Introduction
Access to a dermatologist improves melanoma health outcomes.1 Yet, patients in the United States face significant barriers to dermatologic care,2 a problem that can be partially ameliorated through telemedicine or the “use of medical information exchanged via electronic communications to improve a patient's clinical health status.”3 As a highly visual specialty, dermatology is particularly well-suited for telemedicine (ie, teledermatology).4 This report details a patient case in which teledermatology was essential for identifying an atypical lesion as amelanotic melanoma. This case is a prime example of teledermatology's utility in expediting urgent dermatologic care, especially for rare skin cancers, the atypical appearances of which often result in missed diagnosis and worse prognosis.
Case report
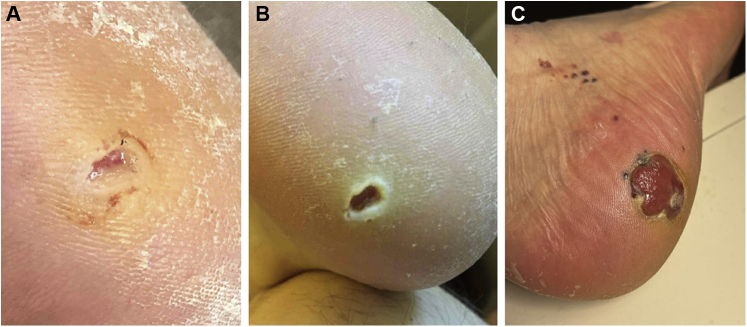
A 69-year-old man with no significant past medical history first presented to his primary care physician (PCP) with a small, dot-sized, bleeding sore on his right heel for a duration of 1 month. He was initially diagnosed with a fissured callus and treated with ciclopirox cream and triple antibiotic ointment. On a follow-up with his PCP 3 months later, the patient's lesion was ulcerated and erythematous. His diagnosis was updated to cellulitis, and he was put on a course of amoxicillin and clavulanic acid. When, after an additional month, the lesion had still not healed, he sent digital images to his PCP (Fig 1, A) and again after 24 days (Fig 1, B), and the patient was then referred to podiatry and seen 1 month later, at which time the lesion was debrided and bandaged with Aquacel (ConvaTec Group) gauze and the patient was instructed to use corn pads for offloading. Over the next 7 months, he did not seek medical advice until he noticed the development of “black spots” ascending from his heel lesion to his lower leg, which prompted him to seek dermatologic care. Due to difficulty obtaining a clinic visit, he submitted photos of his left heel (Fig 1, C) through the University of Pittsburg Medical Center Health Plan eDermatology consumer to physician asynchronous teledermatology platform, which is available to all enrollees and anyone in the state of Pennsylvania at https://edermatology.upmc.com/ for a self-requested dermatologic consultation.
Fig 1.
Patient taken digital images sent to health care team via patient electronic medical record. (A) Right calcaneal lesion (May 5, 2020). (B) Right calcaneal lesion (May 29, 2020). (C) Right calcaneal lesion with disseminated pigmented papules (February 9, 2021, date of University of Pittsburg Medical Center eDermatology encounter).
The patient-submitted photos, which were evaluated less than 24 hours after submission, deemed to require an urgent in-person appointment. The patient presented to our clinic in less than 48 hours, at which time 2 biopsies were taken and sent to Dermatopathology. The following day, he was ultimately diagnosed with acral malignant melanoma (Breslow thickness of 1.5 mm) with surface ulcer and a mitotic count of 4 and cutaneous in-transit metastases 14 months after the lesion had developed. He was transitioned to the University of Pittsburgh Medical Center - Hillman Cancer Center for oncologic staging and management within 7 additional days, where his condition was evaluated as stage IIID with unresectable disease and started in a clinical trial.
Discussion
Across the United States, there are significant disparities in access to dermatologic care, especially along racial, urban/rural, and socioeconomic lines. This divide is perhaps most evident in the elevated mortality rates of melanoma and nonmelanoma skin cancers among minorities, rural residents, individuals occupying lower socioeconomic strata, and the uninsured, whose cases often fail to be diagnosed early and subsequently progress unchecked to more severe stages.2 It has been well documented in the literature that access to a dermatologist significantly improves melanoma health outcomes, with some empirical analyses suggesting that the presence of 1.001 to 2 dermatologists per 100,000 people is associated with a 53.0% reduction in the melanoma mortality rate.1 Yet, even among patients such as ours, who do not belong to traditionally underserved categories, access to dermatologic care remains a stubborn problem; one that is exacerbated by the long-standing dermatology workforce shortage and a tightly regulated, protracted training process for qualified practitioners.5
Though the solution to these care deficits is far from straightforward, telemedicine offers an opportunity to begin bridging delivery gaps in dermatology, and its use has only gained in popularity since the beginning of the COVID-19 pandemic.6 In particular, teledermatology can play a role in earlier and more accurate detection of skin cancer, leading to improved patient outcomes. Aided by advancements in digital image quality on smart devices and the ability to zoom in on image files, current teledermatology platforms may also be used in triage of lesions with few distinguishing features, allowing patients with pressing dermatologic conditions to access care in a timely manner.7
Amelanotic melanoma is a rare variant, comprising anywhere from 2% to 8% of all melanoma cases. It is often initially misdiagnosed, owing to its depigmented appearance and diverse clinical presentation. Patients and clinicians are often educated on the ABCDEs (asymmetry, border irregularity, color variation, large diameter, and evolution) of melanoma and advised to look for new or changing moles, which can cause them to miss amelanotic lesions that do not exhibit these typical warning signs. These lesions also pose a diagnostic challenge to the clinician and are frequently diagnosed as nonmelanoma skin cancers, vascular lesions like pyogenic granulomas, or even dermatitides, such as eczema or contact dermatitis, leading to delayed diagnosis until the lesion has reached an advanced stage that portends a worse prognosis.8 Thus, there still is a need to advocate for skin cancer education to advance practice providers and PCPs, especially of atypical presentations.9
We describe a patient presenting with an ulcerated nonhealing heel lesion for over a year, who was later correctly diagnosed with amelanotic melanoma initiated by a teledermatology encounter. As demonstrated in our case, teledermatology and its ease of access played a crucial role in expediting dermatologic care for this patient. As medical technologies continue to advance, we anticipate that teledermatology will serve as an indispensable tool for dermatologists and patients alike to triage skin conditions and, ultimately, improve health access and outcomes, which will depend on future regulatory and insurance issues at the State and Federal levels.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Aneja S., Aneja S., Bordeaux J.S. Association of increased dermatologist density with lower melanoma mortality. Arch Dermatol. 2012;148(2):174–178. doi: 10.1001/archdermatol.2011.345. [DOI] [PubMed] [Google Scholar]
- 2.Buster K.J., Stevens E.I., Elmets C.A. Dermatologic health disparities. Dermatol Clin. 2012;30(1):53–59. doi: 10.1016/j.det.2011.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Voran D. Telemedicine and beyond. Mo Med. 2015;112(2):129–135. [PMC free article] [PubMed] [Google Scholar]
- 4.Maddukuri S., Patel J., Lipoff J.B. Teledermatology addressing disparities in health care access: a review. Curr Dermatol Rep. 2021;10(1):40–47. doi: 10.1007/s13671-021-00329-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kimball A.B., Resneck J.S., Jr. The US dermatology workforce: a specialty remains in shortage. J Am Acad Dermatol. 2008;59(5):741–745. doi: 10.1016/j.jaad.2008.06.037. [DOI] [PubMed] [Google Scholar]
- 6.Portnoy J., Waller M., Elliot T. Telemedicine in the era of COVID-19. J Allergy Clin Immunol Pract. 2020;8(5):1489–1491. doi: 10.1016/j.jaip.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chuchu N., Dinnes J., Takwoingi Y. Teledermatology for diagnosing skin cancer in adults. Cochrane Database Syst Rev. 2018;12(12):CD013193. doi: 10.1002/14651858.CD013193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bono A., Maurichi A., Moglia D. Clinical and dermatoscopic diagnosis of early amelanotic melanoma. Melanoma Res. 2001;11(5):491–494. doi: 10.1097/00008390-200110000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Deng W., Yu R., Cui Y., Zheng Z. Amelanotic acral melanoma misdiagnosed as verruca plantaris. An Bras Dermatol. 2019;94(1):86–88. doi: 10.1590/abd1806-4841.20197568. [DOI] [PMC free article] [PubMed] [Google Scholar]