Abstract
Management of critically ill coronavirus disease 2019 (COVID-19) patients has evolved considerably during the pandemic. We investigated rates and causes of ventilator-associated events (VAEs) in COVID-19 patients in the late versus early waves in 4 Massachusetts hospitals. VAE rates per episode decreased, rates per ventilator day were stable, and most cases were caused by acute respiratory distress syndrome (ARDS).
The management of patients hospitalized with severe coronavirus disease 2019 (COVID-19) has changed considerably over the course of the pandemic.1,2 Early on, many experts advocated early intubation for hypoxemic patients rather than intubation-sparing modalities, such as high-flow nasal cannula (HFNC) and noninvasive positive pressure ventilation, for fear of generating aerosols and increasing risks for healthcare workers.3 With time, however, many institutions evolved to favor intubation-sparing modalities, reserving intubation for patients with more severe disease. Simultaneously, the use of medications associated with better outcomes, including dexamethasone, remdesivir, and tocilizumab, has increased. Little is known, however, about the impact of these changes on the incidence and precipitants of ventilator-associated events (VAEs) in patients with COVID-19. We evaluated changes in incidence rates and clinical triggers for VAE in 4 hospitals during the first COVID-19 wave versus the second COVID-19 wave in Massachusetts.
Methods
We retrospectively identified all adult patients with COVID-19 requiring mechanical ventilation (defined as spending any portion of a day on the ventilator) in 2 quaternary academic hospitals and 2 community hospitals in eastern Massachusetts during the first and second waves of the pandemic (ie, March–August 2020 and November 2020–January 2021). VAEs were identified using Centers for Disease Control and Prevention criteria applied to data extracted from participating hospitals’ electronic health record systems. Briefly, VAEs are defined by ≥2 days of sustained increases in ventilator settings (rise in daily minimum positive end expiratory pressure of ≥3 cm H2O and/or rise in the absolute fraction of inspired oxygen of ≥20%) after ≥2 days of stable or decreasing ventilator settings.4 We calculated VAE rates for each calendar month and compared incidence rates per 100 episodes of mechanical ventilation and per 1,000 ventilator days during the first wave versus the second wave using 2-sample tests of proportions.
We then compared the conditions precipitating VAEs in the first wave versus the second wave. We reviewed 100 randomly selected COVID-19 patients from the first wave and all VAEs from the second wave. We assessed whether VAE causes differed for early versus late VAEs (ie, ≤7 vs >7 days after intubation). Precipitating conditions were adapted from prior research.5 All records were reviewed by one intensivist (J.W.), and interrater reliability, which was reviewed by a second intensivist (C.R.), was high.6 Statistical analyses were performed using R version 4.0.2 software (https://www.R-project.org/, R Foundation for Statistical Computing, Vienna, Austria).
Results
The demographics and characteristics of ventilated COVID-19 patients are shown in Table 1. The first wave included 628 COVID-19 patients who underwent 661 episodes of mechanical ventilation over 11,178 ventilator days. Overall, 192 VAEs corresponded to 29.0 VAEs per 100 episodes and 17.2 per 1,000 ventilator days. During the second wave, 267 COVID-19 patients underwent 283 episodes of mechanical ventilation over 4,245 ventilator days. Also, 61 VAEs corresponded to 21.6 VAEs per 100 episodes and 14.4 per 1,000 ventilator days.
Table 1.
Demographics and Characteristics of Mechanically Ventilated COVID-19–Positive Patients With and Without a VAE during the First Versus Second Waves of the Pandemic
| Variable | COVID-19 + Requiring Mechanical Ventilation | |||
|---|---|---|---|---|
| VAE + | VAE - | |||
| First Wave (N=172) |
Second Wave (N=60) |
First Wave (N=489) |
Second Wave (N=223) |
|
| Age, mean y (SD) | 60.0 (14) | 67.3 (15) | 61.6 (16) | 64.7 (15) |
| Sex, male, no. (%) | 123 (72) | 37 (62) | 300 (61) | 149 (67) |
| Hypertension, no. (%) | 117 (68) | 42 (70) | 324 (66) | 159 (71) |
| Diabetes, no. (%) | 93 (54) | 28 (47) | 229 (47) | 98 (44) |
| Elixhauser score (mean, SD) | 5.8 (2) | 6.2 (2) | 5.3 (2) | 5.7 (2) |
| Time from admission to intubation, median d (IQR) | 0 (2) | 1 (4) | 0 (2) | 1 (4) |
| Duration of MV, median d (IQR) | 21 (19) | 17 (10) | 10 (13) | 8 (10) |
| Time from initiation of MV to VAE, median d (IQR) | 5 (9) | 8 (8) | N/A | N/A |
| In-hospital mortality, no. (%) | 52 (30) | 36 (60) | 158 (32) | 92 (41) |
| VAE rate per 100 EMV | 29.0 | 21.6 | N/A | N/A |
| VAE rate per 1000 ventilator days | 17.2 | 14.4 | N/A | N/A |
| VAE subtype, no. (%) | ||||
| VAC | 95 (55) | 31 (51) | ||
| IVAC | 53 (31) | 18 (30) | ||
| PVAP | 24 (14) | 11 (18) | ||
Note. N corresponds to the number of episodes of mechanical ventilation. IQR, interquartile range; SD, standard deviation; VAE, ventilator-associated event; MV, mechanical ventilation; EMV, episodes of mechanical ventilation; VAC, ventilator-associated complication; IVAC, infection-related ventilator-associated complication; PVAP, possible ventilator-associated pneumonia.
The VAE rate per 100 episodes of mechanical ventilation was higher during the first wave versus the second wave (29.0 vs 21.6; P = .02), but the rates per 1,000 ventilator days were similar (17.2 vs 14.4; P = .22). Percentages of noninfectious VAEs (VAC alone) and potentially infectious VAEs (IVAC plus) were also similar: VAC alone (55% first wave vs 51% second wave; P = .47) and IVAC-plus (45% in the first wave vs 49% in the second wave; P = .47).
Among COVID-19 patients with VAEs, the interval from admission to intubation was shorter during the first wave versus the second wave (median, 0 vs 1 days; P < .01), whereas the duration of mechanical ventilation was longer (median, 21 vs 17 days; P = .04). Times from initiation of mechanical ventilation to VAE were similar in both waves (median, 5 vs 8 days; P = .10). Unadjusted mortality was lower among COVID-19 patients with VAEs during the first wave versus the second wave (30% vs 60%; P < .01) and for ventilated COVID-19 patients without VAEs during the first wave versus the second wave (32% vs 41%; P = .02).
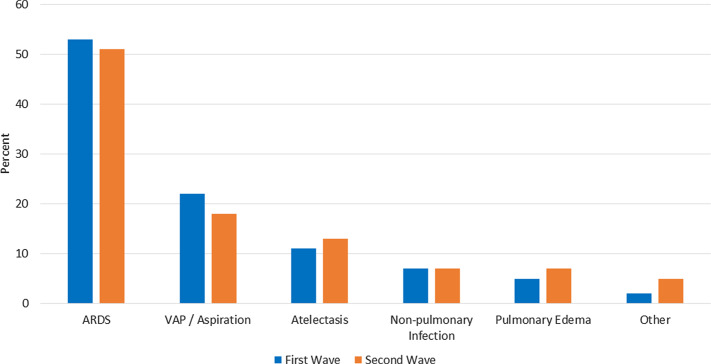
Acute respiratory distress syndrome (ARDS; 53% vs 51%) and VAP (22% vs 18%) were the most common events leading to VAE during the first wave versus the second wave (Fig. 1). More VAEs occurred during the first 7 days of intubation in the first wave versus the second wave (58% vs 40%; P =.02), but the causes of early VAEs were similar.
Fig. 1.
Clinical event leading to VAE among COVID-19 patients stratified by the first pandemic wave versus the second wave.
Discussion
We report on changes in the incidence, causes, and outcomes of VAEs in COVID-19–positive patients during the first wave versus the second wave of the pandemic. The VAE incidence per 100 episodes of mechanical ventilation decreased but the rate per 1,000 ventilator days remained stable. In-hospital mortality rates of ventilated COVID-19 patients with and without VAEs was higher in the second wave. In both waves, the rate of VAE was higher compared to prepandemic cohorts. ARDS was the most common cause of VAEs in both COVID-19 waves, whereas before the COVID-19 pandemic most were caused by pneumonia and pulmonary edema.6,7
The higher mortality rate among COVID-19 patients with VAEs during the second wave versus the first wave (60% vs 30%) may reflect the preference to defer intubation whenever possible during the second wave in favor of HFNC or noninvasive ventilation. Noninvasive ventilation and HFNC were used sparingly at our institutions and many others during the first wave for fear of aerosol generation and healthcare worker exposure, but their use rapidly expanded over time based on local experience and increasing evidence of safety and efficacy.3,8 As a result, invasive ventilation was reserved for a much sicker segment of the COVID-19 population. This finding is supported by the longer average interval between admission and intubation in the second wave versus the first wave. Likewise, progression to intubation despite the use of evidence-based therapeutics (eg, remdesivir, dexamethasone, and tocilizumab) may have further selected for severely ill patients. Notably, however, VAEs per episode of mechanical ventilation were less frequent in the second wave. This finding may reflect changes in ventilation strategies and the increased use of anti-inflammatory medications mitigating the risk of progressive ARDS triggering VAEs.
The causes of VAEs among COVID-19–positive patients were similar between the first wave and the second wave, and progressive ARDS was the most common trigger in both waves. Fewer VAEs occurred within 7 days of intubation during the second wave. This finding may also be attributable to advances in therapeutics or increasing resumption of VAE prevention best practices such as minimizing sedation, low-tidal-volume ventilation, conservative transfusion thresholds, and mobilizing patients.7 Improved therapeutics may forestall or blunt the severity of ARDS and thus precipitate fewer ARDS-related VAEs.9,10
This study had several limitations. We focused on 4 hospitals in eastern Massachusetts alone, potentially limiting generalizability. However, many of the therapeutics and practice changes that occurred in these hospitals were widespread. We identified a primary clinical event leading to VAE in each case via manual chart review but may have missed additional complications (eg, pulmonary embolisms, which are common in severe COVID-19) if they were undiagnosed by medical teams. Our analysis did not provide insight into which specific clinical factors most affected changes in VAE epidemiology nor did it include granular data on severity-of-illness, whether it has changed over time, or its association with VAE risk. These are important topics for future research.
In conclusion, VAE rates per 100 episodes of mechanical ventilation decreased among COVID-19 patients over the first 2 waves of the pandemic, whereas rates per 1,000 ventilator days remained stable. The most common cause of VAEs in both waves was progressive ARDS, in contrast to historical series where most VAEs have been caused by pneumonia and fluid overload. These observations underscore the ongoing need to optimize VAE prevention strategies with increased emphasis on minimizing and mitigating ARDS in patients with COVID-19.
Acknowledgments
The Centers for Disease Control and Prevention and National Institutes of Health had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Contributor Information
Collaborators: for the CDC Prevention Epicenters Program
Financial support
This work was funded by the Centers for Disease Control and Prevention (grant no. 6U54CK000484-04-02) and by the National Heart Lung and Blood Institute of the National Institutes of Health (grant no. T32HL007633).
Conflicts of interest
All authors report no conflicts of interest relevant to this article.
References
- 1. Anesi GL, Jablonski J, Harhay MO, et al. Characteristics, outcomes, and trends of patients with COVID-19–related critical illness at a learning health system in the United States. Ann Intern Med 2021;174:613–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kurtz P, Bastos LSL, Dantas LF, et al. Evolving changes in mortality of 13,301 critically ill adult patients with COVID-19 over 8 months. Intensive Care Med 2021;47:538–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Papoutsi E, Giannakoulis VG, Xourgia E, Routsi C, Kotanidou A, Siempos II. Effect of timing of intubation on clinical outcomes of critically ill patients with COVID-19: a systematic review and meta-analysis of non-randomized cohort studies. Crit Care 2021;25:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ventilator-associated event (VAE) device-associated module. Centers for Disease Control and Prevention website. https://www.cdc.gov/nhsn/pdfs/pscmanual/10-vae_final.pdf 2021. Published January 2021. Accessed October 26, 2021.
- 5. Kerlin MP, Trick WE, Anderson DJ, et al. Interrater reliability of surveillance for ventilator-associated events and pneumonia. Infect Control Hosp Epidemiol 2017;38:172–178. [DOI] [PubMed] [Google Scholar]
- 6. Weinberger J, Rhee C, Klompas M. Incidence, characteristics, and outcomes of ventilator-associated events during the COVID-19 pandemic. Ann Am Thorac Soc 2021. doi: 10.1513/AnnalsATS.202103-364OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cocoros NM, Klompas M. Ventilator-associated events and their prevention. Infect Dis Clin N Am 2016;30:887–908. [DOI] [PubMed] [Google Scholar]
- 8. Mellado-Artigas R, Ferreyro BL, Angriman F, et al. High-flow nasal oxygen in patients with COVID-19–associated acute respiratory failure. Crit Care 2021;25:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Investigators R-C, Gordon AC, Mouncey PR, et al. Interleukin-6 receptor antagonists in critically ill patients with COVID-19. N Engl J Med 2021;384:1491–1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tomazini BM, Maia IS, Cavalcanti AB, et al. Effect of dexamethasone on days alive and ventilator-free in patients with moderate or severe acute respiratory distress syndrome and COVID-19: the CoDEX randomized clinical trial. JAMA 2020;324:1307–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]