Abstract
BACKGROUND
Lung cancer is made up of distinct subtypes, including non–small-cell lung cancer (NSCLC) and small-cell lung cancer (SCLC). Although overall mortality from lung cancer has been declining in the United States, little is known about mortality trends according to cancer subtype at the population level because death certificates do not record subtype information.
METHODS
Using data from Surveillance, Epidemiology, and End Results (SEER) areas, we assessed lung-cancer mortality and linked deaths from lung cancer to incident cases in SEER cancer registries. This allowed us to evaluate population-level mortality trends attributed to specific subtypes (incidence-based mortality). We also evaluated lung-cancer incidence and survival according to cancer subtype, sex, and calendar year. Joinpoint software was used to assess changes in incidence and trends in incidence-based mortality.
RESULTS
Mortality from NSCLC decreased even faster than the incidence of this subtype, and this decrease was associated with a substantial improvement in survival over time that corresponded to the timing of approval of targeted therapy. Among men, incidence-based mortality from NSCLC decreased 6.3% annually from 2013 through 2016, whereas the incidence decreased 3.1% annually from 2008 through 2016. Corresponding lung cancer–specific survival improved from 26% among men with NSCLC that was diagnosed in 2001 to 35% among those in whom it was diagnosed in 2014. This improvement in survival was found across all races and ethnic groups. Similar patterns were found among women with NSCLC. In contrast, mortality from SCLC declined almost entirely as a result of declining incidence, with no improvement in survival. This result correlates with limited treatment advances for SCLC in the time frame we examined.
CONCLUSIONS
Population-level mortality from NSCLC in the United States fell sharply from 2013 to 2016, and survival after diagnosis improved substantially. Our analysis suggests that a reduction in incidence along with treatment advances — particularly approvals for and use of targeted therapies — is likely to explain the reduction in mortality observed during this period.
Lung cancer is made up of a group of molecularly and histologically heterogeneous subtypes.1 Two major histologic subtypes are non–small-cell lung cancer (NSCLC) and small-cell lung cancer (SCLC), which account for 76% and 13%, respectively, of all cases of lung cancer in the United States.2 Although incidence trends for these subtypes have been well described,3-5 less is known about their respective mortality trends. It is important to assess trends in mortality from lung cancer according to subtype because the potential adoption of lung-cancer screening coupled with reductions in smoking are likely to influence future mortality from lung cancer differentially according to histologic subtype.6-8 Furthermore, major improvements have been made in NSCLC treatment with the advent of targeted therapies and immunotherapies. The presence of an oncogenic driver mutation — in the genes encoding anaplastic lymphoma kinase (ALK) or epidermal growth factor receptor (EGFR), for example — renders a tumor sensitive to targeted tyrosine kinase inhibition. On the basis of the success of these tyrosine kinase inhibitors in selected patients, the National Comprehensive Cancer Network recommended in 2012 that all patients with nonsquamous NSCLC undergo genetic testing for EGFR mutations and ALK rearrangements. Although these systemic therapies are palliative (i.e., unable to render cure), advancements in identifying and treating cancers that have phenotypes that depend on these oncogenes, coupled with Food and Drug Administration (FDA) approval of effective immune-based therapies in 2015, could contribute to population-level improvement in NSCLC cancer-specific survival.9
In comparison, treatments for SCLC have shown limited improvements in efficacy in the time frame of the data presented. Indirect support for the hypothesis that advances in treatment for NSCLC may have been associated with improved lung-cancer outcomes can be gleaned from the Annual Report to the Nation on the Status of Cancer.10 The report documents that U.S. mortality from cancer of the lung and bronchus is decreasing faster than the incidence (for men, a −2.6% mean annual change in incidence from 2011 through 2015, as compared with a −4.3% mean annual change in mortality from 2012 through 2016; for women, a −1.2% mean annual change in incidence and −3.1% mean annual change in mortality during these same periods).
However, to understand lung-cancer mortality trends and the effect of preventive interventions as compared with treatment interventions, it is important to assess the individual contributions of NSCLC and SCLC to overall lung-cancer incidence and mortality trends in the United States. National data on causes of death reported on death certificates make it possible to assess mortality trends for lung cancer overall. As noted, overall mortality from lung cancer has been decreasing among men and women.2 However, this overall trend cannot be separated directly into subtype-specific trends, because death certificates do not record the cancer subtype.
To address this data limitation, the U.S. Surveillance, Epidemiology, and End Results (SEER) Program has linked mortality records to incident cancer cases. Consequently, it is possible to calculate “incidence-based mortality,” which captures the population-level mortality attributable to particular tumor types reported to SEER registries.11 The numerator in the calculation of incidence-based mortality is the number of cancer-specific deaths among persons with a particular cancer diagnosis reported to the registry. The denominator is the general population at risk at the time of death in the SEER areas. This approach enables general population mortality to be partitioned according to characteristics that are associated with the cancer diagnosis (e.g., tumor subtype or stage at diagnosis) and recorded in the SEER registries. This incidence-based method of estimating mortality has been used to assess the effect of screening, and to a lesser extent the effect of treatment, on mortality trends for several cancer types.12-19
In this study, we applied the incidence-based mortality method to SEER data to evaluate population-level U.S. mortality trends, according to sex, attributable to NSCLC and SCLC from 2001 through 2016. Since mortality captures the combined effects of lung-cancer incidence and survival after diagnosis, we also assessed the contributions of lung-cancer incidence and lung-cancer–specific survival to these trends.
METHODS
STUDY DATA
We identified patients with invasive lung and bronchus cancer from the SEER 18-registry database, which covers 28% of the U.S. population. The SCLC and NSCLC subtypes were defined according to the classification system of Lewis et al.,3 in which histologic groupings were created on the basis of International Classification of Diseases for Oncology, 3rd Edition (ICD-O-3), morphology codes. We used 2001 as the first year in the analysis period because NSCLC was reliably identified only beginning in 2001, as a result of evolving clinical practice, diagnostic methods, and classification.5 Patients with cancer that was diagnosed by death certificate or autopsy were excluded because subtype information was unavailable for these patients (resulting in the exclusion of 1.4% of patients with lung cancer overall). Lung-cancer incidence from 2001 through 2016 was calculated after accounting for reporting delay.20
Causes of death were ascertained from death certificates obtained by the National Center for Health Statistics.21 The registries routinely link their incidence data with the death-certificate data, using state death records and the National Death Index to ascertain deaths and update information on the date and cause of death. Since the National Death Index is a national database, if a patient with cancer moves out of the SEER catchment area and dies elsewhere, the corresponding cause-of-death information can still be used to determine when and where the patient died. We report mortality based on deaths from all lung cancers. For incidence-based mortality, we used linked SEER data on patients with lung cancer to classify these deaths from lung cancer according to histologic subtype (details are provided in the Supplementary Appendix, available with the full text of this article at NEJM.org).
STATISTICAL ANALYSIS
We report incidence-based mortality and incidence according to calendar year, sex, and subtype. We used Joinpoint software, version 4.7.0.0, to characterize piecewise log-linear time calendar trends in the age-standardized rates by sex and cancer subtype22,23 (details are provided in the Supplementary Appendix). Finally, we provide estimates of 2-year relative survival among patients with lung cancer according to sex, subtype, and calendar year, using the relative survival approach.24
RESULTS
DETERMINATION OF MORTALITY FROM LUNG CANCER
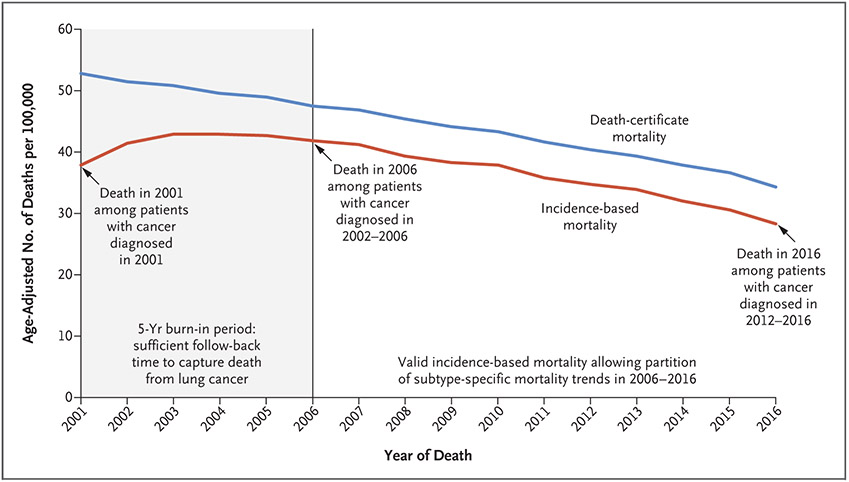
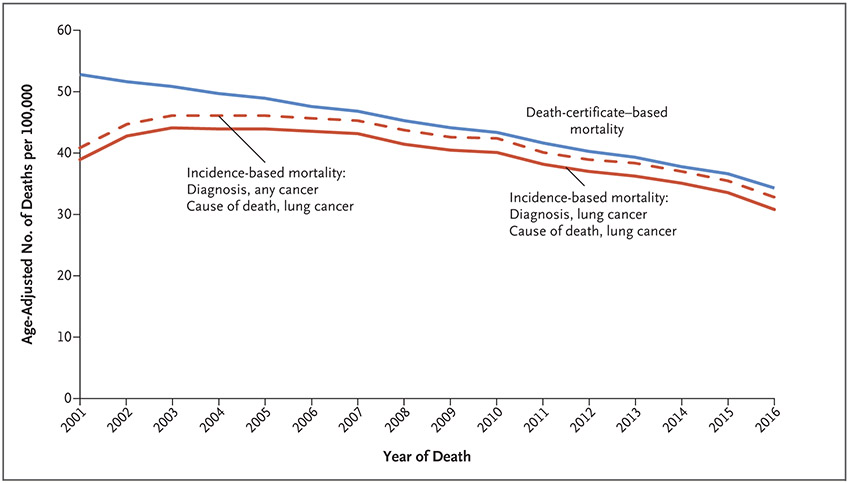
Mortality from lung cancer appeared to be higher when estimated on the basis of National Center for Health Statistics death-certificate mortality records than when we used the incidence-based mortality approach (Fig. 1). Given that the lungs are a common site of metastasis for other cancers at diagnosis, misattribution or overattribution of deaths to lung cancer is possible in the death-certificate data. In fact, using the incidence-based mortality approach, we identified a number of lung-cancer deaths linked to non–lung-cancer diagnoses in SEER (Fig. 2), indicating overattribution of deaths to lung cancer in death certificates. For example, 15,866 deaths from lung cancer in the National Center for Health Statistics database did not link to a lung-cancer diagnosis, instead being matched to a non–lung-cancer diagnosis in SEER (Fig. 2). Of these 15,866 deaths from lung cancer, 11,078 (approximately 70%) were linked to persons with only one primary diagnosis that was not a lung-cancer diagnosis, clearly indicating misattribution. This observation suggests that mortality from lung cancer may be lower than currently reported and may be captured more accurately with the incidence-based mortality approach than with National Center for Health Statistics death-certificate data.
Figure 1. Mortality Estimates Based on Data from Death Certificates and on Incidence among Patients with Lung or Bronchus Cancer.
Shown are the estimates of mortality from lung and bronchus cancer based on data from death certificates (blue line) and the corresponding estimates of mortality based on incidence (red line). In the area to the left of the vertical line at calendar year 2006, the incidence-based mortality underestimates mortality from lung cancer. Results are shown for the Surveillance, Epidemiology, and End Results (SEER) 18-registry database, which includes the following registries: San Francisco, Connecticut, Detroit, Hawaii, Iowa, New Mexico, Seattle, Utah, Atlanta, San Jose–Monterey, Los Angeles, Alaska Native, Rural Georgia, California (excluding San Francisco, San Jose–Monterey, and Los Angeles), Kentucky, Louisiana, New Jersey, and Georgia (excluding Atlanta and Rural Georgia). For both measures of mortality, attribution to lung-cancer death is made when the cause of death on the death certificate is stated as lung and bronchus cancer (International Classification of Diseases, 10th Revision, code C34).
Figure 2. Comparison of Mortality Estimates Based on Data from Death Certificates and on Two Measures of Incidence among Patients with Lung or Bronchus Cancer.
Shown are the estimates of mortality from lung and bronchus cancer determined on the basis of data from death certificates (blue line) and the corresponding incidence-based mortality from lung or bronchus cancer that was linked to patients with a diagnosis of lung cancer (solid red line) or to patients with any cancer diagnosis (i.e., not limited to a lung-cancer diagnosis) (dashed red line). Mortality from lung cancer may be more accurately represented with the incidence-based approach than with the approach based on death-certificate data. Results are shown for the SEER 18-registry database.
TRENDS IN MORTALITY FROM LUNG CANCER
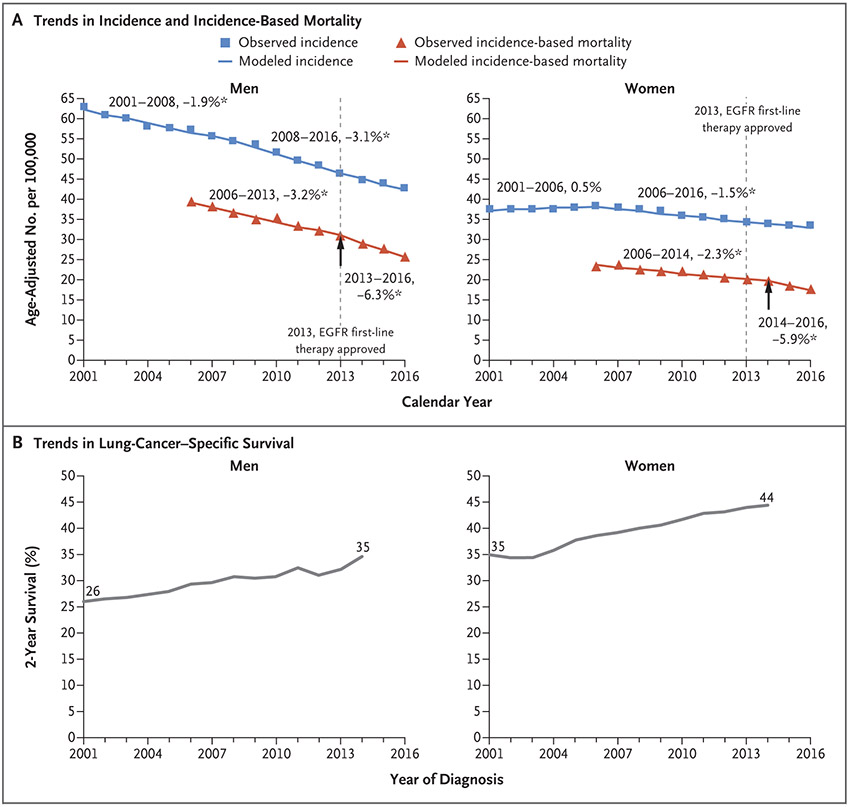
Figure 3 shows the results for NSCLC separately for men and women. Among men (Fig. 3A, left), the incidence of NSCLC decreased gradually, by 1.9% annually (95% confidence interval [CI], 1.6 to 2.2) from 2001 through 2008 and then more steeply, by 3.1% annually (95% CI, 2.8 to 3.3), from 2008 through 2016. Incidence-based mortality decreased by 3.2% annually (95% CI, 2.5 to 4.0) from 2006 through 2013, then decreased more quickly, by 6.3% annually (95% CI, 3.4 to 9.0), from 2013 through 2016. The 2-year relative survival among patients with lung cancer improved substantially (Fig. 3B), from 26% among men with NSCLC diagnosed in 2001 to 35% among those with NSCLC diagnosed in 2014.
Figure 3. Non–Small-Cell Lung-Cancer (NSCLC) Incidence, Incidence-Based Mortality, and Survival Trends among Men and Women.
Panel A shows age-adjusted incidence (blue) and incidence-based mortality (red) for the NSCLC histologic subtype among men and women. Incidence was adjusted for reporting delays. The line segments of each curve were selected with the Joinpoint program, and the percentage associated with each line represents the annual percentage change during the indicated range of years. Asterisks indicate annual percentage changes that are significantly different from zero (P<0.05). The dashed vertical line indicates calendar year 2013, when epidermal growth factor receptor (EGFR)–directed first-line therapy was approved by the Food and Drug Administration (FDA). For each incidence-based mortality curve, an arrow indicates the point at which there is a change in slope for mortality corresponding with the timing of routine testing for molecular alterations in EGFR and FDA approval for targeted therapy. Panel B shows 2-year lung-cancer–specific survival according to year of NSCLC diagnosis among men and women. Results are shown for the SEER 18-registry database. The following International Classification of Diseases for Oncology, 3rd Edition (ICD-O-3), histology codes were used to define the NSCLC subtype — squamous and transitional cell: 8051, 8052, 8070–8076, 8078, 8083, 8084, 8090, 8094, 8120, and 8123; adenocarcinoma: 8015, 8050, 8140, 8141, 8143–8145, 8147, 8190, 8201, 8211, 8250–8255, 8260, 8290, 8310, 8320, 8323, 8333, 8401, 8440, 8470, 8471, 8480, 8481, 8490, 8503, 8507, 8550, 8570–8572, 8574, and 8576; large cell: 8012–8014, 8021, 8034, and 8082; non–small-cell carcinoma, not otherwise specified: 8046; and other specified carcinomas: 8003, 8004, 8022, 8030, 8031–8033, 8035, 8200, 8240, 8241, 8243–8246, 8249, 8430, 8525, 8560, 8562, and 8575.
Among women (Fig. 3A, right), the NSCLC incidence was flat from 2001 through 2006 and then started decreasing by 1.5% annually (95% CI, 1.3 to 1.7) from 2006 through 2016. In contrast, incidence-based mortality decreased slowly, by 2.3% annually (95% CI, 1.8 to 2.8), from 2006 through 2014 and then at a faster rate of 5.9% annually (95% CI, 1.3 to 10.2) from 2014 through 2016.
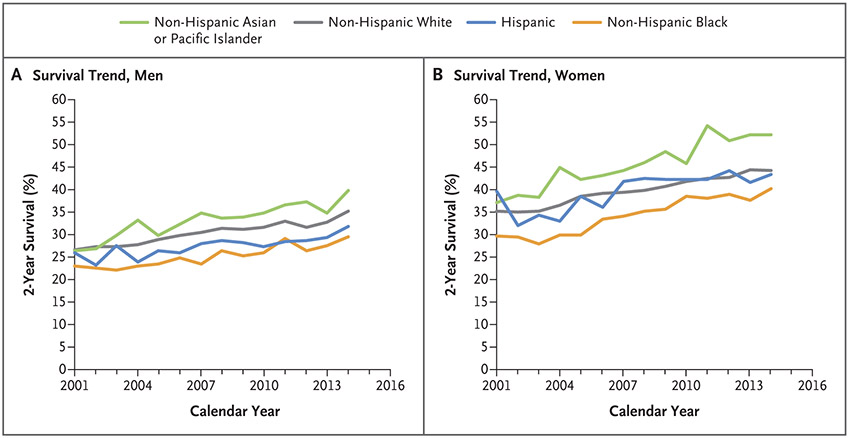
This greater reduction in mortality than in incidence during the more recent period translates into an estimated 6800 deaths from lung cancer among men and 3200 deaths from lung cancer among women that may have been delayed in the United States from 2014 through 2016 (Figs. S1 and S2 in the Supplementary Appendix). Meanwhile, 2-year relative survival among patients with NSCLC was higher among women than among men; survival among women improved from 35% in 2001 to 44% in 2014 (Fig. 3B). Such improvement among patients with NSCLC was seen for all races (Fig. 4).
Figure 4. NSCLC Survival Trends among Men and Women According to Race and Ethnic Group.
Results for 2-year lung-cancer–specific survival are shown for the NSCLC subtype according to race and ethnic group among men (Panel A) and women (Panel B). Results are shown for the SEER 18-registry database, excluding data from the Alaska Native registry.
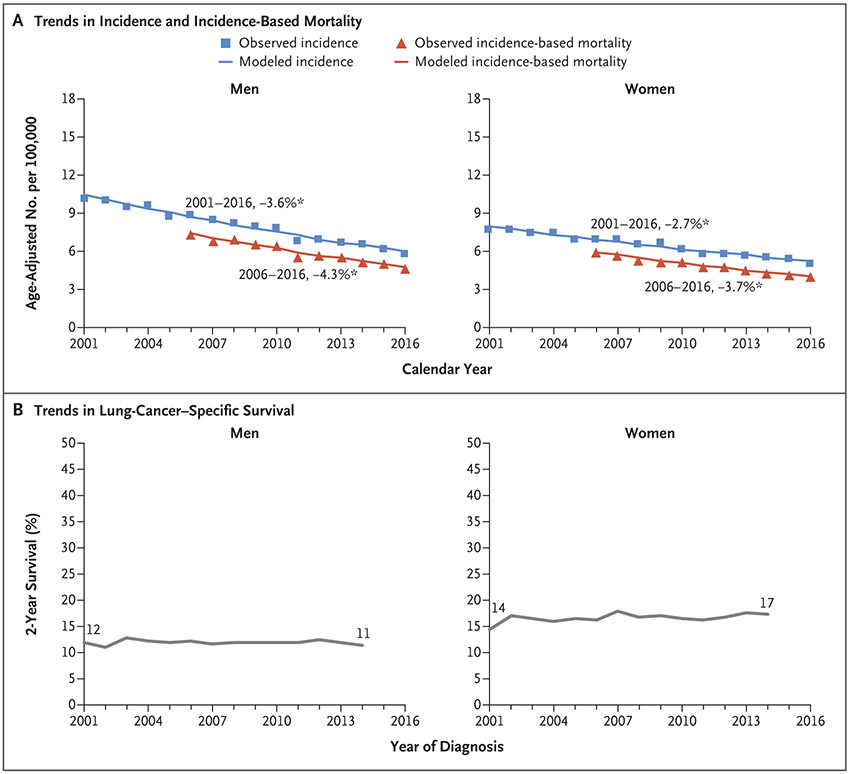
For patients with SCLC, mortality decreased similarly to incidence among men and women. For example, among men, incidence-based mortality decreased by 4.3% annually (95% CI, 3.7 to 4.3), whereas the incidence declined by 3.6% annually (95% CI, 3.3 to 3.9) (Fig. 5A, left). The corresponding relative survival curve for SCLC was more or less flat, indicating a lack of improvement during this period (Fig. 5B, left). We observed similar patterns among women (Fig. 5A and 5B. right).
Figure 5. Small-Cell Lung-Cancer (SCLC) Incidence, Incidence-Based Mortality, and Survival Trends among Men and Women.
Panel A shows age-adjusted incidence (blue) and incidence-based mortality (red) for the SCLC subtype among men and women. Incidence was adjusted for reporting delays. The line segments of each curve were selected with the Joinpoint program, and the percentage associated with each line represents the annual percentage change during the indicated range of years. Asterisks indicate annual percentage changes that are significantly different from zero (P<0.05). Panel B shows 2-year lung-cancer–specific survival according to year of SCLC diagnosis among men and women. Results are shown for the SEER 18-registry database. The following ICD-O-3 histology codes were used to define the SCLC subtype: 8002 and 8041–8045.
DISCUSSION
In this study, we describe trends in mortality among patients with different subtypes of lung cancer in the context of changing incidence and survival patterns in the U.S. general population. Overall mortality from lung cancer has declined. Similar patterns, based on estimations of incidence-based mortality, were observed for histologic subtypes of lung cancer — especially for NSCLC and to a lesser extent for SCLC. Specifically, we found a rapid decline in mortality from NSCLC during the period from 2006 through 2013; this decline began to accelerate in 2013, shortly after routine testing for molecular alterations in EGFR and ALK was recommended and commercial use of FDA-approved targeted therapy was introduced. For SCLC, we found steadily declining mortality from 2006 through 2016.
The decline in mortality from NSCLC has been driven by both declining incidence and improving survival. In particular, our results suggest that the substantial improvements in 2-year survival are probably behind the faster decrease (double the rate) in mortality from NSCLC as compared with incidence. The observed improvements in survival are not due to stage shifts, because these patients moved from unknown stages to more specific stage categories (as a result of the availability of better imaging) rather than shifting from late to early stages (Figs. S3 and S4). In addition, although lung-cancer screening has been recommended since 2014, uptake was low at least through 2016.25 Improvement in 2-year lung-cancer–specific survival among patients with NSCLC was seen in all races and ethnic groups in our study, despite understandable concerns that the new and frequently expensive cancer treatments may increase disparities.26,27 Nonetheless, utilization of these new targeted agents has increased over time, highlighting rapid changes in practice patterns.28
Over the past decade, the treatment paradigm for advanced NSCLC has evolved dramatically. The identification of “druggable” oncogenes (i.e., EGFR and ALK) has provided new, effective treatment targets, improving survival significantly among patients harboring the corresponding driver mutation.29-31 More recently, immune-based therapies — specifically, programmed cell death protein 1–programmed death ligand 1 (PD-1–PD-L1) inhibitors — have substantially improved outcomes of NSCLC treatment. Single-agent PD-1 pathway inhibitors (nivolumab, pembrolizumab, and atezolizumab) were first approved as second-line treatments in 2015. In randomized phase 3 trials, each drug was found to provide an improvement in overall survival as compared with the single-agent chemotherapeutic docetaxel in patients without EGFR or ALK mutations.32-35 Although not all patients have a response to immunotherapy, approximately 20% have substantial and often durable responses.36 The approval and adoption of these agents over the past 5 to 10 years has undoubtedly contributed to the decline we observed in incidence-based mortality. Meanwhile, the approval of immune-checkpoint inhibition in 2015 is unlikely to have contributed considerably to the decline in lung-cancer mortality in 2013. Although some patients with thoracic cancers received these agents in clinical trials before their FDA approval, improvement in antitumor outcomes in this relatively small cohort would contribute only marginally to improved outcomes overall. Finally, the introduction of a new therapy that is not curative would contribute to a temporary decline in mortality, but mortality would return to the background level. The Cancer Intervention and Surveillance Modeling Network (CISNET) lung-modeling consortium is developing natural history models aimed at predicting whether and when one should see a return in background mortality in the future as a result of the adoption of noncurative targeted therapy and immunotherapy for lung cancer in the United States.
In contrast, mortality from SCLC declined at a rate that was similar to that of the decline in incidence. Our study shows that the decrease in SCLC mortality can be explained entirely by a decrease in incidence, since we observed no improvement in survival among patients with SCLC over time. This result correlates with the limited treatment advances for SCLC over the same period. Studies have shown some promising immunotherapy strategies for the treatment of this recalcitrant disease37,38; however, the long-term effect of these agents is unknown.
Our results update previous analyses of trends in lung-cancer incidence according to histologic type.3,4 Here we found that overall incidence continued to decrease through 2016, but with faster decreases in the incidence of SCLC than in the incidence of NSCLC and with faster decreases among men than among women. Since most of the decrease in lung-cancer incidence is probably due to the considerable reduction in smoking in the United States since the 1960s, the faster decrease in SCLC incidence than in NSCLC incidence can be explained by the higher attributable fraction and relative risk of smoking for SCLC relative to the overall NSCLC group.4,7,8 Similarly, the faster decreases in lung-cancer incidence among men than among women can be attributed to the relative differences in smoking prevalence according to sex.39 Continued monitoring of trends in lung-cancer incidence according to histologic type (and stage) will be important, particularly because the adoption of lung-cancer screening is likely to lead to increased diagnosis of adenocarcinoma, as a result of early detection and overdiagnosis.
We used incidence-based mortality methods to partition deaths from lung cancer according to disease subtype. In fact, using the incidence-based mortality approach, we show that the numbers of deaths from lung cancer nationally are somewhat lower than the numbers currently reported on the basis of death-certificate data alone; a likely reason is that death-certificate data include deaths from cancers that have metastasized to the lung from other cancer sites, whereas the incidence-based mortality method excludes those deaths. Nonetheless, some challenges of incidence-based mortality methods must be considered. Since incidence-based mortality includes deaths among incident cases diagnosed in previous years, follow-up of cases diagnosed a number of years in the past is required. The number of years required depends on the aggressiveness of the cancer under study; for more aggressive cancers, fewer years after a particular index calendar year are necessary to reliably partition trends with the incidence-based mortality method. This is true for lung cancer, for which incidence-based mortality can be reliably calculated with a 5-year follow-up period.11 Furthermore, when patients with cancer move in or out of a registry catchment area, mismatches between mortality based on incidence and mortality based on death certificates can result. Again, this problem is alleviated for high-mortality cancers such as lung cancer: we found that 97.3% of the deaths from lung cancer occurred in the same state as the diagnoses. The incidence-based mortality approach has been used in our study to evaluate treatment outcomes to a limited degree, and it is difficult to attribute the improvement to a specific drug, since SEER does not capture detailed treatment information. However, pilot projects linking registry data with oncology practice claims data might enable more specific treatment analyses in the future. Lastly, given the nature of our analyses, we cannot rule out changes in some other factors contributing to the declining lung-cancer mortality. However, an important event occurred in 2013 that may have changed the slope of the incidence-based mortality trend: the approval of EGFR tyrosine kinase inhibitors as stage IV NSCLC first-line therapy. By 2013, genetic testing was performed in the majority of patients with NSCLC. In addition, although improvements in treatment, especially for stage IV disease, can have an immediate effect on mortality, upstream factors, such as changes in risk factors (e.g., smoking), tend to have a more gradual and diffuse effect, even if the changes in risk factors are rather abrupt or persistent. Therefore, any changes in risk factors were less likely to have had an immediate effect on the rapid decline in mortality we observed. However, without data on the fraction of patients now being treated with targeted therapies, the attribution of the improved survival to these therapies must be done with caution.
Our study has several strengths. First, we report U.S. population–based estimates of subtype-specific lung-cancer incidence, mortality, and survival trends. Second, these estimates are derived with high-quality cancer-registry data from the SEER Program, which reliably captures and classifies all newly diagnosed cancer cases in the registry catchment areas. Third, our results are more generalizable than those from single centers, and clinical trials are unlikely to include representative samples of older, sicker, and low-income patients.
We found a significant reduction in mortality from lung cancer in the U.S. general population, mainly due to a rapid decline in mortality from NSCLC. A recent study reported a large decrease in mortality from lung cancer in 2017 that was likely to have been driven by treatment, but the mortality trend included all histologic types.40 The faster decreases in mortality from NSCLC as compared with the incidence of NSCLC are probably driven by improvements in survival, which in turn are potentially driven by dissemination of targeted therapies for NSCLC; these therapies were approved as first-line treatment for stage IV EGFR-positive NSCLC in 2013. The survival benefit for patients with NSCLC treated with targeted therapy has been shown in clinical trials, but our study highlights their possible effect at the population level. We anticipate that incidence-based mortality methods will be valuable for evaluating trends in subtype-specific mortality in the future, as additional new lung-cancer treatments, as well as screening, are disseminated in the population.
Supplementary Material
Footnotes
Contributor Information
Nadia Howlader, Surveillance Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, MD
Gonçalo Forjaz, Surveillance Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, MD
Meghan J. Mooradian, Massachusetts General Hospital, Harvard Medical School, Boston
Rafael Meza, Department of Epidemiology, School of Public Health, University of Michigan, Ann Arbor
Chung Yin Kong, Massachusetts General Hospital, Harvard Medical School, Boston
Kathleen A. Cronin, Surveillance Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, MD
Angela B. Mariotto, Surveillance Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, MD
Douglas R. Lowy, Surveillance Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, MD.
Eric J. Feuer, Surveillance Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, MD
REFERENCES
- 1.Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG. Introduction to the 2015 World Health Organization classification of tumors of the lung, pleura, thymus, and heart. J Thorac Oncol 2015;10:1240–2. [DOI] [PubMed] [Google Scholar]
- 2.Howlader N, Krapcho M, Miller D, et al. SEER cancer statistics review, 1975-2016 [November 2018 SEER data submission posted to the SEER web site, April 9, 2020]. Bethesda, MD: National Cancer Institute; (https://seer.cancer.gov/csr/1975_2016/). [Google Scholar]
- 3.Lewis DR, Check DP, Caporaso NE, Travis WD, Devesa SS. US lung cancer trends by histologic type. Cancer 2014;120:2883–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meza R, Meernik C, Jeon J, Cote ML. Lung cancer incidence trends by gender, race and histology in the United States, 1973-2010. PLoS One 2015;10(3):e0121323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu M, Feuer EJ, Cronin KA, Caporaso NE. Use of multiple imputation to correct for bias in lung cancer incidence trends by histologic subtype. Cancer Epidemiol Biomarkers Prev 2014;23:1546–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haiman CA, Stram DO, Wilkens LR, et al. Ethnic and racial differences in the smoking-related risk of lung cancer. N Engl J Med 2006;354:333–42. [DOI] [PubMed] [Google Scholar]
- 8.Kenfield SA, Wei EK, Stampfer MJ, Rosner BA, Colditz GA. Comparison of aspects of smoking among the four histological types of lung cancer. Tob Control 2008;17:198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li Y, Appius A, Pattipaka T, Feyereislova A, Cassidy A, Ganti AK. Real-world management of patients with epidermal growth factor receptor (EGFR) mutation-positive non-small-cell lung cancer in the USA. PLoS One 2019;14(1):e0209709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ward EM, Sherman RL, Henley SJ, et al. Annual report to the nation on the status of cancer, featuring cancer in men and women age 20-49 years. J Natl Cancer Inst 2019;111:1279–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chu KC, Miller BA, Feuer EJ, Hankey BF. A method for partitioning cancer mortality trends by factors associated with diagnosis: an application to female breast cancer. J Clin Epidemiol 1994;47:1451–61. [DOI] [PubMed] [Google Scholar]
- 12.Feuer EJ, Merrill RM, Hankey BF. Cancer surveillance series: interpreting trends in prostate cancer — part II: cause of death misclassification and the recent rise and fall in prostate cancer mortality. J Natl Cancer Inst 1999;91:1025–32. [DOI] [PubMed] [Google Scholar]
- 13.Hur C, Miller M, Kong CY, et al. Trends in esophageal adenocarcinoma incidence and mortality. Cancer 2013;119:1149–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brenner H, Hoffmeister M, Jansen L. Comparisons of colorectal cancer mortality between screening participants and the general population are strongly biased unless an incidence-based mortality approach is used. J Clin Epidemiol 2014;67:184–9. [DOI] [PubMed] [Google Scholar]
- 15.Phipps AI, Scoggins J, Rossing MA, Li CI, Newcomb PA. Temporal trends in incidence and mortality rates for colorectal cancer by tumor location: 1975-2007. Am J Public Health 2012;102:1791–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jatoi I, Chen BE, Anderson WF, Rosenberg PS. Breast cancer mortality trends in the United States according to estrogen receptor status and age at diagnosis. J Clin Oncol 2007;25:1683–90. [DOI] [PubMed] [Google Scholar]
- 17.Howlader N, Morton LM, Feuer EJ, Besson C, Engels EA. Contributions of subtypes of non-Hodgkin lymphoma to mortality trends. Cancer Epidemiol Biomarkers Prev 2016;25:174–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Howlader N, Shiels MS, Mariotto AB, Engels EA. Contributions of HIV to non-Hodgkin lymphoma mortality trends in the United States. Cancer Epidemiol Biomarkers Prev 2016;25:1289–96. [DOI] [PubMed] [Google Scholar]
- 19.Wachtel MS, Nelius T, Haynes AL, Dahlbeck S, de Riese W. PSA screening and deaths from prostate cancer after diagnosis — a population based analysis. Prostate 2013;73:1365–9. [DOI] [PubMed] [Google Scholar]
- 20.Clegg LX, Feuer EJ, Midthune DN, Fay MP, Hankey BF. Impact of reporting delay and reporting error on cancer incidence rates and trends. J Natl Cancer Inst 2002;94:1537–45. [DOI] [PubMed] [Google Scholar]
- 21.SEER cause of death recode. Bethesda, MD: National Cancer Institute; (http://seer.cancer.gov/codrecode/). [Google Scholar]
- 22.Joinpoint trend analysis software. Bethesda, MD: Statistical Research and Applications Branch, National Cancer Institute; (https://surveillance.cancer.gov/joinpoint/). [Google Scholar]
- 23.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000;19:335–51. [DOI] [PubMed] [Google Scholar]
- 24.Mariotto AB, Noone A-M, Howlader N, et al. Cancer survival: an overview of measures, uses, and interpretation. J Natl Cancer Inst Monogr 2014;2014:145–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jemal A, Fedewa SA. Lung cancer screening with low-dose computed tomography in the United States — 2010 to 2015. JAMA Oncol 2017;3:1278–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blom EF, Ten Haaf K, Arenberg DA, de Koning HJ. Disparities in receiving guideline-concordant treatment for lung cancer in the United States. Ann Am Thorac Soc 2020;17:186–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nabi J, Trinh Q-DK. New cancer therapies are great — but are they helping everyone? Health Affairs Blog. April 12, 2019. (https://www.healthaffairs.org/do/10.1377/hblog20190410.590278/full/). [Google Scholar]
- 28.Bradley CJ, Eguchi M, Perraillon MC. Factors associated with utilization of high cost agents for the treatment of metastatic non-small cell lung cancer. J Natl Cancer Inst 2019. November 9 (Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shaw AT, Friboulet L, Leshchiner I, et al. Resensitization to crizotinib by the lorlatinib ALK resistance mutation L1198F. N Engl J Med 2016;374:54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sequist LV, Yang JC, Yamamoto N, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol 2013;31:3327–34. [DOI] [PubMed] [Google Scholar]
- 31.Soria J-C, Ohe Y, Vansteenkiste J, et al. Osimertinib in untreated EGFR-mutated advanced non–small-cell lung cancer. N Engl J Med 2018;378:113–25. [DOI] [PubMed] [Google Scholar]
- 32.Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus docetaxel in advanced nonsquamous non–small-cell lung cancer. N Engl J Med 2015;373:1627–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Herbst RS, Baas P, Kim DW, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet 2016;387:1540–50. [DOI] [PubMed] [Google Scholar]
- 34.Rittmeyer A, Barlesi F, Waterkamp D, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet 2017;389:255–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus docetaxel in advanced squamous-cell non–small-cell lung cancer. N Engl J Med 2015;373:123–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Horn L, Spigel DR, Vokes EE, et al. Nivolumab versus docetaxel in previously treated patients with advanced non-small-cell lung cancer: two-year outcomes from two randomized, open-label, phase III trials (CheckMate 017 and CheckMate 057). J Clin Oncol 2017;35:3924–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Antonia SJ, López-Martin JA, Bendell J, et al. Nivolumab alone and nivolumab plus ipilimumab in recurrent small-cell lung cancer (CheckMate 032): a multicentre, open-label, phase 1/2 trial. Lancet Oncol 2016;17:883–95. [DOI] [PubMed] [Google Scholar]
- 38.Horn L, Mansfield AS, Szczęna A, et al. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med 2018;379:2220–9. [DOI] [PubMed] [Google Scholar]
- 39.Jeon J, Holford TR, Levy DT, et al. Smoking and lung cancer mortality in the United States from 2015 to 2065: a comparative modeling approach. Ann Intern Med 2018;169:684–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin 2020;70:7–30. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.