Solute carrier family 51 alpha subunit (SLC51A) encodes the alpha subunit of the heteromeric organic solute transporter alpha–beta (OSTα–OSTβ), an important contributor to intestinal bile acid (BA) reabsorption in the enterohepatic circulation.(1,2) Here, we identified the first case of OSTα deficiency in a child with unexplained elevated liver transaminases, cholestasis, and congenital diarrhea.
Case Report
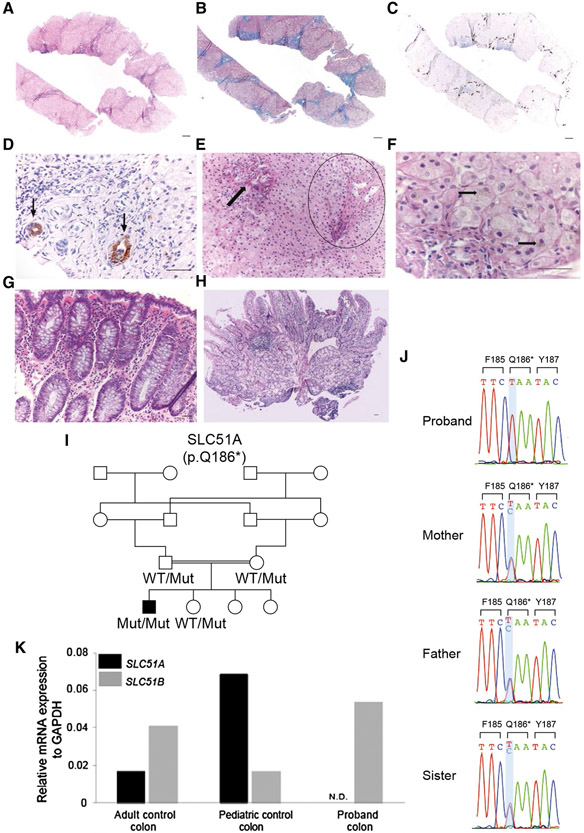
A 2.5-year-old Pakistani boy, born from a first-cousin union, was evaluated in a liver clinic. His past medical history is significant for chronic malabsorptive diarrhea of 10-15 oily daily stools, easy bruising, two episodes of prolonged bleeding that required blood transfusions, and failure to thrive. Stool studies included normal pH, and negative occult blood, reducing substance, and ova cysts. The patient was exclusively breastfed until 1 year of age, when he was started on soy-based formula milk, nutritional rehabilitation, and fat-soluble vitamin supplementation, with improvement in his weight and height. At age 2.5, he was found to have elevated transaminases and alkaline phosphatase (Table 1). Liver biopsy revealed a lobular architecture suggestive of early cirrhosis with portal and periportal fibrosis and many thin fibrous septa (Fig. 1A,B). Portal areas showed minimal lymphocytic inflammation, no interface activity, and patchy mild bile ductular proliferation (Fig. 1C,D). Bile ducts were missing in three of the portal tracts (Fig. 1E), not meeting criteria for bile duct paucity. The hepatocytes showed rare foci of subtle hepatocytic cholestasis (Fig. 1F). Duodenal and colonic biopsies showed no significant abnormality (Fig. 1G,H). Since a comprehensive workup was unrevealing (Supporting Table S1), his exome was sequenced. Consistent with consanguinity, the proband harbors 23 rare homozygous protein-altering variants, including 22 missense variants predicted to be tolerated by a meta-analytic support vector machine (MetaSVM) and therefore unlikely to be pathogenic in this child. Notably, the other homozygous mutation led to a premature termination at codon 186 in SLC51A (NM_152672,c.556C>T,p.Gln186*), which encodes OSTα. This variant allele is extremely rare, with only one instance among more than 251,400 alleles sequenced from diverse populations, including South Asians (gnomAD: https://gnomad.broadinstitute.org, last accessed September 25, 2019). Sanger sequencing confirmed the homozygous variant in the proband and showed the heterozygous carrier state of both his parents and an unaffected sister (Fig. 1I,J). Furthermore, the proband’s colon tissue showed undetectable SLC51A transcripts (Fig. 1K). Analysis of the BA concentrations in the proband’s blood spot by liquid chromatography–tandem mass spectrometry (LC-MS/MS) showed that BA concentrations were within the normal range despite underlying cholestasis. He was started on ursodiol at 5 years and 1 month and 9 months later on cholestyramine. While the coagulopathy resolved, his growth is adequate and he has two or three bulky daily bowel movements; his transaminases, direct bilirubin, and gamma-glutamyl-transferase (GGT) levels remain elevated (Table 1).
TABLE 1.
Clinical and Laboratory Findings in Proband Who Harbors a Homozygous Premature Termination Mutation (P.Gln186*) in SLC51A
| Proband’s Age in Years |
|||||
|---|---|---|---|---|---|
| Laboratory Test | Reference | 2.5 | 3.8 | 4 | 5 |
| AST (U/L) | 15-40 | 126 (H) | 112(H) | 98 (H) | 66 (H) |
| ALT (U/L) | 4-25 | 227(H) | 126 (H) | 117 (H) | 90 (H) |
| Bilirubin total/direct (mg/dL) | 0.1-1.2/<0.3 | 0.7/n.a. | 1.6 (H)/n.a. | 1.8/1.2 (H) | 2.3/1.9 (H) |
| GGT (U/L) | 5–32 | n.a. | n.a. | n.a. | 104 (H) |
| ALP (U/L) | 100–320 | 708 (H) | 1320 (H) | 661 (H) | 268 |
| INR | 0.9-1.1 | 3.1 (H) | 1.6 (H) | 1.6 (H) | 1.1 |
| Vitamin D, 25-OH (ng/mL) | 16-65 | 8.7 | n.a. | n.a. | 28* |
| Albumin (mg/dL) | 3.5-5.5 | n.a. | n.a. | 3.7 | n.a. |
| BAs measured in DBS samples† | |||||
| Cholic acid | 0.003-0.19 | n.a. | n.a. | n.a. | 0.02 |
| Dihydroxycholanoates‡ (μM) | 0.09-2.21 | n.a. | n.a. | n.a. | 0.11 |
| Glychocholic acid (μM) | 0.005-2.52 | n.a. | n.a. | n.a. | 0.11 |
| Glycodihydroxycholanoates§ (μM) | 0.22-4.16 | n.a. | n.a. | n.a. | 0.33 |
| Taurocholic acid (μM) | 0.001-0.612 | n.a. | n.a. | n.a. | 0.06 |
| Taurodihydroxycholanoates∥ (μM) | 0.03-0.43 | n.a. | n.a. | n.a. | 0.07 |
On vitamin D supplement.
Prior to initiation of ursodeoxycholic acid supplement.
Chenodeoxycholic acid + deoxycholic acid.
Glycochenodeoxycholic acid + glycodeoxycholic acid.
Taurochenodeoxycholic acid + taurodeoxycholic acid.
Abbreviations: ALP, alkaline phosphatase; DBS, dried blood spots; H, high; INR, international normalized ratio; n.a., not available.
FIG. 1.
Histological and molecular findings in a child with OSTα deficiency. (A) Liver parenchyma (hematoxylin and eosin) shows distorted lobular architecture and expanded portal areas with mild ductular proliferation. (B) Trichrome stain reveals portal and periportal fibrosis along with many thin fibrous septa, with nodularity of the lobular architecture suggestive of early cirrhosis. (C) Cytokeratin 7 immunOSTain highlights the portal tracts and shows mild bile ductular proliferation in most of the portal areas. (D) Higher magnification of cytokeratin 19 immunOSTain of one of the portal tracts showing presence of two bile duct profiles (arrows). (E) Two portal areas are depicted: one with few bile ductular profiles (arrow) and one devoid of any bile ducts (circle). The portal areas show only minimal lymphocytic inflammation and no interface activity. The hepatocytes are otherwise unremarkable. (F) Periportal area showing rare foci of subtle hepatocytic cholestasis (arrows). (G) Duodenal and (H) colonic mucosa show no significant histologic abnormality. (I) Proband and his unaffected family members are shown in black and white symbols, respectively. Consanguineous union is depicted by a double line. SLC51A alleles are denoted as wild type or mutant (p.Gln186*). (J) Sanger sequencing chromatograms of the proband and his unaffected parents and sibling are shown. The SLC51A p.Gln186* mutation is homozygous in the proband and heterozygous in the unaffected parents and sister. (K) Relative expression of SLC51A and SLC51B to GAPDH in proband’s colon tissue compared to normal-appearing colon tissue from two unrelated individuals shows absent SLC51A and preserved SLC51B mRNA expression in proband’s colon tissue. Scale bars, 100 μm in (A-C) and 50 μm in the remaining panels. Abbreviations: GAPDH, glyceraldehyde-3-phosphate dehydrogenase; Mut, mutant; N.D., not detected; WT, wild type.
Discussion
Our findings provide the first demonstration of human OSTα deficiency in a child with elevated liver transaminases, cholestasis, liver fibrosis, and congenital diarrhea. The evidence implicating SLC51A genotype as the cause of the proband’s phenotype is strong. First, the proband represents the first homozygote for an extremely rare premature termination mutation in SLC51A. Second, there is an absence of SLC51A mRNA expression in the proband’s colon tissue, consistent with his recessive premature termination mutation in SLC51A leading to mRNA decay. Third, the proband’s clinical phenotype is consistent with a defect in BA metabolism. Fourth, human deficiency for OSTβ, which forms a heterodimer with OSTα in the active transporter, has been described in two siblings who also presented with congenital diarrhea and features of cholestasis at pediatric age.(3) Altogether, these 3 patients with either OSTα or OSTβ deficiency have elevated transaminases (alanine aminotransferase [ALT] > aspartate aminotransferase [AST]) and GGT and low-normal circulating BAs. It is noteworthy that the liver biopsy from our proband revealed a more advanced liver disease than the liver injury reported in the two OSTβ-deficient siblings.(3) The full clinical spectrum attributable to the loss of SLC51A will need to be determined by the identification and study of additional patients with OSTα deficiency.
Collectively, this case underscores how an unbiased genomic approach is highly valuable in clinical hepatology practice,(4) while uncovering gene contributions in human health and disease.
Supplementary Material
Acknowledgment:
We thank the proband and his family for their invaluable contribution to this work and the staff of the Yale Center for Genome Analysis for exome sequencing.
Supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (K08 DK113109, to S.V.) the US National Institutes of Health (NIH) Centers for Mendelian Genomics (U54 HG006504), the Doris Duke Charitable Foundation (2019081), and the NIH–Yale Liver Center (P30DK034989). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Supporting Information
Additional Supporting Information may be found at onlinelibrary.wiley.com/doi/10.1002/hep.31087/suppinfo.
Potential conflict of interest: Nothing to report.
REFERENCES
- 1).Ballatori N, Christian WV, Lee JY, Dawson PA, Soroka CJ, Boyer JL, et al. OSTalpha-OSTbeta: a major basolateral bile acid and steroid transporter in human intestinal, renal, and biliary epithelia. Hepatology 2005;42:1270–1279. [DOI] [PubMed] [Google Scholar]
- 2).Dawson PA, Hubbert M, Haywood J, Craddock AL, Zerangue N, Christian WV, et al. The heteromeric organic solute transporter alpha-beta, OSTalpha-Ostbeta, is an ileal basolateral bile acid transporter. J Biol Chem 2005;280:6960–6968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Sultan M, Rao A, Elpeleg O, Vaz FM, Abu-Libdeh B, Karpen SJ, et al. Organic solute transporter-beta (SLC51B) deficiency in two brothers with congenital diarrhea and features of cholestasis. Hepatology 2018;68:590–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Vilarinho S, Mistry PK. Exome sequencing in clinical hepatology. Hepatology 2019;70:2185–2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.