To the Editor: While being one of the common causes of low back pain (LBP), the pathogenesis, as well as definitive diagnostic criteria and expert treatment recommendations for endplate inflammation remain largely unclear. Clinically, vertebroplasty and local injection of corticosteroids are often used for relieving the pain instead of targeting the cause.
Secukinumab is a humanized monoclonal antibody used against interleukin (IL)-17A, which is mainly prescribed to treat patients with psoriatic arthritis or ankylosing spondylitis. We report a patient with severe endplate inflammation complicated by hepatitis B virus (HBV) infection who achieved complete remission using secukinumab.
A 36-year-old woman who carried HBV suffered from continuous LBP at rest and in daily activities for 5 years. She had no obvious morning stiffness, rashes, pain in her joints and heels, or a family history of similar diseases. In the past year, the LBP had become worse, and she was unable to bend over due to worse LBP, which affected basic activities such as getting up and turning over. Her visual analog scale (VAS; range: 0–10) score was seven, and her Oswestry Disability Index (ODI; range: 0–50 points) score was 38 points.
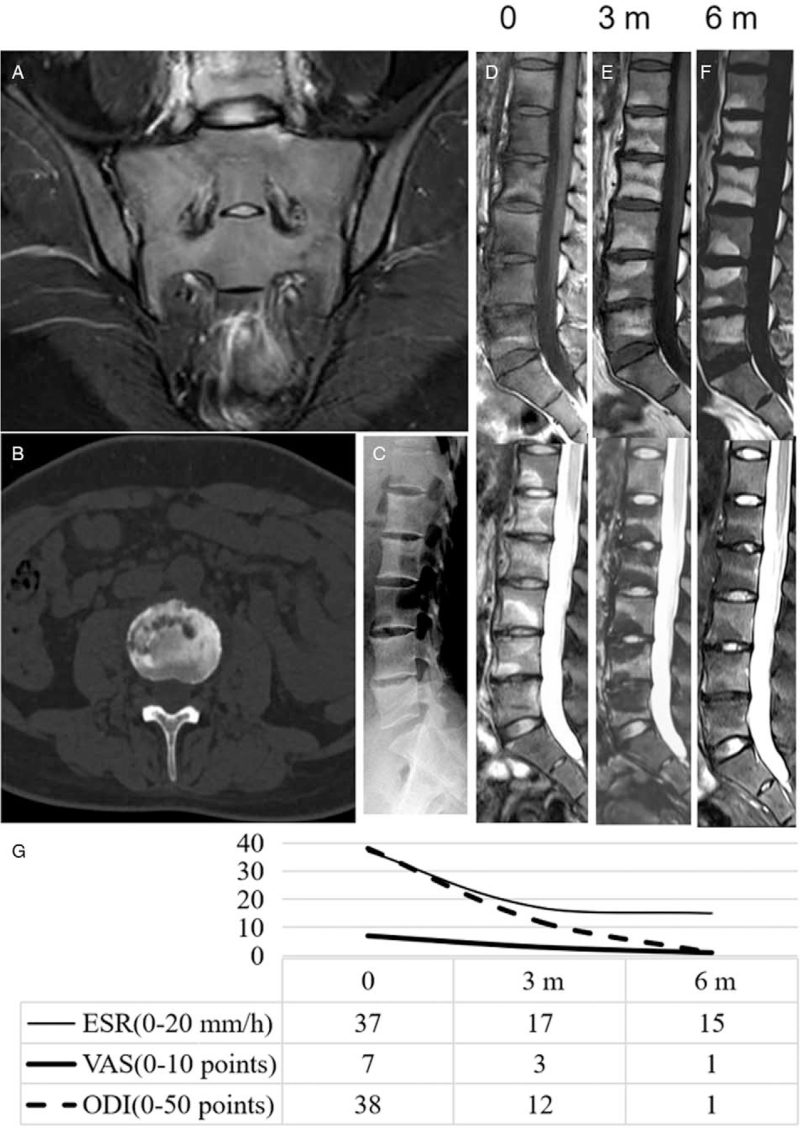
Physical examination revealed straightening of the lumbar spine curvature, as well as movement restriction. The distance between her fingers and the ground was >40 cm after bending downward. Routine blood, hepatic and renal function tests were normal. Her erythrocyte sedimentation rate (ESR) was 37 mm/1h, and her C-reactive protein level was 3.62 mg/L. She tested positive for hepatitis B surface antibody, as well as antigen, hepatitis B core antibody, and hepatitis B e antibody. The quantitative HBV-DNA level was 48.4 IU/mL. Tuberculosis T cell spot detection (T-SPOT.TB) and HLA-B27 tests were negative. Magnetic resonance imaging (MRI) of the sacroiliac joint showed no obvious abnormity [Figure 1A]. Lumbar imaging results revealed poor vertebral sequence and L3–4 vertebral displacement, hyperostosis, significant bone destruction, and bone marrow edema in the lumbar spine [Figure 1B–F].
Figure 1.
X-ray, CT, MRI scan, ESR (0–20 mm/h), VAS (range: 0–10) score, and ODI (0–50 points) score. (A) MRI of the sacroiliac joint was normal. (B) Lumbar spine CT shows vertebral edge destruction. (C) Lumbar spine X-ray shows straightening of the lumbar spine curvature, poor alignment, bone hyperplasia in the vertebral body, and L4–5 vertebral space stenosis. (D–F) Lumbar spine MRI shows T12–L5 VESB signal changes, with T1 hypointensity (upper) and T2 hyperintensity (lower). (E) Lumbar spine MRI after 3 months of treatment; (F) Lumbar spine MRI after 6 months of treatment; (E, F) Additional MR examination shows L1–5 VESB changes, with T1 hyperintensity (left) and T2 hypointensity (right). (G) The chart shows the changes in ESR, VAS, and ODI scores before and after treatment. CT: Computed tomography; ESR: Erythrocyte sedimentation rate; MRI: Magnetic resonance imaging; ODI: Oswestry Disability Index; VESB: Vertebral endplate subchondral bone; VAS: Visual analog scale.
She was eventually diagnosed with endplate inflammation and prescribed secukinumab 150 mg by subcutaneous injection once a week for 5 weeks. The dosing frequency was subsequently changed to once a month. At the 3- and 6-month follow-up, the LBP symptoms of the patient were relieved, whereas her ESR, VAS, and ODI scores had dropped sharply [Figure 1G]. An additional lumbar MRI showed the disappearance of bone marrow edema from the affected vertebral bodies [Figure 1E and 1F]. HBV-DNA level after 6 months of treatment was 113 IU/mL, which was slightly higher than that at presentation. The doctor of the infectious diseases department suggested that antiviral treatment was not needed for the time being, and HBV-DNA monitoring was continued.
Both endplate inflammation and spondyloarthritis (SpA) can cause the symptom of LBP. The onset of most patients with endplate inflammation is related to injury, chondral degeneration, infection, and so on., whereas SpA is a group of genetically related diseases with specific clinical manifestations. Clinically, vertebral MR changes in SpA and signal changes in other causes of vertebral endplate inflammation are not easily distinguished. The patient in our report had LBP but no morning stiffness; HLA-B27 was negative, and MRI of the sacroiliac joint was normal. Despite the vertebral lesion, there was insufficient evidence for the diagnosis of axial spinal arthropathy (axSpA) for the time being. Of course, the possibility of her condition developing into typical axSpA in the future cannot be excluded. The poor alignment of the lumbar spine and instability of the vertebral bodies in this patient may be related to the endplate inflammation.
According to present studies, the activation of T helper 17 (Th17) lymphocytes and dendritic cells and the release of cytokines, such as IL-17 and tumor necrosis factor (TNF)-α, play important roles in the pathogenesis of both diseases.[1,2] The increased levels of inflammatory cytokines, such as IL-6, IL-1, IL-17, and TNF-α, in the intervertebral discs of patients with endplate inflammation suggest the significance of the inflammatory response in disease pathogenesis.[2] Among these key cytokines, IL-17 can mediate the migration and activation of immune cells and aggravate the inflammatory response.[3] IL-17 is also known to activate mesenchymal stem cells in the vertebral bodies, promoting new subperiosteal bone formation and the production of bone spurs.[3] IL-17 also promotes the expression of RANKL by osteocytes, which enhances the differentiation of osteoclasts, which are involved in bone destruction.[4]
IL-17A is a primary member of the IL-17 family. Secukinumab, a human monoclonal antibody, selectively binds IL-17A and inhibits inflammation, bone destruction, and formation of new bone. However, it remains unclear whether endplate inflammation can be treated by inhibiting the IL-17/Th17 axis. A recent study[2] reported higher IL-17 levels in the peripheral blood and intervertebral discs and significant upregulation of Th17 lymphocytes of patients with endplate inflammation compared with those in healthy controls. These studies provided a theoretical basis for treating endplate inflammation using secukinumab. In this case, the patient's clinical symptoms, laboratory tests, and imaging results improved significantly after 6 months of treatment with secukinumab, and she had achieved nearly complete remission. These results are consistent with previous predictions that IL-17A may play a vital role in endplate inflammation.
In addition, IL-17A can activate Kupffer cells and stellate cells in the liver and participate in the development of hepatitis B.[5] Therefore, although the patient's HBV-DNA copy number did not increase significantly during secukinumab treatment, regular long-term testing is still required. The efficacy of secukinumab in the treatment of endplate inflammation and its side effects need to be studied in a larger sample.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the article. The patient understands that her name and initials will not be published and due efforts will be made to conceal the identity of the patient, although anonymity cannot be guaranteed.
Acknowledgements
Author thanks all the doctors for providing care to this patient. We thank the patient for her cooperation and consent to the publication of this article.
Conflicts of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
How to cite this article: Hou RH, Wen XT, Wang Q, Wang L. Using secukinumab in a patient with endplate inflammation complicated by hepatitis B virus infection. Chin Med J 2021;134:2644–2646. doi: 10.1097/CM9.0000000000001801
References
- 1.Rosine N, Miceli-Richard C. Innate cells: the alternative source of IL-17 in axial and peripheral spondyloarthritis? Front Immunol 2020; 11:553742.doi: 10.3389/fimmu.2020.553742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang J, Sun W, Bond A, Xu C, Li K, Ren D, et al. A positive feedback loop between Th17 cells and dendritic cells in patients with endplate inflammation. Immunol Investig 2019; 48:39–51. doi: 10.1080/08820139.2018.1496097. [DOI] [PubMed] [Google Scholar]
- 3.Schett G, Lories RJ, D’Agostino MA, Elewaut D, Kirkham B, Soriano ER, et al. Enthesitis: from pathophysiology to treatment. Nat Rev Rheumatol 2017; 13:731–741. doi: 10.1038/nrrheum.2017.188. [DOI] [PubMed] [Google Scholar]
- 4.Zhang XM, Liu CY, Shao ZH. Advances in the role of helper T cells in autoimmune diseases. Chin Med J 2020; 133:968–974. doi: 10.1097/CM9.0000000000000748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen YF, Chen J, Li LJ. The role of intestinal microbiota, bile acids, and Th17/IL17 axis in hepatitis B virus-related liver fibrosis. Chin Med J 2020; 133:2902–2904. doi: 10.1097/CM9.0000000000001199. [DOI] [PMC free article] [PubMed] [Google Scholar]