Guidelines recommend surveillance of nondysplastic Barrett’s esophagus (BE) every 3 to 5 years, but do not provide guidance on when to discontinue surveillance.1 There is limited understanding of practice patterns in surveillance of BE. We hypothesized that surveillance of BE persists through older age, even in individuals with substantially diminished life expectancy.
Methods
We accessed a nationwide insurance claims dataset of enrollees in Medicare with employer-sponsored supplemental insurance (MarketScan Commercial Claims and Encounters Database, Truven Health Analytics, Ann Arbor, MI). Approximately 30% of Medicare enrollees in 2010 had such supplemental insurance.2 Using Current Procedural Terminology (CPT) and International Classification of Diseases, 9th Revision, Clinical Modification (ICD9CM) codes, we identified enrollees who were aged ≥65 years and underwent an upper endoscopy (CPTs 43200, 43202, 43220, 43226, 43231, 43235, 43237, 43238, 43239, 43242, 43245, 43248, or 43249) in 2009 with a diagnosis of BE (ICD9CM 530.85) within 1 year of the endoscopy, an algorithm previously validated.3 We excluded patients whose index diagnosis was adenocarcinoma of the esophagus or gastric cardia (ICD9CMs 150.3–150.5, 150.8–151.0) and those who received endoscopic therapy at index or follow-up (CPTs 43217, 43228, 43229, 43251, 43258, or 43270) to minimize the proportion of subjects with dysplasia included in the analysis. We then assessed whether the patient had a repeat endoscopy within 5 years of the index endoscopy.
We classified the appropriateness of repeat endoscopy based on a previously validated algorithm using administrative codes at index endoscopy, follow-up endoscopy, and intervening diagnoses, modified to exclude BE from consideration in classification, and classified regardless of whether the patient actually had a repeat endoscopy.4 For instance, repeat endoscopy is likely appropriate if the patient undergoes endoscopic dilation or has cirrhosis. Repeat is possible overuse for conditions such as peptic ulcer disease or anemia without endoscopic findings. Repeat is probable overuse for symptoms without specific endoscopic findings, such as dysphagia without stenosis or dilation, or gastroesophageal reflux disease without other significant findings. We used Cox proportional hazards regression to estimate the effects of age, weighted Charlson-Deyo comorbidity scores (calculated from all encounters), sex, and geographic region on the rate of a repeat endoscopy, censoring those with loss of follow-up, and excluding those in whom a repeat endoscopy was likely appropriate. Loss of follow-up could be due to death, patient electing to drop supplemental insurance, or change in insurance provider.
Results
Inclusion criteria were met by 20,387 patients (Supplementary Figure 1). Mean age at the time of index endoscopy was 74 years, 61% were men, and median weighted Charlson-Deyo comorbidity score was 3 (interquartile range = 1, 5). A total of 3158 (15.5%) patients were classified as likely appropriate for repeat endoscopy (mainly esophageal stricture), 12,094 (59.3%) as possible overuse (mainly esophagitis), and 4879 (23.9%) as probable overuse. Patients classified as likely appropriate for repeat were more likely, and those classified as possible overuse were slightly more likely, to have repeat endoscopy than those classified as probable overuse (hazard ratio [HR] 1.43; 95% confidence interval [Cl] 1.35–1.52; and HR 1.07; 95% CI 1.02–1.12, respectively). Of those with repeat within 3 years, 19.9% were likely appropriate. Excluding those with likely appropriate indication for repeat, 51.3% had a repeat within 5 years at a median of 1.54 years, and 85.3% of those with a repeat were within 3 years.
A total of 6311 patients (31.0%) were lost to follow-up. Censoring for loss to follow-up, and excluding those likely appropriate for repeat, 85.3% of patients underwent repeat endoscopy within 5 years. Most of each age group underwent repeat endoscopy within 5 years; the least likely were those aged 90 or older, but even 55.5% of this group underwent repeat within 5 years (Figure 1). Those with short life expectancy frequently underwent repeat endoscopy. For example, 79.3% of men aged 80 to 84 with weighted Charlson-Deyo comorbidity score of 4 or greater (whose life expectancy is less than 5 years)5,6 underwent repeat endoscopy within 5 years.
Figure 1.
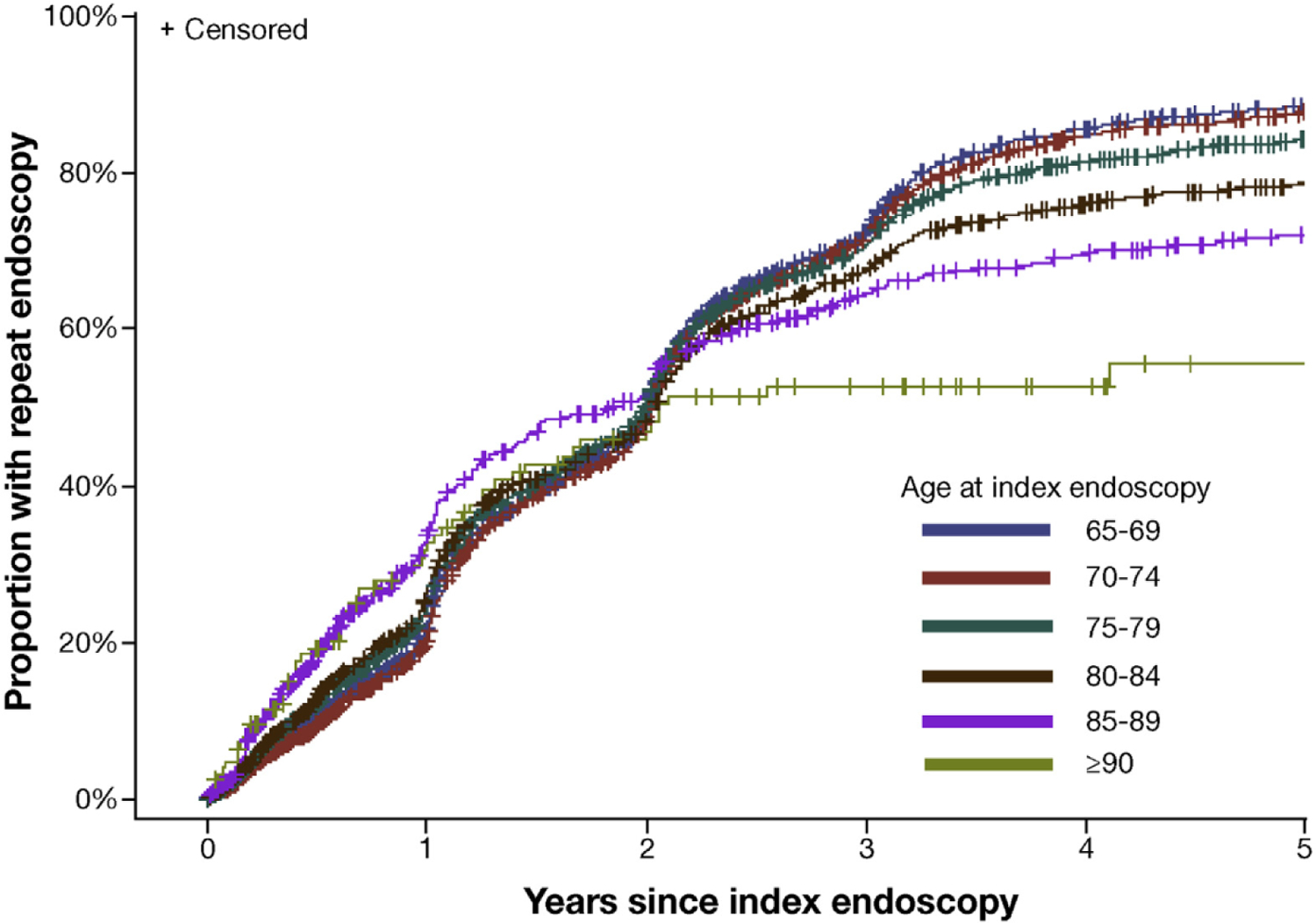
Time to repeat endoscopy stratified by age. Data censored for loss to follow-up, and excludes those with likely appropriate classification for repeat endoscopy.
In multivariable analysis, advancing age was only weakly inversely associated with the rate of repeat endoscopy until age 90, when there was a larger decrease in rate (adjusted HR vs ages 65–69: ages 85–90 = 0.818, 95% CI 0.735–0.911; age ≥ 90 = 0.610, 95% CI 0.471–0.790) (Supplementary Table 1). Comorbidity was not associated with repeat endoscopy (Supplementary Table 1).
Discussion
Guidelines recommend performing surveillance endoscopy at intervals of 3 to 5 years.1 We found that most patients who undergo surveillance endoscopy do so sooner than 3 years, even after excluding those who have a likely appropriate indication for early repeat endoscopy. BE guidelines do not specify when surveillance should be discontinued. Our data suggest that surveillance of BE is likely overused in individuals with limited life expectancy.
Our study is limited to Medicare enrollees with employer-sponsored supplemental health insurance, who are more affluent, on average, than the general population, and might differ in health status.2 However, we found that even those with severe comorbidity were no less likely to undergo repeat upper endoscopy than those with little comorbidity. A substantial proportion were censored because of loss to follow-up during the 5 years after index endoscopy. The median life expectancy of a 75-year-old man in 2009 was 11.2 years, and for a woman 13.0 years,7 so much of this loss to follow-up was likely due to death. Strengths of our study include the large population assessed across the United States, duration of follow-up, and access to comorbid conditions.
In summary, we found that upper endoscopy is frequently repeated in patients with BE sooner than recommended, and repeated even in those with limited life expectancy. Efforts are needed to encourage adherence to guidelines recommending against overly frequent surveillance of BE. In addition, research is needed to define under what conditions surveillance should be discontinued. Providers need explicit guidance regarding when to discontinue surveillance of BE and strategies for how to implement such recommendation into clinical practice.
Supplementary Material
Acknowledgments
We appreciate the constructive feedback of this manuscript by John Inadomi, Iris Lansdorp-Vogelaar, Elissa Ozanne, and Sameer Saini. We also appreciate the technical assistance of Robert Holleman.
Abbreviations used in this paper:
- BE
Barrett’s esophagus
- CI
confidence interval
- CPT
Current Procedural Terminology
- HR
hazard ratio
- ICD9CM
International Classification of Diseases, 9th Revision, Clinical Modification
Footnotes
Supplementary Material
Note: To access the supplementary material accompanying this article, visit the online version of Gastroenterology at www.gastrojournal.org, and at https://doi.org/10.1053/j.gastro.2019.10.022.
Conflicts of interest
The authors disclose no conflicts.
References
- 1.Spechler SJ, Sharma P, Souza RF, et al. American Gastroenterological Association medical position statement on the management of Barrett’s esophagus. Gastroenterology 2011;140:1084–1091. [DOI] [PubMed] [Google Scholar]
- 2.Jacobson G, Huang J, Neuman T. Medigap reform: setting the context for understanding recent proposals. The Kaiser Family Foundation, 2014. Available at: https://www.kff.org/medicare/issue-brief/medigap-reform-setting-the-context/. Accessed March 12, 2019. [Google Scholar]
- 3.Shakhatreh MH, Duan Z, Kramer J, et al. The incidence of esophageal adenocarcinoma in a national veterans cohort with Barrett’s esophagus. Am J Gastroenterol 2014;109:1862–1868; quiz 1861,1869. [DOI] [PubMed] [Google Scholar]
- 4.Rubenstein JH, Pohl H, Adams MA, et al. Overuse of repeat upper endoscopy in the Veterans Health Administration: a retrospective analysis. Am J Gastroenterol 2017;112:1678–1685. [DOI] [PubMed] [Google Scholar]
- 5.Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity index. J Clin Epidemiol 1994; 47:1245–1251. [DOI] [PubMed] [Google Scholar]
- 6.Kistler CE, Kirby KA, Lee D, et al. Long-term outcomes following positive fecal occult blood test results in older adults: benefits and burdens. Arch Intern Med 2011; 171:1344–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.US Social Security Administration Actuarial Life Table. 2019. Available at: www.ssa.gov/oact/STATS/table4c6.html. Accessed September 12, 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


