Abstract
Background
Little research has examined the relationship between non-fatal workplace injuries and illnesses and long-term mortality.
Methods
We linked non-fatal injury cases reported to the New Mexico workers’ compensation system 1994-2000 with Social Security Administration data on individual earnings and mortality through 2014. We then derived sex-specific Kaplan-Meier curves to show time to death for workers with lost-time injuries (n=36,377) and comparison workers (n=70,951). We fit multivariable Cox survival models to estimate the hazard ratio separately for male and female workers with lost-time injuries.
Results
The estimated hazard ratio for lost-time injuries is 1.24 for women and 1.21 for men. 95 percent confidence intervals were (1.15, 1.35) and (1.15, 1.27) respectively.
Conclusion
Lost-time occupational injuries are associated with a substantially elevated mortality hazard. This implies an important formerly unmeasured cost of these injuries and a further reason to focus on preventing them.
BACKGROUND
Every year millions of occupational injuries and illnesses occur in the United States. Workplace injuries and illnesses directly affect health, employment, and long-term earnings. That they affect health is virtually definitional, even though in many cases the direct health impacts may be short-lived. The impact on labor-market outcomes, including job loss, income reduction, and a decline in wealth has become well-established over the past decade [Boden and Galizzi 2003, Dong, et al. 2015, Galizzi and Zagorsky 2009, Reville, et al. 2001, Seabury, et al. 2014]. These impacts together may contribute to premature mortality, yet this potential consequence of “non-fatal” injuries has received little attention. (For simplicity, in the rest of this paper, “injuries” refers to both injuries and illnesses.) Our aim is to examine the hypothesis that workplace injuries are associated with a shortened lifespan.
One possible pathway to premature mortality is a long-term change in health status directly related to the occupational injury. A second pathway is through changes in income and employment status subsequent to injury. Reduced income has been associated with poorer health [Sullivan and von Wachter 2009]. During the past 15 years, research has demonstrated that occupational injuries can lead to substantial and long-lasting reductions in earnings and a substantial decline in wealth. As disabled workers age, the impact of these disabilities may remain or increase, leading to continued lost earnings and eventual withdrawal from the labor force [Welch, et al. 2010]. A recent study has found that lost-time occupational injuries result in a substantial increase in the number of workers receiving Social Security Disability Insurance benefits, benefits only available to people whose disability is total and expected to be long-lasting [O'Leary, et al. 2012].
Workplace injuries are associated with declines in income similar in magnitude to job loss from mass layoffs [Jacobson, et al. 1993, Kletzer 1998, Reville, et al. 2001]. Studies have shown that lower wages are associated with worse health-related outcomes [Du and Leigh 2015, Leigh and Du 2012], and studies of job loss have shown increased mortality. For example, Sullivan and Von Wachter followed long-tenure displaced workers for 25 years after job loss [Sullivan and von Wachter 2009]. They found that, in the 5 years after mass layoffs, high-seniority male workers had a mortality hazard that was 50 to 100 percent greater than would otherwise have been expected. Over the next decade, the hazard was smaller, but was still 10 to 15 percent greater than expected. Studies in Denmark, Sweden, and the Netherlands also show mortality impacts of job loss.
There is some direct evidence that non-fatal workplace injuries are associated with increased mortality. Standardized mortality studies of workers with permanent partial disabilities in Taiwan have shown substantial increases in mortality among workers with the highest workers’ compensation disability ratings as compared with those rated least severe [Ho, et al. 2006, Lin, et al. 2010]. These increases may have been understated because the comparison group was workers with minor permanent disability. A more recent study observed workers in Ontario receiving permanent partial disability benefits [Scott-Marshall, et al. 2013]. This study compared the mortality of injured workers with matched comparison workers and found hazard ratios of 1.29 for women and 1.22 for men. Our study captures a wider range of injured workers, including not only those categorized as having permanent disabilities but also others who lost more than a week’s work as a result of their injuries.
Building on previous studies, we derive Kaplan-Meier and Cox regression estimates of mortality among injured workers in New Mexico. We base these estimates on injury data from the New Mexico workers’ compensation system and earnings and mortality data from the Social Security Administration (SSA).
METHODS
Identification of injuries and linking to SSA data
The state of New Mexico Workers’ Compensation Administration (WCA) provided us with data on all cases with injury dates from 1992 through 2001 for which workers’ compensation benefits were paid (N=214,230).
The New Mexico data includes information on the characteristics of the injured worker, the injury and the employer, compensated time lost from work, and benefits paid. The New Mexico workers’ compensation system pays only medical benefits for injuries that require seven or fewer calendar days off work and entail no permanent disability. It pays additional “lost-time benefits for injuries involving more than seven calendar days off work or some permanent disability. We hypothesize that these “lost-time” cases are potentially at increased risk of mortality compared with injured workers who received “medical-only” benefits. From 1992-2001, there were 63,689 lost-time cases (30 percent of the total). The remaining 150,541 cases (70 percent) involved only medical-care benefits.
In the 1992-2001 data, 22 percent of workers have more than one injury, and 49 percent of second injuries occur within 2 years of the first injury. This is important because the first injury might causally affect the occurrence and impact of subsequent injuries. We do not observe individuals before 1992, so some of the injuries, particularly in the early years of our sample, may not have been the first injury. For this reason, we removed workers whose first observed injury occurred in 1992 or 1993 as a compromise between reducing the number of subsequent injuries included in the analysis and maintaining sample size. We also excluded injuries occurring after 2000. This is because claim data were collected in 2003, and new cases can enter the system or change from medical-only to lost-time in the first few years after injury. This left us with injuries from 1994-2000.
Finally, we eliminated death cases, cases where death is tied directly to the injury and usually occurs close to the date of injury. After these exclusions, 156,961 workers’ compensation cases remained. This sample consisted of 44,675 lost-time cases and 112,286 medical-only cases.
We kept one injury record for each injured worker and considered the index injury to be the first lost-time injury in the data. If a worker incurred only medical-only injuries, we considered the first of these as the index injury. If a worker had a medical-only injury and one or more subsequent lost-time injuries, the index injury was the first lost-time injury. We also excluded people who were below age 15 or above age 80 at the time of injury. Confining our sample to one observation per person and introducing the age restriction reduced our analytic sample to 107,328 cases, of which 70,951 (66%) were medical-only and 36,377 (34%) were lost-time.
We linked the workers’ compensation data to SSA data using Social Security’s enumeration validation system (EVS) based on each workers’ Social Security Number (SSN), name, date of birth, and gender. Approximately 96 percent of the workers’ compensation claims had valid SSNs. Using the validated SSN, we linked each worker to his or her Detailed Earnings Record in the SSA Master Earnings File, retrieving annual earnings from 7 years before injury through 2014. These data include regular wages and salaries, tips, self-employment income, and deferred compensation. (See Seabury et al. [Seabury, et al. 2014] and O’Leary et al. [2012] for detailed descriptions of the data.)
The institutional review boards at Boston University and the National Institute of Occupational Safety and Health provided human subjects’ institutional approval. Both waived informed consent based on the criteria under 45 CFR 46.116(d). The State of New Mexico and the institutions sharing its data – Boston University, and the SSA – signed confidentiality agreements. Similarly, Boston University and the SSA signed confidentiality agreements with the National Center for Health Statistics, which holds the National Death Index data.
Mortality
Prior research on mortality using SSA data has generally used SSA’s publicly available Death Master File (DMF). Several studies have evaluated the completeness of the DMF and found validation rates as low as 74 percent for younger individuals, but with better DMF validation rates for older populations, and improving validation rates in more recent years [Cowper, et al. 2002, Lash and Silliman 2001, Quinn, et al. 2008]. Public DMF data, however, include only “reportable” deaths from SSA’s Numerical Identification System (NUMIDENT), SSA’s registry of all SSNs. Deaths that come from state records are not reportable to the DMF. Because of these limitations of the DMF, we use the full public NUMIDENT directly and combine this information with data from SSA’s Vital Status System (VSS). The VSS is a standard SSA routine that scans the NUMIDENT for reportable deaths and scans other available records at SSA for evidence that an individual remains alive. Evidence that people are alive comes from sources like reported earnings from the Internal Revenue Service and SSA benefit records. Combining these data produces the most complete SSA data on deaths, people presumed alive, and those of unknown vital status as of October 30, 2014. From this combined data, we find 9,060 (8%) known to be deceased, 85,162 (80%) presumed alive, and 13,106 (12%) of unknown status. The 9,060 known deceased includes 2,038 who would have been classified as unknown in the DMF, but who we reclassified using the full NUMIDENT.
We sent a random sample of 1000 people of unknown vital status to the National Death Index (NDI) to see how many of them the NDI classified as dead. Only six of these people (0.6 percent) were classified as dead in the NDI. We therefore decided to classify all those of unknown status in the SSA data as alive. Thus, our analysis sample includes 9,060 known to be deceased and 98,268 presumed to be alive. Results omitting those of unknown vital status are very similar and are available upon request.
Table I displays summary statistics for the New Mexico data used in this study. For both men and women, the ratio of lost-time to medical-only injuries tends to increase with age. For women, this ratio tends to decline as earnings increase. For men, it is similar across earnings categories, except possibly for the highest earnings group. Male workers in mining and in transportation, communication, and utilities industries are more likely than others to have lost-time injuries than medical-only injuries. For women, retail trade has a higher proportion of lost-time injuries. Cumulative mortality is greater for men and women with lost-time injuries 5, 10, 15, and 20 years after injury.
TABLE I.
Summary Statistics for New Mexico 1994-2000 Occupational Injuriesa
| Women | Men | |||
|---|---|---|---|---|
| Lost time | Medical-only | Lost time | Medical-only | |
| N | 12,415 | 27,868 | 23,962 | 43,083 |
| Age at injury (%) (years) | ||||
| 15-24 | 12.1 | 18.9 | 16.4 | 24.7 |
| 25-34 | 24.2 | 26.6 | 29.6 | 32.0 |
| 35-44 | 31.2 | 28.1 | 28.9 | 24.4 |
| 45-54 | 21.5 | 18.8 | 16.6 | 12.9 |
| 55-64 | 9.2 | 6.8 | 7.4 | 5.3 |
| 65+ | 1.9 | 0.9 | 1.2 | 0.8 |
| Earnings, year before injury (%) (2007 $) | ||||
| 0 - 9,999 | 34.4 | 30.3 | 24.4 | 24.8 |
| 10,000 - 19,999 | 31.9 | 28.0 | 23.4 | 22.0 |
| 20,000 - 29,999 | 18.2 | 19.5 | 20.9 | 20.1 |
| 30,000 - 39,999 | 8.2 | 11.1 | 13.9 | 13.4 |
| 40,000- 49,999 | 4.0 | 5.8 | 8.0 | 8.4 |
| 50,000 + | 3.4 | 5.3 | 9.4 | 11.3 |
| Industry of At-Injury Employer (%) | ||||
| Missing | 0.5 | 6.7 | 1.0 | 9.8 |
| Agriculture, Forestry, and Fishing | 1.0 | 0.9 | 2.3 | 1.7 |
| Mining | 0.5 | 0.4 | 8.2 | 4.5 |
| Construction | 2.0 | 3.0 | 22.8 | 17.0 |
| Nondurable Manufacturing | 3.7 | 2.8 | 4.6 | 4.1 |
| Durable Manufacturing | 2.8 | 3.4 | 4.7 | 5.5 |
| Transportation, Communication, | 6.3 | 7.2 | 10.1 | 6.5 |
| Wholesale Trade | 2.2 | 1.8 | 5.6 | 5.0 |
| Retail Trade | 28.0 | 19.7 | 14.4 | 16.2 |
| Finance, Insurance, and Real Estate | 2.6 | 3.0 | 1.3 | 1.1 |
| Hospitality, Recreation, Business, and Personal Services | 12.0 | 9.4 | 10.4 | 10.3 |
| Healthcare Services | 16.0 | 14.0 | 2.0 | 2.4 |
| Legal, Educational, and Social Services | 17.6 | 21.1 | 6.9 | 7.8 |
| Public Administration | 5.1 | 6.6 | 5.9 | 8.1 |
| Cumulative mortality (%) | ||||
| 5 years post-injury | 1.0 | 0.7 | 2.0 | 1.3 |
| 10 years post-injury | 3.1 | 2.0 | 5.0 | 3.5 |
| 15 years post-injury | 6.1 | 3.9 | 9.3 | 6.4 |
| 20 years post-injury | 8.1 | 5.4 | 11.8 | 8.5 |
Lost-time cases involve more than seven calendar days lost from work or permanent disability benefits. Medical-only cases have seven or fewer days lost from work and no permanent disability benefits.
Statistical Analysis
Our hypothesis is that work-related injuries are associated with an increased hazard of mortality. To test this hypothesis, we compared the mortality hazard of workers with non-fatal lost-time injuries (“injured workers”) to workers with medical-only injuries (“comparison workers”). Injuries were classified as fatal if they were classified as such in the workers’ compensation claim records. Workers with medical-only injuries have lost seven or fewer days from work and have no recorded permanent disability as a consequence of their injuries. We estimated the increased risk of mortality from lost-time injuries by estimating the difference between the covariate-adjusted probability of mortality for injured workers to that of the sample of comparison workers described above. Estimation was done separately for men and women to allow for different baseline mortality and labor-market experience. We used SAS 9.3© (Cary, NC) for all statistical estimates.
After assembling the data, we first derived sex-specific Kaplan-Meier curves to estimate time to death for injured workers and comparison workers. Although the Kaplan-Meier curves have the advantage of being nonparametric and easy to interpret, they fail to account for other covariates in the data. To account for other covariates available in our data, we first estimated Cox proportional hazard models separately for men and women, with a lost-time injury dummy variable, 10-year age categories, industry, and pre-injury earnings as independent variables. Age is a critical covariate, as mortality hazard rises with age. Health status is known to vary by industry, which can be related to selection into industry by health status or to industry-specific health risks [Arheart, et al. 2011]. Pre-injury earnings can also capture the impact of pre-injury health and are related to education, a well-known predictor of health status and mortality.
The Cox model assumes that the hazard ratio for each covariate is constant over time. We tested the proportional hazards assumption by adding time-covariate interactions to the basic model. Interactions between age categories and dummy variables for more than 5 years and more than 10 years after injury were statistically significant. Thus, these estimates rejected the proportional hazards assumption for the age categories. To account for this, we estimated the Cox model stratifying the estimates by age category. As a consequence, we do not estimate the effect of age on mortality.
RESULTS
Figure 1 shows Kaplan-Meier curves for female lost-time and medical-only cases from 1994 to 2000, and Figure 2 shows these curves for male cases. By the end of the twenty years, 11.0 percent of female lost-time cases had died, as compared to only 7.0 percent of female medical-only cases. The comparable numbers for men are 15.1 percent and 10.6 percent. Overall, we see substantial differences in mortality between workers with lost-time and medical-only injuries. (Differences are significant at p<.0001 for log-rank, Wilcoxon, and likelihood ratio tests.) Of course, we also see much lower mortality for women than men.
FIGURE 1.
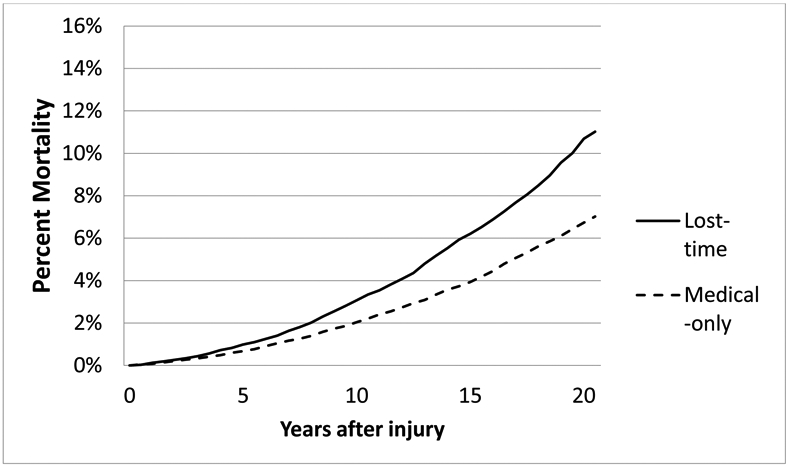
Cumulative Mortality, Lost-time and Medical-only cases, New Mexico Women, 1994-2000 Injuries
FIGURE 2.
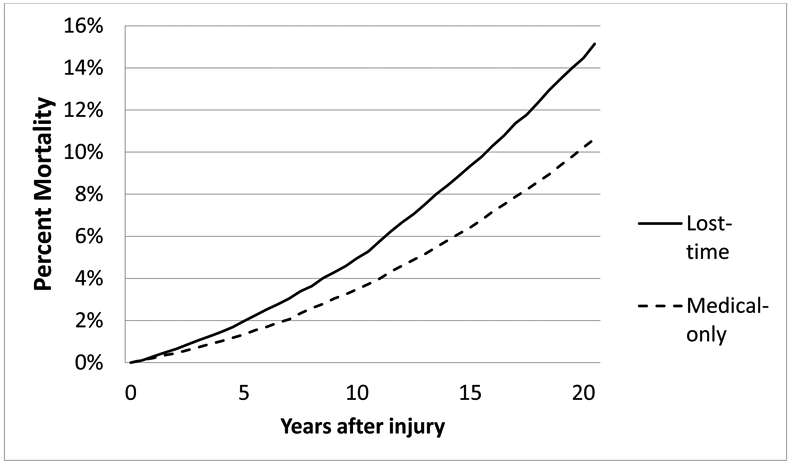
Cumulative Mortality, Lost-time and Medical-only cases, New Mexico Men, 1994-2000 Injuries
To account for the impact of age, sex, earnings, and industry of employment on mortality, we estimated Cox proportional hazards models of mortality. Because of the substantial gender differences in mortality hazard and causes of mortality, we estimated separate models for men and women, and we stratified by age category because age had failed the proportional hazards test. The results are shown in Table II. Estimated mortality hazard ratio for lost-time injuries is 1.26 for women and 1.21 for men, with 95 percent confidence intervals far from 1.00. Thus, it appears that lost-time occupational injuries may substantially increase mortality risk. We also see a substantial income effect. For both women and men, the hazard ratio in the lower income groups is elevated when compared to the higher income groups. Women earning less than $10,000 per year have 1.94 times the mortality hazard as women earning at least $50,000 per year. For men, this ratio is 2.37. There are some industry differences in odds ratios, but many of the odds ratios are not significantly different from 1.0.
TABLE II.
Proportional Hazards Mortality Estimates, New Mexico Injured Workers, 1994-2000 Injuries, Estimates Stratified by Agea
| Women | Men | |||
|---|---|---|---|---|
| Hazard Ratio |
95% Confidence Interval |
Hazard Ratio |
95% Confidence Interval |
|
| Lost-time Injury b | 1.24 | 1.15 – 1.35 | 1.21 | 1.15 – 1.27 |
| Earnings, Year Before Injury (2007 $) | ||||
| 0 - 9,999 | 1.94 | 1.57 – 2.40 | 2.37 | 2.15 – 2.61 |
| 10,000 - 19,999 | 1.53 | 1.24 – 1.89 | 1.90 | 1.72 – 2.09 |
| 20,000 - 29,999 | 1.29 | 1.03 – 1.60 | 1.57 | 1.42 – 1.73 |
| 30,000 - 39,999 | 1.16 | 0.92 – 1.47 | 1.34 | 1.20 – 1.49 |
| 40,000- 49,999 | 1.27 | 0.98 – 1.64 | 1.21 | 1.08 – 1.37 |
| 50,000 + (Reference group) | -- | -- | -- | -- |
| Industry | ||||
| Missing | 1.00 | 0.82 – 1.22 | 1.07 | 0.96 – 1.21 |
| Agriculture, Forestry, and Fishing | 0.89 | 0.57 – 1.39 | 0.83 | 0.68 – 1.00 |
| Mining | 0.96 | 0.52 – 1.81 | 1.15 | 1.02 – 1.29 |
| Construction | 1.08 | 0.84 – 1.40 | 1.07 | 0.99 – 1.17 |
| Nondurable Manufacturing | 0.70 | 0.54 – 0.91 | 0.93 | 0.81 – 1.07 |
| Durable Manufacturing | 0.73 | 0.56 – 0.96 | 0.95 | 0.83 – 1.08 |
| Transportation and Communication | 0.70 | 0.58 – 0.85 | 1.05 | 0.94 – 1.17 |
| Wholesale Trade | 1.14 | 0.86 – 1.51 | 0.89 | 0.78 – 1.02 |
| Retail Trade (Reference group) | -- | -- | -- | -- |
| Finance, Insurance, and Real Estate | 0.75 | 0.57 – 0.98 | 0.84 | 0.67 – 1.06 |
| Hospitality, Recreation, Business, and Personal Services | 0.91 | 0.79 – 1.05 | 1.16 | 1.06 – 1.28 |
| Healthcare Services | 0.97 | 0.85 – 1.10 | 1.14 | 0.97 – 1.35 |
| Legal, Educational, and Social Services | 0.67 | 0.59 – 0.75 | 0.95 | 0.86 – 1.06 |
| Public Administration | 0.98 | 0.82 – 1.16 | 0.85 | 0.75 – 0.96 |
Stratifying by age allows for a different baseline hazard for each age group, but no hazard ratios are estimated for age groups.
Lost-time cases involve more than seven calendar days lost from work or permanent disability benefits. Medical-only cases have seven or fewer days lost from work and no permanent disability benefits.
DISCUSSION
This is the first U.S. study of the relationship between non-fatal occupational injuries and mortality. It is the only study to date to include injuries other than those classified by workers’ compensation as involving permanent disability. The results show a substantial increase in the mortality hazard of both men and women who incurred lost-time occupational injuries. This increase in overall health risk related to non-fatal occupational injuries adds an extra dimension to what we already know about the overall benefits of controlling workplace hazards. Past research has found that these injuries cause substantial lost earnings and medical costs [Leigh 2011], limitations in family roles (household chores, parenting, etc.), depression and anxiety, and disruptions in family life.[Keogh, et al. 2000, Morse, et al. 1998, Pransky, et al. 2000, Strunin and Boden 2004]. This study adds another potential impact: a decline in workers’ lifespan.
It is helpful to consider our results in comparison with another, more well-known health risk. Studies have estimated that the mortality hazard ratio for a 10-mm increase in either daytime or nighttime systolic blood pressure in hypertensive individuals is less than 1.2 [Dolan, et al. 2005, Fagard, et al. 2008]. This is smaller than our estimate of the effect of a lost-time injury. This suggests that the resources devoted to research on and prevention of workplace injuries and illnesses should at least match those devoted to hypertension.
Beyond understanding the mortality risk associated with workplace injuries as a potential measure of the cost of those injuries, this mortality analysis also serves as a means of validating the link between the health impacts of workplace injuries and receipt of disability benefits. Death is prima facie evidence of poor health. Some argue that filing for disability benefits includes an incentive/choice component — that those who are injured exaggerate their injuries to attain benefits rather than work. This argument does not extend to death, so the fact that we see the same kind of long-term relationship between workplace injury and death as we see between workplace injury and receipt of disability benefits [O'Leary, et al. 2012] provides support for the hypothesis that the disability consequences of workplace injuries are real. This also suggests a potential future research topic: to what extent does the receipt of Social Security Disability benefits predict future mortality?
Limitations
This is a study in one state of injuries in specific years. We do not know whether these results would extend to other states with different populations and labor market conditions. Also, we do not know whether the recent extension of health insurance by the Affordable Care Act has modified the relationship between injuries and mortality by improving access to health care.
We also must consider the role of misclassification, which has been shown to have greater potential for bias on occupational studies than confounding [Blair, et al. 2007]. Exposure misclassification could occur, for example, if the data from workers’ compensation claims contained incorrect or incomplete information on the worker and/or the injury. It is possible that errors in matching to the Social Security data on mortality may occur or that the Social Security mortality data contains inaccuracies. The data sources are independent from each and therefore we anticipate that any misclassification would be nondifferential. In particular, we note that recording of the exposure data was documented prior to death occurring, further supporting nondifferential misclassification of exposure. As a result, misclassification of binary exposure or outcome has the potential to induce a bias to the null, leading us to underestimate the association between non-fatal injury and long-term mortality.
The most important potential limitation of this study is that unobserved confounders may bias upward our estimate of injury effect. We believe that important candidates are pre-injury health, health habits, disability, and occupation, all of which can affect both injury rates [Galizzi and Tempesti 2015, Ryan, et al. 1992, Xiang, et al. 2008] and health and mortality [Centers for Disease Control and Prevention 2008, Conti, et al. 2010, Walter, et al. 2009, Winkleby, et al. 1992]. The impact of these as potential confounders may, however, be muted by the inclusion of pre-injury earnings in the survival regressions. Lower earnings may reflect, in part, disability or poor health [Seabury, et al. 2014, Smith 1999]. As a consequence, their inclusion in the analysis may have reduced the bias caused by these potential confounders. Still, some residual confounding seems likely. Also, our comparison group is workers with medical-only injuries. If this group has a greater hazard of mortality than uninjured workers, then our estimates may be biased toward zero.
In addition, we know that many injuries go unreported [Azaroff, et al. 2002, Boden and Ozonoff 2008, Rosenman, et al. 2006]. As a result, our results would only apply to paid workers’ compensation cases. Because of how experience-rated premiums are calculated, employers may make an effort to limit time off work to the waiting period (seven days in New Mexico) [Kralj 1994]. This would imply that some injuries that would otherwise be classified lost-time would be moved to the medical-only category. Misclassification in the other direction would be less likely to occur. We can think of no reason for this exposure misclassification to be differential – for it to be more or less common among people at greater risk of dying.
CONCLUSIONS
Lost-time occupational injuries are associated with a substantially elevated mortality hazard. Estimated hazard ratios are 1.24 for women and 1.21 for men, with 95 percent confidence intervals of (1.15, 1.35) and (1.15, 1.27) respectively. This suggests that, beyond substantial financial and family consequences, we have identified an important potential cost of these injuries and a further reason to focus on preventing them.
Still, research on this subject is in its early stages. To get more accurate estimates of the mortality impact, we need to account for possible bias associated with confounding.
If non-fatal injuries are associated with premature mortality, then it is important to quantify these effects and to begin a line of study to replicate results, to test alternative causal hypotheses, to determine which causes of death contribute to premature mortality [Burnett, et al. 1997], and so see if results are similar in other jurisdictions. The ultimate goal of this line of research would be to determine the contribution of specific work hazards to mortality, leading to the elimination or sizeable reduction of those hazards.
Acknowledgements
The National Institute for Occupational Safety and Health (grant number R21-OH010555) provided financial support for this work. The views expressed here are not necessarily the views of that organization. We thank Abay Asfaw, David Ozonoff and two anonymous reviewers for their helpful insights. No author has any potential conflicts of interest to report.
Footnotes
Institution and Ethics approval and informed consent: The work was performed at Boston University School of Public Health, Social Security Administration, and George Washington University. Human subjects’ institutional review and approval was given by the Boston University Institutional Review Board for protection of human subjects and the National Institute for Occupational Safety and Health Institutional Review Board. Both waived the requirement for informed consent because (1) the research involves no more than minimal risk to the subjects, (2) the waiver will not adversely affect the rights and welfare of the subjects, (3) the research could not practicably be carried out without the waiver or alteration; and (4) whenever appropriate, the subjects will be provided with additional pertinent information after participation.
Disclosure (Authors): The authors declare no conflicts of interest.
Disclaimer: None
REFERENCES
- Arheart KL, Fleming LE, Lee DJ, LeBlanc WG, Caban-Martinez AJ, Ocasio MA, McCollister KE, Christ SL, Clarke T, Kachan D. 2011. Occupational vs. Industry Sector Classification of the US Workforce: Which approach is more strongly associated with worker health outcomes? Am J Ind Med 54: 748–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azaroff LS, Levenstein C, Wegman DH. 2002. Occupational injury and illness surveillance: Conceptual filters explain underreporting. Am J Public Health 92: 1421–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair A, Stewart P, Lubin JH, Forastiere F. 2007. Methodological issues regarding confounding and exposure misclassification in epidemiological studies of occupational exposures. Am J Ind Med 50: 199–207. [DOI] [PubMed] [Google Scholar]
- Boden LI, Galizzi M. 2003. Income losses of women and men injured at work. J Hum Resour 38: 722–757. [Google Scholar]
- Boden LI, Ozonoff A. 2008. Capture-recapture estimates of nonfatal workplace injuries and illnesses. Ann Epidemiol 18: 500–506. [DOI] [PubMed] [Google Scholar]
- Burnett C, Maurer J, Dosemeci M. 1997. Mortality by occupation, industry, and cause of death, 24 reporting states (1984-1988). Mortality by occupation, industry, and cause of death, 24 reporting states (1984-1988): National Institute for Occupational Safety and Health. [Google Scholar]
- Centers for Disease Control and Prevention. 2008. Smoking-attributable mortality, years of potential life lost, and productivity losses - United States, 2000-2004. Morbidity and Mortality Weekly Report 57: 1226–1228. [PubMed] [Google Scholar]
- Conti G, Heckman J, Urzua S. 2010. The education-health gradient. The American economic review 100: 234–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowper DC, Kubal JD, Maynard C, Hynes DM. 2002. A primer and comparative review of major US mortality databases. Ann Epidemiol 12: 462–468. [DOI] [PubMed] [Google Scholar]
- Dolan E, Stanton A, Thijs L, Hinedi K, Atkins N, McClory S, Den Hond E, McCormack P, Staessen JA, O’Brien E. 2005. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality the Dublin outcome study. Hypertension 46: 156–161. [DOI] [PubMed] [Google Scholar]
- Dong XS, Wang X, Largay JA, Sokas R. 2015. Long-term health outcomes of work-related injuries among construction workers—findings from the National Longitudinal Survey of Youth. Am J Ind Med 58: 308–318. [DOI] [PubMed] [Google Scholar]
- Du J, Leigh JP. 2015. Effects of wages on smoking decisions of current and past smokers. Ann Epidemiol 25: 575–582. [DOI] [PubMed] [Google Scholar]
- Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML, De Bacquer DA. 2008. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension 51: 55–61. [DOI] [PubMed] [Google Scholar]
- Galizzi M, Tempesti T. 2015. Workers’ Risk Tolerance and Occupational Injuries. Risk analysis 35: 1858–1875. [DOI] [PubMed] [Google Scholar]
- Galizzi M, Zagorsky JL. 2009. How do on-the-job injuries and illnesses impact wealth? Labour Econ 16: 26–36. [Google Scholar]
- Ho JJ, Hwang JS, Wang JD. 2006. Life-expectancy estimations and the determinants of survival after 15 years of follow-up for 81 249 workers with permanent occupational disabilities. Scand J Work Env Hea 32: 91–98. [DOI] [PubMed] [Google Scholar]
- Jacobson LS, Lalonde RJ, Sullivan DG. 1993. Earnings Losses of Displaced Workers. Am Econ Rev 83: 685–709. [Google Scholar]
- Keogh JP, Nuwayhid I, Gordon JL, Gucer PW. 2000. The impact of occupational injury on injured worker and family: outcomes of upper extremity cumulative trauma disorders in Maryland workers. Am J Ind Med 38: 498–506. [DOI] [PubMed] [Google Scholar]
- Kletzer LG. 1998. Job displacement. J Econ Perspect 12: 115–136. [Google Scholar]
- Kralj B 1994. Employer responses to workers' compensation insurance experience rating. Relations industrielles/Industrial Relations: 41–61. [Google Scholar]
- Lash TL, Silliman RA. 2001. A comparison of the national death index and social security administration databases to ascertain vital status. Epidemiology 12: 259–261. [DOI] [PubMed] [Google Scholar]
- Leigh JP. 2011. Economic burden of occupational injury and illness in the United States. Milbank Q 89: 728–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh JP, Du J. 2012. Are low wages risk factors for hypertension? The European Journal of Public Health 22: 854–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin SH, Lee HY, Chang YY, Jang Y, Chen PC, Wang JD. 2010. Increased Mortality Risk for Workers With a Compensated, Permanent Occupational Disability of the Upper or Lower Extremities: A 21-Year Follow-up Study. Am J Epidemiol 171: 917–923. [DOI] [PubMed] [Google Scholar]
- Morse TF, Dillon C, Warren N, Levenstein C, Warren A. 1998. The economic and social consequences of work-related musculoskeletal disorders: the Connecticut Upper-Extremity Surveillance Project (CUSP). International journal of occupational and environmental health 4: 209–216. [DOI] [PubMed] [Google Scholar]
- O'Leary P, Boden LI, Seabury SA, Ozonoff A, Scherer E. 2012. Workplace injuries and the take-up of Social Security disability benefits. Social security bulletin 72: 1–17. [PubMed] [Google Scholar]
- Pransky G, Benjamin K, Hill-Fotouhi C, Himmelstein J, Fletcher KE, Katz JN, Johnson WG. 2000. Outcomes in work-related upper extremity and low back injuries: results of a retrospective study. Am J Ind Med 37: 400–409. [DOI] [PubMed] [Google Scholar]
- Quinn J, Kramer N, McDermott D. 2008. Validation of the Social Security Death Index (SSDI): an important readily-available outcomes database for researchers. Western Journal of Emergency Medicine 9: 6–8. [PMC free article] [PubMed] [Google Scholar]
- Reville RT, Boden LI, Biddle J, Mardesich C. 2001. An evaluation of New Mexico workers' compensation permanent partial disability and return to work Santa Monica, CA: Rand Institute for Civil Justice. xxvii, 90 p. p. [Google Scholar]
- Rosenman KD, Kalush A, Reilly MJ, Gardiner JC, Reeves M, Luo Z. 2006. How much work-related injury and illness is missed by the current national surveillance system? J Occup Environ Med 48: 357–365. [DOI] [PubMed] [Google Scholar]
- Ryan J, Zwerling C, Orav EJ. 1992. Occupational risks associated with cigarette smoking: a prospective study. Am J Public Health 82: 29–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott-Marshall HK, Tompa E, Wang Y, Liao Q. 2013. Long-term mortality risk in individuals with permanent work-related impairment. Canadian journal of public health= Revue canadienne de sante publique 105: e330–e335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seabury SA, Scherer E, O'Leary P, Ozonoff A, Boden L. 2014. Using linked federal and state data to study the adequacy of workers' compensation benefits. Am J Ind Med 57: 1165–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JP. 1999. Healthy bodies and thick wallets: the dual relation between health and economic status. J Econ Perspect 13: 144–166. [PMC free article] [PubMed] [Google Scholar]
- Strunin L, Boden LI. 2004. Family consequences of chronic back pain. Soc Sci Med 58: 1385–1393. [DOI] [PubMed] [Google Scholar]
- Sullivan D, von Wachter T. 2009. Average Earnings and Long-Term Mortality: Evidence from Administrative Data. Am Econ Rev 99: 133–138. [DOI] [PubMed] [Google Scholar]
- Sullivan D, von Wachter T. 2009. Job Displacement and Mortality: An Analysis Using Administrative Data. Q J Econ 124: 1265–1306. [Google Scholar]
- Walter S, Kunst A, Mackenbach J, Hofman A, Tiemeier H. 2009. Mortality and disability: the effect of overweight and obesity. International journal of Obesity 33: 1410–1418. [DOI] [PubMed] [Google Scholar]
- Welch LS, Haile E, Boden LI, Hunting KL. 2010. Impact of Musculoskeletal and Medical Conditions on Disability Retirement-A Longitudinal Study Among Construction Roofers. Am J Ind Med 53: 552–560. [DOI] [PubMed] [Google Scholar]
- Winkleby MA, Jatulis DE, Frank E, Fortmann SP. 1992. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health 82: 816–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang H, Kidwell K, Wheeler K. 2008. Role of disability in the association between obesity and unintentional injuries. Disability and health journal 1: 99–107. [DOI] [PubMed] [Google Scholar]


