Abstract
The success of immune checkpoint inhibitors in metastatic renal cell carcinoma (RCC) has renewed interest in studying these agents in preoperative settings. Here, we present a case of metastatic RCC with an inferior vena cava (IVC) tumor thrombus extending to the right atrium. Preoperative systemic therapy with ipilimumab/nivolumab was initiated for four cycles. The IVC tumor thrombus level was significantly downstaged from IV to I according to the Mayo classification, which enabled us to perform cytoreductive nephrectomy and IVC thrombectomy without extracorporeal circulation. Preoperative ipilimumab/nivolumab may lead to significant downstaging of caval tumor thrombus in metastatic RCC.
Keywords: Renal cell carcinoma, Tumor thrombus, Preoperative treatment, Ipilimumab/nivolumab
Abbreviations: renal cell carcinoma, RCC; inferior vena cava, IVC; immune checkpoint inhibitors, ICIs; cytoreductive nephrectomy, CN; computed tomography, CT; magnet resonance imaging, MRI; overall survival, OS
1. Introduction
The treatment of metastatic renal cell carcinoma (RCC) with inferior vena cava (IVC) tumor thrombus is complicated. Cytoreductive nephrectomy (CN) is an option for treating metastatic RCC, but patients with venous tumor thrombus have higher perioperative mortality in concordance with the level of thrombus.1 These patients may benefit from immune checkpoint inhibitors (ICIs), which have become important drugs in the field. Immunotherapy with combined ipilimumab and nivolumab has become a first-line therapy in the intermediate- and poor-risk groups of metastatic RCC according to the CheckMate 214 trial.2 However, there are few reports using ICIs as preoperative treatment, and efficacy to the level of tumor thrombus is unknown.2,3 Herein, we describe a case of metastatic RCC with IVC tumor thrombus extending to the right atrium treated with preoperative ipilimumab and nivolumab.
2. Case presentation
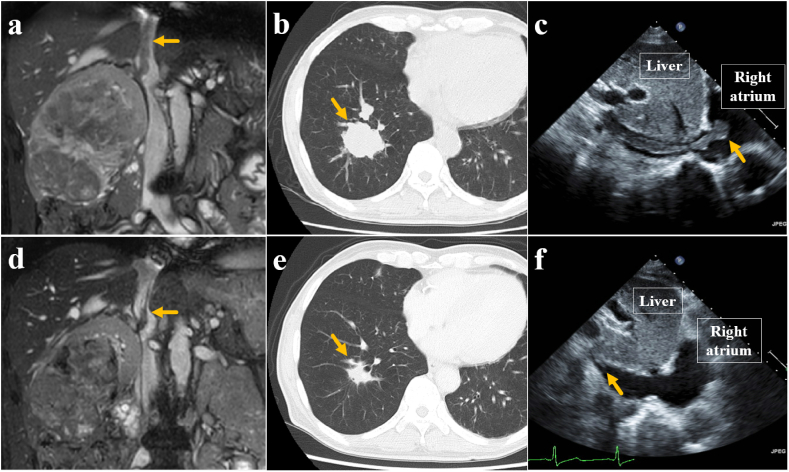
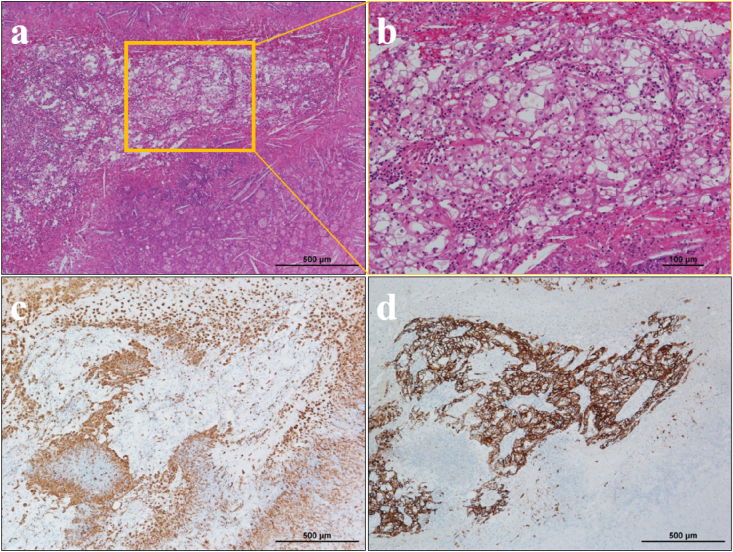
A 67-year-old man was admitted to our hospital with continuous hiccups for 3 years. Computed tomography (CT) revealed a 137- × 95-mm tumor in the right kidney, multiple lung metastases, and mediastinal lymphadenopathy (Fig. 1a and b). Magnetic resonance imaging and echocardiography revealed an IVC tumor thrombus extending to the right atrium (Mayo classification level IV) (Fig. 1c). A core needle biopsy of the right renal tumor showed clear cell RCC with no variant histology. We diagnosed him with cT3cN0M1 RCC. The performance status was good, and the International Metastatic RCC Database Consortium scoring system indicated the patient was in the poor-risk group. We suggested a preoperative systemic therapy with ipilimumab and nivolumab to be initiated for tumor downstaging to possibly reduce surgical morbidity and mortality, which was administered at a dose of 1 and 240 mg/kg every 3 weeks, respectively. According to the Common Terminology Criteria for Adverse Events, the patient experienced grade 1 rash and fever. After four cycles of therapy, CT showed shrinkage of the primary tumor to 105- × 74-mm and a reduction in lung metastases and lymphadenopathy (Fig. 1d and e). IVC tumor thrombus level was significantly downstaged to 14 mm above the right renal vein (level I) (Fig. 1f), and we therefore decided to perform CN and IVC thrombectomy through a chevron incision. There was no adhesion around the tumor, and we performed intraoperative transesophageal echocardiography for identifying the thrombus. The surgical procedures were completed without extracorporeal circulation. Operative time was 182 min and the blood loss was 375 mL. Histological findings showed residual viable cells in the primary site and tumor thrombus, co-existing with extensive necrotic tissues, cholesterol clefts, and invasion of macrophages and lymphocytes, which are typical features of immune-related pathologic responses (Fig. 2a–d). There were no postoperative events and biweekly nivolumab monotherapy was started 4 months after surgery. Pulmonary metastases were identified as stable disease at 1 year postoperatively.
Fig. 1.
Representative magnet resonance imaging (MRI), computed tomography (CT), and echocardiography at the time of diagnosis (a, b, c), and after four courses of preoperative ipilimumab/nivolumab combination therapy (d, e, f). Primary tumor and pulmonary metastases showed partial response, and IVC tumor thrombus was significantly downstaged from level IV to level I.
Fig. 2.
Pathological assessments. HE staining (a, b), immunostaining of CD68 (c) and AE1/AE3 (d) of the primary tumor. CD68 shows macrophage, and AE1/AE3 shows where viable cell exists. It was clear cell renal cell carcinoma, and around the viable lesion, there was immune activation with dense tumor infiltrating macrophage and massive cell death with cholesterol clefts, which were the features of immune-related pathologic response.
3. Discussion
For patients with metastatic RCC, CN followed by cytokine therapy has been established as the standard treatment of care. However, the success of targeted therapies in prolonging median overall survival (OS) in the CARMENA and SURTIME trials has been encouraging as a replacement for immediate CN in metastatic RCC patients with intermediate- or poor-risk classifications.1,4 Abel et al. reported that patients with expected poor OS, including level IV tumor thrombus, should be considered for preoperative therapy rather than immediate CN.5
The reduction of the primary tumor and the possible downstaging of tumor thrombus by preoperative treatment may improve surgical resectability and decrease surgical morbidity.1 Additionally, a lack of response to preoperative therapy may identify patients with poor prognosis, helping us avoid performing unnecessary CN.5 However, there is no firmly evidenced regimen to be used in preoperative settings. With preoperative targeting therapy, the median primary tumor diameter reduction was 9.5%–28.3%, but the median decrease in tumor thrombus height was 1.5 cm.1 Cost et al. showed that only 1 of 24 patients showed sufficient downstaging of caval tumor thrombus to justify downscaling the surgical procedure. While individual case reports have indicated some success, the routine use of preoperative targeting therapy is considered unlikely to significantly shrink the tumor thrombus.1
ICIs have revolutionized the treatment of metastatic RCC, which has renewed interest in investigating these agents in preoperative settings. There are two ongoing phase III clinical trials, the NORDIC-SUN trial and the PROBE trial, that are prospectively investigating the value of CN and preoperative ICIs in metastatic RCC.4 Although some reports have shown the effectiveness of preoperative ICIs for the primary tumor and metastases, there are only a few case reports demonstrating the impact on tumor thrombus. Lebbate et al. reported that four cycles of preoperative ipilimumab/nivolumab and nivolumab monotherapy downstaged level IV tumor thrombus to level III.2 Okada et al. reported that four cycles of preoperative ipilimumab/nivolumab and five cycles of nivolumab monotherapy downstaged level III tumor thrombus (level not mentioned).3
To the best of our knowledge, this is the first case of metastatic RCC with caval tumor thrombus in which preoperative ICIs significantly downstaged the level of thrombus from level IV to level I.
4. Conclusion
Our case report provides evidence that preoperative therapy by ICIs might be beneficial for downstaging level IV tumor thrombus, which allows for the reduction of perioperative morbidity and mortality. Because of the lack of clinical trials, the effect of ICI therapy followed by CN has not yet been clarified but needs to be better redefined in the era of immunotherapy.
Consent
Written informed consent was obtained from the patient.
Author contributions
Hikari Otsuka: Conceptualization, Methodology, Validation, Investigation, Data Curation, Writing- Original Draft, Visualization. Kimihiko Masui: Writing- Reviewing and Editing. Toshihide Hosomi: Writing- Reviewing and Editing. Yuki Makino: Writing- Reviewing and Editing. Noboru Shibasaki: Writing- Reviewing and Editing. Yasumasa Shichiri: Supervision, Writing- Reviewing and Editing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
None.
Acknowledgement
None.
References
- 1.Shinder B.M., Rhee K., Farrell D. Surgical management of advanced and metastatic renal cell carcinoma: a multidisciplinary approach. Front Oncol. 2017;7:107. doi: 10.3389/fonc.2017.00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Labbate C., Hatogai K., Werntz R. Complete response of renal cell carcinoma vena cava tumor thrombus to neoadjuvant immunotherapy. J Immunother Cancer. 2019;7:66. doi: 10.1186/s40425-019-0546-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Okada T., Hamamoto S., Etani T. Complete response of renal cell carcinoma with an inferior vena cava tumor thrombus and lung metastases after treatment with nivolumab plus ipilimumab. Int Canc Conf J. 2020;9:88–91. doi: 10.1007/s13691-020-00403-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuusk T., Abu-Ghanem Y., Mumtaz F. Perioperative therapy in renal cancer in the era of immune checkpoint inhibitor therapy. Curr Opin Urol. 2021;31:262–269. doi: 10.1097/MOU.0000000000000868. [DOI] [PubMed] [Google Scholar]
- 5.Psutka S.P., Leibovich B.C. Management of inferior vena cava tumor thrombus in locally advanced renal cell carcinoma. Ther Adv Urol. 2015;7:216–229. doi: 10.1177/1756287215576443. [DOI] [PMC free article] [PubMed] [Google Scholar]