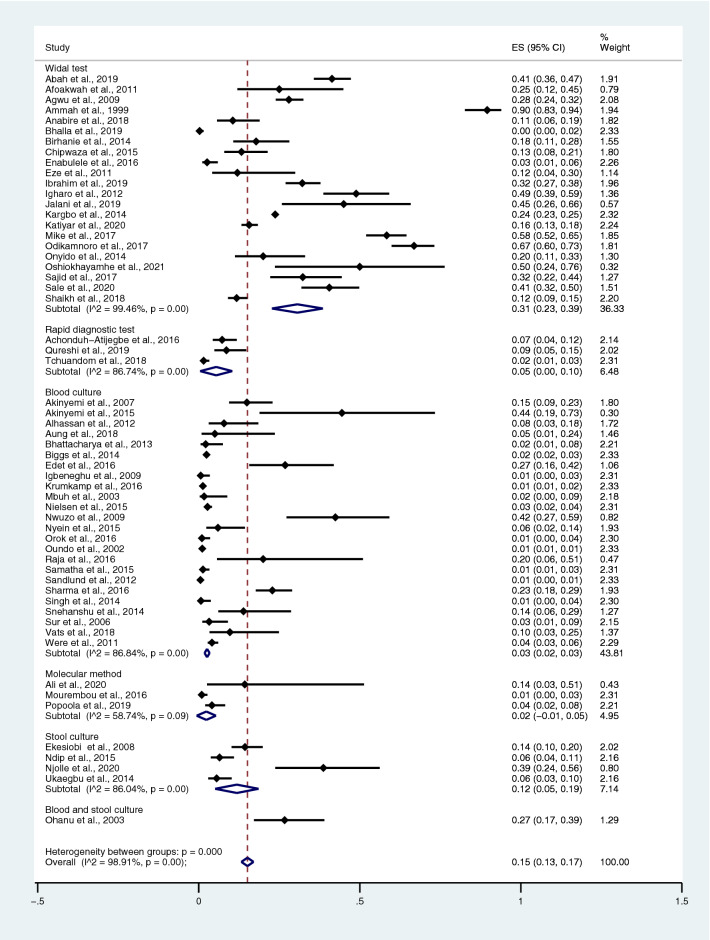
The pooled prevalence rate of typhoidal/NTS infection among malaria patients was estimated from 57 studies28,35–41,43–48,50–53,55–60,64–66,68–71,73,75–78,81,83,84,86–90,92,93,95,97–99,102–108. The studies were divided into groups based on diagnostic tests for Salmonella spp. The pooled prevalence rates of typhoidal/NTS infection among patients with malaria were 31% (95% CI 23–39%; I2, 99.5%) using the Widal test, 5% (95% CI 0–10%; I2, 86.7%) using RDTs, 3% (95% CI 2–3%; I2, 86.8%) using blood culture, 2% (95% CI − 1 to 5%; I2, 58.7%) using molecular methods, 12% (95% CI 5–19%; I2, 86%) using stool cultures, and 27% (95% CI 17–39%) using a combination of blood and stool cultures (Fig. 11).
Figure 11.
Prevalence of typhoidal/NTS infection among patients with malaria detected using diagnostic tests for Salmonella spp. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval.
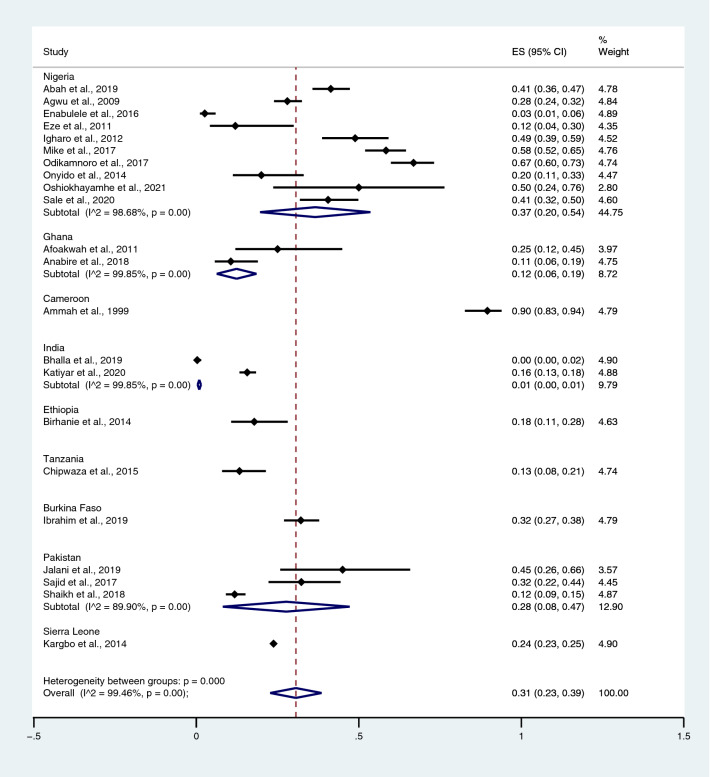
Among the studies using the Widal test for the identification of Salmonella spp. infections, the highest prevalence rate of typhoidal/NTS among patients with malaria was reported in Cameroon (90%; 95% CI 83–94%) and Nigeria (37%; 95% CI 20–54%; I2, 98.7%), whereas lower prevalence rates were reported in Burkina Faso (32%; 95% CI 27–38%), Pakistan (28%; 95% CI 8–47%; I2, 89.9%), Sierra Leone (24%; 95% CI 23–25%), Ethiopia (18%; 95% CI 11–28%), Tanzania (13%; 95% CI 8–21%), Ghana (12%; 95% CI 6–19%; I2, 99.9%), and India (1%; 95% CI 0–1%) (Fig. 12). Among the studies using hemoculture for the identification of Salmonella spp. infections, the highest prevalence rate of typhoidal/NTS among patients with malaria was reported in Nigeria (8%; 95% CI 4–12%; I2, 89%), whereas lower prevalence rates were reported in Myanmar (6%; 95% CI 1–11%; I2, 98.4%), India (6%; 95% CI 3–10%; I2, 89.3%), Tanzania (2%; 95% CI 2–3%), Ghana (1%; 95% CI 1–2%; I2, 97.9%), Kenya (1%; 95% CI 1–1%; I2, 98.5%), and Sweden (1%; 95% CI 0–1%) (Fig. 13).
Figure 12.
Prevalence of typhoidal/NTS infection among patients with malaria using the Widal test for the identification of Salmonella spp. infection stratified by countries. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval.
Figure 13.
Prevalence of typhoidal/NTS infection among patients with malaria detected using blood cultures for the identification of Salmonella spp. infection stratified by countries. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval.
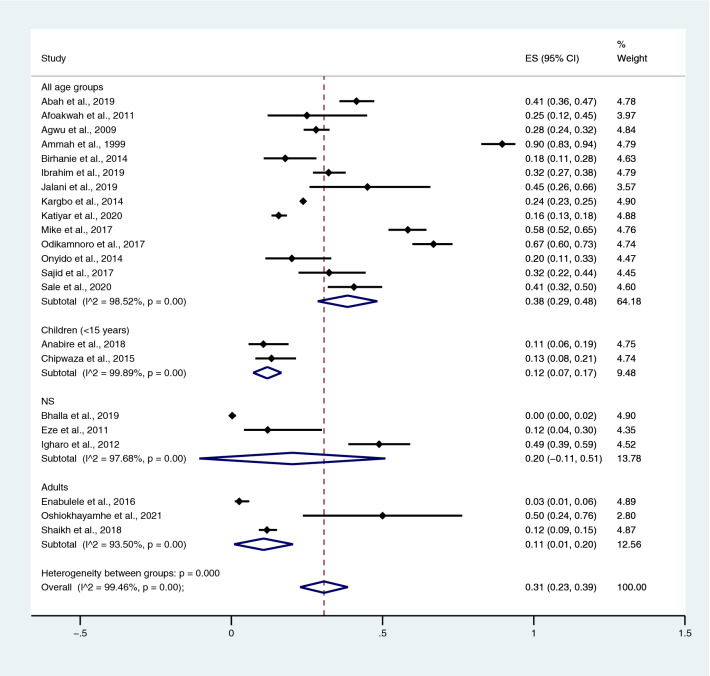
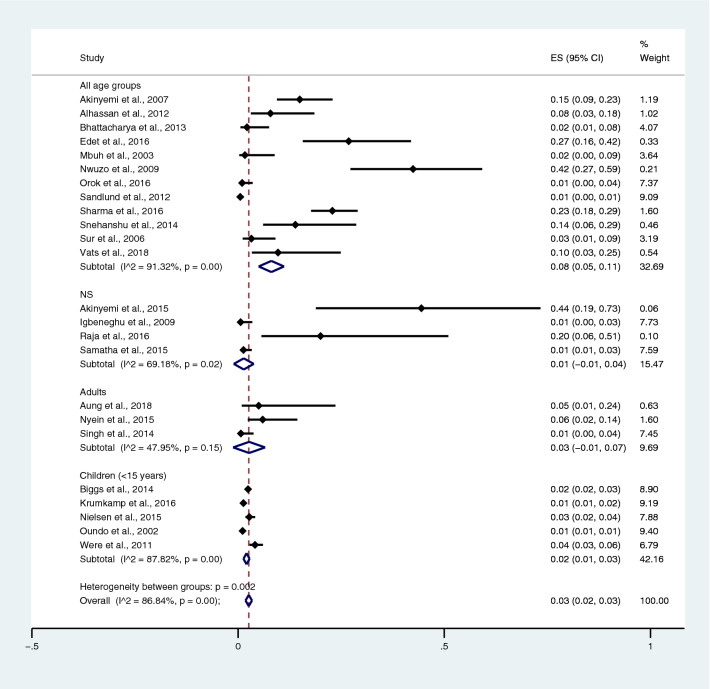
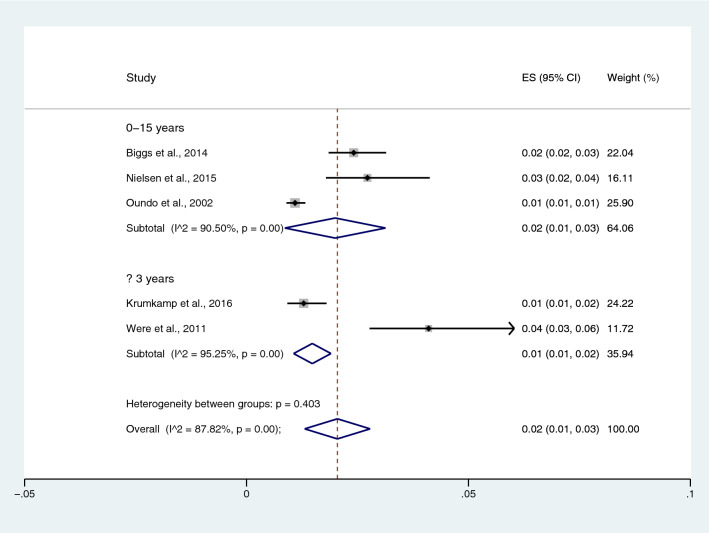
Among the studies using the Widal test for the identification of Salmonella spp. infections, the prevalence rates of typhoidal/NTS among patients with malaria in all age groups were 38% (95% CI 29–48%; I2, 98.5%), 12% in children (95% CI 7–17%; I2, 99.9%), 20% in the NS age group (95% CI − 11 to 51%; I2, 97.7%), and 11% in adults (95% CI 1–20%; I2, 93.5%) (Fig. 14). Among the studies using blood culture for the identification of Salmonella spp. infections, the prevalence rates of typhoidal/NTS among malarial patients were 8% in all age groups (95% CI 5–11%; I2, 91.3%), 1% in the NS age group (95% CI − 1 to − 4%; I2, 69.2%), 3% in adults (95% CI − 1 to 7%; I2, 48%), and 2% in children (95% CI 1–3%; I2, 87.8%) (Fig. 15). Subgroup analysis of age (≤ 3 years and 0–15 years) of NTS infection among patients with malaria was performed using the data of five studies28,44,53,56,60. Results showed that the prevalence rates of NTS infection among patients with malaria were 2% in patients aged 0–15 years (95% CI − 1 to − 43%; I2, 90.5%) and 1% in patients aged ≤ 3 years (95% CI 1–2%; I2, 95.3%) (Fig. 16).
Figure 14.
Prevalence of typhoidal/NTS infection among patients with malaria using the Widal test for the identification of Salmonella spp. infection stratified by age groups. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval, NS not specified.
Figure 15.
Prevalence of typhoidal/NTS infection among patients with malaria using blood cultures for the identification of Salmonella spp. infection stratified by age groups. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval, NS not specified.
Figure 16.
Prevalence of NTS infection among patients with malaria using blood cultures for the identification of Salmonella spp. infection stratified by age groups. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval, NS not specified.
Subgroup analysis of typhoidal/NTS, regions (Africa and Asia), and time (publication year) was performed using the data from studies using blood culture for typhoidal/NTS identification28,37,38,44,50,53,56–58,60,66,68,69,71,77,78,81,83,89,98,104–106,108. Results showed that the prevalence rates of typhoidal and NTS infection among patients with malaria were 6% (95% CI 3–8%; I2, 86.9%) and 2% (95% CI 1–2%; I2, 87.7%) (Fig. 17). Subgroup analysis of regions showed that the prevalence rates of typhoidal/NTS among patients with malaria were 2% in Afica (95% CI 1–3%; I2, 87.5%), 6% in Asia (95% CI 3–9%; I2, 86.7%), and 1% in Europe (95% CI 0–1%) (Fig. 18). Subgroup analysis of time showed that the prevalence rate of typhoidal Salmonella infection among patients with malaria was highest (17%) in 2016 (95% CI 1–33%; I2, 95.6%), 8% in 2012 (95% CI 3–18%) and 7% in 2018 (95% CI 0–14%; I2, 98.5%). The low prevalence of typhoidal Salmonella infection infection among patients with malaria was demonstrated in 2016 (13%), 2003 (2%), 2013 (2%), and 2009 (1%) (Fig. 19). Subgroup analysis of time showed that the prevalence rates of NTS infection among patients with malaria were highest in 2011 (4%), 2015 (3%), and 2014 (2%) and low in 2014 (2%), 2002 (1%), 2012 (1%), and 2016 (1%) (Fig. 20).
Figure 17.
Prevalence of typhoidal/NTS infection among patients with malaria using blood cultures for the identification of Salmonella spp. infection stratified by typhoidal/NTS infection. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval, NS not specified.
Figure 18.
Prevalence of typhoidal/NTS infection among patients with malaria using blood cultures for the identification of Salmonella spp. infection stratified by regions. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval, NS not specified.
Figure 19.
Prevalence of Salmonella spp. infection among patients with malaria using blood cultures for the identification of Salmonella spp. infection stratified by time (publication years). ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval, NS not specified.
Figure 20.
Prevalence of NTS infection among patients with malaria using blood cultures for the identification of Salmonella spp. infection stratified by time (publication years). ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval, NS not specified.
Comparison of typhoidal/NTS infections among patients with severe and non-severe malaria
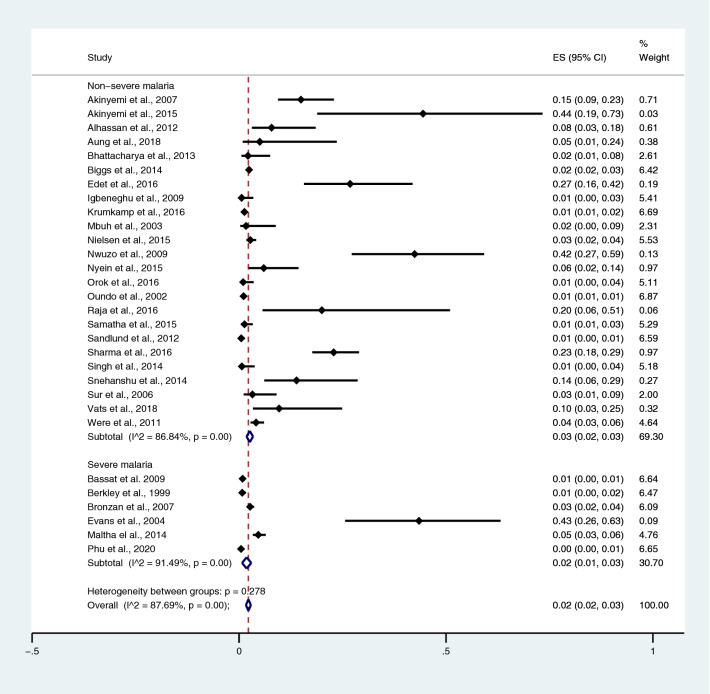
The pooled prevalence rates of typhoidal/NTS infections among patients with severe and non-severe malaria were estimated using data from 24 studies that enrolled patients with non-severe malaria28,37,38,44,50,53,56–58,60,66,68,69,71,77,78,81,83,89,98,104–106,108 and 6 studies that enrolled patients with severe malaria30,54,63,79,80,85. All 30 studies employed the blood culture method to identify Salmonella spp. infections. The pooled prevalence rates of typhoidal/NTS infection were 2% in patients with severe malaria (95% CI 1–3%; I2, 91.5%) and 3% in patients with non-severe malaria (95% CI 2–3%; I2, 86.8%) (Fig. 21).
Figure 21.
Pooled prevalence of typhoidal/NTS infection among patients with severe and non-severe malaria. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval.
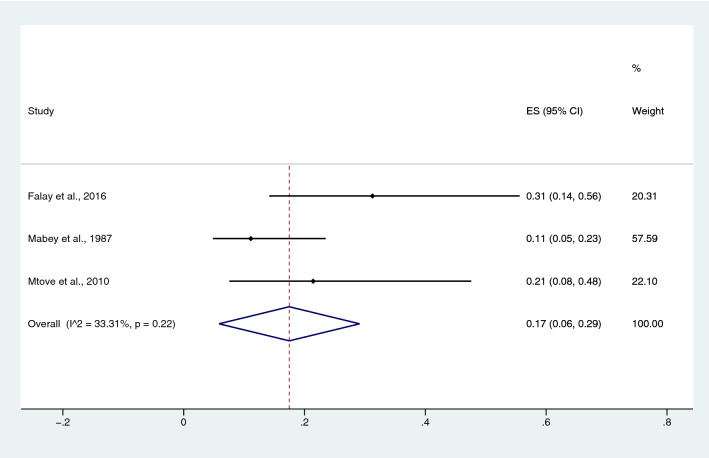
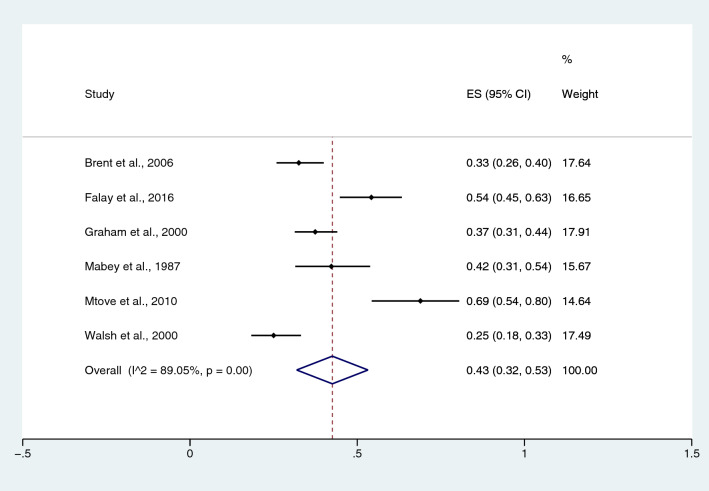
Prevalence of malaria infections among patients with typhoidal/NTS infections
The pooled prevalence rate of malaria infections among patients with typhoidal Salmonella spp. infection was estimated from three studies20,31,49. The pooled prevalence rate of malaria infection in patients with typhoidal Salmonella spp. was 17% in children (95% CI 6–29%; I2, 33.3%) (Fig. 22). The pooled prevalence rate of malaria infection among patients with NTS, which was estimated from six studies17,20,27,29,31,49, was 43% in children (95% CI 32–53%; I2, 89.1%) (Fig. 23).
Figure 22.
Pooled prevalence of malaria infection among patients with typhoidal Salmonella spp. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval.
Figure 23.
Pooled prevalence of malaria infection among patients with NTS. ES proportion estimate (multiply 100 units for interpreted as prevalence estimate), CI confidence interval.
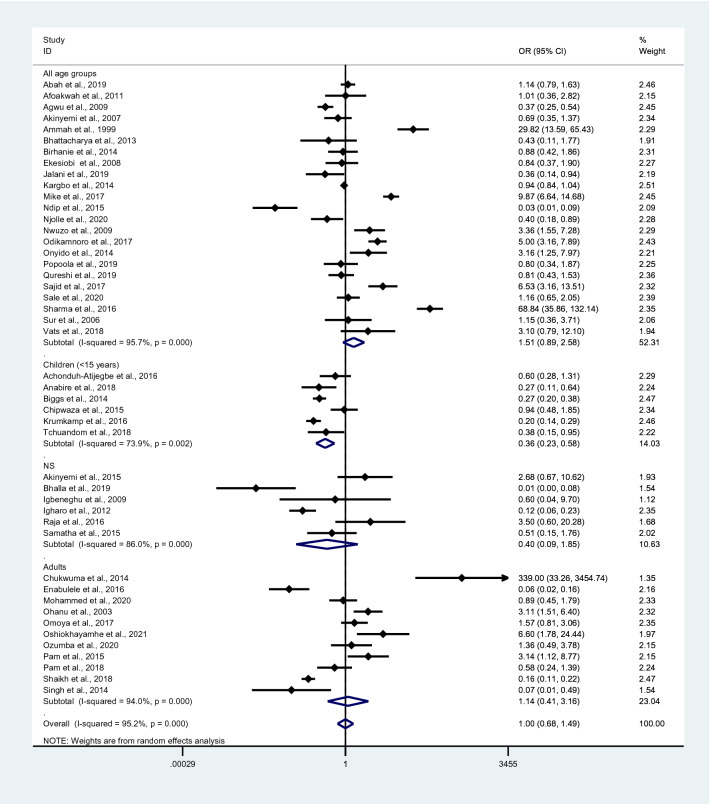
Probability of Plasmodium spp. and Salmonella spp. co-infections
The probability of Plasmodium spp. and Salmonella spp. co-infections was estimated from 46 studies35–38,40,41,43–47,50–53,57,59,61,64–66,68,70,71,73,75,76,81,82,84,87,90–93,95–97,99–104,106,108, which reported the following parameters: total number of Plasmodium spp. and Salmonella spp. co-infections, total number of malaria, total number of malaria without typhoid, and total number of febrile patients without malaria/typhoid. Plasmodium spp. and Salmonella spp. co-infections in all age groups occurred by chance (p = 0.126; odds ratio, 1.51; 95% CI 0.89–2.58; I2, 95.7%), whereas Plasmodium spp. and Salmonella spp. co-infections in children did not (p < 0.0001; odds ratio, 0.36; 95% CI 0.23–0.58; I2, 73.9%). No association between Plasmodium spp. and Salmonella spp. infections was observed in the NS age group (p, 0.24; odds ratio, 0.40; 95% CI 0.09–1.85; I2, 86%) or adults (p, 0.799; odds ratio, 1.14; 95% CI 0.41–3.16; I2, 94%). Overall, Plasmodium spp. and Salmonella spp. co-infection occurred by chance (p, 0.987; odds ratio, 1.00; 95% CI 0.68–1.49; I2, 95.2%) (Fig. 24). A significantly higher odds ratio of co-infection was reported in Nigeria57,59,82,90,95,97,101, Cameroon40, India104, and Pakistan102, whereas a significantly lower odds ratio of co-infection was found in Nigeria36,47,51, Cameroon73,92,93, Pakistan52,70, Ghana41,53, Tanzania44, Kenya60, and India43,71.
Figure 24.
Probability of Plasmodium spp. and Salmonella spp. co-infections. OR odds ratio, CI confidence interval, NS not specified.
Outcomes of malaria and typhoidal/NTS co-infections
A limited number of studies reported clinical outcomes of patients with co-infections (Table S2). Five studies60,63,79,80,92 reported outcomes of co-infection. Among those studies, three studies60,80,92 reported outcomes of malaria and NTS co-infections, and one study63 reported outcomes of malaria and typhoid co-infections. The case fatality rate in patients with malaria and NTS co-infections was 16% (95% CI 9–24%; I2, 89.1%; three studies), while one study63 reported the case fatality rate in patients with malaria and typhoidal Salmonella co-infections at 33% (95% CI 6–79%) (Supplementary Fig. S1). The difference in malarial parasitemia between co-infections and Plasmodium spp. monoinfection was estimated by two studies79,80. Results showed a higher mean of malarial parasitemia in patients with co-infections than those with Plasmodium spp. monoinfection (p, 0.023; WMD, 7926.7 parasites⁄µL of blood (95% CI 1091–14,762.3 parasites⁄µL of blood; I2, 0%, two studies) (Supplementary Fig. S2). The study by Bassat et al.79 showed a lower rate of respiratory distress in patients with co-infections (4/12, 33.3%) than those with Plasmodium spp. monoinfection (542/1328, 40.8%). The study by Bassat et al.79 also showed a lower mean hematocrit in patients with co-infections (22.1 ± 9.3%, 12 cases) than those with Plasmodium spp. monoinfection (23.4 ± 8.4%, 1328 cases).
Sensitivity test
After excluding outliers40,82,104, the probability of Plasmodium spp. and Salmonella spp. co-infection was estimated from 43 studies35–38,41,43–47,50–53,57,59,61,64–66,68,70,71,73,75,76,81,84,87,90–93,95–97,99–103,106,108. Overall, Plasmodium spp. and Salmonella spp. co-infection occurred by chance (p, 0.148; odds ratio, 0.77; 95% CI 0.54–1.10; I2, 93.6%) (Supplementary Fig. S3). However, the use of a fixed-effects model in the meta-analysis indicated that Plasmodium spp. and Salmonella spp. co-infection did not occur by chance (p < 0.0001; odds ratio, 0.82; 95% CI 0.76–0.88; I2, 93.6%) (Supplementary Fig. S4).
Publication bias
Publication bias among the 43 included studies used for determining the probability of Plasmodium spp. and Salmonella spp. co-infection was evaluated using a funnel plot and Egger’s test. The funnel plot exhibited an asymmetrical distribution of ES, and the seES was far from the middle line (no effect) (Supplementary Fig. S5). Egger’s test demonstrated no small study effect (p, 0.379; coefficient, 1.62; standard error, 1.82; t, 0.89). A contour-enhanced funnel plot analysis revealed missing studies in the significant areas (p < 0.01) (Supplementary Fig. S6), indicating that the funnel plot asymmetry was likely due to factors such as heterogeneity, selection bias, and quality of the included studies rather than publication bias.
Discussion
The present meta-analysis revealed a high prevalence of malaria and typhoidal/NTS co-infections among febrile patients detected using the Widal test (14%) and a low prevalence of malaria and typhoidal/NTS co-infections among febrile patients detected using blood cultures (1%). Moreover, the meta-analysis demonstrated that the prevalence of typhoidal/NTS infection among patients with malaria using the Widal test was high (31%), whereas the prevalence of typhoid/non-typhoid using blood culture was low (3%). A high prevalence of malaria infections among patients with typhoidal Salmonella spp. infections (17%) and NTS (43%) was also detected. The highest prevalence of co-infections detected using the Widal test was observed in Cameroon40, followed by Nigeria36,51,59,75,90,103 and Sierra Leone87, compared with Ghana, India, Ethiopia, Tanzania, and Pakistan. In using blood cultures, the gold standard method for the identification of Salmonella spp., the results indicated that the highest prevalence of co-infection was reported in Nigeria37,57,83 compared with India, Tanzania, Ghana, and Kenya. Based on these results, typhoid/non-typhoid and malaria co-infection among febrile patients frequently occurred in Nigeria. In 2020, Nigeria accounted for the most malaria cases (27%) and malaria-related deaths (23%) worldwide1. Moreover, typhoid fever is a major disease in Nigeria due to increased urbanization, insufficient water supply, movement of immigrant workers, poor processing of human waste, and overuse of antibiotics109. Due to the co-endemicity of these two pathogens, the possibility of co-infection might increase in this country.
Using the data from studies perfoming blood culture to identify typhoidal/NTS infection, the subgroup analysis of typhoidal/NTS infection demonstrated low prevalence of malaria and typhoid co-infections among febrile patients (1%) and low prevalence of typhoid among patients with malaria (6%). Moreover, the low prevalence of malaria and NTS co-infections among febrile patients (1%) and NTS infection among patients with malaria (2%) was observed. The highest prevalence of malaria and typhoid co-infections among febrile patients was reported in Nigeria, suggesting that malaria and typhoid are indeed halo-endemic in this area83. In the meta-analysis of typhoid among patients with malaria, the highest prevalence of typhoid among patients with malaria was noted in Nigeria38,57. These results suggested an increasing episode of persistent fever among patients with S. typhi and P. falciparum infections in Nigeria. For NTS infection among patients with malaria, the prevalence was higest in Kenya, and NTS infection was the most common bacteremia in children with malaria28. The high rate of bacteremia in patients with malaria in Nigeria might be due to the high prevalence of NTS infections and malnutrition28.
Using the data from studies performing blood culture to identify typhoidal/NTS infection, the subgroup analysis of regions demonstrated that the prevalence of malaria and typhoidal/NTS co-infections were 1% in both Africa and Asia. However, the prevalence of typhoidal/NTS among patients with malaria was higher in Asia (6%) than those of Africa (2%). The difference in the prevalence of typhoidal/NTS co-infections between two regions might be caused by the heterogeneity of the prevalence estimates between two regions or real difference caused by environmental factors. For example, studies in India suggested that malaria and typhoid are endemic because of poor hygiene and environmental factors104,108. In Africa, although the pooled prevalence of typhoidal/NTS infection among patients with malaria was lower than those in Asia; the results of individual studies were heterogenous. For example, the high prevalence of typhoidal/NTS infection among patients with malaria were reported by four studies conducted in Nigeria37,38,57,83, while a lower prevalence was reported by other studies included in the meta-analysis.
Using the data from studies performing blood culture to identify typhoidal/NTS infection, the subgroup analysis of time (year of publication) showed that the prevalence of malaria and typhoid co-infections among febrile patients, and typhoidal Salmonella infections among patients with malaria was highest in 2016, while lower prevalence was reported in before and after 2016. In 2016, three studies conducted in Nigeria and India66,83,104 reported the highest prevalence rates of typhoid among patients with malaria. The peak of typhoid among patients with malaria in 2016 was different from those of NTS infections among patients with malaria. The subgroup analysis showed that the peak prevalence rate of NTS infection among patients with malaria was highest in 2011, lower in 2012–2016, and 2001. These results indicated that the prevalence of NTS might decreased with time in 2011–2016, while the prevalence of typhoid among patients with malaria might not depend on time, which are needed to be further investigated.
Using the data from studies performing blood culture to identify typhoidal/NTS infection, the subgroup analysis of age of patients demonstrated that the prevalence rate of typhoidal/NTS infection among patients with malaria was higher in adults (3%) compared to that in children (2%). The previous study showed that peaks of NTS infection occurred in children aged < 2 years and adults aged 25–40 years110, while the lower rate of NTS infection occurred in children aged less than 12 years old, and the proportion of hospitalization was decreased with age111. These age groups were supported by the subgroup analysis of age that the prevalence of typhoidal/NTS was higher in adults than in children. Nevertheless, as the limitation of age information in studies reported typhoidal/NTS co-infections among febrile patients, the subgroups analysis of age might not represent the exact difference in the prevalence of typhoidal/NTS co-infections between adults and children.
The present meta-analysis demonstrated a wide gap in prevalence of malaria and typhoid/non-typhoid co-infections among febrile patients as measured by the Widal test and blood culture in analysis. The high rate of typhoid/non-typhoid and malaria co-infections detected using the Widal test and low rate of co-infections detected using blood cultures might be due to the lack of differentiation between Salmonella species/serotypes by the Widal test and cross-reactivity with other Enterobacteriaceae5,7. Moreover, false-positive Widal tests have been reported in patients with malaria and other infections5. The malaria Plasmodium may share similar strong immunogenic antigens with the typhoidal Salmonella (S. typhi); thus, Plasmodium infections could induce the generation of antibodies against S. typhi antigens, leading to cross-reactivity and false-positive results47. Furthermore, malaria loading strongly correlated with Salmonella antibody titers in numerous studies47. This cross-reaction of typhoidal/NTS antibodies with malarial antigen leads to overdiagnosis of typhoid fever74,112. The Widal test also generates false-negative results if patients are tested during the early phase of typhoid fever5. The high prevalence of typhoid fever may also be due to poor interpretation of the Widal test when diagnosing typhoid fever113. Nevertheless, in Africa and other territories, the Widal test is the most common diagnostic tool used for typhoid fever; owing to its low cost, ease of performance, and minimal training and equipment requirements. Of note, false-positive results of the Widal tests in febrile patients suspected of having Salmonella spp. infection may lead to incorrect treatment for malaria parasites. Thus, careful interpretation of the Widal test for the diagnoses of typhoid fever in resource-poor countries is required, as the overdiagnosis of typhoid fever can lead to unnecessary treatment of patients with antibiotics, microbial resistance, and poor outcome. The use of Widal test alone for the diagnosis of typhoid fever will cause misdiagnoses.
Using blood cultures alone to identify Salmonella spp. infection may underestimate Salmonella spp. infections, as blood culture has a lower sensitivity compared with the Widal test. Negative blood culture test results may be noted in patients with acute disease before the antibody response5. Based on the results of this study, the Widal test should not be used alone but in combination with blood/stool cultures. Therefore, a combination of the Widal test and blood and stool cultures is an excellent choice for diagnosing Salmonella spp. infection among febrile patients or patients with malaria. Although the high laboratory expenses for combination testing are difficult to overcome, the use of more than one diagnostic method to identify Salmonella spp. infections among patients with malaria is important to prevent incorrect treatment and misdiagnoses of malaria and other acute febrile illnesses. Infections caused by typhoidal Salmonella, including S. typhi and S. paratyphi, and the associated serious complications require treatment with antibiotics, including chloramphenicol, cefixime, amoxicillin, trimethoprim/sulfamethoxazole, azithromycin, aztreonam, and cefotaxime, to prevent severe illness and death3,114. NTS infections do not usually require treatment with antibiotics. However, complications, such as septicemia and meningitis, require treatment with ciprofloxacin, ceftriaxone, and ampicillin, according to the WHO3,114. Presently, antibiotic resistance of Salmonella species is an emerging threat, so reliable diagnostic test and appropriate treatments for typhoid/non-typhoid fever are important.
The present meta-analysis demonstrated that Salmonella spp. bacteremia developed in approximately 2% of patients with severe malaria. This occurrence was not much different from the Salmonella spp. bacteremia pooled prevalence of 3% in patients with non-severe malaria. Several mechanisms have been suggested to elucidate why patients with malaria may be predisposed to Salmonella spp. infection and bacteremia. First, immunosuppression occurs during malaria infection and treatment115. Second, malaria can lead to hemolysis, which may predispose patients to infection with Gram-negative bacteria, such as typhoidal Salmonella/NTS spp.69. Third, changes in iron storage metabolism from malaria-induced hemolysis cause neutrophil dysfunction and increased susceptibility116–118. Increased free iron from hemolysis may also promote the survival of Salmonella spp.19. Fourth, the sequestration of parasitized red blood cells in the intestine causes reduced blood flow in the mucosal gut barrier, which increases intestinal susceptibility to bacterial infection119,120. The high rate of NTS bacteremia is well described in patients with malaria-related severe anemia121. Severe anemia and hemolysis increase the iron level in the blood and tissues; therefore, pathogens can be actively transported, and iron acquisition is easier121. Based on our results, the increased risk of typhoidal Salmonella bacteremia in patients with severe malaria might reflect the high rate of parasite sequestration and vital organ dysfunction. Moreover, bacteremia cannot be excluded from patients with severe malaria; severe malaria is difficult to distinguish from bacterial sepsis56,85. Therefore, the WHO guidelines for malaria recommend that children with severe falciparum malaria in high-transmission areas should receive empirical broad-spectrum antibacterial therapy. However, empirical antibiotics should not be administered to adults with severe malaria unless there is clear evidence of bacterial infection122. In the low-transmission areas, WHO suggests that physicians should determine whether patients should receive antibiotics depending on the patient’s condition or parasitemia levels, but patients with severe malaria should not be routinely treated with antibiotics122,123. In addition to the WHO guidelines, two studies conducted in Myanmar58,78 stated that “clinicians should have a lower threshold for commencing empirical antibacterial therapy in adults diagnosed with falciparum malaria in these locations than is presently recommended.”
The present meta-analysis revealed that typhoidal/NTS and malaria co-infection occurred by chance when the random-effects model was employed to combine the effect estimates. However, the subgroup analysis demonstrated a decreased odds ratio of co-infection in children aged < 15 years, indicating that the current malaria infection was negatively associated with typhoidal/non-typhoidal Salmonella spp. infection in children35,41,44,46,53,73. Although the meta-analysis did not provide a significant outcome, individual studies demonstrated significantly higher odds ratios of co-infection in Nigeria57,59,82,90,95,97,101, Cameroon40, India104, and Pakistan102 and significantly lower odds ratio of co-infection in Nigeria36,47,51, Cameroon73,92,93, Pakistan52,70, Ghana41,53, Tanzania44, Kenya60, and India43,71. Based on these results, the probability of co-infection varies. The fixed-effects model indicated that typhoid/non-typhoid and malaria co-infection did not occur by chance or that there was an association between typhoid/non-typhoid and malaria co-infection in some way. Further studies are required to investigate this association.
The present meta-analysis of case fatality rate of patients with co-infection demonstrated the high rate of mortality (16%) without heterogeneity among the three included studies60,80,92. These three studies enrolled patients with severe malaria and co-infected with NTS and indicated that both diseases facilitate the higher fatality rate than those of the malaria or NTS infection alone. Moreover, the meta-analysis of two studies79,80 showed a higher mean parasitemia level in patients with malaria and co-infected with NTS compared to those with malaria alone (without heterogeneity, 0%), but it is important to note the limitation in the number of included studies in the analysis. Therefore, there is a need to investigate if co-infection of malaria and NTS leads to poor outcome or demonstrated the association of both diseases.
This study had several limitations. First, most included studies were cross-sectional studies that determined the prevalence of typhoidal/non-typhoidal Salmonella spp. and malaria co-infection. Therefore, data were not available to determine the differences between co-infected patients and mono-infected patients. Second, the number of studies evaluating the occurrence of Salmonella spp. bacteremia in patients with severe malaria was limited; therefore, the pooled prevalence of Salmonella spp. bacteremia in patients with severe malaria might not represent all patients with severe malaria. Third, the heterogeneity among the included studies used to determine the probability of typhoidal/non-typhoidal Salmonella spp. and malaria co-infection was high; therefore, the association between typhoidal/non-typhoidal Salmonella spp. and malaria co-infection should be carefully interpreted with the results from the sensitivity test. Compared with the previous systematic review32, the present study excluded studies with recent malaria infection; most included studies used microscopy rather than RDTs for malaria detection; and there was no publication bias among the included studies.
In conclusion, whether typhoidal/non-typhoidal Salmonella spp. and malaria co-infection occurred by chance or not, healthcare providers must provide support to patients with nonspecific clinical symptoms of malaria or typhoidal/non-typhoidal diseases. In the present study, malaria associated with typhoidal/NTS infection in children and the high case fatality rate among few co-infected patients were highlighted. Future prospective longitudinal studies using the appropriate and confirmatory diagnosis for Salmonella spp. infections are highly recommended to ensure the real prevalence of co-infection and highlight the outcome of co-infection for providing adequate treatment of co-infections in febrile patients who live in areas where malaria is endemic like tropical Africa or India.
Supplementary Information
Acknowledgements
The authors would like to thank the New Strategic Research (P2P) project, Walailak University, Thailand, for providing partial funding for this study.
Author contributions
M.K., P.W. and W.M. carried out the study design, study selection, data extraction, and statistical analysis; and drafted the manuscript. W.K.K., K.U.K. and P.R. participated in approving the manuscript. All authors read and approved the final manuscript.
Funding
This research was partially supported by the New Strategic Research (P2P) project, Walailak University, Thailand. The funders had a role in the collection, analysis, and interpretation of the data.
Data availability
All data related to the present study in this manuscript are available.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-00611-0.
References
- 1.WHO . World Malaria Report 2020. WHO; 2020. [Google Scholar]
- 2.Kuhn KG, Falkenhorst G, Ceper TH, Dalby T, Ethelberg S, Molbak K, et al. Detecting non-typhoid Salmonella in humans by ELISAs: A literature review. J. Med. Microbiol. 2012;61(Pt 1):1–7. doi: 10.1099/jmm.0.034447-0. [DOI] [PubMed] [Google Scholar]
- 3.Smith SI, Seriki A, Ajayi A. Typhoidal and non-typhoidal Salmonella infections in Africa. Eur. J. Clin. Microbiol. Infect. Dis. 2016;35(12):1913–1922. doi: 10.1007/s10096-016-2760-3. [DOI] [PubMed] [Google Scholar]
- 4.Buckle GC, Walker CL, Black RE. Typhoid fever and paratyphoid fever: Systematic review to estimate global morbidity and mortality for 2010. J. Glob. Health. 2012;2(1):010401. doi: 10.7189/jogh.01.010401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deksissa T, Gebremedhin EZ. A cross-sectional study of enteric fever among febrile patients at Ambo hospital: Prevalence, risk factors, comparison of Widal test and stool culture and antimicrobials susceptibility pattern of isolates. BMC Infect. Dis. 2019;19(1):288. doi: 10.1186/s12879-019-3917-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Azmatullah A, Qamar FN, Thaver D, Zaidi AK, Bhutta ZA. Systematic review of the global epidemiology, clinical and laboratory profile of enteric fever. J. Glob. Health. 2015;5(2):020407. doi: 10.7189/jogh.05.020407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gut AM, Vasiljevic T, Yeager T, Donkor ON. Salmonella infection—Prevention and treatment by antibiotics and probiotic yeasts: A review. Microbiology (Reading) 2018;164(11):1327–1344. doi: 10.1099/mic.0.000709. [DOI] [PubMed] [Google Scholar]
- 8.Andino A, Hanning I. Salmonella enterica: Survival, colonization, and virulence differences among serovars. Sci. World J. 2015;2015:520179. doi: 10.1155/2015/520179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andrews JR, Ryan ET. Diagnostics for invasive Salmonella infections: Current challenges and future directions. Vaccine. 2015;33(Suppl 3):C8–C15. doi: 10.1016/j.vaccine.2015.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sanchez-Vargas FM, Abu-El-Haija MA, Gomez-Duarte OG. Salmonella infections: An update on epidemiology, management, and prevention. Travel Med. Infect. Dis. 2011;9(6):263–277. doi: 10.1016/j.tmaid.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 11.Ford L, Glass K, Veitch M, Wardell R, Polkinghorne B, Dobbins T, et al. Increasing incidence of Salmonella in Australia, 2000–2013. PLoS ONE. 2016;11(10):e0163989. doi: 10.1371/journal.pone.0163989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crump JA, Sjolund-Karlsson M, Gordon MA, Parry CM. Epidemiology, clinical presentation, laboratory diagnosis, antimicrobial resistance, and antimicrobial management of invasive salmonella infections. Clin. Microbiol. Rev. 2015;28(4):901–937. doi: 10.1128/CMR.00002-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bula-Rudas FJ, Rathore MH, Maraqa NF. Salmonella infections in childhood. Adv. Pediatr. 2015;62(1):29–58. doi: 10.1016/j.yapd.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 14.Barrett FC, Knudsen JD, Johansen IS. Cases of typhoid fever in Copenhagen region: A retrospective study of presentation and relapse. BMC Res Notes. 2013;6:315. doi: 10.1186/1756-0500-6-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bennett SD, Lowther SA, Chingoli F, Chilima B, Kabuluzi S, Ayers TL, et al. Assessment of water, sanitation and hygiene interventions in response to an outbreak of typhoid fever in Neno District, Malawi. PLoS ONE. 2018;13(2):e0193348. doi: 10.1371/journal.pone.0193348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brockett S, Wolfe MK, Hamot A, Appiah GD, Mintz ED, Lantagne D. Associations among water, sanitation, and hygiene, and food exposures and typhoid fever in case-control studies: A systematic review and meta-analysis. Am. J. Trop. Med. Hyg. 2020;103(3):1020–1031. doi: 10.4269/ajtmh.19-0479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Graham SM, Walsh AL, Molyneux EM, Phiri AJ, Molyneux ME. Clinical presentation of non-typhoidal Salmonella bacteraemia in Malawian children. Trans. R. Soc. Trop. Med. Hyg. 2000;94(3):310–314. doi: 10.1016/S0035-9203(00)90337-7. [DOI] [PubMed] [Google Scholar]
- 18.Mweu E, English M. Typhoid fever in children in Africa. Trop. Med. Int. Health. 2008;13(4):532–540. doi: 10.1111/j.1365-3156.2008.02031.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morpeth SC, Ramadhani HO, Crump JA. Invasive non-Typhi Salmonella disease in Africa. Clin. Infect. Dis. 2009;49(4):606–611. doi: 10.1086/603553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mtove G, Amos B, von Seidlein L, Hendriksen I, Mwambuli A, Kimera J, et al. Invasive salmonellosis among children admitted to a rural Tanzanian hospital and a comparison with previous studies. PLoS ONE. 2010;5(2):e9244. doi: 10.1371/journal.pone.0009244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Siba V, Horwood PF, Vanuga K, Wapling J, Sehuko R, Siba PM, et al. Evaluation of serological diagnostic tests for typhoid fever in Papua New Guinea using a composite reference standard. Clin. Vaccine Immunol. 2012;19(11):1833–1837. doi: 10.1128/CVI.00380-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kumar P, Kumar R. Enteric fever. Indian J. Pediatr. 2017;84(3):227–230. doi: 10.1007/s12098-016-2246-4. [DOI] [PubMed] [Google Scholar]
- 23.Wain J, Pham VB, Ha V, Nguyen NM, To SD, Walsh AL, et al. Quantitation of bacteria in bone marrow from patients with typhoid fever: Relationship between counts and clinical features. J. Clin. Microbiol. 2001;39(4):1571–1576. doi: 10.1128/JCM.39.4.1571-1576.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wain J, Diep TS, Bay PV, Walsh AL, Vinh H, Duong NM, et al. Specimens and culture media for the laboratory diagnosis of typhoid fever. J. Infect. Dev. Ctries. 2008;2(6):469–474. doi: 10.3855/jidc.164. [DOI] [PubMed] [Google Scholar]
- 25.Beyene G, Asrat D, Mengistu Y, Aseffa A, Wain J. Typhoid fever in ethiopia. J. Infect. Dev. Ctries. 2008;2(6):448–453. doi: 10.3855/jidc.160. [DOI] [PubMed] [Google Scholar]
- 26.Prabagaran SR, Kalaiselvi V, Chandramouleeswaran N, Deepthi KNG, Brahmadathan KN, Mani M. Molecular diagnosis of Salmonella typhi and its virulence in suspected typhoid blood samples through nested multiplex PCR. J. Microbiol. Methods. 2017;139:150–154. doi: 10.1016/j.mimet.2017.05.013. [DOI] [PubMed] [Google Scholar]
- 27.Walsh AL, Phiri AJ, Graham SM, Molyneux EM, Molyneux ME. Bacteremia in febrile Malawian children: Clinical and microbiologic features. Pediatr. Infect. Dis. J. 2000;19(4):312–318. doi: 10.1097/00006454-200004000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Were T, Davenport GC, Hittner JB, Ouma C, Vulule JM, Ong'echa JM, et al. Bacteremia in Kenyan children presenting with malaria. J. Clin. Microbiol. 2011;49(2):671–676. doi: 10.1128/JCM.01864-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brent AJ, Oundo JO, Mwangi I, Ochola L, Lowe B, Berkley JA. Salmonella bacteremia in Kenyan children. Pediatr. Infect. Dis. J. 2006;25(3):230–236. doi: 10.1097/01.inf.0000202066.02212.ff. [DOI] [PubMed] [Google Scholar]
- 30.Bronzan RN, Taylor TE, Mwenechanya J, Tembo M, Kayira K, Bwanaisa L, et al. Bacteremia in Malawian children with severe malaria: Prevalence, etiology, HIV coinfection, and outcome. J. Infect. Dis. 2007;195(6):895–904. doi: 10.1086/511437. [DOI] [PubMed] [Google Scholar]
- 31.Mabey DC, Brown A, Greenwood BM. Plasmodium falciparum malaria and Salmonella infections in Gambian children. J. Infect. Dis. 1987;155(6):1319–1321. doi: 10.1093/infdis/155.6.1319. [DOI] [PubMed] [Google Scholar]
- 32.Church J, Maitland K. Invasive bacterial co-infection in African children with Plasmodium falciparum malaria: A systematic review. BMC Med. 2014;12:31. doi: 10.1186/1741-7015-12-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moola SMZ, Tufanaru C, Aromataris E, Sears K, Sfetcu R, Currie M, Qureshi R, Mattis P, Lisy K, Mu P-F. Chapter 7: Systematic Reviews of Etiology and Risk. JBI; 2020. [Google Scholar]
- 35.Achonduh-Atijegbe OA, Mfuh KO, Mbange AH, Chedjou JP, Taylor DW, Nerurkar VR, et al. Prevalence of malaria, typhoid, toxoplasmosis and rubella among febrile children in Cameroon. BMC Infect. Dis. 2016;16(1):658. doi: 10.1186/s12879-016-1996-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Agwu E, Ihongbe JC, Okogun GR, Inyang NJ. High incidence of co-infection with Malaria and Typhoid in febrile HIV infected and AIDS patients in Ekpoma, Edo State, Nigeria. Braz. J. Microbiol. 2009;40(2):329–332. doi: 10.1590/S1517-83822009000200022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Akinyemi KO, Bamiro BS, Coker AO. Salmonellosis in Lagos, Nigeria: Incidence of Plasmodium falciparum-associated co-infection, patterns of antimicrobial resistance, and emergence of reduced susceptibility to fluoroquinolones. J. Health Popul. Nutr. 2007;25(3):351–358. [PMC free article] [PubMed] [Google Scholar]
- 38.Akinyemi KO, Iwalokun BA, Alafe OO, Mudashiru SA, Fakorede C. bla CTX-M-I group extended spectrum beta lactamase-producing Salmonella typhi from hospitalized patients in Lagos. Nigeria. Infect. Drug Resist. 2015;8:99–106. doi: 10.2147/IDR.S78876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ali MA, James OC, Mohamed AA, Joachim A, Mubi M, Omodior O. Etiologic agents of fever of unknown origin among patients attending Mnazi Mmoja Hospital, Zanzibar. J. Community Health. 2020;45(5):1073–1080. doi: 10.1007/s10900-020-00832-w. [DOI] [PubMed] [Google Scholar]
- 40.Ammah A, Nkuo-Akenji T, Ndip R, Deas JE. An update on concurrent malaria and typhoid fever in Cameroon. Trans. R. Soc. Trop. Med. Hyg. 1999;93(2):127–129. doi: 10.1016/S0035-9203(99)90282-1. [DOI] [PubMed] [Google Scholar]
- 41.Anabire NG, Aryee PA, Addo F, Anaba F, Kanwugu ON, Ankrah J, et al. Evaluation of hematological indices of childhood illnesses in Tamale Metropolis of Ghana. J. Clin. Lab. Anal. 2018;32(8):e22582. doi: 10.1002/jcla.22582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anjorin AA, Nwammadu JE. Seroepidemiology of seasonal influenza virus among unvaccinated pregnant women in Lagos, Nigeria. Infez. Med. 2020;28(3):407–415. [PubMed] [Google Scholar]
- 43.Bhalla K, Rao P, Manipura R. A clinico-epidemiological analysis of seropositive cases of tropical infections and their co-infection in tertiary care hospital in South India. Indian J. Public Health Res. Dev. 2019;10(10):74–79. doi: 10.5958/0976-5506.2019.02771.2. [DOI] [Google Scholar]
- 44.Biggs HM, Lester R, Nadjm B, Mtove G, Todd JE, Kinabo GD, et al. Invasive Salmonella infections in areas of high and low malaria transmission intensity in Tanzania. Clin. Infect. Dis. 2014;58(5):638–647. doi: 10.1093/cid/cit798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Birhanie M, Tessema B, Ferede G, Endris M, Enawgaw B. Malaria, typhoid fever, and their coinfection among febrile patients at a rural health center in Northwest Ethiopia: A cross-sectional study. Adv. Med. 2014;2014:531074. doi: 10.1155/2014/531074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chipwaza B, Mhamphi GG, Ngatunga SD, Selemani M, Amuri M, Mugasa JP, et al. Prevalence of bacterial febrile illnesses in children in Kilosa district, Tanzania. PLoS Negl. Trop. Dis. 2015;9(5):e0003750. doi: 10.1371/journal.pntd.0003750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Enabulele O, Awunor SN. Typhoid fever in a Tertiary Hospital in Nigeria: Another look at the Widal agglutination test as a preferred option for diagnosis. Niger. Med. J. 2016;57(3):145–149. doi: 10.4103/0300-1652.184057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Eze EA, Ukwah BN, Okafor PC, Ugwu KO. Prevalence of malaria and typhoid co-infections in University of Nigeria, Nsukka District of Enugu State. Nigeria. Afr. J. Biotechnol. 2011;10(11):2135–2143. [Google Scholar]
- 49.Falay D, Kuijpers LMF, Phoba MF, De Boeck H, Lunguya O, Vakaniaki E, et al. Microbiological, clinical and molecular findings of non-typhoidal Salmonella bloodstream infections associated with malaria, Oriental Province, Democratic Republic of the Congo. BMC Infect. Dis. 2016 doi: 10.1186/s12879-016-1604-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Igbeneghu C, Olisekodiaka MJ, Onuegbu JA. Malaria and typhoid fever among adult patients presenting with fever in Ibadan, southwest Nigeria. Int. J. Trop. Med. 2009;4(3):112–115. [Google Scholar]
- 51.Igharo EA, Osazuwa F, Ajayi SA, Ebueku A, Igbinigie O. Dual infection with typhoid and malaria in febrile patients in Ikare Akoko, Nigeria. Int. J. Trop. Med. 2012;7(1):49–52. doi: 10.3923/ijtmed.2012.49.52. [DOI] [Google Scholar]
- 52.Jalani HA, Shah SMA, Anjum F, Khan SG, Akhter N, Khan M, et al. Prevalence and co-infection of Malaria and Typhoid in the local population of Faisalabad, Pakistan. Pak. J. Pharm. Sci. 2019;32(1):323–326. [PubMed] [Google Scholar]
- 53.Krumkamp R, Kreuels B, Sarpong N, Boahen KG, Foli G, Hogan B, et al. Association between malaria and invasive nontyphoidal Salmonella infection in a hospital study: Accounting for Berkson's bias. Clin. Infect. Dis. 2016;62(Suppl 1):S83–S89. doi: 10.1093/cid/civ950. [DOI] [PubMed] [Google Scholar]
- 54.Maltha J, Guiraud I, Kaboré B, Lompo P, Ley B, Bottieau E, et al. Frequency of severe malaria and invasive bacterial infections among children admitted to a rural hospital in Burkina Faso. PLoS ONE. 2014;9(2):e89103. doi: 10.1371/journal.pone.0089103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mourembou G, Nzondo SM, Ndjoyi-Mbiguino A, Lekana-Douki JB, Kouna LC, Matsiegui PB, et al. Co-circulation of Plasmodium and bacterial DNAs in blood of febrile and afebrile children from urban and rural areas in Gabon. Am. J. Trop. Med. Hyg. 2016;95(1):123–132. doi: 10.4269/ajtmh.15-0751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nielsen MV, Amemasor S, Agyekum A, Loag W, Marks F, Sarpong N, et al. Clinical indicators for bacterial co-infection in Ghanaian children with P. falciparum infection. PLoS ONE. 2015;10(4):e0122139. doi: 10.1371/journal.pone.0122139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nwuzo AC, Onyeagba RA, Iroha IR, Nworie O, Oji AE. Parasitological, bacteriological, and cultural determination of prevalence of malaria parasite (Plasmodium falciparum) and typhoid fever co-infection in Abakaliki, Ebonyi State. Sci. Res. Essays. 2009;4(10):966–971. [Google Scholar]
- 58.Nyein PP, Aung NM, Kyi TT, Htet ZW, Anstey NM, Kyi MM, et al. High frequency of clinically significant bacteremia in adults hospitalized with falciparum malaria. Open Forum Infect. Dis. 2016;3(1):028. doi: 10.1093/ofid/ofw028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Odikamnoro OO, Ikeh IM, Okoh FN, Ebiriekwe SC, Nnadozie IA, Nkwuda JO, et al. Incidence of malaria/typhoid co-infection among adult population in Unwana community, Afikpo north local government area, Ebonyi State, Southeastern Nigeria. Afr. J. Infect. Dis. 2018;12(1):33–38. doi: 10.21010/ajid.v12i1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Oundo JO, Muli F, Kariuki S, Waiyaki PG, Iijima Y, Berkley J, et al. Non-typhi salmonella in children with severe malaria. E. Afr. Med. J. 2002;79(12):633–639. doi: 10.4314/eamj.v79i12.8670. [DOI] [PubMed] [Google Scholar]
- 61.Pam VA, Landan S, Adejoh VA, Pam DD, Danjuma K. Co-infection of malaria and typhoid fever among pregnant women attending antenatal clinics at general hospital, wuse, federal capital territory (FCT), Abuja, Nigeria. Niger. J. Parasitol. 2018;39(2):148–153. doi: 10.4314/njpar.v39i2.6. [DOI] [Google Scholar]
- 62.Park SE, Pak GD, Aaby P, Adu-Sarkodie Y, Ali M, Aseffa A, et al. The relationship between invasive nontyphoidal Salmonella disease, other bacterial bloodstream infections, and malaria in Sub-Saharan Africa. Clin. Infect. Dis. 2016;62(Suppl 1):S23–S31. doi: 10.1093/cid/civ893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Phu NH, Day NPJ, Tuan PQ, Mai NTH, Chau TTH, Van Chuong L, et al. Concomitant bacteremia in adults with severe falciparum malaria. Clin. Infect. Dis. 2020;71(9):E465–E470. doi: 10.1093/cid/ciaa191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Popoola O, Kehinde A, Ogunleye V, Adewusi OJ, Toy T, Mogeni OD, et al. Bacteremia among febrile patients attending selected healthcare facilities in Ibadan, Nigeria. Clin. Infect. Dis. 2019;69(Suppl 6):S466–S473. doi: 10.1093/cid/ciz516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Qureshi AW, Khan ZU, Khan L, Mansoor A, Minhas R. Prevalence of malaria, typhoid and co-infection in district dir (lower), Pakistan. Biosci. J. 2019;35(1):317–325. doi: 10.14393/BJ-v35n1a2019-42250. [DOI] [Google Scholar]
- 66.Raja JM, Mary A, Usha S. A study on dual infections in pyrexia cases. Int. J. Med. Res. Health Sci. 2016;5(8):150–155. [Google Scholar]
- 67.Ramya TG, Sunitha BR. Enteric fever cases showing concurrent seropositivity with dengue and malaria: A sero-diagnostic challenge. Microbiol. Res. 2017;8(2):4. [Google Scholar]
- 68.Samatha P, Rao KC, Sowmya BS. Malaria typhoid co-infection among febrile patients. J. Evol. Med. Dent. Sci. 2015;4(65):11322–11327. doi: 10.14260/jemds/2015/1633. [DOI] [Google Scholar]
- 69.Sandlund J, Naucler P, Dashti S, Shokri A, Eriksson S, Hjertqvist M, et al. Bacterial coinfections in travelers with malaria: Rationale for antibiotic therapy. J. Clin. Microbiol. 2013;51(1):15–21. doi: 10.1128/JCM.02149-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shaikh S, Jamali GM, Jamali AA, Tanwani BM, Malik AS, Shaikh NS. Malaria and typhoid fever: positive Widal test in malaria patients reported at tertiary care hospital. Indo Am. J. Pharm. Sci. 2018;5(12):15717–15729. [Google Scholar]
- 71.Singh R, Singh SP, Ahmad N. A study of etiological pattern in an epidemic of acute febrile illness during monsoon in a tertiary health care institute of Uttarakhand, India. J. Clin. Diagn. Res. 2014;8(6):01–03. doi: 10.7860/JCDR/2014/8965.4435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tabu C, Breiman RF, Ochieng B, Aura B, Cosmas L, Audi A, et al. Differing burden and epidemiology of non-Typhi Salmonella bacteremia in rural and urban Kenya, 2006–2009. PLoS ONE. 2012;7(2):e31237. doi: 10.1371/journal.pone.0031237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tchuandom SB, Tchouangueu TF, Antonio-Nkondjio C, Lissom A, Djang JON, Atabonkeng EP, et al. Seroprevalence of dengue virus among children presenting with febrile illness in some public health facilities in Cameroon. Pan Afr. Med. J. 2018;31:177. doi: 10.11604/pamj.2018.31.177.16390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Verma D, Kishore S, Siddique ME. Comparative evaluation of various tests for diagnosis of concurrent malaria and typhoid fever in a tertiary care hospital of northern India. J. Clin. Diagn. Res. 2014;8(5):41–44. doi: 10.7860/JCDR/2014/7745.4403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Abah AEFP. Preliminary investigation of malaria, typhoid and their coinfection among febrile subjects in Port Harcourt, Rivers State Nigeria. Eur. J. Pharm. Med. Res. 2019;6(5):626–631. [Google Scholar]
- 76.Afoakwah RAD, Boampong J, Baidoo M, Nwaefuna E, Tefe P. Typhoid malaria coinfection in Ghana. Eur. J. Exp. Biol. 2011;1(3):1–6. [Google Scholar]
- 77.Alhassan HSN, Manga S, Abdullahi K, Hamid K. Co-infection profile of Salmonella typhi and malaria parasite in Sokoto-Nigeria. Int. J. Eng. Sci. Technol. 2012;2:13–20. [Google Scholar]
- 78.Aung NM, Nyein PP, Htut TY, Htet ZW, Kyi TT, Anstey NM, et al. Antibiotic therapy in adults with malaria (ANTHEM): High rate of clinically significant bacteremia in hospitalized adults diagnosed with falciparum malaria. Am. J. Trop. Med. Hyg. 2018;99(3):688–696. doi: 10.4269/ajtmh.18-0378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bassat Q, Guinovart C, Sigauque B, Mandomando I, Aide P, Sacarlal J, et al. Severe malaria and concomitant bacteraemia in children admitted to a rural Mozambican hospital. Trop. Med. Int. Health. 2009;14(9):1011–1019. doi: 10.1111/j.1365-3156.2009.02326.x. [DOI] [PubMed] [Google Scholar]
- 80.Berkley J, Mwarumba S, Bramham K, Lowe B, Marsh K. Bacteraemia complicating severe malaria in children. Trans. R. Soc. Trop. Med. Hyg. 1999;93(3):283–286. doi: 10.1016/S0035-9203(99)90024-X. [DOI] [PubMed] [Google Scholar]
- 81.Bhattacharya SK, Sur D, Dutta S, Kanungo S, Ochiai RL, Kim DR, et al. Vivax malaria and bacteraemia: A prospective study in Kolkata, India. Malaria J. 2013;12:176. doi: 10.1186/1475-2875-12-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chukwuma OG, Taiwo SO, Adekeye BT. Prevalence of Plasmodium and Salmonella infections among pregnant women with fever, presented to three hospitals in Ogun and Lagos State, South-West Nigeria. Int. Blood Res. Rev. 2014;2(4):160–167. doi: 10.9734/IBRR/2014/8690. [DOI] [Google Scholar]
- 83.Edet UOER, Etok CA, Ukanukumo JA. Prevalence of malaria and typhoid co-infection amongst residents of Uyo, Akwa Ibom State. Nigeria. Int. J. Infect. Dis. 2016;17(1):1–6. [Google Scholar]
- 84.Ekesiobi AOIM, Njoku OO. Co-infection of malaria and typhoid fever in a tropical community. Anim. Res. Int. 2017;5:888–891. [Google Scholar]
- 85.Evans JA, Adusei A, Timmann C, May J, Mack D, Agbenyega T, et al. High mortality of infant bacteraemia clinically indistinguishable from severe malaria. QJM. 2004;97(9):591–597. doi: 10.1093/qjmed/hch093. [DOI] [PubMed] [Google Scholar]
- 86.Ibrahim SYS, Wenceslas BW, Constant S, Fabrice D, Soufiane DS, Jacques Z, Armel P, Salam OA, Sanata B. Malaria and typhoid fever coinfection in the Hospital University of Bobo-Dioulasso, Burkina Faso. J. Parasitol. Res. 2019;1(1):18–24. [Google Scholar]
- 87.Kargbo MSML, Samura SK, Meng X, Zou F. The relative prevalence of typhoid and malaria in febrile patients in Freetown, Sierra Leone. Open J. Prev. Med. 2014;4:338–346. doi: 10.4236/ojpm.2014.45041. [DOI] [Google Scholar]
- 88.Katiyar GDAA, Khan S, Chaudhary BC, Sharma M. Malaria or typhoid co-infection in a tertiary care hospital of Bareilly, Uttar Pradesh, India. Int. J. Community Med. Public Health. 2020;7(2):578–583. doi: 10.18203/2394-6040.ijcmph20200430. [DOI] [Google Scholar]
- 89.Mbuh FAGM, Ogbadu L. Rate of coinfection with malaria parasites and Salmonella typhi in Zaria, Kaduna State, Nigeria. Ann. Afr. Med. 2003;2:64–67. [Google Scholar]
- 90.Mike IML, Adamu A, Longshit SG, Garba M, Sado F, Shittu AN. Prevalence of malaria and typhoid co-infections among patients who attended State Specialist Hospital Gombe from May to August 2015 for malaria and Widal tests. Greener J. Epidemiol. Public Health. 2017;5(5):37–43. doi: 10.15580/GJEPH.2017.5.080817103. [DOI] [Google Scholar]
- 91.Mohammed HIMI, Sadiq HA. Malaria and typhoid fever: Prevalence, co-infection and socio-demographic determinants among pregnant women attending antenatal care at a primary healthcare facility in Central Nigeria. Int. J. Pathog. Res. 2020;5(4):17–24. doi: 10.9734/ijpr/2020/v5i430140. [DOI] [Google Scholar]
- 92.Ndip LMEF, Kimbi HK, Njom HA, Ndip RN. Co-infection of malaria and typhoid fever in feverish patients in the Kumba Health District, Southwest Cameroon: Public health implications. Int J. Trop. Dis. Health. 2015;9(4):1–11. doi: 10.9734/IJTDH/2015/18935. [DOI] [Google Scholar]
- 93.Njolle ABTB, Asaah S, Forfuet DF, Kamga HLF. The prevalence of Salmonellosis in patients with malaria attending an urban hospital in Douala, Littoral region, Cameroon. J. Adv. Med. Med. Res. 2020;32(2):32–45. doi: 10.9734/jammr/2020/v32i230364. [DOI] [Google Scholar]
- 94.Nwabueze USCO-OA. Rate of malaria-typhoid co-infection among pregnant women attending antenatal clinics in Anambra State South-east Nigeria. Int. J. Trop. Med. Public Health. 2013;2(1):1–11. doi: 10.5455/ijtmph.44. [DOI] [Google Scholar]
- 95.Ohanu ME, Mbah AU, Okonkwo PO, Nwagbo FS. Interference by malaria in the diagnosis of typhoid using Widal test alone. W. Afr. J. Med. 2003;22(3):250–252. doi: 10.4314/wajm.v22i3.27961. [DOI] [PubMed] [Google Scholar]
- 96.Omoya FOAO. Co-infection of malaria and typhoid fever among pregnant women attending primary health care centre, Ojo Local Government, Lagos, Nigeria. Health Sci. J. 2017;11(2):495. doi: 10.21767/1791-809X.1000495. [DOI] [Google Scholar]
- 97.Onyido AEIC, Umeanaeto PU, Irikannu KC, Aribodor DN, Ezeanya LC, Ugha CN, Obiechina IO. Co-Infection of malaria and typhoid fever in Ekwulumili Community Anambra State, South-east Nigeria. N. Y. Sci. J. 2014;7(7):18–27. [Google Scholar]
- 98.Orok DUA, Ikpan O, Duke E, Eyo E, Edadi U, Ati B, Udida J. Prevalence of malaria and typhoid fever co-infection among febrile patients attending College of Health Technology Medical Centre in Calabar, Cross River State Nigeria. Niger. Int. J. Curr. Microbiol. Appl. Sci. 2016;5(4):825–835. doi: 10.20546/ijcmas.2016.504.095. [DOI] [Google Scholar]
- 99.Oshiokhayamhe IKNO, Israel IO, Agumeile K-I. Assessment of the prevalence of malaria and typhoid fever among apparently healthy undergraduates. Int. J. Med. Sci. Public Health. 2021;7(2):13–17. [Google Scholar]
- 100.Ozumba GI, Adejoh VA, Danjuma K. Co-infection of malaria and typhoid fever among pregnant women attending antenatal clinics at Dalhatu Araf Specialist Hospital Lafia, Nasarawa State, Nigeria. J. Infect. Dis. Prev. Med. 2020;8:55. [Google Scholar]
- 101.Pam VALS, Pamc DD, Gullekd JF, Okorof J, Ogbue KI, Bote CJ, Akinyerae AO. The prevalence of malaria and typhoid co-infection in pregnant women attending antenatal in Wuse general hospital Abuja, Nigeria. J. Vet. Adv. 2015;4(6):39–50. [Google Scholar]
- 102.Sajid MZM, Ahmad R, Rasool M, Shah M, Ullah I, Jawad SM. Co infection of malaria and typhoid in district Dir (Lower) Khyber Pakhtunkhwa, Pakistan. J. Entomol. Zool. Stud. 2017;5(3):912–914. [Google Scholar]
- 103.Sale MPM, Adedeji BAM, Shehu A. Prevalence of typhoid and malaria co-infection among patients attending a public hospital in Yola, Nigeria. Int. J. Mosq. Res. 2020;7(3):42–47. [Google Scholar]
- 104.Sharma BMM, Gaind R, Pandey K. Malaria and typhoid co-infection in India: A diagnostic difficulty. J. Dent. Med. Sci. 2016;15(9):101–104. [Google Scholar]
- 105.Snehanshu SHP, Chandrim S, Parul C, Chaudhary B. Malaria and typhoid, do they coexist as an alternative diagnosis in tropics? A tertiary care hospital experience. Int. J. Curr. Microbiol. Appl. Sci. 2014;3:207–214. [Google Scholar]
- 106.Sur D, von Seidlein L, Manna B, Dutta S, Deb AK, Sarkar BL, et al. The malaria and typhoid fever burden in the slums of Kolkata, India: Data from a prospective community-based study. Trans. R. Soc. Trop. Med. Hyg. 2006;100(8):725–733. doi: 10.1016/j.trstmh.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 107.Ukaegbu CONA, Mawak JD, Igwe CC. Incidence of concurrent malaria and typhoid fever infection in febrile patients in Jos, Plateau State Nigeria. Int. J. Sci. Technol. Res. 2014;3(4):157–161. [Google Scholar]
- 108.Vats AD. Incidence of co-infection of malaria and typhoid and their diagnostic dilemmas. RAPL. 2018;4(4):10–12. doi: 10.24321/2454.8642.201815. [DOI] [Google Scholar]
- 109.Akinyemi KO, Oyefolu AOB, Mutiu WB, Iwalokun BA, Ayeni ES, Ajose SO, et al. Typhoid fever: Tracking the trend in Nigeria. Am. J. Trop. Med. Hyg. 2018;99:41–47. doi: 10.4269/ajtmh.18-0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gordon MA. Invasive nontyphoidal Salmonella disease: Epidemiology, pathogenesis and diagnosis. Curr. Opin. Infect. Dis. 2011;24(5):484–489. doi: 10.1097/QCO.0b013e32834a9980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Saha S, Islam MS, Sajib MSI, Saha S, Uddin MJ, Hooda Y, et al. Epidemiology of typhoid and paratyphoid: Implications for vaccine policy. Clin. Infect. Dis. 2019;68(Suppl 2):S117–S123. doi: 10.1093/cid/ciy1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sundufu AJJM, Foday IK. Role of co-infection with malaria parasites and Salmonella typhoid in Bo City, Southern Sierra Leone. Public Health Res. 2012;2(6):204–207. doi: 10.5923/j.phr.20120206.05. [DOI] [Google Scholar]
- 113.Sultana S, Hossain MA, Paul SK, Kabir MR, Yesmin T, Maruf MA, et al. Evaluation of TH agglutinin titres of Widal test in the diagnosis of typhoid fever. Mymensingh Med. J. 2014;23(1):1–6. [PubMed] [Google Scholar]
- 114.Parry CM, Hien TT, Dougan G, White NJ, Farrar JJ. Typhoid fever. N. Engl. J. Med. 2002;347(22):1770–1782. doi: 10.1056/NEJMra020201. [DOI] [PubMed] [Google Scholar]
- 115.Alemu A, Shiferaw Y, Addis Z, Mathewos B, Birhan W. Effect of malaria on HIV/AIDS transmission and progression. Parasit. Vectors. 2013;6:18. doi: 10.1186/1756-3305-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Cunnington AJ, de Souza JB, Walther M, Riley EM. Malaria impairs resistance to Salmonella through heme- and heme oxygenase-dependent dysfunctional granulocyte mobilization. Nat. Med. 2011;18(1):120–127. doi: 10.1038/nm.2601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cunnington AJ, Njie M, Correa S, Takem EN, Riley EM, Walther M. Prolonged neutrophil dysfunction after Plasmodium falciparum malaria is related to hemolysis and heme oxygenase-1 induction. J. Immunol. (Baltimore) 2012;189(11):5336–5346. doi: 10.4049/jimmunol.1201028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Roux CM, Butler BP, Chau JY, Paixao TA, Cheung KW, Santos RL, et al. Both hemolytic anemia and malaria parasite-specific factors increase susceptibility to nontyphoidal Salmonella enterica serovar typhimurium infection in mice. Infect. Immun. 2010;78(4):1520–1527. doi: 10.1128/IAI.00887-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Seydel KB, Milner DA, Jr, Kamiza SB, Molyneux ME, Taylor TE. The distribution and intensity of parasite sequestration in comatose Malawian children. J. Infect. Dis. 2006;194(2):208–215. doi: 10.1086/505078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Olsson RA, Johnston EH. Histopathologic changes and small-bowel absorption in falciparum malaria. Am. J. Trop. Med. Hyg. 1969;18(3):355–359. doi: 10.4269/ajtmh.1969.18.355. [DOI] [PubMed] [Google Scholar]
- 121.Abuga KM, Muriuki JM, Williams TN, Atkinson SH. How severe anaemia might influence the risk of invasive bacterial infections in African children. Int. J. Mol. Sci. 2020;21(18):6976. doi: 10.3390/ijms21186976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.WHO . WHO Guidelines for Malaria. WHO; 2021. [Google Scholar]
- 123.White, N. J. Reply to Aung et al. Clinical infectious diseases: An official publication of the Infectious Diseases Society of America 72(3), 536–538 (2021). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data related to the present study in this manuscript are available.