Abstract
Background and aim:
Providing care to an older adult with a disability has been associated with increased risk to the caregiver’s health, but most previous studies of caregiving and health compare persons who are already caregivers with poorly matched non-caregiving controls and are often based on convenience samples. In this report, we describe the enrollment of persons who transitioned into a family caregiving role while participating in a national epidemiological study.
Methods:
Participants in the REasons for Geographic And Racial Differences in Stroke (REGARDS) study were asked on two occasions 9-14 years apart if they were providing care on an ongoing basis to a family member with a chronic illness or disability. Those who answered “no” and “yes,” respectively, to this caregiving question and reported sufficient caregiving responsibilities after their transitions were enrolled in the present study as incident caregivers (N = 251). Participants matched on multiple demographic and health history variables and who reported no history of caregiving were enrolled as non-caregiving controls (N = 251).
Results:
Among eligible participants, 84% agreed to participate, and 47% of caregivers reported caring for a person with dementia. Descriptive analyses confirmed the success of the matching procedures for balancing the groups on multiple demographic and pre-caregiving health variables. Depressive symptoms and perceived stress increased significantly after the transition to caregiving.
Conclusion:
Comparable, population-based samples of incident caregivers and matched non-caregivers have been enrolled. Future analyses will examine within-person changes in health and circulating biomarkers as a function of the transition to caregiving.
Keywords: Caregiving, Epidemiology, Dementia, Health
As the older adult population expands in much of the developed world, more family members and other informal caregivers will be required to provide ongoing, long-term care to older adults with disabilities. Caregiving has long been considered to be an excellent, non-experimental model for studying the impact of real-world, chronic stressors on measures of health [1-3]. Systematic reviews and meta-analyses have generally found that caregivers report poorer psychological well-being (e.g., more problems with depression and anxiety) than non-caregiving comparison groups [4, 5], but differences tend to be larger in studies that use convenience samples compared to those that use more representative, population-based samples [4]. Dementia caregiving has also been associated with higher levels of burden and depression among caregivers than other forms of caregiving [4, 6, 7].
A number of studies have reported biomarker indications of inflammation or immunologic vulnerability to chronic stress among dementia caregivers [8-11]. However, systematic reviews of these and other studies have found this evidence to be inconsistent [1, 12], and a meta-analysis of these findings found the associations for specific biomarkers to be quite small in overall magnitude and of questionable clinical significance [13]. A substantial majority of the published studies comparing the health and well-being of family caregivers with non-caregivers have used convenience samples and have provided only minimal information on the characteristics of the healthy volunteers who served as the non-caregiving comparison participants.
One widely-cited, population-based study of caregiving and mortality found significantly higher 4-year mortality rates among strained spouse caregivers compared to spouses of non-disabled partners [14], but several, more recent, population-based studies with larger sample sizes and longer follow-up periods have identified the opposite pattern of findings, namely that informal or family caregivers have lower mortality rates (i.e., live longer) than non-caregiving control samples [15-20]. The few population-based comparisons of caregivers and non-caregivers on circulating biomarker indicators of inflammation or immune system functioning have also generally failed to detect any significant vulnerabilities among the caregivers compared to non-caregiving control groups [21-24].
Although population-based studies of caregiving and health are potentially advantageous over studies of convenience samples, many population-based analyses are limited by minimal inclusion/exclusion criteria to define caregiving and do not include key variables important for assessing caregiving stress. For example, most of the population-based studies of health, biomarkers, or mortality associated with caregiving include rather general classifications of caregiving status and do not include more detailed indicators of caregiving involvement such as the duration of caregiving, the clinical condition(s) and disability levels of the care recipients, whether those care recipients have dementia, or whether care for activities of daily living (ADL) or instrumental ADLs is provided. In addition, the vast majority of existing studies on the health and well-being of caregivers consist of comparisons of pre-existing caregivers to varying samples of non-caregiving controls.
Surprisingly little research has examined changes on health indicators prospectively within persons who transition into a family caregiving role over time while participating in a longitudinal epidemiologic study. One study focused on spouses who did or did not transition to caregiving over a five-year period, but participants who either did or did not experience this transition differed at baseline key demographic and health risk behaviors [24]. Another study identified a sizeable sample of individuals who reported transitioning to caregiving over a five-year period, but a very low threshold for caregiving (any assistance with personal care over the previous year) was used, raising concerns about the degree of stress exposure of many of these caregivers [25].
Several research design characteristics would be ideal for strengthening an inference that an observed health difference between caregivers and non-caregivers could be attributed to the caregiving role. First, a relatively large, population-based sample of individuals who have been administered measures of health and well-being prior to becoming caregivers should be identified. Second, the same or similar health measures should be obtained again at a later point after some individuals have made the transition to caregiving. Third, minimal thresholds for the duration of caregiving and amount of care provided (e.g., hours per week) should be set to assure that caregivers have sufficient exposure to potential caregiving stressors. Fourth, individual differences in caregiving experiences, such as the types of assistance provided and whether care is provided to persons with dementia or serious cognitive impairment, should be assessed. Finally, because health can change over time simply due to aging, longitudinal measures of health should also be collected for a comparable group of non-caregivers, who have been confirmed to not have any significant exposure to caregiving stress over the same study interval.
In this report, we describe the design, development, and application of methods that were used to screen and enroll a sample of persons who transitioned into a family caregiving role while participating in a national, population-based, longitudinal cohort study. We provide data on the prevalence of becoming a caregiver among a sample of adults 45 years of age and older who were not initially family caregivers, and how rigorous inclusion and exclusion criteria were applied to produce comparable samples of incident caregivers and a carefully-matched group of non-caregivers from the same longitudinal cohort study. We provide initial comparisons between these incident caregivers and non-caregivers to examine the effectiveness of our methods for balancing the two groups at and to show expected differences in relation to the stress exposure of caregiving. Our goal in this paper is to provide a detailed description of the design our study on caregiving transitions and our screening and enrollment methods. This information will be useful not only for understanding and interpreting future publications from this project but also for guiding other investigators who seek to implement more optimal research methods for identifying the specific effects of family caregiving on multiple measures of health and well-being.
Methods
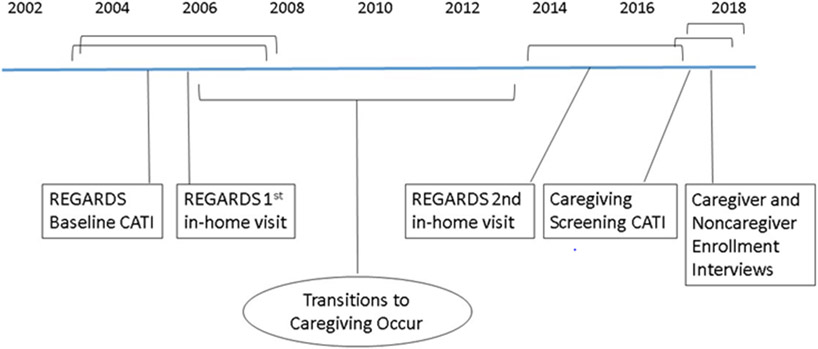
The Caregiving Transitions Study (CTS) is a nested case-control ancillary study of the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. The CTS enrolls REGARDS participants who have transitioned into a family caregiving role at some point between the 1st and 2nd REGARDS in-home visits along with individually-matched REGARDS participants who have never been caregivers throughout the same time period. The general timeline of the assessments and procedures used in the REGARDS study and the CTS are illustrated in Figure 1.
Figure 1.
Timeline of REGARDS and CTS Sessions. Assessments occurred in the same order for all participants, and brackets indicate range of when assessments occurred.
REGARDS Study Design and Participant Enrollment
The REGARDS study is a national longitudinal investigation of 30,239 adults in the United States who were 45 or more years of age when enrolled from 2003-2007. Potential participants for the REGARDS study were randomly sampled from a commercially-available nationwide list, and exclusion criteria included age less than 45, self-reported race other than African American or White, previous diagnosis of cancer requiring chemotherapy, or residence in or on a waiting list for a nursing home. African Americans and residents from the southern "stroke belt" region of the United States were oversampled by design. Additional information on the design, sampling, enrollment, and long-term follow-up procedures used in the REGARDS study have been described in detail elsewhere [20, 25-29]The study was reviewed and approved by the Institutional Review Boards of the University of Alabama at Birmingham and each participating institution.
REGARDS Data Collection Procedures
Baseline CATI.
Trained interviewers contacted potential participants by telephone, established eligibility for participation, and obtained verbal informed consent. A computer-assisted telephone interview (CATI) was then administered that collected information on demographic variables and multiple risk factors for stroke. Sex, race (African American or White), marital status, date of birth, education received, and annual household income category were all obtained by self-report.
An important variable for the CTS collected during the REGARDS baseline CATI was a question on caregiving status. Specifically, each participant was asked: “Are you currently providing care on an on-going basis to a family member with a chronic illness or disability? This would include any kind of help such as watching your family member, dressing or bathing this person, arranging care, or providing transportation." Participants who answered “yes” were categorized as caregivers, and those who answered “no” were characterized as non-caregivers at REGARDS baseline [28]. Other baseline CATI variables included a 4-item short-form of the Center for Epidemiological Studies Depression (CES-D) scale [30], a 4-item short-form of Cohen’s Perceived Stress scale [31], and the 12-item short-form health survey (SF-12) to assess health-related quality of life [32, 33].
REGARDS In-Home Visit #1:
A few weeks after completing the baseline CATI (M = 5.6 weeks), participants completed an in-home assessment during which directly observed health data were obtained (e.g., BMI, electrocardiogram) and biologic specimens were collected (e.g., blood, urine). Assessments were conducted by trained examiners employed by Examination Management Services, Incorporated (EMSI). Biological specimens were subsequently shipped for storage to the biomarker assessment laboratory at the University of Vermont [34].
Semi-annual follow-up CATIs.
REGARDS participants have been subsequently followed with semi-annual follow-up CATIs that inquire about possible strokes, other major health events such as myocardial infarctions, and screen for changes in cognitive functioning. These semi-annual follow-up interviews continue at the present time for over 13,000 participants who are still actively participating in the REGARDS study.
REGARDS Interview and In-Home Visit #2:
Approximately 9 years after the 1st in-home visit (M = 9.4 years), a second comprehensive assessment was conducted by the REGARDS team. This included a follow-up CATI on risk factors and a 2nd in-home assessment conducted by EMSI examiners with updated biomarker assessments [28].
CTS Data Collection Procedures
Follow-up Caregiving Screening CATI.
Approximately 12 years after enrollment into REGARDS (M = 11.7 years, range = 9.1 to 14.1 years) active REGARDS participants were screened by telephone during a regular REGARDS semi-annual follow-up CATI to obtain updated information on family relationship variables (e.g., current marital status, information on whether their parents were still living) and on caregiving status. During this screening CATI, each participant was asked “Are you currently providing care on an ongoing basis to a family member, friend, or neighbor with a chronic illness or a disability? This would include any kind of regular help with basic activities such as dressing, bathing, grooming this person, managing bills, arranging for medical care, watching or supervising this person, or providing transportation.” For those who answered “yes,” additional questions were asked about this care including the age of that person; their relationship with that person (e.g., spouse, child, parent, etc.); whether they currently lived together; whether the person had Alzheimer’s disease, another form of dementia, or serious memory problems; other major health problems that the person may have had; how many hours of care per week they provided because of their disability or health problems; how many years they have been providing this care; and how much of a mental or emotional strain was it to provide this care (no strain, some strain, or a lot of strain).
Participants who reported that they were not caregivers at the first REGARDS baseline CATI but had become caregivers at some point between the 1st and 2nd REGARDS in-home assessments were potentially eligible to be enrolled in the CTS as incident caregivers. Participants who answered “no” to the caregiving status questions at both the baseline CATI and the 12-year follow-up caregiver screening CATI were potentially eligible to be enrolled as non-caregiving controls. Additional eligibility criteria were examined in the CTS enrollment interviews.
Incident Caregiver Enrollment and Telephone Interview.
Participants who were potentially eligible to be enrolled as incident caregivers were subsequently contacted by a trained interviewer and asked to provide details on their caregiving experiences. Specifically, each potential caregiver was asked when they began serving in the caregiving role (month and year), whether they had been caregivers for this person continuously since that time, their relationship with the care recipient, whether their care recipient currently or previously lived in a nursing home or assisted living facility, and how many hours per week they provided care because of the person’s health problems or disabilities. In order to be eligible for the CTS, the reported month and year of the transition into a family caregiving role had to be at least six months after the 1st REGARDS in-home visit and at least 3 months before the 2nd REGARDS in home visit. In addition, potential caregivers were excluded if: 1) their care recipient was less than 18 years of age; 2) the care recipient resided in a nursing home, assisted living facility, or other institutional residential care setting; 3) the caregiver provided less than 5 hours of care per week; 4) the caregiver lived more than 50 miles from the care recipient; 5) the participant reported a paid (formal) caregiving relationship, or 6) the caregiver did not provide usable blood samples at either of the REGARDS in-home assessments.
Incident caregivers who were eligible to participate were then given more information about the CTS and asked to provide verbal informed consent. Those who consented were administered a series of questionnaires by telephone including a 10-item CES-D [35], the 4-item PSS [31], and the SF-12 [32]. They were also administered an 8-item screening measure to assess whether their care recipients had dementia (AD8 [36]), and a series of questions about whether assistance was provided for certain activities of daily living (ADLs), instrumental ADLs, or memory and behavior problems.
Matched Non-caregiving Control Enrollment and Telephone Interview.
Once an incident caregiver was enrolled, the REGARDS database was then searched to generate a list of up to 5 participants who: 1) answered “no” to the caregiving status questions at both the baseline CATI and the 12-year follow-up caregiver screening; 2) matched the enrolled caregiver on up to 7 demographic and health history factors; and 3) provided usable blood samples for analysis at both REGARDS in-home assessments. The 7 matching factors were age ± 5 years, sex, race, education level, marital status, self-rated health at the REGARDS baseline CATI, and an indicator used in previous research for any self-reported history of stroke, myocardial infarction, or other serious cardiovascular disease from the REGARDS baseline CATI [20]. In addition, potential non-caregiving controls who would be matched to spouse caregivers had to be married, and potential controls who would be matched to adult child caregivers had to have at least one living parent. For a small number of cases, exact person-to-person matching was not achieved on all 7 factors, and the self-rated health or cardiovascular disease history matching criteria were relaxed in those instances. All caregiver and non-caregiver control cases were completely and individually matched on the other 5 matching factors.
Potential non-caregiving controls for each enrolled caregiver were randomly called and further screened for eligibility. Potential controls who reported serving as a family caregiver at any point during their participation in the REGARDS study were excluded. Calls continued until one participant was determined to be eligible and gave verbal informed consent to participate in the project. These non-caregiving controls then completed a series of questionnaires including the 10-item CES-D [35], the 4-item PSS [31], and the SF-12 [32].
Results
Figure 2 summarizes the selection and enrollment of the incident caregivers and matched non-caregiving controls into the CTS. Of the 13,270 REGARDS participants who completed the 12-year follow-up caregiving screening CATI, 11,483 (87%) were not caregivers at the REGARDS baseline CATI and were, therefore, potentially eligible to participate in the CTS. Of these, 1,229 (11%) answered “yes” to the caregiving status question at the caregiving screening CATI, but 683 of these were determined to be ineligible for the CTS based on data already obtained from either the caregiving screening CATI (e.g., care began after the 2nd REGARDS in-home visit) or the REGARDS database (e.g., no usable blood samples obtained from the REGARDS in-home visits). This left 546 potential caregivers who were contacted by telephone for additional eligibility screening, and 248 of these participants (45%) were determined to be ineligible during the incident caregiver enrollment interview, leaving 298 eligible incident caregivers who were invited to participate in the CTS. Of these, 251 (84%) agreed to participate in the study.
Figure 2.
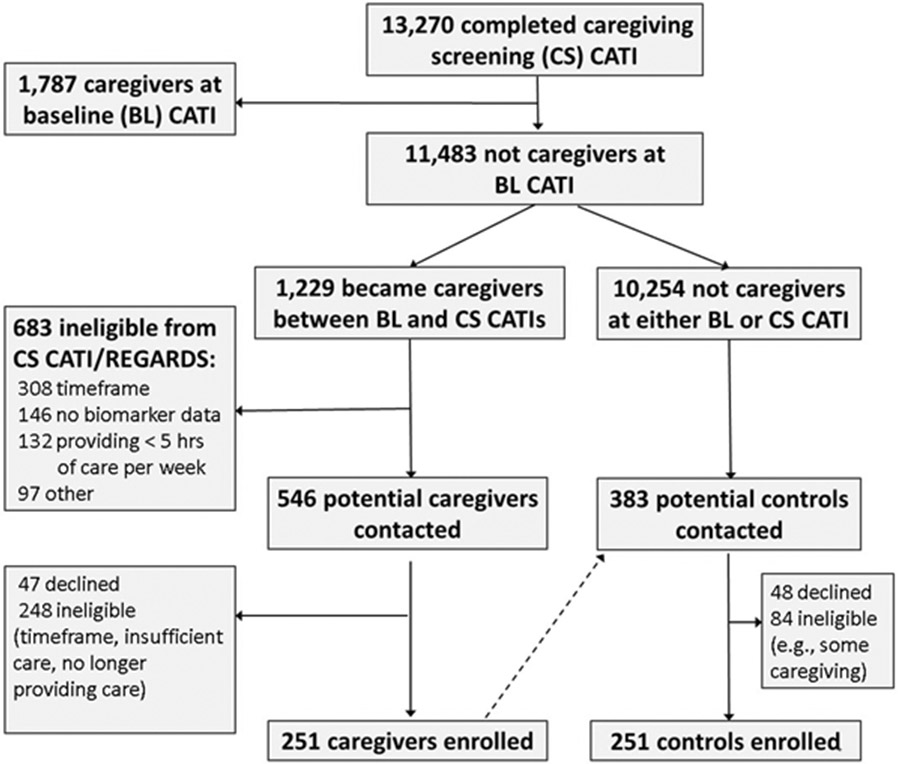
Flow Diagram of CTS Participant Selection.
Of the 10,254 REGARDS participants who answered “no” to the caregiving status questions at both the REGARDS baseline and 12-year caregiving screening CATIs, 383 were contacted as potential matched controls for the incident caregivers. Eighty-four (22%) were determined to be ineligible, many because they had engaged in some form of family caregiving during their participation in the REGARDS project. Among the remaining 299 potential non-caregiving controls, 251 (84%) agreed to participate and were enrolled.
Table 1 presents descriptive information for the 251 incident caregivers and 251 matched controls. Overall, caregivers were 65% female, 36% African American, and 76% married or cohabiting. Because groups were individually matched on sex, race, education, marital status, and age (± 5 years), p-values that would test group differences on these variables are not reported. Among the other variables, caregivers and controls did not differ on self-rated health, history of serious cardiovascular disease, CES-D, PSS, or the SF-12 summary scores assessed from the REGARDS baseline CATI (i.e., before the transition to caregiving when all participants were non-caregivers). The groups also did not differ on their duration of participation in the REGARDS project.
Table 1.
Descriptive Comparisons of Incident Caregivers and Matched Non-Caregiving Controls
| Variable | Total Sample | Incident Caregivers |
Noncaregiving Controls |
P |
|---|---|---|---|---|
| N | 502 | 251 | 251 | --- |
| Sex, Female N (%) | 326 (65) | 163 (65) | 163 (65) | --- |
| Race, African American N (%) | 180 (36) | 90 (36) | 90 (36) | --- |
| Education, College graduate N (%) | 220 (44) | 106 (42) | 114 (45) | --- |
| Marital Status at Transitions Int, N (%) | --- | |||
| Married/Cohabiting | 380 (76) | 190 (76) | 190 (76) | |
| Widowed | 41 (8) | 19 (8) | 22 (9) | |
| Divorced/Separated | 51 (10) | 26 (10) | 25 (10) | |
| Single / Never Married | 30 (6) | 16 (6) | 14 (6) | |
| Age at REGARDS baseline CATI, M (SD) | 59.9 (7.5) | 60.1 (7.7) | 59.7 (7.3) | --- |
| Age at Transitions interview, M (SD) | 71.9 (7.9) | 71.8 (8.1) | 72.0 (7.8) | --- |
| Self-Rated Health at REGARDS baseline CATI, N (%) | 0.43 | |||
| Excellent | 115 (23) | 61 (24) | 54 (22) | |
| Very Good | 169 (34) | 81 (32) | 88 (35) | |
| Good | 172 (34) | 84 (33) | 88 (35) | |
| Fair | 43 (9) | 22 (9) | 21 (8) | |
| Poor | 3 (1) | 3 (1) | 0 (0) | |
| Self-reported history of major cardiovascular disease at REGARDS baseline, Yes N (%) | 53 (11) | 27 (11) | 26 (10) | 0.88 |
| Duration between REGARDS Baseline CATI and Caregiver Screening CATI, Years, M (SD) | 11.7 (1.2) | 11.7 (1.2) | 11.7 (1.3) | 0.59 |
| Duration between REGARDS 1st and 2nd in-home visits, Years, M (SD) | 9.3 (0.9) | 9.3 (0.9) | 9.2 (0.8) | 0.60 |
| REGARDS baseline CATI variables (before transition to caregiving for caregivers) | ||||
| 4-item CES-D, M (SD) | 0.9 (1.7) | 0.8 (1.6) | 0.9 (1.8) | 0.79 |
| 4-item PSS, M (SD) | 3.0 (2.7) | 2.9 (2.6) | 3.0 (2.8) | 0.54 |
| PCS from SF-12, M (SD) | 48.7 (9.8) | 48.1 (10.3) | 49.3 (9.1) | 0.18 |
| MCS from SF-12, M (SD) | 55.0 (6.9) | 54.9 (6.7) | 55.0 (7.1) | 0.87 |
Note. P-values are for group comparisons from Pearson chi-square tests when frequencies (N, %) are reported and from independent sample t-tests when means (M) and standard deviations (SD) are reported.
Figures 3 and 4 present means and standard errors for well-being measures collected from the CTS interviews. After the transition to caregiving, caregivers reported significantly more symptoms of depression (p < 0.0001), more perceived stress (p < 0.0001), and lower physical (p = 0.003) and mental (p < 0.0001) health-related quality of life than the matched non-caregiving controls.
Figure 3.
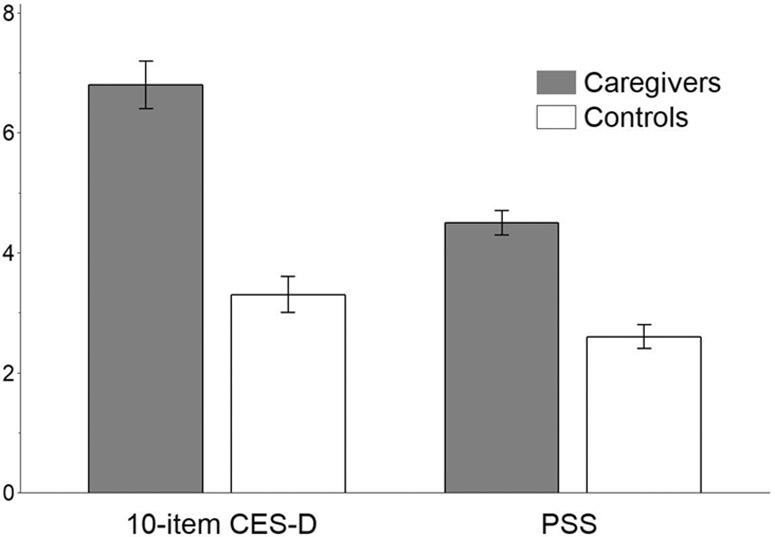
Means and Standard Errors of Depressive Symptoms (CES-D) and Perceived Stress (PSS) in Incident Caregivers Compared to Matched Controls
Figure 4.
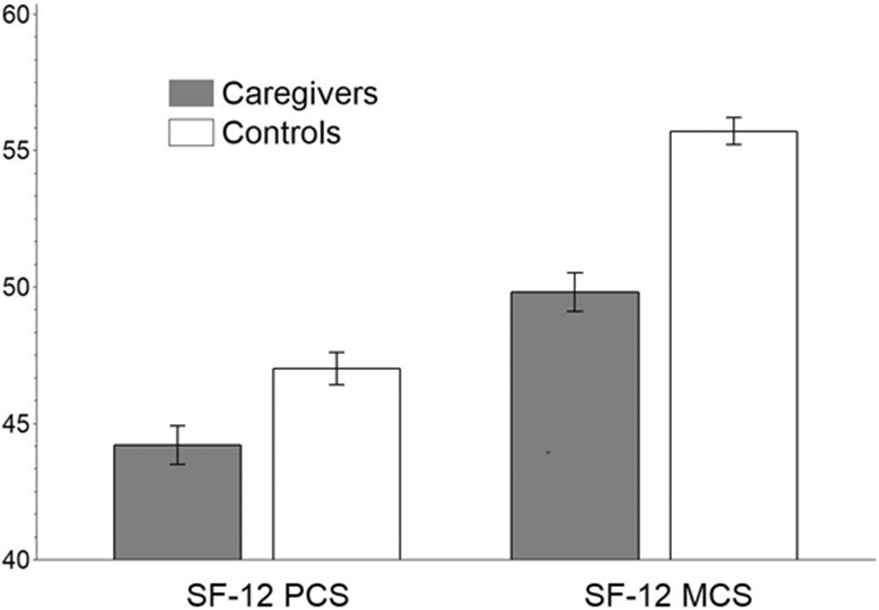
Means and Standard Errors of the Physical Component Summary (PCS) and Mental Component Summary (MCS) Measures of Health-Related Quality of Life for Incident Caregivers Compared to Matched Controls
Table 2 summarizes descriptive information for the 251 caregivers and compares caregivers who reported on the follow-up caregiving screening CATI that they were caring for a person with Alzheimer’s disease, another form of dementia, or serious memory problems (dementia caregivers) with all other caregivers. Among all caregivers, 47% were dementia caregivers, 51% were caring for spouses, 25% were caring for a parent or a parent-in-law, and 24% were caring for another family member or friend. Caregivers, on average, provided 43 hours of care per week. Care recipients ranged in age from 50 to 100 years.
Table 2.
Descriptive Comparisons of Dementia and Non-Dementia Caregivers
| Variable | Caregivers of Persons with Dementia |
Caregivers of Persons with Other Health Conditions |
P |
|---|---|---|---|
| N | 117 | 134 | --- |
| Gender, Female N (%) | 73 (62) | 90 (67) | 0.43 |
| Race, African American N (%) | 45 (38) | 45 (34) | 0.42 |
| Education, College graduate N (%) | 49 (42) | 57 (42) | 0.64 |
| Marital Status at Transitions Interview, N (%) | 0.88 | ||
| Married/Cohabiting | 89 (76) | 101 (75) | |
| Widowed | 9 (8) | 10 (7) | |
| Divorced/Separated | 13 (11) | 13 (10) | |
| Single / Never Married | 6 (5) | 10 (7) | |
| Caregiving Relationship, N (%) | 0.25 | ||
| Spouse | 56 (48) | 72 (54) | |
| Child (or Child-in-Law) of Care Recipient | 35 (30) | 28 (21) | |
| Parent of Disabled Adult Child Care Recipient | 5 (4.3) | 3 (2.2) | |
| Other | 21 (18) | 31 (23) | |
| Caregiver resides with Care Recipient, N (%) | 85 (73) | 100 (75) | 0.72 |
| Duration of Caregiving (to Transitions Interview), Years, M (SD) | 5.7 (2.4) | 5.8 (2.6) | 0.77 |
| Hours per week of care, M (SD) | 49.7 (29.4) | 37.7 (27.9) | 0.001 |
| Caregiver Age at Transitions interview, M (SD) | 73.1 (8.3) | 70.7 (7.7) | 0.016 |
| Care Recipient Age at Transitions Interview, M (SD) | 80.9 (11.3) | 76.8 (11.0) | 0.004 |
| AD8, M (SD) | 6.5 (1.6) | 2.8 (2.3) | <0.0001 |
Note. P-values are for group comparisons from Pearson chi-square tests when frequencies (N, %) are reported and from independent sample t-tests when means (M) and standard deviatons (SD) are reported.
Chi-square tests indicated that dementia and non-dementia caregivers did not differ on sex, race, education level, marital status, caregiving relationship, or whether the caregiver lived with the care recipient. There was no difference on the duration of caregiving, but dementia caregivers provided more hours of care and reported more symptoms of dementia in their care recipients on the AD8 than non-dementia caregivers. Dementia caregivers and their care recipients were also significantly older than non-dementia dyads.
Discussion
The CTS project has successfully identified a large sample of participants from the REGARDS study who were not caregivers at enrollment but have subsequently transitioned into a family caregiving role at some point over the course of their participation in that longitudinal study. The inclusion criteria for the CTS ensured that incident caregivers had substantial exposure to the potential stressors of caregiving because all were providing at least 5 hours of care per week and they averaged over 40 hours of care per week. The average duration of such care was nearly six years. Individually-matched non-caregiver control participants who were not caregivers at any point during their participation in the REGARDS study were also successfully identified and enrolled. These non-caregivers were carefully matched with the caregivers on demographic variables at baseline, and did not differ from those who subsequently became caregivers on initial depressive symptoms, perceived stress, self-reported health, or health-related quality of life.
Of the REGARDS participants who were not caregivers at baseline, 11% reported becoming caregivers by the follow-up Caregiving Screening CATI approximately 12 years later, but many of these individuals were ineligible for the CTS due to time frame of the caregiving (e.g., care not provided continuously for at least 3 months before the 2nd REGARDS in-home visit) or to insufficient exposure to caregiving activities (e.g., low hours of care per week). Thus, conducting a project of this type requires a substantial initial sample size in order to carefully screen out persons with minimal caregiving experiences or exposure to caregiving stressors. Our methods focused on rigorously enrolling only incident caregivers who were actively and consistently providing extensive care and non-caregiving comparison persons who reported no previous history of providing such care and who were individually matched with each caregiver on multiple demographic and health history variables. We considered other methods of matching, such as propensity score matching methods that we have used in previous research [20], but propensity score approaches only match on a composite of covariate information, and we believe that the specific matching on multiple individual covariates represents a more rigorous approach for the current prospective investigation.
As expected, incident caregivers reported significant increases in perceived stress and depressive symptoms and decreases in health-related quality of life after the onset of caregiving. Also consistent with previous literature [4, 6], caregivers of persons with dementia reported substantially more hours of care and more symptoms of cognitive decline in their care recipients than non-dementia caregivers.
Our unique matched samples of incident caregivers and non-caregivers will allow us to investigate several important research questions that are still unresolved from previous studies. In future analyses, we will compare the baseline and follow up biomarker profiles of participants in order to better characterize any pathophysiological effects of caregiving stress. We will examine within-person effects of the transition to caregiving for these biomarkers and other health-related variables that have been repeatedly shown to differ in cross-sectional analyses by caregiving status. We will contribute to an understanding of how factors such as dementia caregiving status, race, gender, and caregiver relationship are associated with caregivers’ health and well-being, and incorporate factors relevant to stress process models of family caregiving such as caregiving appraisals, perceived benefits of caregiving, and social support.
Concerns about the potential negative health effects of caregiving are widespread [37], and questions about caregiving are now included in major national studies of risk factors in the United States [38]. However, much of the evidence for the negative impact of family caregiving on physical health comes from cross-sectional studies of convenience samples, which have been shown to report more negative consequences from caregiving than population-based samples [4, 39]. Our population-based, prospective study of caregiving will provide an independent and rigorous examination of the health-related changes experienced by caregivers. The results should be useful for further informing healthcare providers and public policy about the true risks and possible rewards of taking on family caregiving responsibilities.
Funding:
This work was supported by a cooperative agreement [U01 NS041588] co-funded by the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institute on Aging (NIA), National Institutes of Health, Department of Health and Human Services; and by an investigator-initiated grant [RF1 AG050609] from the NIA.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NINDS or NIA. Representatives of the NINDS were involved in the review of the manuscript but were not directly involved in the collection, management, analysis, or interpretation of the data. The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
Footnotes
Conflicts of interest: On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval: The study was reviewed and approved by the Institutional Review Boards of the University of Alabama at Birmingham and each participating institution. The research procedures also conform to the principles of the Declaration of Helsinki.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Data availability
In cooperation with the Institutional Review Board (IRB) of the University of Alabama at Birmingham (UAB), the REGARDS project facilitates data sharing through formal data use agreements. Investigators who wish to access the data should send their requests to regardsadmin@uab.edu.
References
- 1.Allen AP, Curran EA, Duggan A et al. (2017) A systematic review of the psychobiological burden of informal caregiving for patients with dementia: Focus on cognitive and biological markers of chronic stress. Neurosci Biobehav Rev 73:123–164 [DOI] [PubMed] [Google Scholar]
- 2.Vitaliano PP, Young HM, Zhang J (2004) Is caregiving a risk factor for illness? Curr Dir Psychol Sci 13:13–16 [Google Scholar]
- 3.Schulz R, Eden J (2016) Families Caring for an Aging America. Washington, DC: The National Academies Press; [PubMed] [Google Scholar]
- 4.Pinquart M, Sörensen S (2003) Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychol Aging 18:250–267 [DOI] [PubMed] [Google Scholar]
- 5.Vitaliano PP, Zhang J, Scanlan JM (2003) Is caregiving hazardous to one's physical health? A meta-analysis. Psychol Bull 129:946–72 [DOI] [PubMed] [Google Scholar]
- 6.Ory MG, Hoffman III RR, Yee JL et al. (1999) Prevalence and Impact of Caregiving: A Detailed Comparison Between Dementia and Nondementia Caregivers. Gerontologist 39:177–186 [DOI] [PubMed] [Google Scholar]
- 7.Elmståhl S, Dahlrup B, Ekström et al. (2018) The association between medical diagnosis and caregiver burden: a cross-sectional study of recipients of informal support and caregivers from the general population study 'Good Aging in Skåne', Sweden. Aging Clin Exp Res 30(9):1023–1032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kiecolt-Glaser JK, Glaser R, Shuttleworth EC et al. (1987) Chronic stress and immunity in family caregivers of Alzheimer's disease victims. Psychosom Med 49:523–535 [DOI] [PubMed] [Google Scholar]
- 9.Gouin JP, Glaser R, Malarkey WB, et al. (2012) Chronic stress, daily stressors, and circulating inflammatory markers. Health Psychol 31(2):264–268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lovell B, Wetherell MA (2011) The cost of caregiving: endocrine and immune implications in elderly and non elderly caregivers. Neurosci Biobehav Rev 35:1342–1352. doi: 10.106/j.neubiorev.2011.02.007 [DOI] [PubMed] [Google Scholar]
- 11.von Kanel R, Dimsdale JE, Mills PJ et al. (2006) Effect of Alzheimer caregiving stress and age on frailty markers interleukin-6, c-reactive protein, and d-dimer. J Gerontol A Biol Sci Med Sci 61:963–969. doi: 10.1093/gerona/61.9.963 [DOI] [PubMed] [Google Scholar]
- 12.Potier F, Degryse JM, de Saint-Hubert M (2018) Impact of caregiving for older people and pro-inflammatory biomarkers among caregivers: a systematic review. Aging Clin Exp Res 30:119–32. doi: 10.1007/s40520-017-0765-0 [DOI] [PubMed] [Google Scholar]
- 13.Roth DL, Sheehan OC, Haley W et al. (2019) Is Family Caregiving Associated With Inflammation or Compromised Immunity? A Meta-Analysis. Gerontologist doi: 10.1093/geront/gnz015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schulz R, Beach SR (1999) Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. JAMA 282:2215–2219 [DOI] [PubMed] [Google Scholar]
- 15.Brown SL, Smith DM, Schultz R et al. (2009) Caregiving behavior is associated with decreased mortality risk. Psychol Sci 20:488–494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fredman L, Cauley JA, Hochberg M et al. (2010) Mortality associated with caregiving, general stress, and caregiving-related stress in elderly women: results of caregiver-study of osteoporotic fractures. J Am Geriatr Soc 58:937–943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O'Reilly D, Connolly S, Rosato M et al. (2008) Is caring associated with an increased risk of mortality? A longitudinal study. Soc Sci Med 67:1282–1290 [DOI] [PubMed] [Google Scholar]
- 18.O'Reilly D, Rosato M, Maguire A (2015) Caregiving reduces mortality risk for most caregivers: a census-based record linkage study. Int J Epidemiol 44:1959–1969. doi: 10.1093/ije/dyv172. doi: [DOI] [PubMed] [Google Scholar]
- 19.Roth DL, Fredman L, Haley WE (2015) Informal caregiving and its impact on health: a reappraisal from population-based studies. Gerontologist 55:309–319. doi: 10.1093/geront/gnu177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roth DL, Haley WE, Hovator M et al. (2013) Family caregiving and all-cause mortality: findings from a population-based propensity-matched analysis. Am J Epidemiol 178:1571–1578. doi: 10.1093/aje/kwt225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dich N, Lange T, Head J et al. (2015) Work stress, caregiving, and allostatic load: prospective results from the Whitehall II cohort study. Psychosom Med 77:539–547. doi? 10.1097/PSY.0000000000000191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Provinciali M, Moresi R, Muzzioli M et al. (2004) Psychological, neuroendocrine and immune measures in non spousal carers of disabled elderly in Italy. Neuro Endocrinol Lett 25:391–396 [PubMed] [Google Scholar]
- 23.Kang S, Marks NF (2014) Filial Caregiving is Associated with Greater Neuroendocrine Dysfunction: Evidence from the 2005 National Survey of Midlife in the U.S. SAGE Open Med 2. doi: 10.1177/2050312113520152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim S, Ferraro KF (2014) Do productive activities reduce inflammation in later life? Multiple roles, frequency of activities, and C-reactive protein. Gerontologist 54:830–839. doi: 10.1093/geront/gnt090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burton LC, Zdaniuk B, Schulz R et al. (2003) Transitions in spousal caregiving. Gerontologist. 43(2):230–41. doi: 10.1093/geront/43.2.230 [DOI] [PubMed] [Google Scholar]
- 26.Choi H, Marks NF (2006) Transition to caregiving, marital disagreement, and psychological well-being: a prospective u.s. national study. J Fam Issues 27:1701–1722. doi: 10.1177/0192513X06291523 [DOI] [Google Scholar]
- 27.Howard VJ, Cushman M, Pulley L et al. (2005) The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology 25:135–143. doi: 10.1159/000086678 [DOI] [PubMed] [Google Scholar]
- 28.Howard G, Safford MM, Moy CS et al. (2017) Racial Differences in the Incidence of Cardiovascular Risk Factors in Older Black and White Adults. J Am Geriatr Soc 65:83–90. doi: 10.1111/jgs.14472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roth DL, Perkin M, Wadley VG et al. (2009) Family caregiving and emotional strain: associations with quality of life in a large national sample of middle-aged and older adults. Qual Life Res 18:679–88. doi: 10.1007/s11136-009-9482-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Melchior LA, Huba GJ, Brown VB et al. (1993) A short depression index for women. Educational and Psychological Measurement 53:1117–1125. doi: 10.1177/0013164493053004024 [DOI] [Google Scholar]
- 31.Cohen S, Kamarck T, Mermelstein R (1983) A Global Measure of Perceived Stress. J Health Soc Behav 24:385–396 [PubMed] [Google Scholar]
- 32.Ware JE, Kisinski M, Keller SD (1996) A 12-item short form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care 34: 220–233 [DOI] [PubMed] [Google Scholar]
- 33.Jakobsson U (2007) Using the 12-item Short Form health survey (SF-12) to measure quality of life among older people. Aging Clin Exp Res 19:457–64 [DOI] [PubMed] [Google Scholar]
- 34.Gillett SR, Boyle RH, Zakai NA et al. (2014) Validating laboratory results in a national observational cohort study without field centers: the Reasons for Geographic and Racial Differences in Stroke cohort. Clin Biochem 47: 243–246. doi: 10.1016/j.clinbiochem.2014.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Irwin M, Artin KH, Oxman MN (1999) Screening for depression in the older adult: Criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D). Arch Intern Med 159:1701–1704 [DOI] [PubMed] [Google Scholar]
- 36.Galvin JE, Roe CM, Powlishta KK et al. (2005) The AD8 A brief informant interview to detect dementia. Neurol 65:559–564 doi: 10.1212/01.wnl.0000172958.95282.2a [DOI] [PubMed] [Google Scholar]
- 37.Talley RC, Crews JE (2007) Framing the public health of caregiving. Am J Public Health. 97:224–228. doi: 10.2105/AJPH.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Anderson LA, Edwards VJ, Pearson WS et al. (2013) Adult caregivers in the United States: characteristics and differences in well-being, by caregiver age and caregiving status. Prev Chronic Dis 10:E135. doi: 10.5888/pcd10.130090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pruchno RA, Brill JE, Shands Y et al. (2008) Convenience samples and caregiving research: How generalizable are the findings? Gerontologist 48:820–827 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
In cooperation with the Institutional Review Board (IRB) of the University of Alabama at Birmingham (UAB), the REGARDS project facilitates data sharing through formal data use agreements. Investigators who wish to access the data should send their requests to regardsadmin@uab.edu.