Abstract
Purpose of review
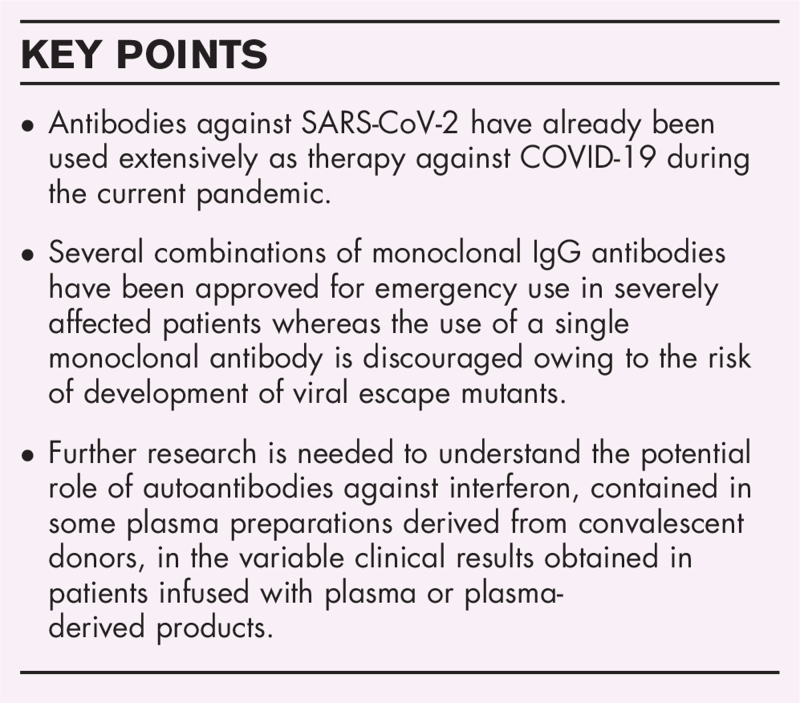
To provide an update of the current state of antibody therapy for Severe Acute Respiratory Syndrome Coronavirus 2 infection that has progressed immensely in a very short time period.
Recent findings
Limited clinical effect of classical passive immunotherapy (plasma therapy, hyperimmune immunoglobulin [IgG] preparations) whereas monoclonal antibody therapy, if initiated early in the disease process, shows promising results.
Summary
Although antibody therapy still remains to be fully explored in patients with COVID-19, a combination of IgG monoclonal antibodies against the receptor-binding domain of the spike protein currently appears to provide the best form of antibody therapy, Immunoglobulin A dimers and Immunoglobulin M pentamers also show promising preliminary therapeutic results.
Keywords: COVID-19, hyperimmunoglobulin, monoclonal antibodies, plasma therapy
INTRODUCTION
Passive immunization has, for more than a century, proven to be highly efficient for treatment and prevention of infectious diseases, particularly in individuals suffering from immunodeficiency, or individuals in whom vaccination is contraindicated. Passive immunization may thus represent a suitable therapy in global emergency situations where vaccines are lacking or where the populations at risk have not been fully vaccinated (for review see [1]).
Box 1.
no caption available
The immunoglobulin (IgG) preparations used for passive immunization are generally purified from human sera with high titers against the microorganisms (following natural infection or vaccination), either as single donations used for plasma therapy or pooled plasma but may also include human/humanized monoclonal antibodies or even sera from animals. Furthermore, the most commonly recommended form of treatment for primary immunodeficiency disorders is replacement therapy with intravenous or subcutaneous gamma globulins (IVIG or SCIG) from healthy human donors. In the past few years, a large number of broader and potent neutralizing monoclonal antibodies have also been isolated, some of which are already in clinical trials/clinical use.
Today's renewed interest in antibody therapies is the consequence of major advances in the technology of antibody development combined with the need for new therapeutic agents against emerging diseases (Ebola, ZIKA, SARS, bird flu, West Nile virus, bioterrorism agents) and new antibiotic resistant microorganisms (Staphylococcus aureus, Enterobacteriaceae, Enterococci, Clostridium difficile). Passive immunization using polyclonal or monoclonal antibody preparation may also be a potential solution for control of current or future pandemics. This review will focus on antibody-based therapies aimed at treating or mitigating infection with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2).
ANTIBODIES AGAINST SARS-CoV-2 IN COMMERCIAL STANDARD GAMMAGLOBULIN PREPARATIONS
As SARS-CoV-2 is a novel coronavirus, there is no prior immunity against this pathogen in the population. Thus, as expected, plasma collected before 2020 does not contain any specific antibodies against the virus [2], nor is there any protective crossreactivity afforded by antibodies against related coronaviruses in these plasma donations. However, starting in the autumn of 2020, the pools of plasma collected for fractionation and production of gammaglobulin preparations started to show positive antibody titers. From then on, levels of specific anti-SARS-CoV-2 antibodies have risen steadily and by the summer of 2021, the levels are expected to be at par with those seen in convalescent plasma used for treatment of patients with COVID-19 [3,4]. Owing to the quarantine requirements, there is a 6–12 months time lag before the collected plasma may be fractionated and made available for therapeutic purposes. With time, these preparations would also be expected to, depending on the geographical origin of the plasma, contain antibodies against the newly emerging virus variants and thus be suitable for prophylaxis or even therapy against SARS-CoV-2.
THE RISE AND FALL OF CONVALESCENT PLASMA THERAPY TO COMBAT SARS-CoV-2 INFECTION
Bearing in mind the historical successful use of convalescent plasma therapy in combating infections, it was early on during the pandemic being considered as a potential therapeutic option for treatment of severely ill COVID-19 patients. Plasma obtained from convalescent donors has previously been used as a therapy against Coronavirus infections, including 80 patients in Hong Kong, infected with SARS-CoV-1 during the 2003 outbreak (resulting in a reported lower mortality rate (12.5%) compared with nonplasma treated patients (17%) [5]. Similarly, Yeh et al. treated three patients with a severe clinical condition using two doses of 500 ml plasma, resulting in a rapid reduction/elimination of virus in blood and survival of the patients [6]. Antibody therapy was also suggested during the Middle East respiratory syndrome (MERS) outbreak [7] but not attempted in patients although a number of animal studies suggested a therapeutic effect of convalescent plasma, hyperimmune IgGs (from animal sources) and monoclonal antibodies.
Plasma therapy in small noncontrolled series of patients with severe SARS-CoV-2 infection [8–12] was initially reported to show beneficial effects. Some subsequent reports (a total of more than 1500 articles in PubMed using the search term plasma therapy COVID-19) also claimed therapeutic results [13,14▪,15]. However, some randomized studies have not supported the initial claims [16,17]. Recent meta-analyses, summarizing large studies with more than 10 000 patients, has concluded that there is in fact no positive effect of convalescent plasma in COVID-19 patients with severe disease [18,19▪▪,20]. The differing results suggest that factors hitherto not fully accounted for, including content and quality/class of the neutralizing anti-SARS-CoV-2 antibodies, timing of the therapy, the volume of plasma used and the content of anti-IFN antibodies in the individual plasma donations (see discussion), may have led to discrepant therapeutic results. On the other hand, growing evidence support the use of plasma therapy in immunocompromised individuals, especially those receiving B cells depleting drugs such as Rituximab [21–23]. All in all, convalescent plasma therapy is difficult to standardize and its role may be restricted to the early epidemic phase, characterized by limited therapeutic options or specific patient groups.
DEVELOPMENT OF A HYPERIMMUNE ANTIBODY PREPARATION
As titers of anti-SARS-CoV-2 antibodies may vary considerably between the plasma donors, resulting in differences in therapeutic efficacy, manufacturing of a hyperimmune IgG would allow standardization of treatment. We initially planned a project on fractionation of plasma from convalescent donors from Wuhan, China, the very center of the pandemic. This was the only region in the world where a significant number of convalescent donors was available in the early stages of the pandemic. However, collecting the required volume of plasma turned out to be an unsurmountable logistic feat owing to the local lock-down in Wuhan and our initiative was terminated. Our commercial partner, however, brought the project forward by joining forces with several other gammaglobulin producing companies (CSL Behring, Takeda, Biotest, BioPharma PlasmaGC Pharma, Octapharma, LFB and Sanquin) in an unprecedented collaborative effort. The joint group, the Plasma Alliance, managed to collect enough starting material and the resulting product, CoVIg, made it possible to design and carry out a global, multicenter, double-blind, placebo-controlled, randomized clinical trial - Inpatient Treatment with Anti-Coronavirus Immunoglobulin (ITAC) on a large number of patients, sponsored by the National Institute of Allergy and Infectious Diseases (NIAID). The study was initiated in the autumn of 2020 and the adult patients (n = 594) were all given Remdesivir and either the hyperimmune IgG preparation or placebo.
The preliminary results of this ambitious study were reported in early summer this year (News release from the Takeda company on April 2nd, 2021: CoVIg-19 Plasma Alliance Announces Topline Results from NIH-Sponsored Clinical Trial of Investigational COVID-19 Hyperimmune Globulin Medicine) and unfortunately showed no therapeutic effect of the antibodies. The full report on the trial is anticipated in the early autumn.
The immune response against SARS-CoV-2 in infected individuals follows the normal pattern with initial production of Immunoglobulin M (IgM) antibodies followed by IgG and Immunoglobulin A (IgA) with continuous affinity maturation of the antibodies where IgA may in fact dominate the early response. The titers of antibodies of the IgM and IgA diminish within a month although the latter may be present in saliva for a for a slightly longer time [24]. Levels of IgG remain for a markedly extended period [25,26] as is also the case with antibodies against other Coronaviruses including SARS-CoV and MERS [27]. Although the IgG antibodies may persist for many years, it remains to be shown how long the protective anti SARS-CoV-2 response will ultimately last.
THE USE OF MONOCLONAL ANTIBODIES FOR THERAPY AGAINST SARS-CoV-2
The early antibody response is dominated by IgA (of the IgA1 subclass), which appears before IgG and contributes to a greater extent to the virus neutralization at mucosal sites in the initial stages of infection [24]. The superiority of the monomeric IgA molecule as compared to IgG may be due to its increased flexibility and its longer hinge region, allowing a more favorable spatial interaction with the spike protein. Dimeric IgA, the molecular form at mucosal surfaces, was subsequently shown to be more potent than the monomeric form both in terms of binding and neutralizing capacity [28▪▪]. Finally, a genetically engineered monoclonal antibody with a Fv portion of an IgG antibody was grafted into human IgM and IgA scaffolds where the IgM was expressed as a pentamer and the IgA1 as a dimer. Again, the dimeric IgA molecule showed superior activity as compared to its IgG parent antibody but the IgM was vastly more effective in terms of binding and neutralization and showed a potent prophylactic and therapeutic effect when applied intranasally in mice [29]. Yet another alternative that has received attention for the past years is the use of camelid Variable region of heavy chain only antibodies (nanobodies9 from camelids) (VHH) fragments (nanobodies) which may recognize epitopes that are often inaccessible to conventional antibodies. Thus, Xu et al. isolated anti-RBD nanobodies from alpacas, dromedaries and camels, some of which targeted a highly conserved epitope in coronaviruses, rarely recognized by human antibodies, and one set of nanobodies which was highly neutralizing even against recently emerging virus variants when expressed as a homotrimer [30▪]. The above observations may have a profound impact on the choice of antibody class/molecular form of monoclonal antibodies for human therapy.
Several monoclonal antibodies against SARS-CoV-2 have been developed, following the successful production of human/humanized monoclonal antibodies against other recently emerging infections, including Zika [31,32] and Ebola [33,34]. Some of the monoclonal antibodies previously raised against SARS-CoV-1 have shown cross-reactivity against SARS-CoV-2 [35] and a large number of novel monoclonal antibodies, mainly of the IgG class, against the new virus have also been generated with an astonishing speed and are continuously being added to the therapeutic arsenal (for review see [36▪▪]).
Three monoclonal antibody preparations against SARS-CoV-2 are currently available for treatment of patients with mild-to-moderate COVID-19 infections. Bamlanivimab (LY-CoV555) from Eli Lilly was initially used as a monotherapy in 452 patients as a single infusion in three different doses [37▪] where the rate of emergency visit or hospitalization was reduced from 6.3% in the placebo group to 1.6% in the combined treatment group. However, owing partly to the risk for emergence of viral escape mutants, etesivimab was later added to the product (2800 mg of each monoclonal antibody) and tested in 1035 infected adults [38▪] with 518 receiving a single infusion of the combination of monoclonal antibodies. These two antibodies bind to different but overlapping sites on the spike protein of the virus and resulted in a reduction in COVID-19 related hospitalization or death from 7% to 2% where all the deaths occurred in the placebo group.
Two other monoclonal IgG antibodies, casirivimab and imdevimab, developed by Regeneron and targeting nonoverlapping epitopes in the receptor-binding domain of the spike protein have also been used successfully in clinical trials. The use of an equal mixture of the antibodies was made to reduce the risk for development of escape mutants. A preliminary report on 275 nonhospitalized patients [39▪] showed a decreased viral load from baseline through day 7 after treatment with a greater effect in patients who were seronegative at the start of therapy, i.e., in the very early stages of infection. Subsequently, a study based on 9785 patients hospitalized with COVID-19 was reported recently [40] using a single dose of 8 g of antibodies (4 g of each) where the primary outcome was 28-day mortality. In the population of seronegative patients, 396 (24%) of the treated patients died whereas 451 (30%) of the patients receiving usual care died within the 28 days period (P = 0.001). In an analysis involving all randomized patients (regardless of baseline antibody status), no difference in mortality between the groups was observed, again emphasizing the crucial importance of early initiation of treatment.
On May 26, 2021, yet another anti-SARS-CoV-2 monoclonal IgG antibody, sotrovimab, originally isolated from a SARS infected patient in 2003, received FDA emergency use authorization based on an unpublished study on 291 patients with a reduced rate of hospitalization or death compared to placebo (1% as compared to 7%).
All anti-SARS-CoV-2 monoclonal antibodies previously or currently authorized for clinical use are restricted to patients with mild or moderate disease who are at a high risk for progression to severe COVID-19, thus limiting their clinical utility. Patients with a severe disease do not benefit from treatment with the above monoclonal antibodies that emphasize the notion that antibody-based therapy should be initiated early in the infectious process. This also has implications for potential treatment of immunocompromised patients with persistent SARS-CoV-2 infections.
It is apparent that monotherapy with monoclonal anti-SARS-CoV-2 antibodies is associated with a high risk for the appearance of viral escape mutants and the emergency use authorization for treatment with bamlanivimab was revoked by the U.S. FDA in April 2021. Meanwhile, the emergence of multiple SARS-CoV-2 variants-of-concern (VOCs) with mutations in the spike Receptor binding domain (RBD) an challenging the neutralizing serum-activity have been reported.
Thus, a cocktail of two separate antibodies is strongly preferred. One alternative approach was recently published [41▪▪] where a bispecific antibody, formed by two human IgG monoclonal antibodies which bind to independent sites on the RBD of the spike protein. This bispecific antibody protects SARS-CoV-2 infected mice from disease and suppressed viral escape and combines the advantages of antibody cocktails with those of single molecule approaches.
This part of our review has focused on antibodies against the SARS-CoV-2 virus itself and it should be recognized that many additional therapeutic monoclonal antibodies have also been developed that target molecules involved in the regulation of the immune response or proinflammatory cytokines contributing to the progress of the disease.
DISCUSSION
Passive immunotherapy is a century old treatment modality that has been successfully used both for oral and systemic administration against bacterial and viral infections. It is therefore somewhat surprising that therapy against SARS-CoV-2 using convalescent plasma and hyper IgG has largely failed, in spite of massive efforts. A contributing factor could be the varying titers of neutralizing antibodies in the individual convalescent plasma donations. However, the latter would not apply to the CoVIg hyperimmune preparation used in the ITAC study, suggesting that other factors such as timing of the start of treatment, may underly the encountered treatment failures.
Patients infected with SARS-CoV-2 develop a wide variety of autoantibodies including type I Interferons, mainly but not limited to IFNα and IFNw [42▪▪], Angiotensin converting enzyme 2 [43], chemokines and complement components [44▪▪]. In some cases, the antiinterferon antibodies have been shown to be present before the infection and associated with a high mortality rate [42▪▪]. In view of the critical importance of Interferons in combating the infection, as shown by the high risk for severe disease in patients with Inborn Errors of Immunity involving the interferon system [45], it is possible that the presence of these autoantibodies in some of the plasma donations contain antiinterferon antibodies which, when infused, will inhibit endogenous interferon production in the patient and thus influence the clinical outcome.
Only a small proportion of patients with mild or moderate SARS-CoV-2 infection will progress to severe disease and thus, although large numbers of patients have been enrolled in the clinical trials to date, the number of infected individuals who benefit from the treatment is rather low. The key is to identify markers (genetic or biochemical) that would rapidly predict the risk for progressive disease in the individual patient in order to avoid excessive treatment costs, an important issue in low-or-middle income countries. Vaccination would probably be a more cost-effective regime but until sufficient coverage in the general population has been reached, monoclonal antibodies will still provide an important therapeutic tool, particularly in patients failing vaccination because of inborn errors of immunity or iatrogenically immunocompromised individuals.
CONCLUSION
Passive immunization using preformed antibodies is a more than a century old therapeutic method for selected infectious diseases. Various approaches, including plasma therapy, hyper IgG and monoclonal antibodies have been used to try to combat the COVID-19 pandemic. The former two methods have achieved limited positive clinical results whereas combinations of monoclonal antibodies show clinical efficacy if administered early in the disease process. Future research within this field should thus be aimed at trying to optimize the composition of the antibody preparations.
Acknowledgements
None.
Financial support and sponsorship
This work was supported by the Swedish Research Council and the European Union's Horizon 2020 research and innovation program (grant no 101003650, ATAC).
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Hammarström L, Abolhassani H, Baldanti F, et al. Development of passive immunity against SARS-CoV-2 for management of immunodeficient patients-a perspective. J Allergy Clin Immunol 2020; 146:58–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schwaiger J, Karbiener M, Aberham C, et al. No SARS-CoV-2 neutralization by intravenous immunoglobulins produced from plasma collected before the 2020 pandemic. J Infect Dis 2020; 222:1960–1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fante CD, Franchini M, Baldanti F, et al. A retrospective study assessing the characteristics of COVID-19 convalescent plasma donors and donations. Transfusion 2021; 61:830–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Farcet MR, Karbiener M, Schwaiger J, et al. Rapidly Increasing SARS-CoV-2 neutralization by intravenous immunoglobulins produced from plasma collected during the 2020 pandemic. J Inf Dis 2021; https://doi-org.proxy.kib.ki.se/10.1093/infdis/jiab142https://doi-org.proxy.kib.ki.se/10.1093/infdis/jiab142. [Online ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng Y, Wong R, Soo YOY, et al. Use of convalescent plasma therapy in SARS patients in Hong Kong. Eur J Clin Microbiol Infect Dis 2005; 24:44–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yeh K-M, Chiueh T-S, Siu LK, et al. Experience of using convalescent plasma for severe acute respiratory syndrome among healthcare workers in a Taiwan hospital. J Antimicrob Chemother 2005; 56:919–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arabi YM, Hajeer AH, Luke T, et al. Feasibility of using convalescent plasma immunotherapy for MERS-CoV Infection, Saudi Arabia. Emerg Infect Dis 2016; 22:1554–1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shen C, Wang Z, Zhao F, et al. Treatment of 5 critically ill patients with COVID-19 with convalescent plasma. JAMA 2020; 323:1582–1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang B, Liu S, Tan T, et al. Treatment with convalescent plasma for critically ill patients with severe acute respiratory syndrome coronavirus 2 infection. Chest 2020; 158:e9–e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duan K, Liu B, Li C, et al. Effectiveness of convalescent plasma therapy in severe COVID-19 patients. PNAS 2020; 117:9490–9496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li L, Zhang W, Hu Y, et al. Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial. JAMA 2020; 324:460–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perotti C, Baldanti F, Bruno R, et al. Mortality reduction in 46 severe Covid-19 patients treated with hyperimmune plasma. A proof of concept single arm multicenter trial. Haematologica 2020; 105:2834–2840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abolghasemi H, Eshghi P, Cheraghali AM, et al. Clinical efficacy of convalescent plasma for treatment of COVID-19 infections: results of a multicenter clinical study. Transfus Apher Sci 2020; 59:102875.doi: 10.1016/j.transci.2020.102875. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14▪.Libster R, Pérez Marc G, Wappner D, et al. Early high-titer plasma therapy to prevent severe covid-19 in older adults. N Engl J Med 2021; 384:610–618. [DOI] [PMC free article] [PubMed] [Google Scholar]; One of the early papers suggesting that early treatment with plasma reduced the porgression of COVID-19 in adults with mild symptoms.
- 15.Salazar E, Christensen PA, Graviss EA, et al. Significantly decreased mortality in a large cohort of coronavirus disease 2019 (COVID-19) patients transfused early with convalescent plasma containing high-titer anti-severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Spike Protein IgG. Am J Pathol 2021; 191:90–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agarwal A, Mukherjee A, Kumar G, et al. Convalescent plasma in the management of moderate covid-19 in adults in India: open label phase II multicentre randomised controlled trial (PLACID Trial). BMJ 2020; 371:m3939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simonovich VA, Pratx LDB, Scibona P, et al. A randomized trial of convalescent plasma in covid-19 severe pneumonia. N Engl J Med 2020; 384:619–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu STH, Aberg JA. Convalescent plasma in patients hospitalised with COVID-19. Lancet 2021; 397:2024–2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19▪▪.Janiaud P, Axfors C, Schmitt AM, et al. Association of convalescent plasma treatment with clinical outcomes in patients with COVID-19: a systematic review and meta-analysis. JAMA 2021; 325:1185–1195. [DOI] [PMC free article] [PubMed] [Google Scholar]; A systematic review of treatment with convalescent plasma in patients with COVID-19. The study showed that as compared to placebo or standard of care, convalescent plasma therapy was not significantly associated with a decrease in all-cause mortality or any benefit for other clinical outcomes.
- 20.Piechotta V, Chai KL, Valk SJ, et al. Convalescent plasma or hyperimmune immunoglobulin for people with COVID-19: a living systematic review. Cochrane Database Syst Rev 2020; 7:CD013600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ferrari S, Caprioli C, Weber A, et al. Convalescent hyperimmune plasma for chemo-immunotherapy induced immunodeficiency in COVID-19 patients with hematological malignancies. Leuk Lymphoma 2021; 62:1490–1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McKemey E, Shields AM, Faustini SE, et al. Resolution of persistent COVID-19 after convalescent plasma in a patient with B cell aplasia. J Clin Immunol 2021; 41:926–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hueso T, Pouderoux C, Péré H, et al. Convalescent plasma therapy for B-cell-depleted patients with protracted COVID-19. Blood 2020; 136:2290–2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sterlin D, Mathian A, Miyara M, et al. IgA dominates the early neutralizing antibody response to SARS-CoV-2. Sci Transl Med 2021; 13:eabd2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sherina N, Piralla A, Du L, et al. Persistence of SARS-CoV-2-specific B and T cell responses in convalescent COVID-19 patients 6–8 months after the infection. Med 2021; 2:281–295. e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cassaniti I, Percivalle E, Bergami F, et al. SARS-CoV-2 specific T-cell immunity in COVID-19 convalescent patients and unexposed controls measured by ex vivo ELISpot assay. Clin Microbiol Inf 2021; 27:1029–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murchu EO, Byrne P, Walsh KA, et al. Immune response following infection with SARS-CoV-2 and other coronaviruses: a rapid review. Rev Med Virol 2021; 31:e2162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28▪▪.Wang Z, Lorenzi JCC, Muecksch F, et al. Enhanced SARS-CoV-2 neutralization by dimeric IgA. Sci Transl Med 2021; 13:eabf1555. [DOI] [PMC free article] [PubMed] [Google Scholar]; A study showing that plasma IgA monomers specific for SARS-CoV-2 proteins were two-fold lesspotent than IgG equivalents whereas dimeric IgA were on average fifteen times more potent than the IgA monomers against the same target. Thus, dimeric IgA may be particularly valuable for protection against the virus.
- 29.Ku Z, Xie X, Hinton PR, et al. Nasal delivery of an IgM offers broad protection from SARS-CoV-2 variants. Nature 2021; 595:718–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30▪.Xu J, Xu K, Jung S, et al. Nanobodies from camelid mice and llamas neutralize SARS-CoV-2 variants. Nature 2021; 595:278–282. [DOI] [PMC free article] [PubMed] [Google Scholar]; The study shows the efficacy of yet another form of antibodies, nanobodies from llamas, which may recognize epitopes normally not accesible to conventional antibodies, when multimerized, shows strong binding to the virus and may thus represent a promising therapeutic tool.
- 31.Dussupt V, Sankhala RS, Gromowski GD, et al. Potent Zika and dengue cross-neutralizing antibodies induced by Zika vaccination in a dengue-experienced donor. Nat Med 2020; 26:228–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rompay KKAV, Coffey LL, Kapoor T, et al. A combination of two human monoclonal antibodies limits fetal damage by Zika virus in macaques. PNAS 2020; 117:7981–7989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mulangu S, Dodd LE, Richard T, Davey J, et al. A randomized, controlled trial of ebola virus disease therapeutics. N Engl J Med 2019; 381:2293–2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Markham A. REGN-EB3: first approval. Drugs 2021; 81:175–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tian X, Li C, Huang A, et al. Potent binding of 2019 novel coronavirus spike protein by a SARS coronavirus-specific human monoclonal antibody. Emerg Microbes Infect 2020; 9:382–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36▪▪.Taylor PC, Adams AC, Hufford MM, et al. Neutralizing monoclonal antibodies for treatment of COVID-19. Nat Rev Immunol 2021; 21:382–393. [DOI] [PMC free article] [PubMed] [Google Scholar]; A comprehensive review on existing monoclonal antibodies for treatment of COVID-19. The review covers aspects on passive immunity during history and lessons learned from using antibody therapies for viral infections, including up-to-date results with the monoclonal antibodies against SARS-CoV-2 authorized for emergency use.
- 37▪.Chen P, Nirula A, Heller B, et al. SARS-CoV-2 neutralizing antibody LY-CoV555 in outpatients with Covid-19. N Engl J Med 2021; 384:229–237. [DOI] [PMC free article] [PubMed] [Google Scholar]; An interim analysis of the clinical efficacy of the monoclonal antibody LY-CoV555 in outpatients with COVID-19 showing a dose-dependent decline in viral load over time.
- 38▪.Gottlieb RL, Nirula A, Chen P, et al. Effect of bamlanivimab as monotherapy or in combination with etesevimab on viral load in patients with mild to moderate COVID-19: a randomized clinical trial. JAMA 2021; 325:632–644. [DOI] [PMC free article] [PubMed] [Google Scholar]; A follow-up of the previous study (ref 33 above), where the effect of the monoclonal antibody (bamlanivimab used as monotherapy or in combination with another monoclonal antibody (etesivimab) in patients with mild to moderate COVID-19 showed reduction in viral load.
- 39▪.Weinreich DM, Sivapalasingam S, Norton T, et al. REGN-COV2, a neutralizing antibody cocktail, in outpatients with Covid-19. N Engl J Med 2021; 384:238–251. [DOI] [PMC free article] [PubMed] [Google Scholar]; The study employed a mixture of two different monoclonal human IgG antibodies (REGN-COV2) in outpatients with COVID-19, showing a reduction in viral load in patients who were treated early after infection (still being anti-SARS-CoV-2 antibody negative).
- 40.Group TRC, Horby PW, Estcourt L, et al. Convalescent plasma in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet 2021; 397:2049–2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41▪▪.De Gasparo R, Pedotti M, Simonelli L, et al. Bispecific IgG neutralizes SARS-CoV-2 variants and prevents escape in mice. Nature 2021; 593:424–428. [DOI] [PubMed] [Google Scholar]; A study using a bi-specific IgG antibody (CoV-X2) targeting two different epitopes on the receptor binding domain of the SARS-CoV-2 spike protein. The molecule neutralizes the virus both in vitro and in a mouse model and prevents the appearance of viral escape mutants. The simultaneous targeting of nonoverlapping epitopes combines the advantages of antibody coctails with those of single molecule approaches.
- 42▪▪.Bastard P, Rosen LB, Zhang Q, et al. Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science 2020; 370:eabd4585. [DOI] [PMC free article] [PubMed] [Google Scholar]; A seminal paper showing the presence of antibodies against type I interferon antibodies in patients with severe COVID-19. These antibodies against multiple interferons constitute a strong risk factor for life-threatening disease and accounts for 10% of all fatalities by neutralizing the interferon response needed to combat the infection.
- 43.Casciola-Rosen L, Thiemann DR, Andrade F, et al. IgM autoantibodies recognizing ACE2 are associated with severe COVID-19. medRxiv 2020; 2020.10.13.20211664. [Google Scholar]
- 44▪▪.Wang EY, Mao T, Klein J, et al. Diverse functional autoantibodies in patients with COVID-19. Nature 2021; 595:283–288. [DOI] [PubMed] [Google Scholar]; A paper showing the presence of a variety of autoantibodies in patients with COVID-19. By examining the profile against 2770 extracellular proteins, the authors identified autoantibodies against a large number of immunomodulatory proteins including cytokines, chemochines, complement components and cell surface proteins, perurbing immune function and impairing virological control.
- 45.Zhang Q, Bastard P, Liu Z, et al. Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science 2020; 370:eabd4570. [DOI] [PMC free article] [PubMed] [Google Scholar]