Abstract
Background
The Canadian 24-Hour Movement Guidelines for Adults was released in 2020. There is a dearth of evidence on the association between adherence to the 24 h movement guidelines and health indicators. This study aims to (a) explore the associations between potential correlates and meeting the 24 h movement guidelines using a sample of Chinese university students; and (b) examine if meeting 24 h movement guidelines is associated with the severity of anxiety symptoms.
Methods
Cross-sectional findings are based on 1846 Chinese university students (mean age = 20.7 years, 64.0% female). Movement behaviors (physical activity, sedentary behavior, and sleep duration), possible correlates, and anxiety symptoms were measured through self-reported online questionnaires. Logistic regression models were performed to examine the associations.
Results
We found that male students and those who had a mother with a master’s degree or above, more close friends and higher perceived family affluence were more likely to meet the overall 24 h guidelines. Meeting all 24 h movement guidelines presented the lower odds for severe anxiety symptoms than those meeting fewer recommendations in the 24 h movement guidelines.
Conclusions
As one of the first to examine the correlates of adherence to the 24 h movement guidelines and the relationship between anxiety symptoms and meeting the guidelines among Chinese university students, our findings contribute to the growing body of evidence linking movement behaviors, psychosocial correlates, and heath indicators. Schools and health providers can encourage movement behaviors that follow the guidelines on campus.
Keywords: Anxiety, Anxiety symptoms, University students, Physical activity, Sedentary behavior, Sleep
Introduction
In the transition from adolescence to adulthood, university students are often exposed to heavy psychosocial pressures, making them more vulnerable to mental health problems [1, 2]. Data has shown that anxiety, characterized by excessive fears or worries [3, 4], has emerged as one of the most prevalent and severe mental health problems among Chinese university students, with a prevalence rate of anxiety symptoms from 7.6 to 54.4% among Chinese university students (age 15–29) in the past decade [5–10]. Anxiety symptoms are linked to various adverse life outcomes, including lower educational attainment, reduced employment, and poor quality of life [11]. Previous cross-cultural studies revealed that Chinese university students tended to be more anxious than their American counterparts [12]. This finding addressed the necessity of investigating the anxiety symptoms and identifying their unique correlates among Chinese university students, which can inform appropriate preventive intervention against anxiety and further facilitate an all-around development of Chinese university students.
24 h movement behaviors
From a perspective of movement behavior, sleep, sedentary behavior (SB), and physical activity (PA) are beneficial to mental health outcomes. Extensive literature has documented significant associations between anxiety symptoms and sleep [13], PA [14], and SB [15]. For example, in the sample of Chinese university students, negative associations were found between PA and anxiety symptoms [16, 17]. Liu et al., observed the bidirectional longitudinal relationships between SB (e.g., long-time mobile phone use) and the severity of anxiety symptoms among Chinese university students [18]. Among Chinese students (aged 18–25), anxiety symptoms are significantly associated with sleep duration [19]. Although traditional studies highlighted the independent effect of the single movement behavior and confirmed the independent roles, those studies had a poor adjustment for time spent in other movement behaviors [20], which overlooks a clear fact that individual has a fixed budget of 24 h a day that was entirely composed of PA, SB, and sleep. In other words, any shift in time invested in a single one of these movement behaviors could inevitably increase or decrease the remaining [21]. Consequently, it is necessary to emphasize that “the whole day matters” and investigate the optimal balance among the time spent in 24 h movement behaviors and the combined health benefits of these co-dependent and interrelated behaviors [20–22].
This holistic perspective of 24 h movement behavior is in line with the integrated vs. isolated movement behavior paradigm and the theoretical framework of studying health-related time-use patterns, Framework for Viable Integrative Research in Time-Use Epidemiology (VIRTUE), which guides studies on methods, determinants, composition, outcomes, and interventions of optimally integrated patterns of time-use for population health [20, 22]. With this lens, Canadian 24-Hour Movement Guidelines for Adults aged 18–64 years, a set of health recommendations of the combination of PA, SB, and sleep, was issued [23, 24]. The fundamental principle of 24 h movement guidelines is to shift the focus from a single movement behavior recommendation to an integrated guideline that contains combined recommendations for PA, SB and sleep throughout the whole day [15, 23]. A recent systematic review examining associations between the 24 h movement compositions and health outcomes reinforces the rationale for packaging recommendations for PA, SB, and sleep into an integrated guideline [25]. Specifically, it is recommended that for an adults to be considered to have a healthy movement behavior profile, they need to meet three specific recommendations for time-use of PA (accumulated ≥150 min of moderate-to-vigorous PA per week), SB (≤ 8 h per day) and sleep (7–9 h per day) [23]. A growing body of evidence has documented these guidelines’ value, demonstrating that the combined effect of 24 h movement behavior throughout the day is vital to various health outcomes for children and youth [26, 27] and may have important implications for health across the adult lifespan [22]. To the best of our knowledge, although the 24 h movement guidelines for adults has been issued, there is a dearth of evidence on the association between adherence to the 24 h movement guidelines and anxiety symptoms. Therefore, we aimed to explore the associations between meeting 24 h movement guidelines and the severity of anxiety symptoms.
Moreover, according to the behavioral epidemiology framework [28], identifying factors is also fundamental to determine whether particular behaviors should be targeted in health interventions. Many factors (e.g., sociodemographic, lifestyle, and environmental factors) would influence the development and adherence to movement guidelines [22, 29]. For example, it was shown previously that female students from the Chinese campus have a significantly higher prevalence of low PA, long sedentary time, and poor sleep quality [17, 30]. Short sleepers tend to have low income and be overweight [31]. A study on university students from 23 low-, middle- and high-income countries across the world has revealed that in 17 out of 23 countries, including China, being female is associated with physical inactivity [32]. Additionally, older age (22–30 years), studying in a low- or lower-middle-income country, unhealthy weight status (i.e., underweight, overweight or obese), and lack of social support are also associated with physical inactivity [32].
The present study
Movement behaviors may have the potential to benefit the mental health of university students. With a holistic lens of 24 h movement behaviors, the current study followed specific recommendations of Canadian 24-Hour Movement Guidelines for Adults aged 18–64 years for time-use of PA, SB, and sleep, and aimed to: [1] explore the associations between potential correlates and meeting the 24 h movement guidelines using a sample of Chinese university students; [2] investigate the association between meeting 24 h movement guidelines and anxiety symptoms.
Methods
Participants
This study employed a cross-sectional design using online surveys. A convenient sampling strategy was adopted to recruit participants. A total of 1942 university students were recruited from 30 provinces and autonomous regions (mainly from Guangdong province), with 1846 participants (response rate = 95.1%) providing answers to all of the study’s variables. Before data was collected, study participants provided their consent to participate in the research through an online survey.
Procedure and data collection
Data collection was conducted from August 21 to 31, 2020. At that time, COVID-19 had been controlled in China, and college students were about to return to campus. Participants completed the survey through online platforms (e.g., Tencent’s QQ, Tencent’s WeChat, Sina Weibo, and campus forums) due to COVID-19 restrictions. It took approximately 15 min for each participant to complete the online questionnaire, and each one received compensation for their time spent on the survey (10 CNY, equivalent to 1.5 USD) via online payment for their participation.
Measures
Movement behaviors
Movement behaviors including PA, SB, and sleep were assessed via two self-report questionnaires, including the International Physical Activity Questionnaire-Short Form (IPAQ-SF) and Pittsburgh Sleep Quality Index (PSQI). The good psychometric properties of the IPAQ-SF and PSQI have been shown in Chinese populations [33, 34].
For PA, six items of IPAQ-SF were adopted. Participants were required to recall the frequency and duration of 1) walking activities; 2) moderate PA (e.g., carrying light loads, bicycling at a regular pace, or doubles tennis); and 3) vigorous PA (e.g., heavy lifting, digging, aerobics, or fast bicycling) that they spent over the past seven days. Example item: During the last seven days, on how many days did you do vigorous physical activities like heavy lifting, digging, aerobics, or fast bicycling? Based on the Canadian 24-Hour Movement Guidelines for Adults [23], participants that accumulated ≥150 min of moderate-to-vigorous PA per week were categorized as meeting the 24 h movement guidelines.
For SB, one item of IPAQ-SF was adopted: During the last seven days, how much time did you spend sitting on a weekday? Include time spent at work, at home, while doing course work and during leisure time. This may include time spent sitting at a desk, visiting friends, reading, or sitting or lying down to watch television. Meeting the Canadian 24-Hour Movement Guidelines for Adults requires ≤8 h of SB per day [23].
For sleep, one item from the PSQI was used to assess the sleep duration: During the past month, how many hours of actual sleep did you get at night? (This may be different from the number of hours you spent in bed). Meeting the Canadian 24-Hour Movement Guidelines for Adults requires 7–9 h of sleep daily [23].
Participants were classified into four groups based on whether they met all 24 h movement guidelines, any combination of two individual guidelines, any single individual guideline, or none of the guidelines. Synthetization as numbers can directly examine participants’ movement behavior profiles and their associated mental health outcomes. This approach can help test whether meeting more movement behavior recommendations is associated with better health outcomes.
Anxiety symptoms
The Chinese version of Zung’s Self-rating Anxiety Scale (SAS) has been employed to assess participants’ anxiety symptoms, which has been widely applied in recent research on university students in the context of COVID-19 [35–37]. SAS consists of 20 items, and each item is rated on a scale from 1 to 4. The total raw score is multiplied by 1.25 and then converted into a standardized index score ranging between 25 and 100, with higher scores suggesting more severe anxiety. SAS has shown the capacity to discriminate between clinical and non-clinical samples [38]. The norms that developed for the Chinese population include an index score of 50 as the cut-off point of clinical significance and index scores of symptom severity (i.e., index score 50–60, 61–70, > 70 indicating mild, moderate, severe anxiety, respectively) [39]. These norms have been widely used among the Chinese population as a valuable screening tool for the presence of anxiety symptoms [39]. Therefore, In the current study, SAS ≥ 50 was applied as the cut-off point beyond which scores are considered indicative of the presence of anxiety symptoms.
Potential correlates
Based on previous studies [40], potential correlates included body mass index (BMI; the body weight divided by the square of the body height [kg/m2]), age (years), sex (male or female), siblings (single, two or more), residence (urban or rural), family structure (complete, divorced or other), parents’ educational level (middle school or below, high school, college or university, master or above), number of friends (none, 1–2, 3–5, 6 or more), and perceived family affluence using a scale (from 0 to 10) with higher scores indicating higher perceived family affluence [41].
Statistical analyses
Statistical analyses were performed using STATA 16.1 (Stata Corp, College Station, Texas). Descriptive statistics were used to report the frequency (percentage) and mean (standard deviation [SD]) of categorical and continuous variables, respectively.
To explore the associations between sociodemographic correlates and meeting the 24 h movement guidelines, we performed a binary logistic regression model to examine if meeting the 24 h movement guidelines was associated with the potential correlates. Whether meeting the 24 h movement guidelines (i.e., meeting none of the guidelines vs. meeting at least one of the guidelines) was treated as the dependent variable, and potential correlates were treated as independent variables. All potential correlates were entered in the regression model at once. Meeting none of the guidelines was set as the reference group. Odds ratios (OR) with 95% confidence interval (CI) were reported. Statistical significance was set up as p < 0.05 (two-sided).
To examine the relationship between meeting 24 h movement guidelines and anxiety symptoms (SAS ≥ 50), we used a binary logistic regression model, with meeting 24 h movement guidelines (i.e., number of recommendations met) as the independent variable and anxiety symptoms (i.e., SAS ≥ 50 vs. SAS < 50) as the dependent variable. Correlates including sex, age, siblings, residence, family structure, father education level, mother education level, perceived family affluence, number of friends, and body mass index were controlled. Odds ratios (OR) with 95% confidence interval (CI) were reported. Statistical significance was set up as p < 0.05 (two-sided).
Results
Sample characteristics
As presented in Table 1, the mean age of the sample was 20.7 years (SD = 1.6), and the average BMI (kg/m2) was 20.3 (SD = 2.9). Overall, the prevalence of meeting the 24-Hour movement guidelines was 27.0%. Participants reported a mean score of 41.8 ± 9.8 for anxiety symptoms. The largest proportion of participants were categorized as having minimal anxiety symptoms (79.2%), and 21.8% of participants indicated mild-to-severe anxiety symptoms.
Table 1.
Descriptive characteristics of study sample (n = 1846)
| n (%) / Mean (SD) |
||
|---|---|---|
| Age (years) | 20.7 | (1.6) |
| BMI (kg/m2) | 20.3 | (2.9) |
| Sex | ||
| Male | 665 | (36.0) |
| Female | 1181 | (64.0) |
| Siblings | ||
| Single | 639 | (34.6) |
| Two or more | 1207 | (65.4) |
| Residence | ||
| Urban | 1278 | (69.2) |
| Rural | 568 | (30.8) |
| Family structure | ||
| Full | 1664 | (90.1) |
| Divorced | 117 | (6.3) |
| Other | 65 | (3.5) |
| Perceived family affluence | 5.7 | (1.6) |
| Father education level | ||
| Middle school or below | 891 | (48.3) |
| High school | 636 | (34.5) |
| College or university | 254 | (13.8) |
| Master or above | 65 | (3.5) |
| Mother education level | ||
| Middle school or below | 1086 | (58.8) |
| High school | 560 | (30.3) |
| College or university | 158 | (8.6) |
| Master or above | 42 | (2.3) |
| Number of friends | ||
| None | 29 | (1.6) |
| 1–2 | 608 | (32.9) |
| 3–5 | 964 | (52.2) |
| 6 or more | 245 | (13.3) |
| Meeting the physical activity guidelines | ||
| No | 950 | (51.5) |
| Yes | 896 | (48.5) |
| Meeting the sedentary behavior guidelines | ||
| No | 575 | (31.1) |
| Yes | 1271 | (68.9) |
| Meeting the sleep guidelines | ||
| No | 555 | (30.1) |
| Yes | 1291 | (69.9) |
| Meeting combinations of 24 h movement guidelines | ||
| None | 119 | (6.4) |
| One | 495 | (26.8) |
| Two | 733 | (39.7) |
| All | 499 | (27.0) |
| Anxiety symptoms (scores: mean ± SD) | 41.8 | (9.8) |
| Anxiety symptoms (severity) | ||
| Minimal anxiety (SAS < 50) | 1462 | (79.2) |
| Mild anxiety (SAS 50–60) | 277 | (15.0) |
| Moderate anxiety (SAS 61–70) | 89 | (4.8) |
| Severe anxiety (SAS > 70) | 18 | (1.0) |
Note. SD = standard deviation. SAS = Index score of Zung’s Self-rating Anxiety Scale
Associations between sociodemographic correlates and meeting the 24 h movement guidelines
Table 2 presents the results of correlates of meeting the 24 h movement guidelines. For intrapersonal correlates (i.e., sex, age, and BMI), sex and BMI showed significant cross-sectional associations with the adherence to 24 h movement guidelines. Specifically, compared with the female, male participants were more likely to meet the guidelines (OR = 2.20, 95% CI [1.75, 2.77]). University students with greater BMI were more likely to meet the guidelines (OR = 1.04, 95% CI [1.00, 1.08]).
Table 2.
Correlates of meeting the 24 h movement guidelines
| OR | 95% CI | ||
|---|---|---|---|
| Intercept | 0.21 | 0.03 | 1.32 |
| Body mass index | 1.04 | 1.00 | 1.08 |
| Age | 0.98 | 0.91 | 1.05 |
| Sex | |||
| Male | 2.20 | 1.75 | 2.77 |
| Female | Ref | ||
| Siblings | |||
| Single | 1.01 | 0.80 | 1.29 |
| Two or more | Ref | ||
| Residence | |||
| Urban | 1.03 | 0.80 | 1.33 |
| Rural | Ref | ||
| Family structure | |||
| Full | 0.90 | 0.50 | 1.62 |
| Divorced | 0.76 | 0.37 | 1.58 |
| Other | Ref | ||
| Perceived family affluence | 1.13 | 1.05 | 1.21 |
| Father education level | |||
| Middle school or below | 1.28 | 0.64 | 2.57 |
| High school | 1.39 | 0.70 | 2.75 |
| College or university | 1.74 | 0.87 | 3.48 |
| Master or above | Ref | ||
| Mother education level | |||
| Middle school or below | 0.42 | 0.19 | 0.93 |
| High school | 0.42 | 0.19 | 0.91 |
| College or university | 0.43 | 0.19 | 0.97 |
| Master or above | Ref | ||
| Number of friends | |||
| None | 1.27 | 0.55 | 2.93 |
| 1–2 | 0.64 | 0.45 | 0.90 |
| 3–5 | 0.97 | 0.71 | 1.33 |
| > 6 | Ref | ||
Note. Meeting none of the guidelines was set as the reference group
For interpersonal factors, significant associations were found between mother educational level, perceived family affluence level, numbers of friends, and the likelihood of meeting the guidelines. Specifically, compared with the mother’s educational level of master degree or above, other educational attainment showed a lower likelihood of meeting the guidelines (OR = 0.42–0.43; 95% CI [0.19, 0.91–0.97]). Participants who reported higher perceived family affluence were better compliant with the guidelines (OR = 1.13, 95% CI [1.05, 1.21]). Participants with 1–2 friends were less likely to meet the guidelines than those with six or more friends (OR = 0.64, 95% CI [0.45, 0.90]). No significant association was observed between family structure, the father’s educational level, and the likelihood of meeting the guidelines.
Associations between meeting the 24 h movement guidelines and anxiety symptoms
Figure 1 shows the results. Compared with those who met all 24 h movement guidelines (i.e., PA, SB, and sleep recommendation), participants who met only two recommendations were more likely to have anxiety symptoms (OR = 1.41, 95%CI [1.09, 1.83] p < 0.001). Likewise, the risk for anxiety symptoms of participants who met only 1 guideline increased to 1.84 times compared with the reference group (OR = 1.84, 95%CI [1.41, 2.39], p < 0.001). Finally, the odds of anxiety symptoms among participants following no recommendations was 2.20 times as the reference group that meeting the guidelines (OR = 2.20, 95%CI [1.55, 3.12], p < 0.001).
Fig. 1.
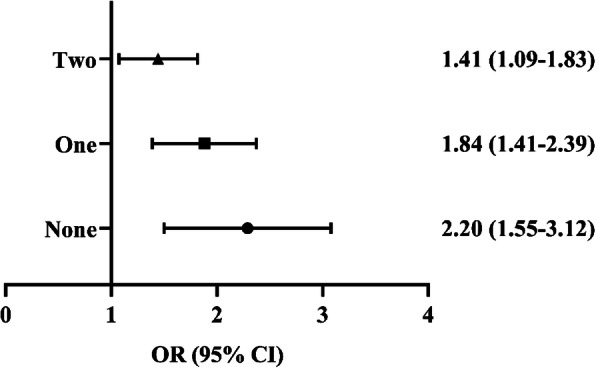
The association between meeting 24 h Guidelines and anxiety symptoms screened positive by Generalized Linear Models. Notes: Models controlled for sex, age, siblings, residence, family structure, father education level, mother education level, perceived family affluence, number of friends, body mass index. Meeting all 24 h movement guidelines was set as the reference group. Two = meeting any two recommendations of the 24 h movement guidelines. One = meeting any one recommendation of the 24 h movement guidelines. None = meeting none of the 24 h movement guidelines
Discussion
To the authors’ knowledge, the current study is one of the first to investigate the correlates of meeting 24 h movement guidelines and its association with anxiety symptoms in a sample of Chinese university students. Those who were male students, had a mother with a master’s degree or above, had more close friends, and perceived higher family affluence were more likely to meet the integrated 24 h guidelines. Among university students, meeting the 24 h movement guidelines presented lower odds for anxiety symptoms than those meeting fewer recommendations in the 24 h movement guidelines.
Understanding factors of compliance with the guidelines is essential for health promotion efforts [22, 28]. Research on the demographic correlates of meeting the 24 h movement guidelines helps identify university students who are most in need of intervention [28]. These demographic correlates may exert potential moderating effects on associations between adherence to the guidelines and health outcomes [22]. However, upon the release of the Canadian 24-Hour Movement Guidelines for Adults in October 2020, current evidence among Chinese university students is insufficient, which limited the capacity of health professionals to target populations with health risks. In other Asian countries, mixed findings were reported. For example, Korean adults who are male, have low incomes, live in nonmetro areas, and have a lower education background tended to comply with the 24 h movement guidelines [42]. Thailand issued a national 24 h movement behavior guidelines, including the recommendations of PA (i.e., at least 150 min/week of moderate and vigorous PA), sleep (between 7 to 9 h per day), and SB (interrupt SB every two hours) [43]. The higher odds for meeting the Thai guidelines were observed among females, those living in rural areas, employed, and those with high education levels [44]. The variations may be attributed to diverse measurements and sample characteristics in different studies, resulting in discrepant research findings. For example, the Thai study used a 24 h time-use diary to assess movement behaviors, and the sample of Thai and Korean study had a wider age range (Thai: 18–59; Korean: 18–64) compared to our sample aged from 18 to 26 years [42, 44]. The Thai study used Thai guidelines that provided recommendations to interrupt SB every 2 h, not to limit SB time to 8 h or less [42].
When comparing the results with those in Chinese children and adolescents, our study yielded similar results that higher parental education levels and family income may facilitate favorable 24 h movement behaviors [26, 44]. The underlying mechanism may be that, like children and adolescents, most university students have not yet achieved financial independence and are dependent on their families in terms of socioeconomic status [45]. Moreover, households of higher socioeconomic provided more opportunities for adopting healthy lifestyles (e.g., less SB and more PA) [46] and maintaining active lifestyles (e.g., more PA) from childhood to adulthood [47]. However, family socioeconomic status cannot represent the whole picture of family-level correlates. Family functioning also plays a vital role in shaping children’s health behaviors [44, 48, 49]. More studies are needed to further explore the influence of multifaceted factors (e.g., family, school, community, and environment) on the adherence to the 24 h movement guidelines [15, 22].
Moreover, in this study, the higher odds for meeting the guidelines were observed in university students with greater BMI. This finding should be interpreted with caution since the value of the odds ratio of BMI was nearly equal to 1 (OR = 1.04), and the lower bound of 95% CI was at the edge of the threshold for significance (95% CI: 1.00 to 1.08). Recent studies found that the distribution of adults’ time-use in movement behaviors was significantly associated with adiposity indicators (i.e., BMI and waist circumference) [22, 44, 50, 51]. Chinese children and adolescents who engaged in the ideal 24 h movement guidelines were shown to be less prone to develop overweight and obesity [26, 44]. Research comparable to those conducted for children and adolescents could be undertaken in adult populations in China and abroad to explore the associations.
Prior research has shown the significant associations between adhering to the 24 h movement guidelines and health benefits across younger populations [22, 27, 44, 52]. The present study found that meeting all recommendations of the guidelines showed a lower odds ratio for higher anxiety symptoms. Our finding is similar to a recent study conducted in western countries indicating that the probability of health benefits increased with the number of guidelines that the adults followed increased [53]. Some of the core biological mechanisms thought to be related to anxiety symptoms may explain the association between movement behaviors and anxiety symptoms. The visceral-afferent feedback model suggests that physical activity may increase the stimulation of the ascending reticular activating system (ARAS), responsible for arousal and the maintenance of wakefulness [54]. When the cortical excitation from physical activity reaches a point at which the inhibitory mechanism of ARAS is activated, the somatic afferent stimulation ultimately decreases [54, 55]. The currently available first-line treatments for anxiety disorders work by interacting with drugs and inhibitory neurotransmitters [56].
Strengths and limitations
A clear and evidence-based guideline on 24 h movement behaviors and its associations with health outcomes could help set measurable indicators for surveillance, provide appropriate guidance to public health professionals, and promote healthy lifestyles among the mass public. As one of the first to assess links between movement behaviors, the correlates, and anxiety symptoms among Chinese university students, our findings show the potential of using this guideline in the field of public health in China by enriching the evidence on 24 h movement behavior guidelines. Our findings also informed preventive intervention design. Chinese university students who are female and have low socioeconomic status should be prioritized as the target population for future programs encouraging optimal movement behaviors. Schools and health professionals can facilitate movement behaviors that comply with the recommendations on campus as a cost-effective solution to alleviate anxiety symptoms and promote mental health.
Notably, there may be differences in university students’ optimal movement behaviors across distinct socio-cultural backgrounds. Existing studies indicated that young people from eastern countries reported lower levels of PA [57], higher levels of SB [30], and shorter sleep duration [58, 59] than their western counterparts, especially in eastern Asian countries. This might be because of the sedentary culture induced by the intensive competition of the higher education, wherein college students have to sacrifice PA and sleep time for better academic performance [60]. Instead of precise recommendations for each behavior that adds up to 24 h, the guidelines provide ranges, which to some degree “respect the individuality, variability, and personal preferences of the end-user” across cultures [23]. However, we encourage researchers to re-evaluate the evidence, especially involving evidence generated from their own cultural contexts, to help develop and improve the optimal 24 h movement behavior composition, and not to adopt such recommendations uncritically just for “fear of missing out” [61].
Our results should be interpreted considering methodological limitations. First, due to the study’s cross-sectional nature, we cannot infer the causal relationship between meeting 24 h movement guidelines, its correlates, and anxiety symptoms. Recent research has adopted a longitudinal design to track the adherence to 24 h movement guidelines at multiple time points and detect longitudinal associations between adherence to 24 h movement guidelines and adiposity over time [62]. Additionally, a bidirectional association might exist between the adherence to the 24 h movement guidelines and mental health since recent research has found that university students who reported better mental health seem to be more likely to meet the guidelines [63]. Therefore, more longitudinal studies are warranted to examine the causality.
Second, the accuracy of data and estimation may be affected during the COVID-19 pandemic. Although our data were collected at the time when most cities in China were classified as low-risk areas, the level of movement behaviors might have been affected due to people’s cautious attitude towards going outside and the strict preventive and control measures. Moreover, recall bias and the exclusive use of self-reported data could also influence the accuracy of data. Future studies can apply device-based measures (e.g., pedometers, accelerometers, heart rate monitors) or combine them with subjective ones (e.g., diaries and questionnaires) to assess movement behaviors [64].
Third, our data was collected through convenient sampling on the online platform, which may result in the under-sampling of young adults with lower socioeconomic status [65, 66] and sex differences in response behaviors (i.e., 64% of participants were female) [67]. For future study, researchers should explore utilizing more efficient techniques (such as multilevel regression and post-stratification) to address the representativeness of online surveys [68].
Forth, although the current study accounted for potential covariates when estimating the association between anxiety symptoms and meeting 24 h movement guidelines, it is possible that the association observed may be influenced by other factors (e.g., cardiometabolic health and mental health disorders) [25]. It would have been critical to explore the complete list of the potential confounding variables. However, the quality of current evidence was not satisfactory enough for researchers to do a thorough job of measuring and controlling for potential covariates [25]. Therefore, we call for more research on the associations, especially the longitudinal associations, between sociodemographic and health factors and 24 h movement behaviors.
Fifth, it is argued that measures of the SAS should be treated as a continuous variable, which can reduce the measurement errors in the relevant studies. However, the dichotomization of SAS is also sensible in clinical and medical applications because this can classify patients according to risks, provide clinical recommendations for additional treatments, and allocate medical resources according to patient need [69]. Although the SAS defines its dichotomy based on a reliable and valid threshold, dichotomization would result in information loss and a decrease in statistical power [70]. Whether dichotomy or continuity is a more effective method is beyond the scope of this research; so we do not discuss the issue in the current study. Some studies examine the degrees of anxiety symptoms using both categorical and continuous ratings [71], which implies that future studies can consider the use of continuous variables to further explain our research findings.
Conclusion
The current study is one of the first to investigate the correlates of meeting 24 h movement guidelines and the relationship between anxiety symptoms and meeting the guidelines among Chinese university students. We observed that individuals who were male, had a better-educated mother, had more close friends, and perceived higher family affluence presented a higher probability of meeting the overall movement guidelines. Compared to meeting fewer recommendations from the 24 h movement guidelines, university students who met the overall guidelines showed the lowest incidence of anxiety symptoms. Following the recent release of the 24 h movement guidelines for adults, more longitudinal investigations should be conducted in heterogeneous adult populations to study adherence to the guidelines, their multidimensional correlates, and causal associations with health indicators.
Acknowledgements
The authors thank our participants for participating in this study. The authors appreciate intellectual contributions from Professor Zeljko Pedisic at Institute for Health and Sport Victoria University.
Abbreviations
- SB
Sedentary Behavior
- PA
Physical Activity
- VIRTUE
Framework for Viable Integrative Research in Time-Use Epidemiology
- IPAQ-SF
Physical Activity Questionnaire-Short Form
- PSQI
Pittsburgh Sleep Quality Index
- SAS
Self-rating Anxiety Scale
- BMI
Body Mass Index
- SD
Standard Deviation
- OR
Odds Ratios
- CI
Confidence Interval
Authors’ contributions
HB was a major contributor in writing the manuscript. AH, NG, LH, and KL analyzed and interpreted the data. AH and NG also contributes to writing the original draft. KK, JM, and YL reviewed and edited the manuscript. SC conceptualized and supervised the study. XC provided resources and administrated the project. All authors read and approved the final manuscript.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article from Guangdong Basic and Applied Basic Research Foundation (Project: No. 2019A1515012134 and No. 2021A1515011330).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. Study protocol and procedures were approved by the Human Research Ethics Committee of Shenzhen University (No: 2020005). The informed written consent of the participant was obtained.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ai He and Na Gong contributed equally to this work.
References
- 1.Regehr C, Glancy D, Pitts A. Interventions to reduce stress in university students: a review and meta-analysis. J Affect Disord. 2013;148(1):1–11. doi: 10.1016/j.jad.2012.11.026. [DOI] [PubMed] [Google Scholar]
- 2.Gao W, Ping S, Liu X. Gender differences in depression, anxiety, and stress among college students: a longitudinal study from China. J Affect Disord. 2020;263:292–300. doi: 10.1016/j.jad.2019.11.121. [DOI] [PubMed] [Google Scholar]
- 3.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 2013. [Google Scholar]
- 4.Wang PSD, Aguilar-Gaxiola SP, Alonso JMD, Angermeyer MCP, Borges GP, Bromet EJP, et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet. 2007;370(9590):841–850. doi: 10.1016/S0140-6736(07)61414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hou H, Feng X, Li Y, Meng Z, Guo D, Wang F, Guo Z, Zheng Y, Peng Z, Zhang W, Li D, Ding G, Wang W. Suboptimal health status and psychological symptoms among Chinese college students: a perspective of predictive, preventive and personalised health. EPMA Journal. 2018;9(4):367–377. doi: 10.1007/s13167-018-0148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lun KW, Chan CK, Ip PK, Ma SY, Tsai WW, Wong CS, et al. Depression and anxiety among university students in Hong Kong. Hong Kong Med J. 2018;24(5):466–472. doi: 10.12809/hkmj176915. [DOI] [PubMed] [Google Scholar]
- 7.Zeng Y, Wang G, Xie C, Hu X, Reinhardt JD. Prevalence and correlates of depression, anxiety and symptoms of stress in vocational college nursing students from Sichuan, China: a cross-sectional study. Psychol Health Med. 2019;24(7):798–811. doi: 10.1080/13548506.2019.1574358. [DOI] [PubMed] [Google Scholar]
- 8.Zeng W, Chen R, Wang X, Zhang Q, Deng W. Prevalence of mental health problems among medical students in China: A meta-analysis. Medicine (Baltimore) 2019;98(18):e15337. doi: 10.1097/MD.0000000000015337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shi M, Liu L, Wang ZY, Wang L. The mediating role of resilience in the relationship between big five personality and anxiety among Chinese medical students: a cross-sectional study. PLoS One. 2015;10(3):e0119916. doi: 10.1371/journal.pone.0119916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feng Q, Zhang Q, Du Y, Ye Y, He Q. Associations of physical activity, screen time with depression, anxiety and sleep quality among Chinese college freshmen. PLoS One. 2014;9(6):e100914. doi: 10.1371/journal.pone.0100914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gibb SJ, Fergusson DM, Horwood LJ. Burden of psychiatric disorder in young adulthood and life outcomes at age 30. Br J Psychiatry. 2010;197(2):122–127. doi: 10.1192/bjp.bp.109.076570. [DOI] [PubMed] [Google Scholar]
- 12.Xie D, Leong FTL. A cross-cultural study of anxiety among Chinese and Caucasian American university students. J Multicult Couns Dev. 2008;36(1):52–63. doi: 10.1002/j.2161-1912.2008.tb00069.x. [DOI] [Google Scholar]
- 13.Pires GN, Bezerra AG, Tufik S, Andersen ML. Effects of acute sleep deprivation on state anxiety levels: a systematic review and meta-analysis. Sleep Med. 2016;24:109–118. doi: 10.1016/j.sleep.2016.07.019. [DOI] [PubMed] [Google Scholar]
- 14.McDowell CP, Dishman RK, Gordon BR, Herring MP. Physical activity and anxiety: a systematic review and meta-analysis of prospective cohort studies. Am J Prev Med. 2019;57(4):545–556. doi: 10.1016/j.amepre.2019.05.012. [DOI] [PubMed] [Google Scholar]
- 15.Allen MS, Walter EE, Swann C. Sedentary behaviour and risk of anxiety: a systematic review and meta-analysis. J Affect Disord. 2019;242:5–13. doi: 10.1016/j.jad.2018.08.081. [DOI] [PubMed] [Google Scholar]
- 16.Yuan J, Liwei Z, Zhixiong M. Physical exercise affects mental health through influencing emotion regulation self-efficacy [in Chinese: 体育锻炼与心理健康:情绪调节自我效能感与情绪调节策略的作用] Studies of Psychology and Behavior. 2018;16(4):570–576. [Google Scholar]
- 17.Wu X, Tao S, Zhang Y, Zhang S, Tao F. Low physical activity and high screen time can increase the risks of mental health problems and poor sleep quality among Chinese college students. PLoS One. 2015;10(3):e0119607. doi: 10.1371/journal.pone.0119607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu S, Wing YK, Hao Y, Li W, Zhang J, Zhang B. The associations of long-time mobile phone use with sleep disturbances and mental distress in technical college students: a prospective cohort study. Sleep. 2018;42(2):1–10. [DOI] [PubMed]
- 19.Wong ML, Lau EYY, Wan JHY, Cheung SF, Hui CH, Mok DSY. The interplay between sleep and mood in predicting academic functioning, physical health and psychological health: a longitudinal study. J Psychosom Res. 2013;74(4):271–277. doi: 10.1016/j.jpsychores.2012.08.014. [DOI] [PubMed] [Google Scholar]
- 20.Pedišić Ž. Measurement issues and poor adjustments for physical activity and sleep undermine sedentary behaviour research--the focus should shift to the balance between sleep, sedentary behaviour, standing and activity. Kinesiology. 2014;46(1):135–146. [Google Scholar]
- 21.Pedišić Ž, Dumuid D, Olds TS. Integrating sleep, sedentary behaviour, and physical activity research in the emerging field of time-use epidemiology: definitions, concepts, statistical methods, theoretical framework, and future directions. Kinesiology. 2017;49(2):252–269. doi: 10.26582/k.49.2.14. [DOI] [Google Scholar]
- 22.Rollo S, Antsygina O, Tremblay MS. The whole day matters: understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J Sport Health Sci. 2020;9(6):493–510. doi: 10.1016/j.jshs.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ross R, Chaput J-P, Giangregorio LM, Janssen I, Saunders TJ, Kho ME, Poitras VJ, Tomasone JR, el-Kotob R, McLaughlin EC, Duggan M, Carrier J, Carson V, Chastin SF, Latimer-Cheung AE, Chulak-Bozzer T, Faulkner G, Flood SM, Gazendam MK, Healy GN, Katzmarzyk PT, Kennedy W, Lane KN, Lorbergs A, Maclaren K, Marr S, Powell KE, Rhodes RE, Ross-White A, Welsh F, Willumsen J, Tremblay MS. Canadian 24-hour movement guidelines for adults aged 18–64 years and adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2020;45(10):S57–S102. doi: 10.1139/apnm-2020-0467. [DOI] [PubMed] [Google Scholar]
- 24.Latimer-Cheung AE, Copeland JL, Fowles J, Zehr L, Duggan M, Tremblay MS. The Canadian 24-Hour Movement Guidelines for Children and Youth: Implications for practitioners, professionals, and organizations. Appl Physiol Nutr Metab. 2016;41(6 (Suppl. 3):S328–SS35. doi: 10.1139/apnm-2016-0086. [DOI] [PubMed] [Google Scholar]
- 25.Janssen I, Clarke AE, Carson V, Chaput J-P, Giangregorio LM, Kho ME, et al. A systematic review of compositional data analysis studies examining associations between sleep, sedentary behaviour, and physical activity with health outcomes in adults. Appl Physiol Nutr Metab. 2020;45(Suppl. 2):S248–SS57. doi: 10.1139/apnm-2020-0160. [DOI] [PubMed] [Google Scholar]
- 26.Chen S-T, Liu Y, Tremblay MS, Hong J-T, Tang Y, Cao Z-B, et al. Meeting 24-hour movement guidelines: prevalence, correlates and the relationships with overweight and obesity among Chinese children and adolescents. J Sport Health Sci. 2021;10(3):349–59. 10.1016/j.jshs.2020.07.002. [DOI] [PMC free article] [PubMed]
- 27.Lee E-Y, Spence JC, Tremblay MS, Carson V. Meeting 24-hour movement guidelines for children and youth and associations with psychological well-being among south Korean adolescents. Ment Health Phys Act. 2018;14:66–73. doi: 10.1016/j.mhpa.2018.02.001. [DOI] [Google Scholar]
- 28.Sallis JF, Owen N, Fotheringham MJ. Behavioral epidemiology: a systematic framework to classify phases of research on health promotion and disease prevention. Ann Behav Med. 2000;22(4):294–298. doi: 10.1007/BF02895665. [DOI] [PubMed] [Google Scholar]
- 29.Knell G, Durand CP, Kohl HW, 3rd, Wu IHC, Pettee GK. Prevalence and likelihood of meeting sleep, physical activity, and screen-time guidelines among US youth. JAMA Pediatr. 2019;173(4):387–389. doi: 10.1001/jamapediatrics.2018.4847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ge Y, Xin S, Luan D, Zou Z, Liu M, Bai X, Gao Q. Association of physical activity, sedentary time, and sleep duration on the health-related quality of life of college students in Northeast China. Health Qual Life Outcomes. 2019;17(1):124. doi: 10.1186/s12955-019-1194-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen X, Wang S-B, Li X-L, Huang Z-H, Tan W-Y, Lin H-C, Hou CL, Jia FJ. Relationship between sleep duration and sociodemographic characteristics, mental health and chronic diseases in individuals aged from 18 to 85 years old in Guangdong province in China: a population-based cross-sectional study. BMC Psychiatry. 2020;20(1):455. doi: 10.1186/s12888-020-02866-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pengpid S, Peltzer K, Kassean HK, Tsala Tsala JP, Sychareun V, Müller-Riemenschneider F. Physical inactivity and associated factors among university students in 23 low-, middle- and high-income countries. Int J Public Health. 2015;60(5):539–549. doi: 10.1007/s00038-015-0680-0. [DOI] [PubMed] [Google Scholar]
- 33.Macfarlane DJ, Lee CCY, Ho EYK, Chan KL, Chan DTS. Reliability and validity of the Chinese version of IPAQ (short, last 7 days) J Sci Med Sport. 2007;10(1):45–51. doi: 10.1016/j.jsams.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 34.Guo S, Sun W, Liu C, Wu S. Structural validity of the Pittsburgh Sleep Quality Index in Chinese undergraduate students. Front Psychol. 2016;7:1126. doi: 10.3389/fpsyg.2016.01126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang C, Zhao H. The Impact of COVID-19 on Anxiety in Chinese University Students. Front Psychol. 2020;11:1168. doi: 10.3389/fpsyg.2020.01168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li Y, Li G-X, Yu M-L, Liu C-L, Qu Y-T, Wu H. Association between anxiety symptoms and problematic smartphone use among Chinese university students: The mediating/moderating role of self-efficacy. Front Psych. 2021;12(164):581367. doi: 10.3389/fpsyt.2021.581367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xiang M-Q, Tan X-M, Sun J, Yang H-Y, Zhao X-P, Liu L, et al. Relationship of physical activity with anxiety and depression symptoms in chinese college students during the covid-19 outbreak. Front Psychol. 2020;11:582436. doi: 10.3389/fpsyg.2020.582436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- 39.Dunstan DA, Scott N. Assigning clinical significance and symptom severity using the zung scales: levels of misclassification arising from confusion between index and raw scores. Depress Res Treat. 2018;2018:1–13. doi: 10.1155/2018/9250972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bennie JA, Teychenne M, Tittlbach S. Muscle-strengthening exercise and depressive symptom severity among a nationally representative sample of 23,635 german adults. J Affect Disord. 2020;266:282–287. doi: 10.1016/j.jad.2020.01.172. [DOI] [PubMed] [Google Scholar]
- 41.Ostrove JM, Adler NE, Kuppermann M, Washington AE. Objective and subjective assessments of socioeconomic status and their relationship to self-rated health in an ethnically diverse sample of pregnant women. Health Psychol. 2000;19(6):613–618. doi: 10.1037/0278-6133.19.6.613. [DOI] [PubMed] [Google Scholar]
- 42.Lee E-Y, Carson V, Jeon JY, Spence JC, Tremblay MS. Levels and correlates of 24-hour movement behaviors among south Koreans: results from the Korea National Health and nutrition examination surveys, 2014 and 2015. J Sport Health Sci. 2019;8(4):376–385. doi: 10.1016/j.jshs.2018.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Khamput T, Phuangkrampun M, Sangsumritpol W, Thongbo T, Sianglee S, Kaeyai T. Thailand recommendations on physical activity, non-sedentary lifestyles, and sleeping. In: Division of Physical Activity and Health MoPH, editor. Nonthaburi 2017.
- 44.Liangruenrom N, Dumuid D, Craike M, Biddle SJH, Pedisic Z. Trends and correlates of meeting 24-hour movement guidelines: a 15-year study among 167,577 Thai adults. Int J Behav Nutr Phys Act. 2020;17(1):106. doi: 10.1186/s12966-020-01011-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cui X, Xiao J, Yi J, Porto N, Cai Y. Impact of family income in early life on the financial independence of young adults: evidence from a matched panel data. Int J Consum Stud. 2019;43(6):514–527. doi: 10.1111/ijcs.12536. [DOI] [Google Scholar]
- 46.Tandon PS, Zhou C, Sallis JF, Cain KL, Frank LD, Saelens BE. Home environment relationships with children’s physical activity, sedentary time, and screen time by socioeconomic status. Int J Behav Nutr Phys Act. 2012;9(1):88. doi: 10.1186/1479-5868-9-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yang X, Telama R, Hirvensalo M, Tammelin T, Viikari JSA, Raitakari OT. Active commuting from youth to adulthood and as a predictor of physical activity in early midlife: the young Finns study. Prev Med. 2014;59(1):5–11. doi: 10.1016/j.ypmed.2013.10.019. [DOI] [PubMed] [Google Scholar]
- 48.Guerrero MD, Barnes JD, Tremblay MS, Pulkki-Råback L. Typologies of family functioning and 24-h movement behaviors. Int J Environ Res Public Health. 2021;18(2):699. doi: 10.3390/ijerph18020699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rhodes RE, Stearns J, Berry T, Faulkner G, Latimer-Cheung AE, O’Reilly N, Tremblay MS, Vanderloo L, Spence JC. Predicting parental support and parental perceptions of child and youth movement behaviors. Psychol Sport Exerc. 2019;41:80–90. doi: 10.1016/j.psychsport.2018.11.016. [DOI] [Google Scholar]
- 50.Gupta N, Hallman DM, Dumuid D, Vij A, Rasmussen CL, Jørgensen MB, Holtermann A. Movement behavior profiles and obesity: a latent profile analysis of 24-h time-use composition among Danish workers. Int J Obes (Lond) 2020;44(2):409–417. doi: 10.1038/s41366-019-0419-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chastin SFM, Palarea-Albaladejo J, Dontje ML, Skelton DA. Combined effects of time spent in physical activity, sedentary behaviors and sleep on obesity and cardio-metabolic health markers: a novel compositional data analysis approach. PLoS One. 2015;10(10):e0139984. doi: 10.1371/journal.pone.0139984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Weatherson K, Gierc M, Patte K, Qian W, Leatherdale S, Faulkner G. Complete mental health status and associations with physical activity, screen time, and sleep in youth. Ment Health Phys Act. 2020;19:100354. doi: 10.1016/j.mhpa.2020.100354. [DOI] [Google Scholar]
- 53.Kastelic K, Pedišić Ž, Lipovac D, Kastelic N, Chen S-T, Šarabon N. Associations of meeting 24-h movement guidelines with stress and self-rated health among adults: is meeting more guidelines associated with greater benefits? BMC Public Health. 2021;21(1):929. doi: 10.1186/s12889-021-10979-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lacey BC, Lacey JI. Two-way communication between the heart and the brain: significance of time within the cardiac cycle. Am Psychol. 1978;33(2):99–113. doi: 10.1037/0003-066X.33.2.99. [DOI] [PubMed] [Google Scholar]
- 55.Edwards MK, Loprinzi PD. Experimentally increasing sedentary behavior results in increased anxiety in an active young adult population. J Affect Disord. 2016;204:166–173. doi: 10.1016/j.jad.2016.06.045. [DOI] [PubMed] [Google Scholar]
- 56.Murrough JW, Yaqubi S, Sayed S, Charney DS. Emerging drugs for the treatment of anxiety. Expert Opin Emerg Drugs. 2015;20(3):393–406. doi: 10.1517/14728214.2015.1049996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Seo D-C, Torabi MR, Jiang N, Fernandez-Rojas X, Park B-H. Correlates of college students’ physical activity: cross-cultural differences. Asia Pac J Public Health. 2009;21(4):421–432. doi: 10.1177/1010539509344112. [DOI] [PubMed] [Google Scholar]
- 58.Cheung BY, Takemura K, Ou C, Gale A, Heine SJ. Considering cross-cultural differences in sleep duration between Japanese and Canadian university students. PLoS One. 2021;16(4):e0250671. doi: 10.1371/journal.pone.0250671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Li L, Wang Y-Y, Wang S-B, Li L, Lu L, Ng CH, Ungvari GS, Chiu HFK, Hou CL, Jia FJ, Xiang YT. Sleep duration and sleep patterns in Chinese university students: a comprehensive meta-analysis. J Clin Sleep Med. 2017;13(10):1153–1162. doi: 10.5664/jcsm.6760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yu J, Bairner A. The Confucian legacy and its implications for physical education in Taiwan. Eur Phy Educ Rev. 2011;17(2):219–230. doi: 10.1177/1356336X11413169. [DOI] [Google Scholar]
- 61.Stamatakis E, Bauman AE. The bold sedentary behavior recommendations in the new Canadian guidelines: are they evidence-based? Response to "sedentary behavior research network members support new Canadian 24-hour movement guideline recommendations". J Sport Health Sci. 2020;9(6):482–484. doi: 10.1016/j.jshs.2020.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chemtob K, Reid RER, RdF G, Henderson M, Mathieu M-E, Barnett TA, et al. Adherence to the 24-hour movement guidelines and adiposity in a cohort of at risk youth: A longitudinal analysis. Pediatr Obes. 2021;16(4):e12730. doi: 10.1111/ijpo.12730. [DOI] [PubMed] [Google Scholar]
- 63.Weatherson KA, Joopally H, Wunderlich K, Kwan MYW, Tomasone JR, Faulkner G. Post-secondary students’ adherence to the Canadian 24-hour movement guidelines for adults: results from the first deployment of the Canadian campus wellbeing survey (CCWS) Health promotion and chronic disease prevention in Canada : research, policy and practice. 2021;41(6):173–181. doi: 10.24095/hpcdp.41.6.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hills AP, Mokhtar N, Byrne NM. Assessment of physical activity and energy expenditure: An overview of objective measures. Front Nutr. 2014;1:5. doi: 10.3389/fnut.2014.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hong YA, Zhou Z, Fang Y, Shi L. The digital divide and health disparities in China: evidence from a national survey and policy implications. J Med Internet Res. 2017;19(9):e317. doi: 10.2196/jmir.7786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Conn VS. Anxiety outcomes after physical activity interventions: meta-analysis findings. Nurs Res. 2010;59(3):224–231. doi: 10.1097/NNR.0b013e3181dbb2f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Smith G. Does gender influence online survey participation?: A record-linkage analysis of university faculty online survey response behavior. ERIC Document Reproduction Service No ED 501717. 2008.
- 68.Salganik MJ. Bit by bit: social research in the digital age: Princeton University press. 2019. [Google Scholar]
- 69.Segerstrom SC. Statistical guideline #1. Avoid creating categorical variables from continuous variables. Int J Behav Med. 2019;26(4):329–330. doi: 10.1007/s12529-019-09790-7. [DOI] [PubMed] [Google Scholar]
- 70.MacCallum RC, Zhang S, Preacher KJ, Rucker DD. On the practice of dichotomization of quantitative variables. Psychol Methods. 2002;7(1):19–40. doi: 10.1037/1082-989X.7.1.19. [DOI] [PubMed] [Google Scholar]
- 71.Yang H, Shi R, Chi Y, Qiao Z, Wu Y, Zhu Z, et al. Knowledge, anxiety, depression, and sleep quality among medical staff in central south areas of China during the break of COVID-19: Does the level of hospitals make a difference. Front Psych. 2021;12:714870. doi: 10.3389/fpsyt.2021.714870. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


