Abstract
Short-chain fatty acids (SCFAs), produced by colonic bacteria and obtained from the diet, have been linked to beneficial effects on human health associated with their metabolic and signaling properties. Their physiological functions are related to their aliphatic tail length and dependent on the activation of specific membrane receptors. In this review, we focus on the mechanisms underlying SCFAs mediated protection against oxidative and mitochondrial stress and their role in regulating metabolic pathways in specific tissues. We critically evaluate the evidence for their cytoprotective roles in suppressing inflammation and carcinogenesis and the consequences of aging. The ability of these natural compounds to induce signaling pathways, involving nuclear erythroid 2-related factor 2 (Nrf2), contributes to the maintenance of redox homeostasis under physiological conditions. SCFAs may thus serve as nutritional and therapeutic agents in healthy aging and in vascular and other diseases such as diabetes, neuropathologies and cancer.
Keywords: Short-chain fatty acids, Medium-chain fatty acid, Long-chain fatty acids, Redox signaling, Keap1-Nrf2, Epigenetics, Inflammation, Cardiovascular diseases, Neurodegenerative diseases, Cancer, Aging
Graphical abstract
Highlights
-
•
SCFAs are a link between the microbiota, redox signaling and host metabolism.
-
•
SCFAs modulate Nrf2 redox signaling through specific free fatty acid receptors.
-
•
Butyrate induces epigenetic regulation and/or Nrf2 nuclear translocation.
-
•
Butyrate and propionate protect the blood-brain barrier by facilitating docosahexaenoic acid transport.
-
•
Regulation of redox homeostasis by SCFAs supports their potential as therapeutic nutrients in health and disease.
List of abbreviations
- Aβ
amyloid β peptide
- AMPK
AMP-activated protein kinase
- BBB
blood-brain barrier
- BMECs
brain microvascular endothelial cells
- ARE
antioxidant response element
- cAMP
cyclic adenosine monophosphate
- CNS
central nervous system
- COX
cyclo-oxygenase
- DHA
docosahexaenoic acid
- EPA
eicosapentaenoic acid
- ERK1/2
extracellular-signal-regulated kinase 1/2
- FFA
free fatty acid
- FFAR
free fatty acid receptor
- GPR
G protein-coupled receptor
- GPx
glutathione peroxidase
- GSH
glutathione
- GSK-3β
glycogen synthase kinase-3β
- GST
glutathione S-transferase
- HAT
histone acetyltransferase
- HBMEC
human brain microvascular endothelial cells
- HDAC
histone deacetylase
- HO-1
heme oxygenase 1
- H3K9/14
histone H3 acetylated in lysine 9/14
- ICAM-1
intercellular adhesion molecule 1
- IEC-6
rat primary epithelial cells
- IL:
interleukin
- iNOS
inducible nitric oxide synthase
- JNK
Jun N-terminal kinase
- Keap1
Kelch-like ECH-associated protein 1
- LCFA
long-chain fatty acid
- LOX
lipoxygenase
- LPS
lipopolysaccharide
- LRP-1
LDL Receptor Related Protein 1
- MDA
malondialdehyde
- MAP kinase
Mitogen-activated kinase
- MCFA
medium-chain fatty acid
- MCP-1
monocyte chemotactic protein 1
- Mn-SOD
Mn-superoxide dismutase
- NaAc
sodium acetate
- NaB
sodium butyrate
- NaP
sodium propionate
- NF-κB
Nuclear factor kappa B
- Nlrp3
NOD-like receptor family pyrin domain containing 3
- NO
nitric oxide
- NOS
nitric oxide synthase
- NOX
NADPH oxidase
- NQ1
NAD(P)H:quinone oxidoreductase-1
- Nrf2
Nuclear erythroid 2-related factor 2
- n-3 PUFAs
omega-3 polyunsaturated fatty acids
- Olfr78
olfactory receptor 78
- P53
tumor suppressor p53
- PGC1-α
peroxisome proliferator-activated receptor γ co-activator 1 α
- PPARγ
peroxisome proliferator-activated receptor gamma
- ROS
reactive oxygen species
- SCFA
short-chain fatty acid
- SFN
sulforaphane
- SMCT1
sodium-coupled monocarboxylate transporter 1
- Sp1
specificity protein 1
- SOD
superoxide dismutase
- TCA
tricarboxylic acid cycle
1. Introduction
The key roles played by the major short-chain fatty acids (SCFAs) acetate, propionate and butyrate (commonly named as their anions) as mediators of the beneficial effects of dietary fibre and gut microbiota in human health has led to renewed interest in their mechanisms of action [1]. Here, we review in detail the in vitro and in vivo evidence supporting a role of SCFAs in regulating redox homeostasis, crosstalk between the redox sensitive Kelch-like ECH-associated protein 1 (Keap1)-Nrf2 signaling pathway and metabolism of free fatty acids (FFAs), and the novel roles that specific SCFAs play in activating Nrf2-regulated gene transcription (see Section 4 and Table 3, Table 4). We also address the beneficial effects of specific SCFAs on redox homeostasis under physiological and pathological conditions, and critically evaluate the potential of these biomolecules as nutritional and therapeutic targets in diseases such as diabetes, neuropathology and cancer.
Table 3.
SCFAs mediated activation of the Keap1-Nrf2 defense pathway protects against oxidative stress in vitro.
| Cell type | Species | SCFA | Treatment | key findings | References | |
|---|---|---|---|---|---|---|
| Endothelial | HBMEC | Human | Propionic | Propionate 1 μM 12–24h |
↓LRP-1 Protected BBB via Nrf2 signaling |
[49] |
| Fibroblast | BMECs mammary | Bovine | Butyric | NaB 2 mM, 1–12h | ↑ nuclear Nrf2 ↑H3K9/14ac ↓H2O2↓apoptosis through GPR109A/AMPK/Nrf2 |
[50] |
| Epithelial | IEC-6 | Rat | Butyric | NaB 2 mM, 24–48h | ↑ nuclear Nrf2 ↑GST, NQO1 ↓p53 |
[64] |
| Hepatocyte | HepG2 | Human | Butyric | NaB 0.3 mM 96h +800 μM H2O2, 4h |
↑ nuclear Nrf2 ↑HO1, NQ1 ↑MnSOD, GPx ↓ ROS ↓apoptosis ↓ GSK-3β ↓ glycolysis ↑β-oxidation ↑TCA |
[65] |
Abbreviations: AMPK: AMP-activated protein kinase; BBB: blood-brain barrier; BMECs: brain microvascular endothelial cells; FFAR2: Free fatty acids receptor 2; GPx: glutathione peroxidase; GSK-3β: glycogen synthase kinase-3β; GR109A: G-protein-coupled receptor; HO1: heme oxygenase-1; H3K9/14; histone H3 acetylated in lysine 9/14; HBMEC: human brain microvascular endothelial cells; ICAM-1: intercellular adhesion molecule 1; IEC-6: rat primary epithelial cells; IL-1β: interleukin 1 beta; LRP-1: LDL Receptor Related Protein 1; MCP-1: monocyte chemotactic protein 1; Mn-SOD: Mn-superoxide dismutase; NaB: sodium butyrate; NQ1: NAD(P)H: quinone oxidoreductase-1; Nrf2: nuclear erythroid 2-related factor 2; ROS: reactive oxygen species; TCA: tricarboxylic acid cycle.
Upward arrow (↑) indicates an increase and downward arrow (↓) a decrease in respective measured outcomes.
Table 4.
SCFAs afford protection against oxidative stress via activation of Keap1-Nrf2 pathway in animal models.
| Species | Strain/diet | SCFA | Treatment | Key findings | References |
|---|---|---|---|---|---|
| Rat | High-fat diet, 9 weeks | Butyric | NaB (300 mg/kg), every 2d, 7 weeks | ↓HDAC1 ↑H3K9ac Nrf2 promoter ↑Nrf2, SOD, GSH ↑Insulin signaling |
[91] |
| Obesity-prone rats | Butyric | 4% NaB, 12 weeks | Reversion of bone loss and body weight gain ↑nuclear Nrf2 ↑HO1, NQO1 ↑ Nrf2/GSK-3β signaling ↑ PGC-1α, TFAM |
[92] | |
| Mouse | C57BL/6 (Nrf2-/-) | Butyric | NaB (5 g/kg/day), 20 weeks | ↓ Renal oxidative damage ↓HDAC ↑Nrf2, HO1, NQ1 No Nrf2 nuclear translocation |
[93] |
| C57BL/6 with experimental autoimmune uveitis | Butyric | NaB orally (1 g/kg/day) 14d | ↓ Ocular inflammatory response ↓Th17 cells ↑Treg cells Nrf2/HO1 dependent |
[94] | |
| C57BL/6 (Nrf2-/-) diabetes-induced | Butyric | NaB (5 g/kg/day) 20 weeks | ↓ Aortic endothelial dysfunction Nrf2-dependent ↓HDAC ↑Nrf2 transcript and protein No significant Nrf2 nuclear translocation |
[66] |
Abbreviations: ERK: extracellular-signal-regulated kinase; FFAR2: free fatty acids receptor 2; GSH: glutathion; GPX2: glutathione peroxidase 2; GSK-3β: glycogen synthase kinase-3β; GR109A: G-protein-coupled receptor; HDAC1: histone deacetylase 1; HO1: heme oxygenase 1; H3K9ac; histone H3 acetylated in lysine 9/14; ICAM-1: intercellular adhesion molecule 1; IL-1β: interleukin 1 beta; JNK: Jun N-terminal kinase; LRP-1: LDL Receptor Related Protein 1; MCP-1: monocyte chemotactic protein 1; MDA: malondialdehyde; SOD1-3: superoxide dismutase 1–3; NaB: sodium butyrate; NQ1: NAD(P)H: quinone oxidoreductase-1; Nrf2: nuclear erythroid 2-related factor 2; PGC1-α: peroxisome proliferator-activated receptor γ co-activator 1 α; p38: mitogen activated (MAP) kinase p38.
Upward arrow (↑) indicates an increase and downward arrow (↓) a decrease in respective measured outcomes.
1.1. SCFAs signaling functions
Short-chain fatty acids, mainly produced by colonic bacteria, have been linked with benefits for human health due to their metabolic and signaling properties [2]. The specific physiological functions of this type of fatty acid are related to their aliphatic tail length. FFAs are classified based on their carbon chain length, with SCFAs having <6 carbon atoms, MCFAs 6–12 carbons atoms and long-chain fatty acids (LCFAs) more than 12 carbon atoms (see Table 1).
Table 1.
Nomenclature and structure of SCFAs.
| Number of carbon atoms | Systematic name | Common name | Common anion name | Structure | Simplified formula |
|---|---|---|---|---|---|
| 2 | Ethanoic | Acetic | Acetate |  |
(C2:0) |
| 3 | Propanoic | Propionic | Propionate |  |
(C3:0) |
| 4 | Butanoic | Butyric | Butyrate |  |
(C4:0) |
| 5 | Pentanoic | Valeric | Valerate |  |
(C5:0) |
FFAs are versatile molecules involved in many physiological functions in mammals. In addition to their well characterized structural and metabolic roles, recent evidence highlights their involvement in cell signaling in a wide range of physiological and pathological conditions [3,4]. Evidence for a role of SCFAs in organs outside the digestive system stems from the fact that numerous transmembrane proteins, receptors and transporters, that specifically bind SCFAs and other monocarboxylic acids, are expressed in a large variety of cell types, including neurons [5,6]. For example, butyrate and other fermentation or diet derived SCFAs like acetate and propionate have shown promising effects in various diseases including obesity, diabetes, inflammatory (bowel) diseases, and colorectal cancer as well as neurological disorders [7].
The health benefits of FFAs have been associated in part with their capacity to regulate metabolic, inflammatory, and neural pathways by maintaining energy homeostasis [8]. Interestingly, as discussed in this review, microbiota metabolites and epigenetic regulation may form the basis of future research (see Section 6).
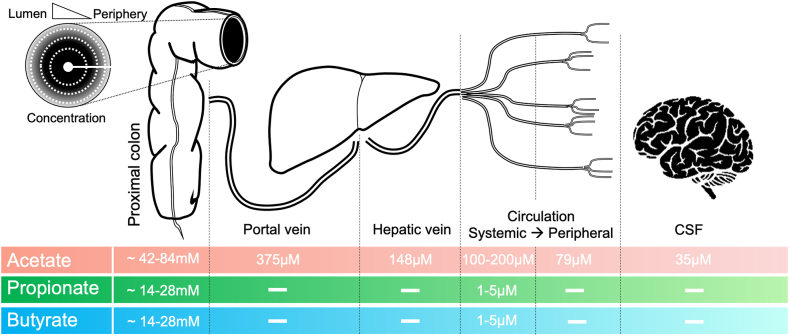
2. Role of SCFAs in energy and anabolic metabolism
SCFAs are important substrates for energy metabolism and anabolic processes in mammals, and there is evidence that diet-driven changes in microbiota diversity lead to variations in SCFAs [9]. Acetate, propionate, and butyrate are the main SCFAs formed in the human colon at an estimated ratio of about 3:1:1 [10], reaching the highest concentrations (70–140 mM) in the proximal colon [11], with a concentration gradient falling from the lumen to the periphery [12] (see Fig. 1). These SCFAs are absorbed from the gut into the hepatic portal circulation and/or lacteal lymphatic system, with total concentrations ranging from 375 μM to 148 μM in portal and hepatic blood, respectively, to 79 μM in peripheral blood [11,13]. Butyrate and propionate, mostly metabolized by hepatocytes, appear at 1–15 μM in the systemic circulation, with acetate ranging between 100 and 200 μM [14,15]. Of relevance to aging (see Section 8), only acetate has been detected in cerebrospinal fluid at around 35 μM [16]. While the significance of these biological gradients is poorly understood, they may be critical in defining physiologically relevant roles of specific SCFAS during immune and inflammatory responses [17]. This is particularly important for clinical translation of findings in animal models, which often utilize oral SCFAs supplementation or high dietary fibre supplementation to induce changes in SCFAs production [18].
Fig. 1.
Schematic illustrating the origin of SCFAs and their target tissues. Gradient concentration of SCFAs between gut lumen and periphery is illustrated.
Notably, mother's milk constitutes an important source of SCFAs for new-born mammals in the form of triglycerides and phospholipids, while animal milk and milk products constitute the main dietary source of SCFAs, mainly butyrate, in adult humans [19]. SCFAs can also be formed in the mammalian liver through the peroxisomal β-oxidation of long-chain fatty acids (LCFAs) [20].
A feature of SCFAs that distinguishes them from LCFAs is that they are rapidly absorbed in the intestine due to their water solubility and transported via the hepatic portal bloodstream to the liver, where they are readily metabolized instead of being stored as fat [9,19]. SCFAs modulate tissue metabolism of carbohydrates and lipids by inhibiting glycolysis and stimulating lipogenesis and gluconeogenesis [21]. However, the traditional view that FFAs serve as metabolic substrates only during carbohydrate restriction has been revised based on observations that ketone bodies play pivotal roles as signaling mediators, drivers of protein post-translational modification and modulators of inflammation and oxidative stress when carbohydrates are abundant [22]. The antioxidant and oxidative stress-mitigating roles of ketone bodies have been widely described in the context of neuroprotection, cardio-protection and cancer [23] and will not be reviewed further.
3. Molecular mechanisms underlying SCFAs signaling: free fatty acid receptors
The regulatory functions of SCFAs depend on specific receptors expressed in different cell types, as well as their developmental stage and differentiation process [5,6]. In vitro and in vivo studies have shown that the physiological functions of free fatty acid receptors (FFARs) contribute not only to the regulation of metabolic energy but also affect the immune system [24]. These transmembrane receptors are members of G protein-coupled receptors (GPR) that detect extracellular molecules and then activate intracellular signal transduction pathways to promote cellular responses [25].
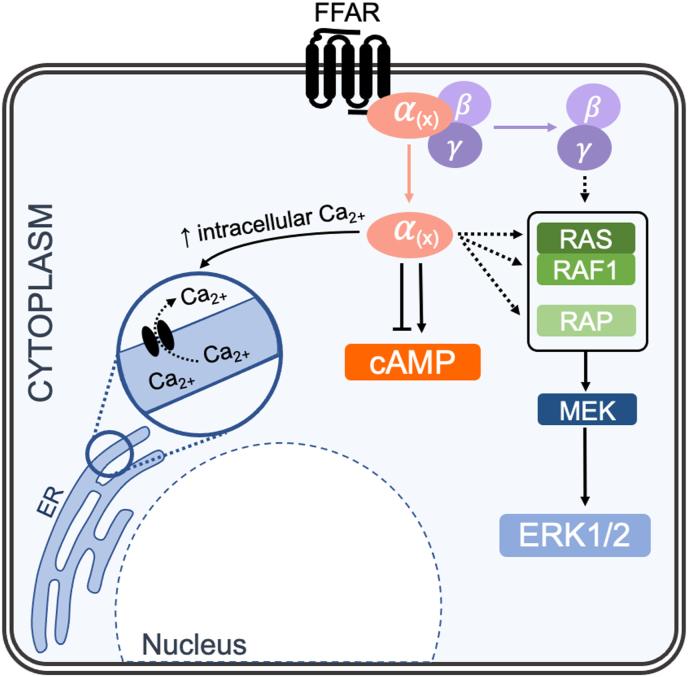
FFARs are activated by free fatty acids with different carbon chain lengths and, under physiological conditions, several FFAs can activate the same receptor, whereas one FFA can activate several FFARs. In fact, SCFAs are ligands of FFAR2/GPR43 and FFAR3/GPR41, but the former is preferentially activated by C3:0-C6:0 and the latter by C2:0-C4:0. Notably, long-chain fatty acids activate both FFAR1/GPR40 and FFAR4 (GPR120), whereas medium chain fatty acids (C6:0-C12:0) can also activate FFAR1/GPR40 5. In addition, several FFAs are able to activate specific receptors, such as propionic (C3:0) (Olfr78), butyric (C4:0) (GPR109A), and capric (C10:0) and lauric (C12:0) acids (GPR84) (see Table 2 and Fig. 2). Kimura et al. (2020) have recently described FFARs in detail, and we refer readers to their comprehensive and elegant review [5].
Table 2.
SCFA receptors and ligand specificity.
| Acetic (C2:00) | Propionic (C3:0) | Butyric (C4:0) | Pentanoic (C5:0) | |
|---|---|---|---|---|
| FFAR3 (GPR41) | ++ | + | ++ | ++ |
| FFAR2 (GPR43) | ++ | ++ | ++ | + |
| GPR109A | ++ | |||
| Olfr78 | ++ | + |
Abbreviations: FFAR1: free fatty acid receptor 1; FFAR2: free fatty acid receptor 2; FFAR3: free fatty acid receptor 3; GPR40: G protein-coupled receptor 40; GPR41: G protein-coupled receptor 41; GPR43: G protein-coupled receptor 43; GPR109A: G protein-coupled receptor 109 A; olfr78: olfactory receptor 78. Note + and ++ denote low and high affinity, respectively [5,6].
Fig. 2.
Main signaling pathways of the free fatty acid receptors (FFARs). cAMP: cyclic adenosine monophosphate; ER: endoplasmic reticulum; ERK1/2: extracellular-signal-regulated kinase 1/2; FFAR: free fatty acid receptor; RAS: GTPase rat sarcoma virus; RAF1: Raf kinase 1; RAP: Ras related protein; MEK: mitogen-activated protein kinase kinase.
Depending on the type of α subunit of the heterotrimeric proteins associated with the FFARs, the reported physiological function of FFARs mainly involves activation of intracellular calcium (Ca2+), cyclic adenosine monophosphate (cAMP) or extracellular-signal-regulated kinase 1/2 (ERK1/2) signaling, via G protein (Gq or Gi/o)-dependent or G protein-independent pathways [25,26]. Furthermore, there is evidence supporting functional redundancy of FFARs that might contribute to maintenance of fatty acid homeostasis under different physiological conditions [5].
4. Protective role of SCFAs against oxidative and mitochondrial stress involving Keap1-Nrf2 signaling
The health benefits of redox signaling have been defined as “oxidative eustress”, whereas the deleterious outcomes in pathophysiology and disease due to higher levels of reactive oxygen species (ROS) is referred to as “oxidative distress” [27]. Under physiological conditions, different ROS play key roles in redox signaling via different post-translational modifications, therefore controlling specific ROS-mediated signaling pathways offers a strategy for refining future redox medicine [28,29].
The evidence that living organisms have developed mechanisms for the advantageous use of free radicals revealed the biological relevance of redox regulation in health and disease [30]. One of the main sources of cellular ROS are mitochondria which constitute a metabolic hub facilitating crosstalk between the metabolic state of the cell with relevant signaling pathways, including those regulating immune responses [31]. Notably, mitochondrial ROS serve as an alarm of extracellular environment changes that in small amounts can promote adaptation to the stressor but in larger quantities produce cell damage and subsequent cell death [32]. Therefore, the original concept of oxidative stress is linked to cellular energy balance, has led to characterization of compartmentation of redox processes and the spatiotemporal organization of hydrogen peroxide metabolism and its relationship to bioenergetics [33]. Discovery of the role of Keap1-Nrf2 system as the major regulator of redox homeostasis has informed new approaches to improve human health and combat diseases [34].
4.1. Natural compounds acting as regulators of cellular redox homeostasis via Nrf2 signaling
Several health benefits of SCFAs and other food derived non-nutrient molecules are related to their ability to modulate gene expression and thereby influence intracellular signaling pathways [35]. Plant-derived compounds can activate signaling pathways involved in the maintenance of cellular redox homeostasis [36,37]. One of the best characterized targets of pharmacological and/or dietary interventions is nuclear erythroid 2-related factor 2 (Nrf2), a master regulator of cellular antioxidant defenses controlling more than 200 genes [34,[38], [39], [40], [41], [42], [43]]. Under quiescent conditions, Nrf2 is sequestered by its cytosolic repressor Keap1 (Kelch-like ECH-associated protein 1), promoting rapid proteasomal degradation via ubiquitination, whereas oxidative and electrophilic stress promote nuclear accumulation of de novo synthesized Nrf2, which together with small Maf proteins binds to the antioxidant response element (ARE) in the promoter of target genes to upregulate phase II and antioxidant enzymes to counteract oxidative stress [38,[40], [41], [42],44]. Thus, current research in this field is focused on identifying biomolecules with significant nutrigenomic potential and efficacy as activators of Nrf2 [45,46]. Among them, broccoli-derived sulforaphane (SFN) is the most potent inducer of Nrf2-targeted cytoprotective genes [39,47,48]. As discussed in this section, specific SCFAs such as butyrate and propionate are activators of the Keap1-Nrf2 defence pathway [49,50] and lipid metabolism is regulated by Nrf2 [51,52].
4.2. Crosstalk between Nrf2 and lipid metabolism
Despite the regulatory functions reported for the main gut microbiome fermentation products acetate, propionate and butyrate, their role in influencing cellular redox homeostasis is currently not well understood [53]. Nrf2 is a major regulator of cellular metabolism in normal, stressed and cancer cells directing the transcription of the metabolic processes [52]. There is increasing evidence that Nrf2 participates in hepatic fatty acid metabolism, suppressing fatty acid synthesis and desaturation [54,55]. Notably, Notch signaling, which enables regulation and control of development, differentiation, and homeostasis through cell-cell communication has been identified as a novel regulator of fatty acid transport across the endothelium [56], and the ROS-Nrf2-Notch pathway seems key for cellular homeostasis [57].
4.3. Specific SCFAs protect against oxidative damage via the Keap1-Nrf2 pathway
SCFAs have been screened for protection against oxidative damage, and the molecular mechanisms underlying this effect and the physiological significance are beginning to be elucidated [58]. In this section, we focus on their role in regulating the Keap1-Nrf2 pathway. Of relevance, targeting the Keap1-Nrf2 signaling pathway using pharmacological and/or dietary interventions has been shown to protect against oxidative stress induced vascular damage in ischemic stroke, gestational diabetes and atherosclerosis as well as other chronic diseases [38,[59], [60], [61], [62], [63]].
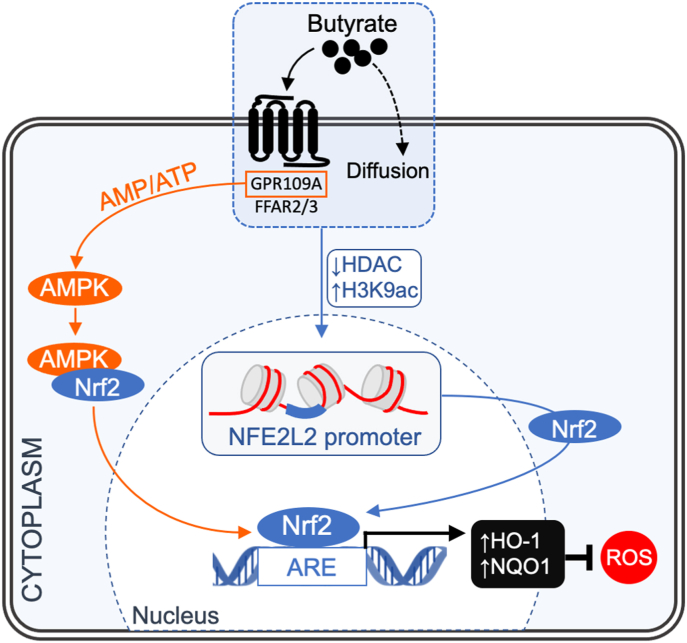
In Table 3, Table 4, we summarize selected cell culture and animal studies in vivo supporting an antioxidant role for specific SCFAs as modulators of Nrf2 redox signaling, with the majority of studies focused on butyrate. In both type of studies, epigenetic regulation involving histone deacetylases (HDACs) and/or Nrf2 nuclear translocation induced by butyrate are the main reported mechanisms of action.
Notably, studies in Nrf2 knockout mice with induced diabetes showed that butyrate mediates protection against endothelial dysfunction by P300 mediated activation of Nrf2 via inhibition of HDAC while, under the same conditions, SFN facilitates Nrf2 nuclear translocation [64]. Recent evidence in bovine epithelial cells implicated GPR109A inactivation of AMPK signaling by butyrate to promote Nrf2 nuclear accumulation [50]. In this case, butyrate also induced epigenetic modification on the Nrf2 promoter associated with synergistic antioxidant effects. Interestingly, in rat intestinal epithelial cells butyrate, in addition to enhancing antioxidant activities via Nrf2, decreased mRNA and protein levels of the tumor suppressor p53 [65], supporting crosstalk between p53 and Nrf2 in the regulation of cellular redox homeostasis [[66], [67], [68]].
Relatively few studies investigating the antioxidant roles of SCFAs have focused on propionate, despite its similar plasma concentration and receptor affinity [69]. Hoyles et al. (2018) demonstrated the expression of the receptor FFAR3 in human brain endothelium and determined that a physiologically relevant propionate concentration (1 μM) protected the blood-brain barrier (BBB) against oxidative stress via Nrf2 signaling [49]. Notably, acetate, propionate and butyrate can cross BBB, affecting BBB integrity and transport rates by reducing permeability and regulating the expression of tight junction proteins [70]. A study using a germ-free mouse model suggested that the microbiota and its metabolites (especially butyrate) can upregulate tight junctional protein expression in the BBB, thereby regulating the interaction between the periphery and the central nervous system (CNS) [71]. This beneficial effect of specific SCFAs on the BBB may affect the transport of molecules such as docosahexaenoic acid (DHA), an omega-3 fatty acid highly enriched in brain, that is essential for normal brain growth and cognitive function and inhibits inflammation in endothelial cells to reduce cardiovascular risk [72,73]. DHA cannot be synthesized de novo in the brain and must be supplied from the blood via specific transporters like the major facilitator super family domain containing 2a (Mfsd2a) and/or through passive diffusion across the endothelial membrane [74,75].
DHA in the plasma is found esterified with phospholipids and other lipids and its uptake into the brain seems to involve endothelial lipase [76]. The significant enrichment of DHA within the brain must be regulated by a number of additional pathways associated with the activation and metabolism of DHA. Once in the brain, DHA is esterified into membrane phospholipids, being released and converted to bioactive mediators during neurotransmission and following brain injury [77]. The antioxidant properties of DHA and its metabolites, resolvins, neuroprotectins and 4-hydroxy-2E-hexenal, are mediated by Nrf2 activation and involve upregulation of heme oxygenase 1 (HO-1) to protect the brain against ischemic damage [[78], [79], [80]]. Post-stroke administration of DHA is effective in reducing brain injury [[81], [82], [83]] and improving sensorimotor function [84,85]. Notably, stroke lowers blood SCFA concentrations, and SCFA supplementation has been reported to reduce damage following post-stroke reperfusion [[86], [87], [88], [89]]. As SCFAs improve functional outcomes after stroke, further research focused on their link with neuroprotective functions of Nrf2 and DHA is warranted.
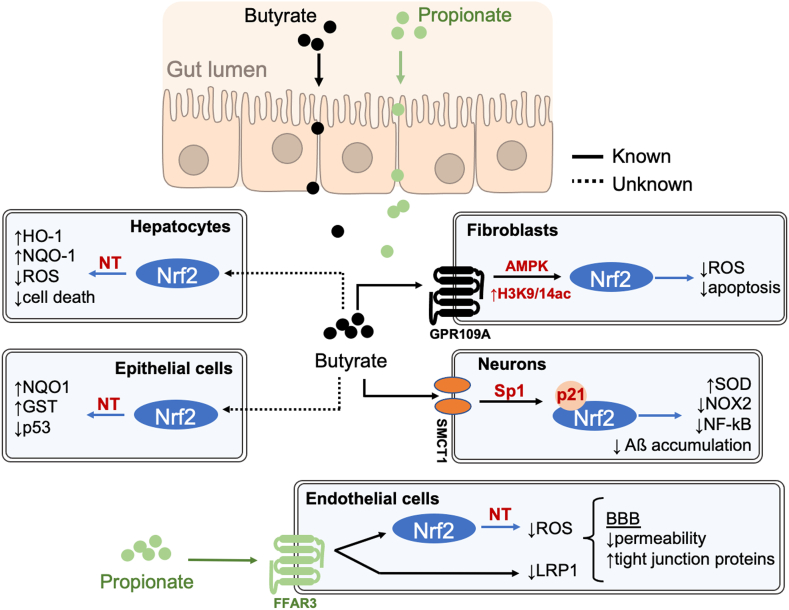
The experimental data summarized in Table 3, Table 4 provide convincing evidence that SCFAs, in particular butyrate but also propionate, by direct or indirect mechanisms, activate the Keap1-Nrf2 signaling pathway to maintain redox homeostasis under physiological conditions (see Fig. 3).
Fig. 3.
Schematic illustrating the mechanisms underlying modulation of the Keap1-Nrf2 defense pathway by butyrate: HDAC inhibition, Nrf2 nuclear translocation. AMPK: AMP-activated protein kinase; ARE: antioxidant response element; GPR109A: G-protein-coupled receptor; FFAR2/3: free fatty acids receptor 2/3; H3K9ac histone H3 acetylated in lysine 9: HDAC: histone deacetylase; HO-1: heme oxygenase 1; Nrf2: nuclear erythroid 2-related factor 2; NQO1: NAD(P)H: quinone oxidoreductase-1; ROS: reactive oxygen species.
Considering that butyrate is a fatty acid oxidized in mitochondria and acts as a signal transduction molecule via FFAR2, FFAR3 and GPR109A, it is reasonable to postulate its involvement in energy and redox homeostasis via the Nrf2 pathway.
Thus, specific SCFAs produced by microbial fermentation or provided in the diet, contribute to host redox homeostasis via epigenetic regulation and/or promoting Nrf2 nuclear translocation, highlighting an interesting link between the microbiota, redox signaling and host metabolism.
5. Anti-inflammatory properties of SCFAs related to antioxidant signaling
SCFAs play an important role in beneficial effects of dietary fibre and gut microbiota, through regulation of inflammation in the gut and other organs [90]. In fact, SCFAs may suppress inflammation by reducing migration and proliferation of immune cells, reducing cytokine levels and inducing apoptosis, but marked changes in SCFAs concentrations in blood or tissues can also cause immunological and metabolic imbalances [17]. Therefore, appropriate concentrations of SCFAs are needed to maintain normal metabolism and in the prevention and treatment of disease [24]. Table 5 includes selected experiments showing that treatment with SCFAs can activate cellular antioxidant mechanisms and downregulate pro-inflammatory mediators.
Table 5.
Anti-inflammatory effects of SCFAs under cell culture conditions.
| Cell type | Species | SCFA | Treatment | Key findings | References | |
|---|---|---|---|---|---|---|
| Endothelial | EOMA | Mouse | Butyric | 1 mM NaB, 2h | ↓O2−.↓Nlrp3 | [96] |
| Immune system | Macrophage | Rat | Butyric | 3 mM NaB, 24h | ↓HDAC↓Il-6↓NO | [97] |
| BMDM | Mouse | Butyric | 1 mM NaB, 24h | ↓HDAC↓Nos2↓NO↓IL-6 | [98] | |
| Myoblast | L6 | Human | Butyric | 5 mM NaB, 24h | ↓HDAC↑SOD2↑Catalase↑FOXO3a↑PGC1α | [99] |
| Glomerular mesangial | SV-40 MES 13 | Mouse | AceticButyric | 25 mM NaAc, 5 mM NaB, 24h | ↓ROS↓MDA↑SOD↓IL-1β | [100] |
Abbreviations: BMDM. Bone-marrow-derived macrophage; CCL2: chemokine (C–C motif) ligand 2; EOMA: Hemangioendothelioma; GSH: glutathione; HDAC: histone deacetylases; IL-6: interleukin 6; IL-8: interleukin 8; IL-1β: interleukin 1 beta; iNOS: inducible nitric oxide synthase; LPS: lipopolysaccharide; MDA: malondialdeyde; NaAc: sodium acetate; NaB: sodium butyrate; Nlrp3: NOD-like receptor family pyrin domain containing 3; NO: nitric oxide; Nos2: nitric oxide synthase 2; O2−: superoxide ion; SCFA: short chain fatty acid; ROS: reactive oxygen species; SOD: superoxide dismutase.
Upward arrow (↑) indicates an increase and downward arrow (↓) a decrease in respective measured outcomes.
SCFAs are generally considered to have beneficial effects in cardiovascular disease, and studies in different animal models report inhibitory effects of butyrate on NLRP3 inflammasome formation associated with activation of antioxidant signaling pathways [91,92]. Notably, treatment of endothelial cells with low concentrations of SCFAs does not disrupt barrier integrity under inflammatory conditions and moreover increases mitochondrial respiratory capacity [93,94]. In addition, butyrate plays an important role in the assembly of tight junctions in intestinal and vascular endothelial cells by inducing cyclo-oxygenase (COX), lipoxygenase (LOX) and reducing inducible NO synthase (iNOS) [95,96]. These findings suggest that supplementation of SCFAs, especially butyrate, may serve as therapeutic nutrients for inflammatory diseases due to their contribution to redox homeostasis.
The anti-inflammatory effects of butyrate and other SCFAs are partly achieved through HDAC inhibition [97,98]. Notably, butyrate modulates immune responses in intestinal macrophages via the reduction of NO due to inhibition of iNOS and decreased activation of nuclear NF-kB [99]. In rats, butyrate inhibition of HDAC leads to downregulation of secondary response genes like Nos2 and Il6 [100]. Thus, butyrate may behave as a microbial signal to maintain host immunity [101]. It is important to note that the beneficial effects of SCFAs-mediated HDAC inhibition may depend not only on the concentration of SCFAs but also on the target tissue or cell type [102].
The demonstrated redox signaling roles of specific lipids underpins the importance of emerging metabolomics and redox lipidomics for diagnosis and therapeutics [103,104]. In addition, systems-level models that permit interpretation of big data, particularly those that account for multiple interactions between metabolic intermediates, are necessary to understand the scope, scale, and complexity of effectors and targets of redox metabolism [29,105].
6. Protective effects of SCFAs on redox dysregulation in disease
In recent years, both human and animal experiments have revealed that gut microflora dysbiosis can accelerate the progression of cardiovascular diseases [106], diabetes [107], and neurodegenerative diseases [108], with SCFAs playing a key role. Gut dysbiosis and increased gut permeability are associated with heightened levels of oxidative stress [109]. Although our understanding of gut microbiota-host interactions has advanced significantly, many questions remain concerning the mechanistic links between the gut microbiome and host diseases, in particular those related with redox dysregulation [58].
In Table 6, we have selected reports that illustrate the effect of specific SCFAs on redox homeostasis in different pathological conditions. For example, mice receiving dietary butyrate supplementation exhibit reduced oxidative stress, attenuated endothelial dysfunction, and decreased aortic atherosclerotic lesions [18]. In rat aortic cells, butyrate and acetate, at pharmacological concentrations (5–10 mM), also improve endothelial dysfunction induced by angiotensin II by stimulating NO production and decreasing NADPH oxidase and mitochondrial ROS generation [110].
Table 6.
Protective effects of SCFAs in animal models of cardiovascular diseases and diabetes.
| Species | Animal model | SCFA/MCFA | Treatment | Key findings | References |
|---|---|---|---|---|---|
| Mouse | (ApoE−/-) mice | Butyric | 1% NaB, orally10 weeks | ↓ Lesion area in aorta↓SOD↓Protein nitrosylation | [18] |
| HFD-induced obese | Butyric | 100 mg/kg NaB,6 weeks | ↑GSH↑GST↑NQO1↓H2O2 | [109] | |
| Non-obese type 2 diabetic MKR | Butyric | 20 mg/kg NaB,8 weeks | ↓HDAC3↓NOX4↓IL-1β | [110] | |
| HFD-induced obese SK-N-MC cells | Butyric | 0.5 mM NaB,30 min | ↑Sp1-p21/Nrf2↓NOX2↑SOD1↓ROS↓NF-kB↓Aβ accumulation | [111] |
Abbreviations: Aβ: amyloid β peptide; GSH: glutathione; GST: glutathione S-transferase; HDAC3: histone deacetylase 3; HFD: high fat diet; H2O2: hydrogen peroxide; IL-1β: interleukin 1 beta; NF-kB: nuclear factor kappa B; NOX2: NADPH oxidase 2; NOX4: NADPH oxidase 4; NQO1: NAD(P)H: quinone oxidoreductase-1; Nrf2: nuclear erythroid 2-related factor 2; p21: transcription factor p21; ROS: reactive oxygen species; SK-N-MC cells: human neuroblastoma cells; SOD: superoxide dismutase; Sp1: specificity protein 1.
Upward arrow (↑) indicates an increase and downward arrow (↓) a decrease in respective measured outcomes.
Butyrate and its synthetic derivative, N-(1-carbamoyl-2-phenyl-ethyl) butyramide (FBA), protect mice against insulin resistance and liver steatosis by acting on hepatic mitochondria, reducing lipid accumulation and oxidative stress [111]. In a recent study in mice with type 2 diabetes mellitus, dysbiosis was associated with a reduction in butyrate-forming bacteria coupled to a decrease in cecal and fecal butyrate content leading to increased activity of the colon HDAC3 [112]. Butyrate treatment also reduced inflammatory markers and ROS production, a mechanism of action previously discussed in Section 5.
Acetate has been reported to improve the viability of islets and the mouse insulinoma cell line MIN6 subjected to oxidative stress by enhancing metabolism of ROS, whilst butyrate promotes “oxidative eustress” by inhibiting FFAR2 and NO generation [113]. These findings suggest that SCFAs play an essential role in supporting β-cell metabolism and promoting survival under stressful conditions contributing to reduce diseases such as diabetes. Interestingly, acetate, propionate and butyrate recapitulate chromatin modification states and transcriptional responses associated with gut microbiota in multiple murine tissues [114]. Notably, accumulating evidence indicates that the beneficial effect of these SCFAs in obesity and diabetes are related to their influences on host epigenetics [115]. In fact, butyrate and propionate protect against diet-induced obesity in mice by regulating gut hormones via FFAR3-independent mechanisms [116].
Oxidative stress is also linked to the etiology of many neurodegenerative diseases such as Alzheimer's disease (AD), Amyotrophic lateral sclerosis, Friedreich's ataxia, Huntington's disease, Multiple sclerosis, and Parkinson's disease [117]. Interestingly, there are data linking regulation of redox homeostasis by specific SCFAs with the development of neurodegenerative diseases, constituting an interesting target for pharmacological interventions in psychiatric disorders [118]. In fact, while many studies have shown that saturated long chain fatty acids (C:20-C:26) increase the risk of AD by promoting amyloid-β peptide (Aβ) generated oxidative stress [119], SFCAs can activate Nrf2 and thereby prevent Aβ accumulation [120]. Recent studies have reported a link between butyrate and Nrf2 in protection against high cholesterol-induced neuronal amyloidogenesis in mice [121]. Obesity increases Aβ accumulation in the brain and reduces butyrate-producing bacteria, and notably butyrate treatment has been reported to decrease expression levels of beta-site amyloid precursor protein cleaving enzyme 1 (BACE1) and Aβ accumulation. In this study, butyrate taken up by cells via a sodium-coupled monocarboxylate transporter 1 (SMCT1), prevented excessive ROS generation by inhibiting NOX2 and upregulating SOD1, following activation of the cyclin-dependent kinase inhibitor 1 (p21)/Nrf2 pathway through acetylation of Sp1. Notably, in mouse microglia, DHA suppresses Aβ-induced ROS production by upregulating the Nrf2/HO-1 pathway [122]. These results highlight that SCFAs link the microbiota with the maintenance of host redox homeostasis through Nrf2 signaling via mechanisms that may involve omega-3 fatty acids, as discussed in Section 4. The experimental data reviewed in this and other sections highlight redox signaling roles of butyrate and other SCFAs and their potential as therapeutic nutrients alone or in combination with other treatments.
Human trials suggest that many biological effects may be mediated by SCFAs (see Table 7), and, as shown, promising in vitro and animal studies have been published, albeit they cannot easily be extrapolated to humans [123]. Although the interplay of SCFAs with the gut microbiome and the associated immune system as well as the role of SCFAs in the gut-brain connection has been established [24,124], a better understanding of the mechanism of action of FFAs will facilitate translation for control and prevention of metabolic diseases.
Table 7.
Clinical trials assessing the impact of supplementation with SCFAs.
| Patients | SCFA | Treatment/Time | Major results | References |
|---|---|---|---|---|
| 10 patients with distal ulcerative colitis | Butyrate | 100 mM NaB, 2 weeks + placebo 2 weeks | NaB irrigation ameliorated distal ulcerative colitis | [121] |
| 30 patients with diverticulitis/22 controls | Butyrate | 300 mg/day NaB, 12 months | Microencapsulated NaB reduced clinical diverticulitis incidence | [122] |
| 13 overweighted and obese men | Acetate Propionate Butyrate |
40–120 mM NaAc, NaP, NaB, 12h | Acute rectal administration of SCFAs modulates whole-body substrate and energy metabolism, with an increase in fasting fat oxidation and resting energy expenditure | [123] |
Abbreviations: NaAc: sodium acetate; NaB: sodium butyrate; NaP: sodium propionate; SCFAs: short chain fatty acids.
7. Lessons from the plant immune system
The health benefits of specific FFAs discussed in this review implicate plant-derived compounds in the maintenance of mammalian cellular redox homeostasis [125]. The fact that specific FFAs act as Nrf2 regulators suggests that plant-derived compounds may serve as natural redox regulators [126]. The FFA hexanoic acid (C6:0) is particularly interesting, because it is a natural priming agent that protects plants against a wide range of pathogens inducing defense mechanisms and controlling plant redox homeostasis [127]. This FFA was considered a SCFA in previous classifications, and in fact acts as ligand of the SCFA receptor FFAR3 and the MCFA receptor FFAR1 in mammalian cells [5]. There are reports demonstrating that treatment of endothelial cells with hexanoic acid improves energy production and attenuates pro-inflammatory cytokine generation [94], with no effects on endothelial barrier integrity [93]. Moreover, hexanoic acid has anti-proliferative and anti-inflammatory properties in mammalian cells [128,129].
Of relevance, hexanoic acid protects tomato plants against infection by the necrotrophic pathogen Botrytis cinerea by regulating GSH levels and potentiating redox-sensitive genes encoding GSTs, peroxiredoxins and glutathione reductase amongst others [130]. Notably, the activation of redox-related genes by this priming agent closely resembles that induced by sulforaphane (SFN) in the preconditioning of mammalian cells [131,132]. In plants, SFN is a secondary metabolite, contributing to the hypersensitive response as well as priming defense genes to protect against biotic stresses [133]. In Arabidopsis plants, treatment with SFN protects against Hyaloperonospora arabidopsidis inducing histone epigenetic modifications in the promoter of defense genes [134]. Therefore, the mechanisms of action of the FFA hexanoic acid and SFN in priming plants resemble those reported for butyrate and SFN in the preconditioning of mammalian cells, supporting conservation of redox-activated pathways.
8. Conclusions and future perspectives
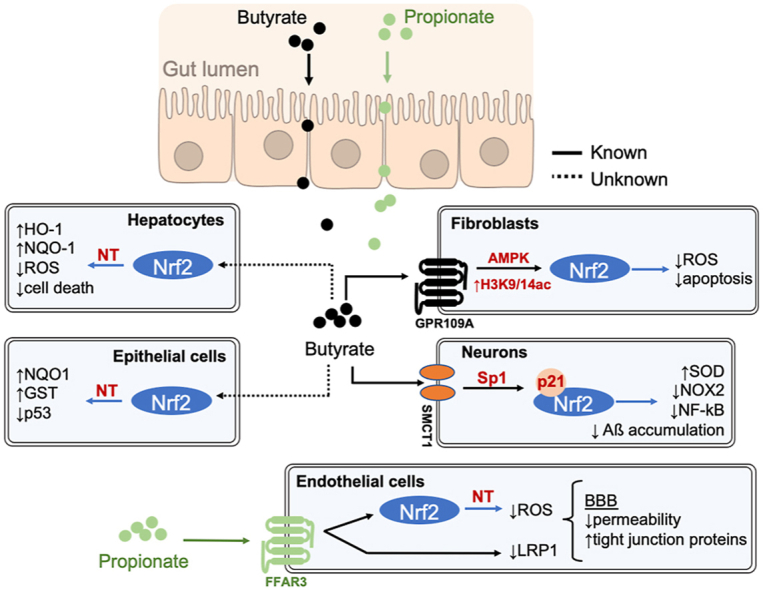
In this review, we discussed the role of SCFAs in regulating redox homeostasis mainly via targeting Keap1-Nrf2 signaling, as illustrated in Fig. 4. These compounds, especially butyrate, exhibit anti-inflammatory and anti-proliferative properties related to their redox signaling activity. SCFAs can inhibit HDAC activities, contributing to the epigenetic regulation of genes, including Nrf2. Among the natural compounds that can modulate the Keap1-Nrf2 pathway, SCFAs offer an advantage as their activity depends on specific receptors and transporters [5], potentially avoiding widespread activation of Nrf2 with undesirable effects on the redox status of healthy versus cancerous tissues [135].
Fig. 4.
Schematic highlighting redox regulation by SCFAs in different cell types. Aβ: amyloid β peptide; AMPK: AMP-activated protein kinase; BBB: blood-brain barrier; FFAR2: free fatty acid receptor 2; FFAR3: free fatty acid receptor 3; GR109A: G-protein-coupled receptor; GST: glutathione S-transferase; HDAC: histone deacetylase 1; HO1: heme oxygenase 1; H3K9/14 ac: histone H3 acetylated in lysine 9/14; iNOS: inducible nitric oxide synthase; LRP-1: LDL Receptor Related Protein 1; NF-kB: Nuclear factor kappa B; NO: nitric oxide; NOX2: NADPH oxidase 2; NQ1: NAD(P)H: quinone oxidoreductase-1; Nrf2: nuclear erythroid 2-related factor 2; NT: nuclear translocation; p21: p53: tumor suppressor p53; ROS: reactive oxygen species; SMCT1: sodium-coupled monocarboxylate transporter 1; SOD: superoxide dismutase; Sp1: specificity protein 1.
Accelerated biological aging is a feature of age-related morbidities, which share common features, including low-grade persistent inflammation, diminished Nrf2 activity, a depleted metabolic capability and a low diversity gut microbiome [136]. In support of the beneficial effect of the microbiome metabolites in aging, recent multi-omics approaches in mice revealed a pattern of shared pathways of improved health and lifespan that included SCFAs and essential polyunsaturated fatty acid (PUFA) metabolism [137]. Notably, SCFA concentrations are likely less than optimal in older adults, possibly due to insufficient daily dietary fibre intake and to a lower capacity to produce butyrate in the elderly gut microbiome [138]. High fibre supplementation increases butyrate levels that attenuate pro-inflammatory cytokine expression in microglia in aged mice [139]. Long-term treatment with butyrate reduced muscle atrophy in mice during aging, leading to reduced fat mass, improved glucose metabolism, and increased enzymes involved in oxidative metabolism, mainly catalase, in old mice [140]. Interestingly, the beneficial effects exerted by butyrate on muscle mass during aging are consistent with inhibition of HDAC3, supporting that inhibitors of specific HDACs could be used to treat age-related metabolic disease and sarcopenia [141]. In fact, an optimal status of relevant nutrients to effectively reduce inflammation and oxidative stress, strengthens the immune system, is important for human health, and particularly relevant at this time when the world is facing the coronavirus-disease 2019 (COVID-19) crisis [142].
The majority of studies in vitro have screened ‘modulators’ of redox homeostasis in cells cultured under hyperoxic conditions in incubators gassed with 5% CO2 and room air (21%, 20.9 kPa O2). Under these conditions, cells are exposed to elevated O2 levels never encountered in vivo, and as consequence Nrf2-regulated antioxidant defences are upregulated to reduce oxidative stress [[143], [144], [145]]. To our knowledge, there are no reported studies of the effects of SCFAs under physiologically relevant O2 levels and thus such studies are necessary to recapitulate SCFAs mediated redox signaling in vivo. Based on emerging data, the use of specific SCFAs as nutritional and therapeutic agents in inflammation, cancer and aging warrants further investigation. The design of improved experimental approaches to explore the mechanisms of production and action of SCFAs in cellular redox signaling under physiological conditions will underpin strategies for developing personalized nutrition and therapeutics for redox medicine.
Declaration of competing interest
Authors declare no conflicts of interest.
Acknowledgements
The authors acknowledge the support of Heart Research UK (Ref. RG2672, G.E.M.), British Heart Foundation (FS/15/6/31298, G.E.M.), Evgen Pharma (G.E.M.), Medical Research Council (E.B., P.Z., G.E.M.), Spanish Ministry of Science, Innovation and Universities (PRX19/00247, C.G.B.)
Contributor Information
Carmen González-Bosch, Email: carmen.gonzalez@uv.es, carmen.gonzalez@uv.es.
Emily Boorman, Email: emily.boorman@kcl.ac.uk.
Patricia A. Zunszain, Email: patricia.zunszain@kcl.ac.uk.
Giovanni E. Mann, Email: giovanni.mann@kcl.ac.uk.
References
- 1.Bach Knudsen K.E. Impact of diet-modulated butyrate production on intestinal barrier function and inflammation. Nutrients. 2018;10 doi: 10.3390/nu10101499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miyamoto J. Nutritional signaling via free fatty acid receptors. Int. J. Mol. Sci. 2016;17:450. doi: 10.3390/ijms17040450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perez S., Talens-Visconti R., Rius-Perez S., Finamor I., Sastre J. Redox signaling in the gastrointestinal tract. Free Radic. Biol. Med. 2017;104:75–103. doi: 10.1016/j.freeradbiomed.2016.12.048. [DOI] [PubMed] [Google Scholar]
- 4.Delmastro-Greenwood M., Freeman B.A., Wendell S.G. Redox-dependent anti-inflammatory signaling actions of unsaturated fatty acids. Annu. Rev. Physiol. 2014;76:79–105. doi: 10.1146/annurev-physiol-021113-170341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kimura I., Ichimura A., Ohue-Kitano R., Igarashi M. Free fatty acid receptors in health and disease. Physiol. Rev. 2020;100:171–210. doi: 10.1152/physrev.00041.2018. [DOI] [PubMed] [Google Scholar]
- 6.Offermanns S. Free fatty acid (FFA) and hydroxy carboxylic acid (HCA) receptors. Annu. Rev. Pharmacol. Toxicol. 2014;54:407–434. doi: 10.1146/annurev-pharmtox-011613-135945. [DOI] [PubMed] [Google Scholar]
- 7.Canani R.B. Potential beneficial effects of butyrate in intestinal and extraintestinal diseases. World J. Gastroenterol. 2011;17:1519–1528. doi: 10.3748/wjg.v17.i12.1519. 10.3748/wjg.v17.i12.1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barrea L. From gut microbiota dysfunction to obesity: could short-chain fatty acids stop this dangerous course? Hormones (Basel) 2019;18:245–250. doi: 10.1007/s42000-019-00100-0. [DOI] [PubMed] [Google Scholar]
- 9.Schonfeld P., Wojtczak L. Short- and medium-chain fatty acids in energy metabolism: the cellular perspective. J. Lipid Res. 2016;57:943–954. doi: 10.1194/jlr.R067629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pouteau E., Nguyen P., Ballevre O., Krempf M. Production rates and metabolism of short-chain fatty acids in the colon and whole body using stable isotopes. Proc. Nutr. Soc. 2003;62:87–93. doi: 10.1079/PNS2003208. [DOI] [PubMed] [Google Scholar]
- 11.Cummings J.H., Pomare E.W., Branch W.J., Naylor C.P., Macfarlane G.T. Short chain fatty acids in human large intestine, portal, hepatic and venous blood. Gut. 1987;28:1221–1227. doi: 10.1136/gut.28.10.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morrison D.J., Preston T. Formation of short chain fatty acids by the gut microbiota and their impact on human metabolism. Gut Microb. 2016;7:189–200. doi: 10.1080/19490976.2015.1134082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hamer H.M. Review article: the role of butyrate on colonic function. Aliment. Pharmacol. Ther. 2008;27:104–119. doi: 10.1111/j.1365-2036.2007.03562.x. [DOI] [PubMed] [Google Scholar]
- 14.Meesters R.J. Application of liquid chromatography-mass spectrometry to measure the concentrations and study the synthesis of short chain fatty acids following stable isotope infusions. J Chromatogr B Analyt Technol Biomed Life Sci. 2007;854:57–62. doi: 10.1016/j.jchromb.2007.03.044. [DOI] [PubMed] [Google Scholar]
- 15.Moreau N.M. Simultaneous measurement of plasma concentrations and 13C-enrichment of short-chain fatty acids, lactic acid and ketone bodies by gas chromatography coupled to mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci. 2003;784:395–403. doi: 10.1016/s1570-0232(02)00827-9. [DOI] [PubMed] [Google Scholar]
- 16.Nagashima H. High-resolution nuclear magnetic resonance spectroscopic study of metabolites in the cerebrospinal fluid of patients with cervical myelopathy and lumbar radiculopathy. Eur. Spine J. 2010;19:1363–1368. doi: 10.1007/s00586-010-1453-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morris G. The role of the microbial metabolites including tryptophan catabolites and short chain fatty acids in the pathophysiology of immune-inflammatory and neuroimmune disease. Mol. Neurobiol. 2017;54:4432–4451. doi: 10.1007/s12035-016-0004-2. [DOI] [PubMed] [Google Scholar]
- 18.Aguilar E.C. Oral butyrate reduces oxidative stress in atherosclerotic lesion sites by a mechanism involving NADPH oxidase down-regulation in endothelial cells. J. Nutr. Biochem. 2016;34:99–105. doi: 10.1016/j.jnutbio.2016.05.002. [DOI] [PubMed] [Google Scholar]
- 19.Babayan V.K. Medium chain triglycerides and structured lipids. Lipids. 1987;22:417–420. doi: 10.1007/BF02537271. [DOI] [PubMed] [Google Scholar]
- 20.Hunt M.C., Siponen M.I., Alexson S.E. The emerging role of acyl-CoA thioesterases and acyltransferases in regulating peroxisomal lipid metabolism. Biochim. Biophys. Acta. 2012;1822:1397–1410. doi: 10.1016/j.bbadis.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 21.Cahill G.F., Jr. Fuel metabolism in starvation. Annu. Rev. Nutr. 2006;26:1–22. doi: 10.1146/annurev.nutr.26.061505.111258. [DOI] [PubMed] [Google Scholar]
- 22.Koutnik A.P., D'Agostino D.P., Egan B. Anticatabolic effects of ketone bodies in skeletal muscle. Trends Endocrinol. Metabol. 2019;30:227–229. doi: 10.1016/j.tem.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 23.Shimazu T. Suppression of oxidative stress by β-hydroxybutyrate, an endogenous histone deacetylase inhibitor. Science. 2013;339:211–214. doi: 10.1126/science.1227166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haase S., Haghikia A., Wilck N., Muller D.N., Linker R.A. Impacts of microbiome metabolites on immune regulation and autoimmunity. Immunology. 2018;154:230–238. doi: 10.1111/imm.12933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marinissen M.J., Gutkind J.S. G-protein-coupled receptors and signaling networks: emerging paradigms. Trends Pharmacol. Sci. 2001;22:368–376. doi: 10.1016/s0165-6147(00)01678-3. [DOI] [PubMed] [Google Scholar]
- 26.Macia L. Metabolite-sensing receptors GPR43 and GPR109A facilitate dietary fibre-induced gut homeostasis through regulation of the inflammasome. Nat. Commun. 2015;6:6734. doi: 10.1038/ncomms7734. [DOI] [PubMed] [Google Scholar]
- 27.Sies H. Findings in redox biology: from H2O2 to oxidative stress. J. Biol. Chem. 2020;295:13458–13473. doi: 10.1074/jbc.X120.015651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sies H., Jones D.P. Reactive oxygen species (ROS) as pleiotropic physiological signalling agents. Nat. Rev. Mol. Cell Biol. 2020;21:363–383. doi: 10.1038/s41580-020-0230-3. [DOI] [PubMed] [Google Scholar]
- 29.Cortese-Krott M.M. The reactive species interactome: evolutionary emergence, biological significance, and opportunities for redox metabolomics and personalized medicine. Antioxidants Redox Signal. 2017;27:684–712. doi: 10.1089/ars.2017.7083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Droge W. Free radicals in the physiological control of cell function. Physiol. Rev. 2002;82:47–95. doi: 10.1152/physrev.00018.2001. [DOI] [PubMed] [Google Scholar]
- 31.Dan Dunn J., Alvarez L.A., Zhang X., Soldati T. Reactive oxygen species and mitochondria: a nexus of cellular homeostasis. Redox Biol. 2015;6:472–485. doi: 10.1016/j.redox.2015.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sena L.A., Chandel N.S. Physiological roles of mitochondrial reactive oxygen species. Mol. Cell. 2012;48:158–167. doi: 10.1016/j.molcel.2012.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sies H. Oxidative stress: a concept in redox biology and medicine. Redox Biol. 2015;4:180–183. doi: 10.1016/j.redox.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yamamoto M., Kensler T.W., Motohashi H. The KEAP1-NRF2 system: a thiol-based sensor-effector apparatus for maintaining redox homeostasis. Physiol. Rev. 2018;98:1169–1203. doi: 10.1152/physrev.00023.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Houghton C.A., Fassett R.G., Coombes J.S. Sulforaphane and other nutrigenomic Nrf2 activators: can the clinician's expectation Be matched by the reality? Oxidative medicine and cellular longevity. 2016:7857186. doi: 10.1155/2016/7857186. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Afrin S. Dietary phytochemicals in colorectal cancer prevention and treatment: a focus on the molecular mechanisms involved. Biotechnol. Adv. 2020;38:107322. doi: 10.1016/j.biotechadv.2018.11.011. [DOI] [PubMed] [Google Scholar]
- 37.Chikara S. Oxidative stress and dietary phytochemicals: role in cancer chemoprevention and treatment. Cancer Lett. 2018;413:122–134. doi: 10.1016/j.canlet.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 38.Mann G.E., Forman H.J. Introduction to special issue on 'Nrf2 regulated redox signaling and metabolism in physiology and medicine. Free Radic. Biol. Med. 2015;88:91–92. doi: 10.1016/j.freeradbiomed.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 39.Cuadrado A. Therapeutic targeting of the NRF2 and KEAP1 partnership in chronic diseases. Nat. Rev. Drug Discov. 2019;18:295–317. doi: 10.1038/s41573-018-0008-x. [DOI] [PubMed] [Google Scholar]
- 40.Ishii T. Transcription factor Nrf2 coordinately regulates a group of oxidative stress-inducible genes in macrophages. J. Biol. Chem. 2000;275:16023–16029. doi: 10.1074/jbc.275.21.16023. [DOI] [PubMed] [Google Scholar]
- 41.Suzuki T., Yamamoto M. Molecular basis of the Keap1-Nrf2 system. Free Radic. Biol. Med. 2015;88:93–100. doi: 10.1016/j.freeradbiomed.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 42.Tebay L.E. Mechanisms of activation of the transcription factor Nrf2 by redox stressors, nutrient cues, and energy status and the pathways through which it attenuates degenerative disease. Free Radic. Biol. Med. 2015;88:108–146. doi: 10.1016/j.freeradbiomed.2015.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Itoh K. Keap1 regulates both cytoplasmic-nuclear shuttling and degradation of Nrf2 in response to electrophiles. Gene Cell. 2003;8:379–391. doi: 10.1046/j.1365-2443.2003.00640.x. [DOI] [PubMed] [Google Scholar]
- 44.Itoh K. Keap1 represses nuclear activation of antioxidant responsive elements by Nrf2 through binding to the amino-terminal Neh2 domain. Genes Dev. 1999;13:76–86. doi: 10.1101/gad.13.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gugliandolo A., Bramanti P., Mazzon E. Activation of Nrf2 by natural bioactive compounds: a promising approach for stroke? Int. J. Mol. Sci. 2020;21 doi: 10.3390/ijms21144875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang D.D., Chapman E. The role of natural products in revealing NRF2 function. Nat. Prod. Rep. 2020;37:797–826. doi: 10.1039/c9np00061e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vanduchova A., Anzenbacher P., Anzenbacherova E. Isothiocyanate from broccoli, sulforaphane, and its properties. J. Med. Food. 2019;22:121–126. doi: 10.1089/jmf.2018.0024. [DOI] [PubMed] [Google Scholar]
- 48.Dinkova-Kostova A.T., Kostov R.V. Glucosinolates and isothiocyanates in health and disease. Trends Mol. Med. 2012;18:337–347. doi: 10.1016/j.molmed.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 49.Hoyles L. Microbiome-host systems interactions: protective effects of propionate upon the blood-brain barrier. Microbiome. 2018;6:55. doi: 10.1186/s40168-018-0439-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Guo W. Butyrate alleviates oxidative stress by regulating NRF2 nuclear accumulation and H3K9/14 acetylation via GPR109A in bovine mammary epithelial cells and mammary glands. Free Radic. Biol. Med. 2020 doi: 10.1016/j.freeradbiomed.2020.01.016. [DOI] [PubMed] [Google Scholar]
- 51.Chambel S.S., Santos-Goncalves A., Duarte T.L. The dual role of Nrf2 in nonalcoholic fatty liver disease: regulation of antioxidant defenses and hepatic lipid metabolism. BioMed Res. Int. 2015:597134. doi: 10.1155/2015/597134. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.DeBlasi J.M., DeNicola G.M. Dissecting the crosstalk between NRF2 signaling and metabolic processes in cancer. Cancers. 2020;12 doi: 10.3390/cancers12103023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hayes J.D., Dinkova-Kostova A.T. The Nrf2 regulatory network provides an interface between redox and intermediary metabolism. Trends Biochem. Sci. 2014;39:199–218. doi: 10.1016/j.tibs.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 54.Ludtmann M.H., Angelova P.R., Zhang Y., Abramov A.Y., Dinkova-Kostova A.T. Nrf2 affects the efficiency of mitochondrial fatty acid oxidation. Biochem. J. 2014;457:415–424. doi: 10.1042/BJ20130863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Slocum S.L. Keap1/Nrf2 pathway activation leads to a repressed hepatic gluconeogenic and lipogenic program in mice on a high-fat diet. Arch. Biochem. Biophys. 2016;591:57–65. doi: 10.1016/j.abb.2015.11.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jabs M. Inhibition of endothelial Notch signaling impairs fatty acid transport and leads to metabolic and vascular remodeling of the adult Heart. Circulation. 2018;137:2592–2608. doi: 10.1161/CIRCULATIONAHA.117.029733. [DOI] [PubMed] [Google Scholar]
- 57.Wakabayashi N., Chartoumpekis D.V., Kensler T.W. Crosstalk between Nrf2 and Notch signaling. Free Radic. Biol. Med. 2015;88:158–167. doi: 10.1016/j.freeradbiomed.2015.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Daschner P.J., Grisham M.B., Espey M.G. Redox relationships in gut-microbiome interactions. Free Radic. Biol. Med. 2017;105:1–2. doi: 10.1016/j.freeradbiomed.2017.02.043. [DOI] [PubMed] [Google Scholar]
- 59.Alfieri A. Sulforaphane preconditioning of the Nrf2/HO-1 defense pathway protects the cerebral vasculature against blood-brain barrier disruption and neurological deficits in stroke. Free Radic. Biol. Med. 2013;65:1012–1022. doi: 10.1016/j.freeradbiomed.2013.08.190. [DOI] [PubMed] [Google Scholar]
- 60.Srivastava S., Alfieri A., Siow R.C., Mann G.E., Fraser P.A. Temporal and spatial distribution of Nrf2 in rat brain following stroke: quantification of nuclear to cytoplasmic Nrf2 content using a novel immunohistochemical technique. J. Physiol. 2013;591:3525–3538. doi: 10.1113/jphysiol.2013.257964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cheng X. Gestational diabetes mellitus impairs Nrf2-mediated adaptive antioxidant defenses and redox signaling in fetal endothelial cells in utero. Diabetes. 2013;62:4088–4097. doi: 10.2337/db13-0169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nezu M., Suzuki N., Yamamoto M. Targeting the KEAP1-NRF2 system to prevent kidney disease progression. Am. J. Nephrol. 2017;45:473–483. doi: 10.1159/000475890. [DOI] [PubMed] [Google Scholar]
- 63.Cuadrado A. Transcription factor NRF2 as a therapeutic target for chronic diseases: a systems medicine approach. Pharmacol. Rev. 2018;70:348–383. doi: 10.1124/pr.117.014753. [DOI] [PubMed] [Google Scholar]
- 64.Wu J. Sodium butyrate attenuates diabetes-induced aortic endothelial dysfunction via P300-mediated transcriptional activation of Nrf2. Free Radic. Biol. Med. 2018;124:454–465. doi: 10.1016/j.freeradbiomed.2018.06.034. [DOI] [PubMed] [Google Scholar]
- 65.Yaku K. The enhancement of phase 2 enzyme activities by sodium butyrate in normal intestinal epithelial cells is associated with Nrf2 and p53. Mol. Cell. Biochem. 2012;370:7–14. doi: 10.1007/s11010-012-1392-x. [DOI] [PubMed] [Google Scholar]
- 66.Song Y. Non-esterified fatty acids activate the ROS-p38-p53/Nrf2 signaling pathway to induce bovine hepatocyte apoptosis in vitro. Apoptosis. 2014;19:984–997. doi: 10.1007/s10495-014-0982-3. [DOI] [PubMed] [Google Scholar]
- 67.Faraonio R. p53 suppresses the Nrf2-dependent transcription of antioxidant response genes. J. Biol. Chem. 2006;281:39776–39784. doi: 10.1074/jbc.M605707200. [DOI] [PubMed] [Google Scholar]
- 68.Wang Y., Li C., Li J., Wang G., Li L. Non-esterified fatty acid-induced reactive oxygen species mediated granulosa cells apoptosis is regulated by nrf2/p53 signaling pathway. Antioxidants. 2020;9 doi: 10.3390/antiox9060523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Stilling R.M. The neuropharmacology of butyrate: the bread and butter of the microbiota-gut-brain axis? Neurochem. Int. 2016;99:110–132. doi: 10.1016/j.neuint.2016.06.011. [DOI] [PubMed] [Google Scholar]
- 70.Logsdon A.F., Erickson M.A., Rhea E.M., Salameh T.S., Banks W.A. Gut reactions: how the blood-brain barrier connects the microbiome and the brain. Exp. Biol. Med. 2018;243:159–165. doi: 10.1177/1535370217743766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Braniste V. The gut microbiota influences blood-brain barrier permeability in mice. Sci. Transl. Med. 2014;6:263ra158. doi: 10.1126/scitranslmed.3009759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yamagata K. Docosahexaenoic acid regulates vascular endothelial cell function and prevents cardiovascular disease. Lipids Health Dis. 2017;16:118. doi: 10.1186/s12944-017-0514-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yin Y. Effects of DHA on hippocampal autophagy and lysosome function after traumatic brain injury. Mol. Neurobiol. 2018;55:2454–2470. doi: 10.1007/s12035-017-0504-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nguyen L.N. Mfsd2a is a transporter for the essential omega-3 fatty acid docosahexaenoic acid. Nature. 2014;509:503–506. doi: 10.1038/nature13241. [DOI] [PubMed] [Google Scholar]
- 75.Bazinet R.P., Laye S. Polyunsaturated fatty acids and their metabolites in brain function and disease. Nat. Rev. Neurosci. 2014;15:771–785. doi: 10.1038/nrn3820. [DOI] [PubMed] [Google Scholar]
- 76.Chen S., Subbaiah P.V. Phospholipid and fatty acid specificity of endothelial lipase: potential role of the enzyme in the delivery of docosahexaenoic acid (DHA) to tissues. Biochim. Biophys. Acta Mol. Cell Biol. Lipids. 2007;1771:1319–1328. doi: 10.1016/j.bbalip.2007.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lacombe R.J.S., Chouinard-Watkins R., Bazinet R.P. Brain docosahexaenoic acid uptake and metabolism. Mol. Aspect. Med. 2018;64:109–134. doi: 10.1016/j.mam.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 78.Bang H.Y., Park S.A., Saeidi S., Na H.K., Surh Y.J. Docosahexaenoic acid induces expression of heme oxygenase-1 and NAD(P)H:quinone oxidoreductase through activation of Nrf2 in human mammary epithelial cells. Molecules. 2017;22 doi: 10.3390/molecules22060969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kang G.J., Kim E.J., Lee C.H. Therapeutic effects of specialized pro-resolving lipids mediators on cardiac fibrosis via NRF2 activation. Antioxidants. 2020;9 doi: 10.3390/antiox9121259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhang M. Omega-3 fatty acids protect the brain against ischemic injury by activating Nrf2 and upregulating heme oxygenase 1. J. Neurosci. 2014;34:1903–1915. doi: 10.1523/JNEUROSCI.4043-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yamagata K. Dietary docosahexaenoic acid inhibits neurodegeneration and prevents stroke. J. Neurosci. Res. 2021;99:561–572. doi: 10.1002/jnr.24728. [DOI] [PubMed] [Google Scholar]
- 82.Belayev L. Docosanoids promote neurogenesis and angiogenesis, blood-brain barrier integrity, penumbra protection, and neurobehavioral recovery after experimental ischemic stroke. Mol. Neurobiol. 2018;55:7090–7106. doi: 10.1007/s12035-018-1136-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tulowiecka N., Kotlega D., Prowans P., Szczuko M. The role of resolvins: EPA and DHA derivatives can Be useful in the prevention and treatment of ischemic stroke. Int. J. Mol. Sci. 2020;21 doi: 10.3390/ijms21207628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Russell K.L., Berman N.E., Levant B. Low brain DHA content worsens sensorimotor outcomes after TBI and decreases TBI-induced Timp1 expression in juvenile rats. Prostaglandins Leukot. Essent. Fatty Acids. 2013;89:97–105. doi: 10.1016/j.plefa.2013.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mayurasakorn K. DHA but not EPA emulsions preserve neurological and mitochondrial function after brain hypoxia-ischemia in neonatal mice. PLoS One. 2016;11 doi: 10.1371/journal.pone.0160870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chen R. Transplantation of fecal microbiota rich in short chain fatty acids and butyric acid treat cerebral ischemic stroke by regulating gut microbiota. Pharmacol. Res. 2019;148:104403. doi: 10.1016/j.phrs.2019.104403. [DOI] [PubMed] [Google Scholar]
- 87.Lee J. Gut microbiota-derived short-chain fatty acids promote poststroke recovery in aged mice. Circ. Res. 2020;127:453–465. doi: 10.1161/CIRCRESAHA.119.316448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sadler R. Short-chain fatty acids improve poststroke recovery via immunological mechanisms. J. Neurosci. 2020;40:1162–1173. doi: 10.1523/JNEUROSCI.1359-19.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tan C. Dysbiosis of gut microbiota and short-chain fatty acids in acute ischemic stroke and the subsequent risk for poor functional outcomes. JPEN - J. Parenter. Enter. Nutr. 2020 doi: 10.1002/jpen.1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.van der Beek C.M., Dejong C.H.C., Troost F.J., Masclee A.A.M., Lenaerts K. Role of short-chain fatty acids in colonic inflammation, carcinogenesis, and mucosal protection and healing. Nutr. Rev. 2017;75:286–305. doi: 10.1093/nutrit/nuw067. [DOI] [PubMed] [Google Scholar]
- 91.Wang X. Sodium butyrate alleviates adipocyte inflammation by inhibiting NLRP3 pathway. Sci. Rep. 2015;5:12676. doi: 10.1038/srep12676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yuan X., Wang L., Bhat O.M., Lohner H., Li P.-L. Differential effects of short chain fatty acids on endothelial Nlrp3 inflammasome activation and neointima formation: antioxidant action of butyrate. Redox Biology. 2018;16:21–31. doi: 10.1016/j.redox.2018.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hennig B. Selective disruption of endothelial barrier function in culture by pure fatty acids and fatty acids derived from animal and plant fats. J. Nutr. 1993;123:1208–1216. doi: 10.1093/jn/123.7.1208. [DOI] [PubMed] [Google Scholar]
- 94.Hecker M. Impact of short- and medium-chain fatty acids on mitochondrial function in severe inflammation. JPEN - J. Parenter. Enter. Nutr. 2014;38:587–594. doi: 10.1177/0148607113489833. [DOI] [PubMed] [Google Scholar]
- 95.Miyoshi M., Usami M., Ohata A. Short-chain fatty acids and trichostatin A alter tight junction permeability in human umbilical vein endothelial cells. Nutrition. 2008;24:1189–1198. doi: 10.1016/j.nut.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 96.Ohata A., Usami M., Miyoshi M. Short-chain fatty acids alter tight junction permeability in intestinal monolayer cells via lipoxygenase activation. Nutrition. 2005;21:838–847. doi: 10.1016/j.nut.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 97.Luu M., Visekruna A. Short-chain fatty acids: bacterial messengers modulating the immunometabolism of T cells. Eur. J. Immunol. 2019;49:842–848. doi: 10.1002/eji.201848009. [DOI] [PubMed] [Google Scholar]
- 98.Chisolm D.A., Weinmann A.S. Connections between metabolism and epigenetics in programming cellular differentiation. Annu. Rev. Immunol. 2018;36:221–246. doi: 10.1146/annurev-immunol-042617-053127. [DOI] [PubMed] [Google Scholar]
- 99.Stempelj M., Kedinger M., Augenlicht L., Klampfer L. Essential role of the JAK/STAT1 signaling pathway in the expression of inducible nitric-oxide synthase in intestinal epithelial cells and its regulation by butyrate. J. Biol. Chem. 2007;282:9797–9804. doi: 10.1074/jbc.M609426200. [DOI] [PubMed] [Google Scholar]
- 100.Chang P.V., Hao L., Offermanns S., Medzhitov R. The microbial metabolite butyrate regulates intestinal macrophage function via histone deacetylase inhibition. Proc. Natl. Acad. Sci. U. S. A. 2014;111:2247–2252. doi: 10.1073/pnas.1322269111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Schulthess J. The short chain fatty acid butyrate imprints an antimicrobial program in macrophages. Immunity. 2019;50:432–445. doi: 10.1016/j.immuni.2018.12.018. e437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Silva L.G., Ferguson B.S., Avila A.S., Faciola A.P. Sodium propionate and sodium butyrate effects on histone deacetylase (HDAC) activity, histone acetylation, and inflammatory gene expression in bovine mammary epithelial cells. J. Anim. Sci. 2018;96:5244–5252. doi: 10.1093/jas/sky373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ni Z., Goracci L., Cruciani G., Fedorova M. Computational solutions in redox lipidomics - current strategies and future perspectives. Free Radic. Biol. Med. 2019;144:110–123. doi: 10.1016/j.freeradbiomed.2019.04.027. [DOI] [PubMed] [Google Scholar]
- 104.Pamplona R. Redox lipidomics to better understand brain aging and function. Free Radic. Biol. Med. 2019;144:310–321. doi: 10.1016/j.freeradbiomed.2019.03.016. [DOI] [PubMed] [Google Scholar]
- 105.Wang R.S., Oldham W.M., Maron B.A., Loscalzo J. Systems biology approaches to redox metabolism in stress and disease states. Antioxidants Redox Signal. 2018;29:953–972. doi: 10.1089/ars.2017.7256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Battson M.L., Lee D.M., Weir T.L., Gentile C.L. The gut microbiota as a novel regulator of cardiovascular function and disease. J. Nutr. Biochem. 2018;56:1–15. doi: 10.1016/j.jnutbio.2017.12.010. [DOI] [PubMed] [Google Scholar]
- 107.Moreno-Indias I., Cardona F., Tinahones F.J., Queipo-Ortuno M.I. Impact of the gut microbiota on the development of obesity and type 2 diabetes mellitus. Front. Microbiol. 2014;5:190. doi: 10.3389/fmicb.2014.00190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Long-Smith C. Microbiota-gut-brain Axis: new therapeutic opportunities. Annu. Rev. Pharmacol. Toxicol. 2020;60:477–502. doi: 10.1146/annurev-pharmtox-010919-023628. [DOI] [PubMed] [Google Scholar]
- 109.Weiss G.A., Hennet T. Mechanisms and consequences of intestinal dysbiosis. Cell. Mol. Life Sci. 2017;74:2959–2977. doi: 10.1007/s00018-017-2509-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Robles-Vera I. Protective effects of short-chain fatty acids on endothelial dysfunction induced by angiotensin II. Front. Physiol. 2020;11:277. doi: 10.3389/fphys.2020.00277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Mollica M.P. Butyrate regulates liver mitochondrial function, efficiency, and dynamics in insulin-resistant obese mice. Diabetes. 2017;66:1405–1418. doi: 10.2337/db16-0924. [DOI] [PubMed] [Google Scholar]
- 112.Noureldein M.H., Bitar S., Youssef N., Azar S., Eid A.A. Butyrate modulates diabetes-linked gut dysbiosis: epigenetic and mechanistic modifications. J. Mol. Endocrinol. 2020;64:29–42. doi: 10.1530/JME-19-0132. [DOI] [PubMed] [Google Scholar]
- 113.Hu S., Kuwabara R., de Haan B.J., Smink A.M., de Vos P. Acetate and butyrate improve beta-cell metabolism and mitochondrial respiration under oxidative stress. Int. J. Mol. Sci. 2020;21 doi: 10.3390/ijms21041542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Krautkramer K.A. Diet-microbiota interactions mediate global epigenetic programming in multiple host tissues. Mol. Cell. 2016;64:982–992. doi: 10.1016/j.molcel.2016.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sharma M., Li Y., Stoll M.L., Tollefsbol T.O. The epigenetic connection between the gut microbiome in obesity and diabetes. Front. Genet. 2019;10:1329. doi: 10.3389/fgene.2019.01329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lin H.V. Butyrate and propionate protect against diet-induced obesity and regulate gut hormones via free fatty acid receptor 3-independent mechanisms. PLoS One. 2012;7 doi: 10.1371/journal.pone.0035240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Islam M.T. Oxidative stress and mitochondrial dysfunction-linked neurodegenerative disorders. Neurol. Res. 2017;39:73–82. doi: 10.1080/01616412.2016.1251711. [DOI] [PubMed] [Google Scholar]
- 118.Rossetti A.C., Paladini M.S., Riva M.A., Molteni R. Oxidation-reduction mechanisms in psychiatric disorders: a novel target for pharmacological intervention. Pharmacol. Therapeut. 2020;210:107520. doi: 10.1016/j.pharmthera.2020.107520. [DOI] [PubMed] [Google Scholar]
- 119.Liu J.J. Effects of chain length of saturated fatty acids on Aβ generation in SH-SY5Y cells. Neurosci. Lett. 2019;698:169–172. doi: 10.1016/j.neulet.2019.01.024. [DOI] [PubMed] [Google Scholar]
- 120.Szczechowiak K., Diniz B.S., Leszek J. Diet and Alzheimer's dementia - nutritional approach to modulate inflammation. Pharmacol. Biochem. Behav. 2019;184:172743. doi: 10.1016/j.pbb.2019.172743. [DOI] [PubMed] [Google Scholar]
- 121.Kim S.Y. Sodium butyrate inhibits high cholesterol-induced neuronal amyloidogenesis by modulating NRF2 stabilization-mediated ROS levels: involvement of NOX2 and SOD1. Cell Death Dis. 2020;11:469. doi: 10.1038/s41419-020-2663-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Geng X. Effects of docosahexaenoic acid and its peroxidation product on amyloid-β peptide-stimulated microglia. Mol. Neurobiol. 2020;57:1085–1098. doi: 10.1007/s12035-019-01805-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Rios-Covian D. Intestinal short chain fatty acids and their link with diet and human health. Front. Microbiol. 2016;7:185. doi: 10.3389/fmicb.2016.00185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Cryan J.F. The microbiota-gut-brain Axis. Physiol. Rev. 2019;99:1877–2013. doi: 10.1152/physrev.00018.2018. [DOI] [PubMed] [Google Scholar]
- 125.Wolters M. Dietary fat, the gut microbiota, and metabolic health - a systematic review conducted within the MyNewGut project. Clin. Nutr. 2019;38:2504–2520. doi: 10.1016/j.clnu.2018.12.024. [DOI] [PubMed] [Google Scholar]
- 126.Gonzalez-Bosch C. Priming plant resistance by activation of redox-sensitive genes. Free Radic. Biol. Med. 2018;122:171–180. doi: 10.1016/j.freeradbiomed.2017.12.028. [DOI] [PubMed] [Google Scholar]
- 127.Aranega-Bou P., de la O.L.M., Finiti I., Garcia-Agustin P., Gonzalez-Bosch C. Priming of plant resistance by natural compounds. Hexanoic acid as a model. Front. Plant Sci. 2014;5:488. doi: 10.3389/fpls.2014.00488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ahmed S. In vitro characterization of gut microbiota-derived bacterial strains with neuroprotective properties. Front. Cell. Neurosci. 2019;13:402. doi: 10.3389/fncel.2019.00402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Narayanan A., Baskaran S.A., Amalaradjou M.A., Venkitanarayanan K. Anticarcinogenic properties of medium chain fatty acids on human colorectal, skin and breast cancer cells in vitro. Int. J. Mol. Sci. 2015;16:5014–5027. doi: 10.3390/ijms16035014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Finiti I. Hexanoic acid protects tomato plants against Botrytis cinerea by priming defence responses and reducing oxidative stress. Mol. Plant Pathol. 2014;15:550–562. doi: 10.1111/mpp.12112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Mann G.E. Nrf2-mediated redox signalling in vascular health and disease. Free Radic. Biol. Med. 2014;75(Suppl 1):S1. doi: 10.1016/j.freeradbiomed.2014.10.595. [DOI] [PubMed] [Google Scholar]
- 132.Patel B., Mann G.E., Chapple S.J. Concerted redox modulation by sulforaphane alleviates diabetes and cardiometabolic syndrome. Free Radic. Biol. Med. 2018;122:150–160. doi: 10.1016/j.freeradbiomed.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 133.Andersson M.X. Involvement of the electrophilic isothiocyanate sulforaphane in Arabidopsis local defense responses. Plant Physiol. 2015;167:251–261. doi: 10.1104/pp.114.251892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Schillheim B. Sulforaphane modifies histone H3, unpacks chromatin, and primes defense. Plant Physiol. 2018;176:2395–2405. doi: 10.1104/pp.17.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Dodson M. Modulating NRF2 in disease: timing is everything. Annu. Rev. Pharmacol. Toxicol. 2019;59:555–575. doi: 10.1146/annurev-pharmtox-010818-021856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Badal V.D. The gut microbiome, aging, and longevity: a systematic review. Nutrients. 2020;12 doi: 10.3390/nu12123759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Aon M.A. Untangling determinants of enhanced health and lifespan through a multi-omics approach in mice. Cell Metabol. 2020;32:100–116. doi: 10.1016/j.cmet.2020.04.018. e104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hippe B. Quantification of butyryl CoA:acetate CoA-transferase genes reveals different butyrate production capacity in individuals according to diet and age. FEMS Microbiol. Lett. 2011;316:130–135. doi: 10.1111/j.1574-6968.2010.02197.x. [DOI] [PubMed] [Google Scholar]
- 139.Matt S.M. Butyrate and dietary soluble fiber improve neuroinflammation associated with aging in mice. Front. Immunol. 2018;9:1832. doi: 10.3389/fimmu.2018.01832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Walsh M.E. The histone deacetylase inhibitor butyrate improves metabolism and reduces muscle atrophy during aging. Aging Cell. 2015;14:957–970. doi: 10.1111/acel.12387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Walsh M.E., Van Remmen H. Emerging roles for histone deacetylases in age-related muscle atrophy. Nutr. Healthy Aging. 2016;4:17–30. doi: 10.3233/nha-160005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Loffredo L., Violi F. COVID-19 and cardiovascular injury: a role for oxidative stress and antioxidant treatment? Int. J. Cardiol. 2020;312:136. doi: 10.1016/j.ijcard.2020.04.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Chapple S.J. Bach1 differentially regulates distinct Nrf2-dependent genes in human venous and coronary artery endothelial cells adapted to physiological oxygen levels. Free Radic. Biol. Med. 2016;92:152–162. doi: 10.1016/j.freeradbiomed.2015.12.013. [DOI] [PubMed] [Google Scholar]
- 144.Keeley T.P., Mann G.E. Defining physiological normoxia for improved translation of cell physiology to animal models and humans. Physiol. Rev. 2019;99:161–234. doi: 10.1152/physrev.00041.2017. [DOI] [PubMed] [Google Scholar]
- 145.Warpsinski G. Nrf2-regulated redox signaling in brain endothelial cells adapted to physiological oxygen levels: consequences for sulforaphane mediated protection against hypoxia-reoxygenation. Redox Biol. 2020;37:101708. doi: 10.1016/j.redox.2020.101708. [DOI] [PMC free article] [PubMed] [Google Scholar]