Abstract
Research and clinical use of circulating cell-free DNA (cirDNA) is expanding rapidly; however, there remain large gaps in our understanding of the influence of lifestyle and biological factors on the amount of cirDNA present in blood. Here, we review 66 individual studies of cirDNA levels and lifestyle and biological factors, including exercise (acute and chronic), alcohol consumption, occupational hazard exposure, smoking, body mass index, menstruation, hypertension, circadian rhythm, stress, biological sex and age. Despite technical and methodological inconsistences across studies, we identify acute exercise as a significant influence on cirDNA levels. Given the large increase in cirDNA induced by acute exercise, we recommend that controlling for physical activity prior to blood collection is routinely incorporated into study design when total cirDNA levels are of interest. We also highlight appropriate selection and complete reporting of laboratory protocols as important for improving the reproducibility cirDNA studies and ability to critically evaluate the results.
Introduction
Circulating cell-free DNA (cirDNA) in blood has been extensively researched due to its potential as a biomarker across multiple settings including oncology, prenatal testing, toxicology, organ transplantation, and cardiovascular and autoimmune diseases. In cancer alone, cirDNA-related publications have increased exponentially (Trigg et al., 2018) with nearly 2000 publications solely in 2020. Considering the enormous investment and effort that has gone into the development of cirDNA biomarkers, understanding the biological and lifestyle factors that impact cirDNA levels is important for appropriate study design.
The release of cirDNA from cells into the blood is thought to be driven by apoptosis, which is closely linked to inflammation and cell damage. In this review, we aim to gather and summarise all published studies that have investigated an association between biological and lifestyle factors and cirDNA. By ‘biological factor‘, we refer to intrinsic physiological variables such as body mass index (BMI), menstruation, hypertension, circadian rhythm, stress, biological sex and age. By ‘lifestyle factor’, we refer to all external variables that involve individual choice, such as exercise, alcohol consumption, occupation and smoking. We have chosen to include only studies conducted on plasma and exclude all studies on serum as serum has been shown to be the less preferred substrate due to its propensity for leukocyte DNA contamination and dependence on processing time (Ammerlaan and Betsou, 2019; Trigg et al., 2018; Warton et al., 2014). The use of serum was the only exclusion criterion that we imposed. We included all identified plasma studies regardless of the sample size, cohort type (healthy or diseased) and laboratory methodology. The cohorts included, but were not limited to, people with cancer, hormone therapy-treated women and haemodialysis patients. In those studies, there are confounding factors related to pathology, and the cirDNA level is partly, if not primarily, influenced by disease-driven cirDNA changes.
In total, this review summarises the results from 66 individual studies published between January 2000 and January 2021 (Supplementary file 1). It is important to note that we did not aim to provide a statistical evaluation of the impacts of each factor on cirDNA level, but rather to create a summary of research endeavours in the field and to raise awareness of the need for large, adequately powered studies with appropriate technical protocols.
1 Biological factors
1.1 Body mass index
BMI, calculated by dividing weight (kg) by the square of height (m2), categorises an individual as underweight (<18.5), normal weight (18.5–24.9), overweight (25–29.9) or obese (>30). BMI, however, does not distinguish whether the weight is fat or muscle mass, hence its usage is not accurate for groups of people such as body builders and athletes.
Eight individual studies on cirDNA and BMI were identified, containing six healthy cohorts (n = 1464) and six cohorts that included individuals with various diseases and women undergoing hormone replacement therapy (HRT). Five of the studies conducted on healthy individuals, totalling to 1098 subjects, reported no relationship between cirDNA and BMI. They contained relatively large, combined numbers of healthy male and female subjects (763 males and 701 females), but most did not sex-disaggregate their data for analysis. A single study reported significantly higher cirDNA level with increasing BMI in a group of 366 healthy women (Jylhävä et al., 2014). Although this is the only study that discovered an association in healthy individuals, it has the strongest statistical power, albeit no information on how the cirDNA was processed (time to processing, number of spins and extraction method).
A positive correlation between BMI and cirDNA was found in 62 hepatitis-related liver fibrosis patients (46 males and 16 females) (Yan et al., 2018). However, in 30 gastric cancer patients (Kim et al., 2014), 218 women receiving oestrogen and/or progestin hormone treatment (Jylhävä et al., 2014), 58 non-alcoholic fatty liver disease patients (Karlas et al., 2017) and 113 type II diabetes (T2D) patients (Bryk et al., 2019) all did not show any relationship between BMI and cirDNA level. It may be that the effect of BMI on cirDNA is moderate and requires a large sample size (such as in the Jylhävä et al., 2014 study) for the effect to be observed. The positive correlation reported in the fibrosis patients may be due to BMI being associated with the disease itself (Cristina et al., 2018). If BMI is indeed linked to cirDNA, one proposed mechanism is that obesity disrupts the balance of the adipose tissue microenvironment, resulting in adipocytes undergoing apoptosis and/or necrosis and releasing cirDNA into the circulation (Nishimoto et al., 2016; Yan et al., 2018).
As discussed in Section 4, accurate cirDNA quantification is strongly dependent on extraction and measurement methods. Limiting discussion to studies that either measured cirDNA directly from plasma or used a dedicated extraction kit, two studies from the same group reported no relationship between BMI and cirDNA concentration in a total of 402 nonagenarians (Jylhävä et al., 2012; Jylhävä et al., 2013), while a single study with 62 liver fibrosis patients reported a positive relationship (Yan et al., 2018). Given the methodological limitations and the lack of consistent results, a definitive answer regarding the effect of BMI on cirDNA levels is still pending.
It is accepted that BMI is not an accurate reflection of obesity (Nuttall, 2015). The question then arises, if cirDNA is not correlated with BMI, is it correlated with fat mass itself? This was further supported by data from a cohort of 131 people (88 men and 44 women) investigated during medical examination. Higher visceral (abdominal) fat area (VFA ≥100 cm2), as determined by computed tomography, positively correlated with plasma single-stranded DNA concentration (Nishimoto et al., 2016). The authors further showed that cirDNA released from obese mice can bind to TLR9 receptors expressed by macrophages, leading to cell accumulation and assisting in causing chronic low inflammation associated with obesity (Nishimoto et al., 2016). In humans, although acute inflammation is associated with cirDNA increase, the correlation with chronic inflammation is inconclusive (Frank, 2016).
BMI is well known to be a risk factor for T2D (Al-Goblan et al., 2014; Bhowmik et al., 2015), a state where reduced insulin production or insulin resistance causes high blood glucose and ultimately leads to many physiological complications. Higher cirDNA has been found to be positively correlated with higher fasting glucose in 113 T2D patients (Bryk et al., 2019), but not in healthy female and male controls or females receiving oestrogen and/or progestin (Jylhävä et al., 2014). Furthermore, cirDNA is positively correlated with insulin levels in healthy women and women receiving oestrogen. but not in healthy men and women receiving oestrogen and progestin (Jylhävä et al., 2014).
1.2 Menstruation
The menstrual cycle is the regular succession of menstruation and ovulation in women. During the follicular phase, the endometrium thickens from approximately 5.4 mm to 9.2 mm (Tsuda et al., 2018). If fertilisation is absent, menstruation follows and is characterised by breakdown of the outer endometrial epithelium layer via apoptosis (Armstrong et al., 2017; Kokawa et al., 1996; Tabibzadeh, 1996) and extensive angiogenesis (Demir et al., 2010).
A single study examined the impact of menstruation on plasma cirDNA levels (Yuwono et al., 2021). Matched plasma samples from 40 women at the menstruating and non-menstruating phases of the cycle were compared, for total and endothelium-derived cirDNA, and no differences were observed. The strengths of this study were the adequate sample size (powered at 90% to detect 30% change), optimum cirDNA processing and good assay sensitivity.
These findings were unexpected given the extensive cell death and proliferation that occurs during the menstrual cycle. In addition to apoptosis occurring within the endometrium, leukocyte numbers increase during menstruation and contribute to the matrix metalloproteinases that break down the endometrial tissue (Maybin and Critchley, 2015); however, the eventual leukocyte cell death was not reflected by an increase in cirDNA amount. Shedding of apoptotic cell debris into the uterine cavity may account for lack of cirDNA increase during menstruation (Greystoke et al., 2013). This contrasts with scenarios like cancer or any diseases involving internal tissue damage, in which cell death occurs completely surrounded by stroma and therefore apoptotic or necrotic DNA is more likely to spill over into the circulation.
1.3 Hypertension
Hypertension, defined by World Health Organization (WHO), as having diastolic blood pressure (DBP) and systolic blood pressure (SBP) of ≥140 mm Hg and ≥90 mm Hg, respectively, can lead to stroke, kidney failure, blindness, rupture of blood vessels and cognitive impairment. The elevated pressure can cause endothelial cell DNA damage, inflammation and oxidative stress (Ranchoux et al., 2016), all of which could potentially result in cirDNA changes.
Five individual studies on cirDNA and hypertension were identified, containing four healthy cohorts (n = 1247) and five cohorts that included patients with various diseases and women undergoing HRT. Overall, conflicting findings were reported. No correlation between cirDNA levels and hypertension was found in 258 nonagenarians (Jylhävä et al., 2012), 218 women receiving oestrogen and/or progestin therapy (Jylhävä et al., 2014), 14 healthy women (Brodbeck et al., 2020) and 113 T2D patients (Bryk et al., 2019). The use of HRT has been shown to improve blood pressure (Butkevich et al., 2000; McCubbin et al., 2002) while the synergy between T2D and hypertension is well established (Lastra et al., 2014). By contrast, in 366 healthy women and 609 healthy men, cirDNA was positively correlated with SBP and/or DBP (Jylhävä et al., 2014). cirDNA was also positively correlated with SBP in 95 haemodialysis patients, 50 of whom were also diabetic (Jeong et al., 2015). Taking into account only studies that use cirDNA dedicated extraction kits or direct from plasma measurement (Brodbeck et al., 2020; Jeong et al., 2015; Jylhävä et al., 2012) retains a mixed picture of the impact of hypertension on cirDNA levels. It is likely that the effect, if any, is small, and may be mitigated by interaction with gender and HRT use.
Due to its global prevalence, the effects of hypertension on cirDNA are of interest. Future studies should include hypertensive people both with and without medication, as well as healthy controls. The studies should be disaggregated by sex and include subjects selected for the absence of other comorbidities and lifestyle variables that can potentially be confounding factors.
1.4 Circadian rhythm
The circadian rhythm, driven by the suprachiasmatic nucleus of the anterior hypothalamus of the brain, influences physiological profiles such as temperature, hormone levels and urine volume, as well as behaviour such as activity and sleep. Daytime is characterised by high body temperature, high urine volume, low melatonin and high cortisol, while the opposite occurs during night-time (Czeisler and Buxton, 2011; Silver and Schwartz, 2005). Disturbances in circadian rhythm lead to increased risk for a range of cancers including lung, colon, bladder and prostate cancers (Parent et al., 2012; Wendeu-Foyet et al., 2018).
Seven individual studies on cirDNA and circadian rhythm were identified, containing seven healthy cohorts (n = 73) and two cancer patient cohorts (colorectal and lung cancers). Overall, there is mixed evidence regarding circadian rhythm influence on cirDNA. No differences in cirDNA as a function of time were observed in a group of 11 healthy subjects measured at 7 AM, 12 PM and 5 PM (Korabecna et al., 2011) or in 4 healthy individuals measured every 2 hr and 45 min between 8:30 AM and 7:30 PM (Wagner et al., 2020). This lack of effect was also seen in 11 moderately trained men measured 11 times over 24 hr (Fatouros et al., 2010) as well as 1 healthy control and 10 colorectal cancer patients (stages I–IV) measured every 6 hr over a 24 hr interval (Tóth et al., 2017). In contrast, two studies reported a decrease in cirDNA levels between morning and evening in 13 and 4 subjects, respectively (Madsen et al., 2019; Meddeb et al., 2019).
Two studies implemented cirDNA tailored pre-analytical practice (short blood processing time, double centrifugation and appropriate cirDNA extraction kit), as well as limiting physical activity of study participants to minimise changes due to exercise. As described above, no circadian pattern was observed in four healthy subjects measured five times between 8:30 AM and 7:30 PM, with the experiment repeated on two separate days (Wagner et al., 2020). However, the study by Madsen and colleagues extended three hourly measurements from 9 AM to 9 PM in 13 healthy subjects and observed a gradual decrease that reached statistical significance at 9 PM (Madsen et al., 2019).
Two studies measured cirDNA fluctuations over short time intervals, specifically over 1 hr (Madsen et al., 2019) and every 5–15 min over 75 min (Brodbeck et al., 2020), both reporting no effect. Two studies compared cirDNA levels between days. There was no difference between days 1, 2 and 3 at 9 AM in either 33 healthy subjects or 10 lung cancer patients (Madsen et al., 2019) or in cirDNA measured 1 week apart (Wagner et al., 2020). All three aforementioned studies employed optimum cirDNA processing.
A relationship between cirDNA levels and circadian rhythm can be expected as multiple studies have shown cirDNA is primarily haematopoietic in origin (Lam et al., 2017; Lui et al., 2002; Moss et al., 2018; Snyder et al., 2016; Sun et al., 2015; Sun et al., 2019; Wong et al., 2016; Zheng et al., 2012) and haematopoietic cell numbers display a 24 hr circadian cycle (Ackermann et al., 2012; Pritchett and Reddy, 2015). On the other hand, the mechanism of cirDNA release into the bloodstream is mainly apoptosis (Jahr et al., 2001; Jiang et al., 2018; Jiang and Lo, 2016), and there is no evidence circadian rhythm influences apoptosis in healthy individuals, and only limited evidence in disease states (Gaddameedhi et al., 2015; Rabinovich-Nikitin et al., 2019; Wang et al., 2015).
The circadian rhythm studies do not report the time interval between waking and blood collection from subjects. Given the rapid clearance of cirDNA following exercise-induced increase, it is possible that cirDNA does change during sleep but returns to normal by the time a blood sample is taken for measurement. Furthermore, only two studies report what activity the participants were involved in between blood draws. In those studies, participants were told to minimise physical activity before blood draws (Madsen et al., 2019) or given access to recliner chairs and allowed to walk around freely (Wagner et al., 2020).
1.5 Psychological stress
Psychological stress burden has been linked to cirDNA changes through inflammation mechanisms (Liu et al., 2017) and DNA damage (Jenkins et al., 2014). Three individual studies on cirDNA and psychological stress were identified, containing two healthy cohorts and a cohort of women undergoing IVF treatment.
Brodbeck et al., 2020 took advantage of the stress created by venepuncture to look for a relationship between stress and cirDNA levels. The nervousness of study participants was quantified on a 0–10 scale. No relationship was observed between self-reported nervousness about the venepuncture procedure and cirDNA levels in 14 healthy women volunteers. However, the subjects might not be a true representative of a cohort experiencing a lot of stress since they volunteered for the venepuncture and were informed of the study procedure, and scaling, while easy and simple, is prone to bias.
Within a longer timeframe, Czamanski-Cohen et al., 2014 examined cirDNA in 14 women undergoing IVF treatment. Women who were offered 5–6 sessions with an experienced psychotherapist and implemented twice daily stress reduction techniques (n = 8) had significantly lower cirDNA levels at the end of the IVF cycle than women who received standard psychological care from IVF nursing staff (n = 6). The cirDNA was quantitated directly from plasma using a nucleic acid stain; however, pre-analytical procedures regarding blood tube type, blood processing time and centrifugation were not described.
Hummel et al., 2018 examined the acute effect of stress on cirDNA using the Trier social stress test – a validated and standardised acute laboratory stress challenge – in 20 healthy male sports science students. The test involved a free speech and an unanticipated math task performed in front of judges and a camera, all leading to consistently raised levels of cortisol. Immediately after the test cirDNA was found to have increased by about twofold, followed by a rapid drop back down to pre-test levels within 15 min. However, there was no correlation between cortisol and cirDNA (Hummel et al., 2018). With 20 paired samples, this study had the highest statistical power. The technical strengths were circadian rhythm control, with all blood sampling performed between 9 and 11 AM and optimum pre-analytical procedures (appropriate kit, immediate blood processing time, double centrifugation). Overall, there is some evidence for the impact of psychological stress on cirDNA.
1.6 Biological sex
Twenty-five individual studies on cirDNA and biological sex were identified. These included 12 cohorts of healthy subjects and 24 cohorts of patients with diagnosed disease (Table 1). In the healthy cohorts, 6/12 studies (n = 240) reported no difference while the remaining half (n = 1868) reported males having significantly higher cirDNA compared to females.
Table 1. Association of cirDNA with gender.
| Authors (year) | Subject | Conclusion to gender differences on cirDNA amount | ||
|---|---|---|---|---|
| Cohort | Male (n) | Female (n) | ||
| Coulet et al., 2000 | Head and neck squamous cell carcinoma patients (n = 117) | 105 | 12 | No effect |
| Sozzi et al., 2001 | Control (n = 43) | NA | NA | No effect |
| Lung cancer patients (n = 84) | 72 | 12 | No effect (p=0.403) | |
| Tamkovich et al., 2005 | Healthy volunteers (n = 35) | 15 | 20 | No effect |
| Zhong et al., 2007 | Healthy adults (n = 54) | 27 | 27 | No effect |
| Lee et al., 2011 | Lung cancer patients (n = 134) | 13 | 121 | No effect (p=0.947) |
| Beiter et al., 2011 | Recreational runners (n = 53) | 34 | 19 | No effect |
| Jylhävä et al., 2012 | Nonagenarians (n = 258) | 62 | 196 | Significantly higher in male (p=0.018) |
| Kim et al., 2014 | Control (n = 34) | 15 | 19 | No effect (p=0.598) |
| Gastric cancer patients (n = 30) | 23 | 7 | Significantly higher in female (p=0.01) | |
| Spindler et al., 2014 | Metastatic colorectal cancer patients (n = 86) | 55 | 31 | No effect (p=0.24) |
| Jylhävä et al., 2014 | Finnish population | 609–681 | 366–409 | Significantly higher in male (p=0.00) |
| Jeong et al., 2015 | Haemodialysis patients (n = 95) | NA | NA | No effect |
| Diabetic haemodialysis patients (n = 50) | NA | NA | No effect (p=0.22) | |
| Spindler et al., 2015 | Metastatic colorectal cancer patients (n = 223) | 126 | 97 | No effect (p=0.1) |
| Chen et al., 2016 | Stage I and II non-small cell lung cancer patients | 33 | 25 | No effect (p=0.318) |
| Hsieh et al., 2016 | Oesophageal squamous cell carcinoma patients | 70 | 11 | No effect (p=0.315) |
| Karlas et al., 2017 | Non-alcoholic fatty liver disease patients (n = 58) | 32 | 26 | 90 bp fragment – no effect; 222 bp fragment – higher in female (p=0.0051) |
| Li et al., 2017 | All lymphoma patients (n = 174) | 107 | 67 | No effect (p=0.769) |
| Diffuse large B cell lymphoma (n = 98) | 61 | 37 | No effect (p=0.507) | |
| Çayir et al., 2018 | Control (n = 51) | 28 | 23 | Significantly higher in male |
| Greenhouse workers (n = 72) | 41 | 31 | Significantly higher in male | |
| Meddeb et al., 2019 | Healthy individuals (n = 104) | 62 | 42 | Significantly higher in male (p=0.048) |
| Colorectal cancer patients (n = 118) | 68 | 50 | No effect | |
| van der Drift et al., 2010 | Healthy controls (n = 21) | 19 | 2 | No effect |
| Lung cancer patients (n = 46) | 30 | 16 | ||
| Catarino et al., 2012 | Healthy controls (n = 205) | 78 | 127 | Significantly higher in male (p<0.001) |
| Lung cancer patients (n = 104) | 86 | 20 | No effect (p=0.123) | |
| Wu et al., 2019 | Newly diagnosed lymphoma patients (n = 60) | 32 | 28 | No effect (p=0.76) |
| Treated lymphoma patients (n = 107) | 59 | 48 | No effect (p=0.4967) | |
| Alghofaili et al., 2019 | Healthy volunteers (n = 275) | 124 | 151 | Significantly higher in male (p=0.000103) |
| Caglar et al., 2020 | Thyroiditis (n = 33) | NA | NA | No effect (p>0.7) |
| Benign (n = 37) | NA | NA | No effect (p=0.054) | |
| Malignant (n = 30) | NA | NA | No effect | |
| All thyroid patients (n = 100) | NA | NA | No effect (p=0.08) | |
| Bryk et al., 2019 | T2D patients (n = 111) | NA | NA | No effect (p=0.51) |
| Bu et al., 2020 | Gastric cancer patients (n = 61) | 41 | 20 | No effect |
T2D: type II diabetes.
In patient cohorts and workers exposed to occupational hazards, most studies (21/24) report no differences in cirDNA between males and females. A single study of 72 greenhouse workers reported higher cirDNA level in males (Çayir et al., 2018), but the remaining two patient studies reported higher cirDNA in females (Karlas et al., 2017; Kim et al., 2014). However, of these, one analysis, conducted in 30 gastric patients, had imbalanced sample numbers with 23 males and only 7 females (Kim et al., 2014), while the other only saw the association with long cirDNA fragments (222 bp), with no effect on short fragments (90 bp) (Karlas et al., 2017).
Considering only studies in healthy volunteers that either measured cirDNA directly from plasma or used a dedicated extraction kit, higher cirDNA levels in males relative to females were measured in three cohorts (total of 584 subjects) (Alghofaili et al., 2019; Çayir et al., 2018; Jylhävä et al., 2012), while no effect was observed in a single cohort of 43 subjects (Sozzi et al., 2001). If sex plays a role, the evidence favours males having higher cirDNA than females. However, the effect of sex appears fairly small, and may be confounded by lifestyle differences between males and females. Carefully controlled studies with large sample numbers, combined with meta-analyses, will be helpful in quantifying the association.
1.7 Age
Twenty-nine individual studies on cirDNA and age were identified. These contained 45 cohorts, with 19 groups of healthy individuals and 26 of patients with diagnosed disease and women undergoing HRT (Table 2). Amongst the healthy cohorts, 14/19 reported no impact of age on cirDNA. Of those that showed a significant difference (5/19), all found that cirDNA is positively correlated with age (Jylhävä et al., 2011; Jylhävä et al., 2014; Jylhävä et al., 2013; Meddeb et al., 2019; Zhong et al., 2007); however, a significant effect was observed in women only in three out of the five studies (Jylhävä et al., 2011; Jylhävä et al., 2014; Zhong et al., 2007). Three of the five studies showing a relationship between age and cirDNA levels in healthy cohorts are from a single research group (Jylhävä et al., 2011; Jylhävä et al., 2014; Jylhävä et al., 2013). While the laboratory methodology is comparable to other published work, two of the studies were unique in investigating cohorts with a large age difference, rather than looking for a continuous effect. cirDNA was compared between two distinct cohorts (19–37 years versus nonagenarians) (Jylhävä et al., 2011; Jylhävä et al., 2013), both mostly women. Since the age difference is large, it is possible the effect is apparent even when the sample size is modest (11 controls and 12 nonagenarians) (Jylhävä et al., 2011). Another publication by the same group reported an age effect in healthy women (average age 60.48 years ± 8.98) and had a substantial sample size of 366 (Jylhävä et al., 2014).
Table 2. Association of cirDNA with age.
| Authors (year) | Subject | Age analysed | Conclusion to age effect on cirDNA amount |
|---|---|---|---|
| Sozzi et al., 2001 | Control (n = 43) | - | No effect |
| Lung cancer patients (n = 84) | 39–59 (n = 31) vs. 60–69 (n = 34) vs. ≥70 (n = 19) | ||
| Sozzi et al., 2003 | Lung cancer patients(n = 100)Mean age: 65.1 ± 8.9 | ≤60 vs. 61–71 vs. ≥72 | Significantly higher with increasing age |
| Tamkovich et al., 2005 | Healthy participants (n = 35 [15 M + 20 W]) | 18–53 | No effect |
| Zhong et al., 2007 | Healthy adults | 20–40 vs. 41–60 vs. >60 | No effect (men and women mixed)Significantly higher cirDNA for >60 years old compared to 20–40 and 41–60 groups in women only |
| Lee et al., 2011 | Lung cancer patients (n = 134) | ≤65 (n = 108) vs. >65 (n = 26) | No effect (p=0.333) |
| Beiter et al., 2011 | Recreational runners (n = 53)Mean age: 34.8 | 17–60 years | No effect |
| Jylhävä et al., 2011 | Control (n = 11, females, 22–37 years old) vs. nonagenarians (n = 12, females, born 1917) | Significantly higher in elderly (p=0.035, < 0.001, 0.015)* | |
| Jylhävä et al., 2013 | Young controls (n = 30 [9 M + 21 W], aged 19–30 years old) vs. nonagenarians (n = 144 [43 M + 101 W], aged ≥90 years old) | Significantly higher in nonagenarian group (p=0.002) | |
| Kim et al., 2014 | Control (n = 34)Mean age = 63.79 ± 6.76 years | <65 vs. ≥65 | No effect |
| Gastric cancer patientsMean age = 66.72 ± 13.16 years | Significantly higher with increasing age | ||
| Spindler et al., 2014 | Metastatic colorectal cancer patients (n = 86)Median age: 66 (37–83) | <66 (n = 43) vs. >66 (n = 43) | No effect |
| Jylhävä et al., 2014 | Women (n = 366–409, mean age 60.48 [8.98]) | Significantly higher with increasing age (p=0.002) | |
| Women (oestrogen HRT user, n = 131–148, mean age 58.57 [6.88]) | No effect (p=0.391) | ||
| Women (oestrogen + progestin HRT user, n = 87–98, mean age 57.23 [6.39]) | No effect (p=0.869) | ||
| Men (n = 609–681), mean age (58.31 [7.91]) | No effect (p=0712) | ||
| Breitbach et al., 2014a | Male athletes (n = 26 [13 handball players + 13 triathletes])Mean age 24.7 (3.1) | No effect | |
| Jeong et al., 2015 | Haemodialysis patients (n = 95) | 58 ± 1.5 | No effect |
| Haemodialysis patients (n = 95) | 58 ± 1.5 | No effect (p=0.80) | |
| Diabetic haemodialysis patients (n = 50) | 66.4 ± 1.8 | No effect (p=0.93) | |
| Spindler et al., 2015 | Metastatic colorectal cancer patients (n = 223)Median age: 63 (35-82) years old | ≤63 (n = 119) vs. >63 (n = 104) | No effect (p=0.39) |
| Korzeneva et al., 2015 | Average age for all groups: 48.5 ± 16.3 years | ||
| Never-exposed control group (n = 109) | *21–86 | No effect (p=0.13) | |
| Chronic gamma-neutron radiation-exposed group (n = 88) | *26–79 | No effect (p=0.6) | |
| Chronic tritium β-radiation-exposed group (n = 88) | *20–80 | No effect (p=0.06) | |
| Never-exposed control group (n = 109) | <65 years old vs. ≥65 years old | Significantly higher with increasing age | |
| Chronic gamma-neutron radiation-exposed group (n = 88) | <65 years old vs. ≥65 years old | Significantly lower with increasing age | |
| Chronic tritium β-radiation-exposed group (n = 88) | <65 years old vs. ≥65 years old | No effect | |
| Hsieh et al., 2016 | Oesophageal squamous cell carcinoma patients (n = 81 [70 M + 11 F]) | <60 (N = 43) vs. >60 (N = 38) | No effect (p=0.588) |
| Tosevska et al., 2016 | Institutionalised elderly aged 65–98 (n = 105) | 65–98 | No effect |
| Karlas et al., 2017 | Non-alcoholic fatty liver disease patients (n = 58) | Age (mean age 62.1 ± 11 years old) | No effect |
| Li et al., 2017 | All lymphoma patients (n = 174) | ≤60 (N = 117) vs. ≥60 (N = 57) | No effect (p=0.414) |
| Diffuse large B cell lymphoma (n = 98) | ≤60 (N = 61) vs. ≥60 (N = 37) | No effect (p=0.668) | |
| Beranek et al., 2017 | Exacerbated psoriasis vulgaris patients (n = 28 [15 M + 13 W]) | 18–69 (median age 50) | No effect |
| Teo et al., 2019 | Young (n = 3) vs. elderly (n = 3) vs. healthy centenarians (n = 3) vs. unhealthy centenarians (n = 3) | No effect | |
| Meddeb et al., 2019 | Healthy individuals (n = 104)Age range: 18–69 | <47 (n = 52) vs. ≥47 (n = 52) | Significantly higher with increasing age (p=0.009) |
| Healthy individuals (n = 104) | Young (n = 79) vs. older (n = 25)† | Significantly higher with increasing age (p=0.0026) | |
| Colorectal cancer patients (n = 118)Age range: 22–91 | <65 (n = 52) vs. ≥65 (n = 66) | No effect | |
| Colorectal cancer patients (n = 118) | Young (n = 25) vs. older (n = 93)† | No effect (p=0.913) | |
| van der Drift et al., 2010 | Healthy controls | <60 vs. ≥60 | No effect (p=0.43) |
| Lung cancer | <60 vs. ≥60 | No effect (p=0.25) | |
| Catarino et al., 2012 | Healthy controls (n = 205) | <64 vs. ≥64 | No effect (p=0.342) |
| Lung cancer patients (n = 104) | <64 vs. ≥64 | No effect (p=0.614) | |
| Wu et al., 2019 | Newly diagnosed lymphoma patients (n = 60) | <60 vs. ≥60 | No effect (p=0.4041) |
| Treated lymphoma patients (n = 107) | <60 vs. ≥60 | No effect (p=0.3127) | |
| Alghofaili et al., 2019 | Healthy volunteers (n = 275) | Correlation plot (0–57 years old; median 27 years old) | No effect (r = –0.09) |
| Caglar et al., 2020 | Thyroiditis (n = 33) | 37.6 ± 10.9 | No effect |
| Benign (n = 37) | 54.1 ± 13.1 | No effect | |
| Malignant (n = 30) | 47.8 ± 11.9 | No effect | |
| All thyroid patients (n = 100) | Significant positive correlation (p<0.05) | ||
| Bryk et al., 2019 | T2D patients | No effect (p=0.63) | |
| Bu et al., 2020 | Gastric cancer patients (n = 61) | 40–83 | No effect (p=0.323 and p=0.280)‡ |
Three different extraction kits.
Using same cutoff for both healthy and cancer cohort as the median age (56) of all individuals tested.
Two different extraction kits.
HRT: hormone replacement therapy; T2D: type II diabetes.
Considering only studies with healthy cohorts and cirDNA-tailored methodology, two studies with a total of 197 subjects observed a relationship between cirDNA levels and age (Jylhävä et al., 2011; Jylhävä et al., 2013), while five studies with a total of 461 subjects reported no relationship (Alghofaili et al., 2019; Breitbach et al., 2014a; Sozzi et al., 2001; Teo et al., 2019; Tosevska et al., 2016). However, as discussed below, comparisons between individual studies are difficult due to the different age ranges of subjects included, for example, very young versus very old (Jylhävä et al., 2011; Jylhävä et al., 2013), compared to studies with a smaller age range (Breitbach et al., 2014a).
In a comprehensive study of the tissue sources of cirDNA conducted by Moss et al., 2018, the sources of cirDNA were unchanged with age; however, older people had higher cirDNA levels. The consistent tissue profile could indicate decreased capacity of cirDNA clearance rather than an increase in apoptosis of specific tissues (Moss et al., 2018). Similarly, Teo et al., 2019 found little change between young people (25 ± 0.5 years old) and healthy centenarians but found larger fluctuations among healthy older subjects (71 ± 1.6 years old) and unhealthy centenarians, including decreased pituitary gland and increased tibial artery cirDNA.
In the patient cohorts, 23/26 observed no age effect, while in three studies comprising 100 thyroid-related pathology patients (Caglar et al., 2020), 30 gastric cancer patients (Kim et al., 2014) and 100 lung cancer patients (Sozzi et al., 2003), a positive correlation with age was seen.
Comparing the effect of age across different studies is difficult for several reasons. Firstly, the way the subjects are categorised, and therefore analysed, varies between the studies. Some studies use specific age cutoffs (younger than or older than a certain age) to split their cohorts into two or three continuous groups. For example, Korzeneva et al., 2015 found no effect in either 109 healthy controls or 88 people chronically exposed to gamma-neutron radiation, unless the cohorts were split into two age groups, which resulted in significantly higher and lower cirDNA with increasing age, respectively. Some studies compared two groups with distinct ages such as Jylhävä et al., 2011, where a young age group (22–37 years old) is compared to nonagenarians. Some studies do not split their subjects but perform a correlation statistical analysis (Table 2). Overall, based on the evidence, the effect of age on cirDNA levels appears small.
2 Lifestyle factors
2.1 Exercise
Of all variables reviewed, exercise holds the most evidence to support its effect on cirDNA levels. A large and robust increase in cirDNA levels is associated with acute exercise, while less consistent changes are reported with chronic exercise (reviewed by Breitbach et al., 2012 and Vittori et al., 2019). Studies of exercise and cirDNA levels are summarised in Table 3.
Table 3. cirDNA measurements in acute exercise.
| Authors (year) | Setting | Subject | CirDNA measurement time points |
|---|---|---|---|
| Atamaniuk et al., 2004 | Race (did not specify duration and distance) | Healthy half-marathon runners (n = 25 [12 M + 13 F]) | Before the race, immediately after race, 2 hr post-race |
| Margeli et al., 2005 | 246 km ultra-marathon | Healthy males (n = 15) | Pre-race, post-race (within 15 min), post-race (48 hr) |
| Atamaniuk et al., 2008 | 6 hr race | Experienced ultra-marathon runners (n = 14 [9 M + 5 F]) | Pre-race, post-race, post-race (2 hr), post-race (24 hr) |
| Fatouros et al., 2010 | Control (rest): remain seated/lying in the labExercise: 45 min treadmill run followed by increase in speed until exhaustion | Moderately trained men (n = 11) | Pre-exercise, post-exercise, post-exercise (0.5 hr, 1, 2, 3, 4, 5, 6, 8, 10, 24 hr) |
| Atamaniuk et al., 2010 | Six sets of six weightlifting exercise | Male competitive weightlifters (n = 12) | Pre-exercise, post-exercise (immediately after), post-exercise (2 hr) |
| Beiter et al., 2011 | Public 10 km cross-country interval run | Recreational runners (n = 53 [34 M + 19 W]) | Pre-exercise, immediately after |
| Incremental test on treadmill (until exhaustion) | Well-trained male athletes (n = 9) | Pre-exercise, immediately after, post-exercise (30 min) | |
| Strenuous treadmill until exhaustion | Well-trained endurance male athlete (n = 1), moderately trained female participant (n = 1), well-trained recreational male runner (n = 1) | Pre-exercise, mid-exercise (3, 6, 9, 12, 15 min), post-exercise (5, 10, 15, 20, 30 min) | |
| de Sousa et al., 2012 | Overload training programme (day 1–8) then 10 × 800 m sprints on day 9 | Highly competitive male endurance runners (n = 24) | Day 1, day 9 (pre-exercise [–140 min], post-exercise [immediate, 80 min]) |
| Breitbach et al., 2014a | Treadmill until exhaustion (average 17.9 min) | Male athletes (n = 26 [13 handball players + 13 triathletes]) | Pre-exercise, post-exercise |
| Beiter et al., 2014 | Increment treadmill until exhaustion | Well-trained male athletes (n = 6) | Pre-exercise, post-exercise (immediately), post-exercise (30 min) |
| High-intensity 60 min cycling | Untrained males (n = 6) | Pre-exercise, post-exercise (immediately), post-exercise (3 hr) | |
| Regularly endurance trained males (n = 6) | Pre-exercise, post-exercise (immediately), post-exercise (3 hr) | ||
| Breitbach et al., 2014b | 10 km relay race | Recreational runners (n = 10 [6 M + 4 F]) | Pre-exercise, post-exercise |
| Tug et al., 2015 | Incremental treadmill test | Healthy male controls (n = 3) | Pre-exercise, post-exercise (immediately), post-exercise (90 min) |
| Healthy female controls (n = 3) | |||
| Sex-mismatched haematopoietic stem cell transplantation patients (n = 5 females with male donors) | |||
| Sex-mismatched haematopoietic stem cell transplantation patients (n = 2 males with female donors) | |||
| Helmig et al., 2015 | Incremental treadmill test until exhaustion | Physically active men (n = 5) | Pre-exercise, post-exercise (immediately after, 10, 30, 90 min) |
| Frühbeis et al., 2015 | Increment cycling test until exhaustion | Physically active male (more than 3 hr/week) tested twice (n = 1) | Pre-exercise, mid-exercise (3, 6, 9, 12, 15, 18, 21 min), post-exercise (immediately after, 10, 30, 90 min) |
| Tug et al., 2017b | Acute strength exercise (whole-body exercises, deadlifts, squats and muscle-targeted exercises) | Regular strength trained men (n = 16) | 12th, 13th, 14th, 15th, 16th exercise |
| High-intensity training | n = 5/16 | Before first exercise, after last exercise | |
| Differential training | n = 5/16 | Before first exercise, after last exercise | |
| Conservation training | n = 6/16 | Before first exercise, after last exercise | |
| Tug et al., 2017a | Incremental bicycle exercise until exhaustion | Competitive male cyclists (n = 11) | Pre-exercise, post-exercise, post-exercise (90 min) |
| Stawski et al., 2017 | Treadmill until exhaustion | Averaged-trained men (n = 11) | Pre- and post-1st bout, 2nd bout and 3rd bout of exercise |
| Haller et al., 2017 | Stepwise increment running test until exhaustion | Athletes (n = 14 [7 M + 7 W]) | Pre-exercise, mid-exercise (3, 6, 9, 12, 15, 18, 21 min), post-exercise (15, 30 min) |
| 40 min endurance run at 9.6 km/hr | Athletes (n = 13 [7 M + 6 W]) | Pre-exercise, post-exercise | |
| Hummel et al., 2018 | Treadmill until exhaustion | Male students of sports science (n = 20) | Pre-exercise (–2 min), post-exercise (2, 15, 30, 40 min) |
| Haller et al., 2018 | 5 × 40 m sprints (5.94 ± 0.50 s) | Healthy subjects (n = 9 [7 M + 2 F]) | Pre-exercise, post-exercise |
| Treadmill test | Male football players playing more than 70 min in game and participated in treadmill test (n = 10) | Pre-exercise, post-exercise | |
| Season football game | Pre-exercise, post-exercise | ||
| Ferrandi et al., 2018 | High-intensity interval exercise (30 min) | Healthy male subjects (n = 14 [seven normal weight and seven obese]) | Pre-exercise, post-exercise, post-exercise (1 hr) |
| Ohlsson et al., 2020 | Cycling until maximal heart rate | Healthy volunteers (n = 8 [4 M and 4 W]) | Pre-exercise, sub-max load, max load, post-exercise (30, 90 min) |
| Mavropalias et al., 2021 | Eccentric cycling | Men unaccustomed to eccentric exercise (n = 20) | Pre-exercise, post-exercise, post-exercise (24, 48, 72 hr) |
2.1.1 Acute exercise
Twenty-two individual studies on cirDNA and acute exercise were identified. In acute exercise, all studies reviewed reported a significant increase in cirDNA during exercise and a decline to pre-exercise levels after cessation. This applied in both resistance and endurance exercise. Resistance exercise works to enhance the strength and build skeletal muscles by repeatedly overcoming resistance force. Two studies in this category reported a 1.4- to 1.7-fold and 3-fold increase in cirDNA after performing strength exercise (Tug et al., 2017b) and weightlifting exercises (Atamaniuk et al., 2010), respectively.
Endurance exercise is activity that increases breathing and heart rate, such as walking, jogging and cycling. Five studies used cycling regime to test their participants. All reported a significant increase in cirDNA ranging from 1.6- to 7.82-fold (Beiter et al., 2014; Frühbeis et al., 2015; Mavropalias et al., 2021; Ohlsson et al., 2020; Tug et al., 2017a). All remaining endurance studies subjected participants to running, ranging from 800 m sprints to 246 km ultra-marathons, with the majority using ‘treadmill test until exhaustion’ (Table 3). All studies reported the same transient rise and fall cirDNA pattern, spanning from 1.6- to 18.6-fold increase from pre-exercise level.
Endurance exercise appears to induce a larger cirDNA response than resistance exercise. Nearly half (10/25) of the endurance exercises reported cirDNA increases ≥9-fold, and the maximum reported increase was 18.6-fold (Atamaniuk et al., 2004). In contrast, amongst the resistance studies, the highest difference was a threefold increase in cirDNA after weightlifting (Atamaniuk et al., 2010). However, this needs further investigation as the number of studies examining resistance exercise was limited to 2.
Duration and intensity of acute exercise
There is some evidence for a positive relationship between duration of exercise and fold change in cirDNA. Mavropalias and colleagues investigated the effect of exercise intensity by splitting their cohort of 20 men into low- or high-intensity eccentric cycling groups. High-intensity cycling induced a significantly higher cirDNA increase in plasma than low-intensity cycling (Mavropalias et al., 2021). Furthermore, five 40 m sprint sessions with long rest intervals (5 min) caused a lower rise in cirDNA than five sprint sessions with short rest intervals (1 min) (Haller et al., 2018), and 24 competitive endurance runners reported a >9.8-fold increase after ten 800 m sprints (de Sousa et al., 2012), while 14 ultra-marathon runners experienced roughly an 18-fold increase after a 6 hr race, with a level above baseline persisting for at least 2 hr (Atamaniuk et al., 2008). Additionally, Haller et al., 2017 and Haller et al., 2018 showed a positive association between duration and distance covered and cirDNA increase during a low-intensity running exercise (Haller et al., 2017) and a football game (Haller et al., 2018), respectively.
Kinetics of cirDNA change during acute exercise
The kinetics of cirDNA during exercise indicate rapid initiation of clearance, with cirDNA peaking either immediately (Fatouros et al., 2010; Haller et al., 2017), 15 min (Hummel et al., 2018) or 30 min (Ohlsson et al., 2020) after exercise. The time required for cirDNA levels to return to baseline is not well defined as studies have reported both elevated (Ohlsson et al., 2020) and a return to baseline levels (Frühbeis et al., 2015) 1.5 hr post-cycling exercise.
Grouping participant results in kinetic studies might not be appropriate due to interindividual differences in cirDNA clearance. Beiter et al., 2011 examined the variation in cirDNA kinetics between individuals, subjecting three people to a treadmill test until exhaustion: one well-trained male endurance athlete, one moderately trained female participant and one well-trained recreational male runner. Although all three had the same general transient pattern, the peak occurred at different times and the decline time also varied (Beiter et al., 2011).
Since 55% of cirDNA comes from leukocytes (Moss et al., 2018), it is possible that the kinetics of leukocytes during exercise influence the kinetics of cirDNA. Increases in leukocyte number during exercise have been observed in several studies (de Sousa et al., 2012; Ohlsson et al., 2020; Tug et al., 2017a). For example, during a cycling exercise, the number of leukocytes peaked at maximal workload while the cirDNA level peaked 30 min after the cessation of exercise (Ohlsson et al., 2020). This burst of cirDNA occurring just after the leukocyte peak could be the result of leukocyte apoptosis during exercise (Krüger and Mooren, 2014). Additionally, circulating DNases may play a part in the clearance of cirDNA following exercise. Beiter et al., 2014 found that DNase activity follows the kinetic pattern of cirDNA, rising by 15-fold immediately after a treadmill test and decreasing to pre-exercise activity levels after 30 min. Moreover, exercise changes blood and plasma volume, which might also affect total cirDNA quantitation (Fellmann, 1992; Kawabata et al., 2004).
Individual fitness
Individual fitness levels appear to have little impact on cirDNA increase and clearance rates. Beiter et al., 2014 investigated the difference in cirDNA changes between untrained and endurance-trained males after 60 min of high-intensity cycling. Both groups had similar pre-exercise cirDNA levels, and the untrained and trained group had 6.9- and 4.5-fold increases, respectively. For both groups, cirDNA returned to normal after 3 hr and there was no statistically significance difference between the two groups in the way the cirDNA level responded to exercise.
Sex differences in cirDNA change during exercise
It is difficult to conclude if there are any differences in the way cirDNA levels respond to exercise in men compared to women. Half of the research studies conducted (11/21) involved male subjects only. Eight studies had a mix of males and females with equal or near equal representation, while two consisted predominantly of male subjects (Table 3). The lack of equal representation is an ongoing issue in the field of sports science, including in cirDNA-related exercise studies, which we highlighted in our recent publication (Hagstrom et al., 2021). Furthermore, in all studies except one, the data on male and female participants were combined, making delineation of sex differences not possible.
2.1.2 Chronic exercise
Six individual studies on cirDNA and chronic exercise were identified, far fewer studies compared to acute exercise. Overall, it appears to have less robust effects than acute exercise. The chronic exercise studies ranged in duration from 8 days (de Sousa et al., 2012) to 6 months (Tosevska et al., 2016), and the predominant exercise examined was resistance-type (4/6 studies) rather than endurance-type (2/6 studies). In all studies, blood samples were collected at least 1 day following cessation of exercise to avoid the confounding effect of acute exercise.
No change in cirDNA levels was observed following a chronic intense running programme in male endurance runners (de Sousa et al., 2012), resistance training in 23 (control group) and 27 (resistance training) elderly participants (Tosevska et al., 2016) or 8 weightlifters (Gentles et al., 2017). In contrast, two studies reported a significant cirDNA increase after performing resistance multi-joint exercises (Fatouros et al., 2006) and a range of strength exercises (Tug et al., 2017b) in 17 recreationally and 16 regularly trained men, respectively. One study of male soccer players observed a significant mid-season cirDNA increase only in players who started games in autumn season (A. Gentles et al., 2015).
Inconsistent effects of chronic exercise intensity are also reported. Fatouros et al., 2006 subjected participants to four 3-week training blocks of varying intensity and found that cirDNA peaked during the highest volume of training and fell as training intensity was decreased. This is opposed by the finding of Tug et al., 2017b that neither low- nor high-intensity acute strength training showed significant association with cirDNA levels. In addition, the frequency of habitual exercise (ranging from 0 to 7 times a week) had no association with cirDNA levels in 14 healthy women (Brodbeck et al., 2020).
2.1.3 Origin of cirDNA increase during exercise
The increase in cirDNA during exercise has been attributed to apoptosis due to the ladder pattern of DNA fragments (Thierry et al., 2016). This pattern is clearly shown in plasma collected before an ultra-marathon race, immediately after, and 2, and 4 hr after the race (Atamaniuk et al., 2008).
Sex-mismatched haematopoietic stem cell transplantation provides a means to determine whether the exercise-induced cirDNA increase originates from haematopoietic lineage cells. In one study, male and female patients with sex-mismatched transplant donors performed incremental treadmill exercise until exhaustion and their total and Y-chromosome cirDNA levels were measured. The results showed that most of the increase in cirDNA is from haematopoietic cells and not from the liver (Tug et al., 2015). Further evidence supporting exercise-induced leukocyte apoptosis is the significant decrease of Bcl2 mRNA expression immediately after exercise, while Bax and Bad mRNA levels increased slightly (Atamaniuk et al., 2008). However, post-exercise blood smears and immunohistochemistry indicated that the damaged cells are neutrophils undergoing a phenomenon termed neutrophil extracellular traps (NETs). In another study, cirDNA was positively associated with myeloperoxidase which is abundant in primary granules of neutrophils (Beiter et al., 2014), providing further evidence for the role of neutrophils in the origin of cirDNA.
Another clear candidate for a cirDNA source during exercise is skeletal muscle; however, only one study to date has specifically measured muscle-derived cirDNA in this setting. Surprisingly, no increase in skeletal muscle-derived cirDNA, as identified via the methylated HOXD4 promoter, was observed after exercise. The authors only analysed 5 out of 20 men recruited in this tissue-origin investigation (Mavropalias et al., 2021). Muscle tissue does not normally contribute to cirDNA (Moss et al., 2018); however, biochemical markers of tissue damage such as creatinine kinase and myoglobin have been reported (Nédélec et al., 2012; Thorpe and Sunderland, 2012). More research is required to validate the result by Mavropalias et al., 2021 and also to determine other possible sources of cirDNA in exercise.
2.2 Alcohol
There is a strong association between alcohol consumption and increased risk of cancers such as liver, breast, oesophageal and pancreatic cancer (Ratna and Mandrekar, 2017). Due to the DNA-damaging properties of alcohol, it has been hypothesised that cirDNA levels increase as a result of alcohol-induced apoptosis (Brooks and Theruvathu, 2005).
Two studies measured association between alcohol consumption and plasma cirDNA levels (Hsieh et al., 2016; Kim et al., 2014) and found no correlation between alcohol intake and cirDNA concentration in either 24 healthy subjects, 23 gastric cancer patients (Kim et al., 2014) or 81 oesophageal cancer patients (Hsieh et al., 2016). Their technical limitations include missing methodological reporting, non-specialised cirDNA extraction kit and no clear specification of alcohol intake used for ‘moderate-severe’ categorisation (Kim et al., 2014) as well as the grouping of ‘social drinker’ and ‘had quit drinking for >5 years’ subjects into a single cohort (Hsieh et al., 2016). Combining data from ‘social drinkers’ with ‘non-drinkers’ can obscure physiological effects since people with long-term abstinence can have different health characteristics to current drinkers (Fein et al., 2006; Sullivan et al., 2010).
In both studies, alcohol consumption was recorded as a part of investigating plasma cirDNA in the context of cancer. A more focused study that utilises protocols tailored to cirDNA measurements to confirm the effect of alcohol on cirDNA is needed. Both acute and chronic effects of alcohol should be investigated with clear information on alcohol intake amounts and duration. Recall bias is also a major issue in self-count-based studies which leads to under-reporting particularly for heavy and non-routine drinking (Boniface et al., 2014; Cherpitel et al., 2018).
2.3 Occupational hazard exposure
Two studies on cirDNA and occupational hazard exposure were identified. One study examined ionising radiation in 176 people working at nuclear sites (Korzeneva et al., 2015) and the second study examined pesticide exposure in 72 greenhouse workers (Çayir et al., 2018). cirDNA was significantly lower in subjects exposed to gamma-neutron radiation (n = 88) and chronic tritium β-radiation (n = 88) compared to a never-exposed group (n = 109). The authors postulated that this decrease may be due to an elevated level of DNase I in the exposed group (Korzeneva et al., 2015). The second study measured DNA directly from plasma and found that greenhouse workers exposed to pesticides for 5–15 years have near double cirDNA levels compared to non-exposed controls and showed a positive correlation between cirDNA concentration and pesticide exposure interval (Çayir et al., 2018). The strengths of the latter study include accounting for smoking, ethnic, social and cultural differences, as well as black tea consumption between exposed and control groups, but information on blood processing time was lacking and a second plasma centrifugation was omitted. Both studies have moderate combined sample sizes (160 control and 248 exposed subjects total). No analysis of the specific tissues that contribute to the increase in cirDNA concentration was carried out in either study.
2.4 Smoking
Cigarette smoke has potent DNA-damaging constituents (Pfeifer et al., 2002; Weng et al., 2018; Zhao et al., 2009); therefore, it is surprising that the documented effect of smoking on cirDNA is scarce. Smoking status is routinely collected in clinical records, especially in the context of cancer.
Ten individual studies on cirDNA and smoking were identified, containing 6 healthy cohorts and 13 cohorts that include cancer patients, women undergoing IVF treatment and greenhouse workers. Four out of six studies that included healthy cohorts reported no effect of smoking on cirDNA levels in a combined sample size of 444 (Catarino et al., 2012; Kim et al., 2014; Sozzi et al., 2003; Yoon et al., 2009). The remaining two studies reported opposing results – higher cirDNA level in former smokers (n = 8) versus current smokers (n = 12) in a study that used a non-specialised kit (van der Drift et al., 2010) and, conversely, higher cirDNA levels in current smokers (n = 13) versus non-smokers (n = 38) quantitated directly from plasma and measured within a cohort that did not segregate the pesticide-exposed greenhouse workers and unexposed controls (Çayir et al., 2018).
Amongst the cancer studies, four lung cancer (Catarino et al., 2012; Sozzi et al., 2003; van der Drift et al., 2010; Yoon et al., 2009), one oesophageal squamous cell cancer (Hsieh et al., 2016) and one thyroid cancer (Caglar et al., 2020) study reported no effect of smoking on cirDNA levels. One gastric cancer study reported significantly lower cirDNA amount in current smokers versus former smokers and non-smokers (Kim et al., 2014). The authors suggested that this may be because the cancer type that occurs in the aged, female, non-smoking cohort is more aggressive than others.
There were no cirDNA differences between former and current smokers versus non-smokers in a group of 37 women undergoing IVF-embryo transfer treatment (Czamanski-Cohen et al., 2013) or in T2D patients (Bryk et al., 2019). cirDNA was not associated with number of packs per year (Yoon et al., 2009), or smoking duration; however, smokers did have more extreme elevated values among cancer-free individuals, possibly reflecting smoking-associated health problems (Sozzi et al., 2003).
One limitation across the published studies is the imbalance of non-smoking and smoking cohorts. For example, in the study conducted by Sozzi et al., 2003, there were 7 never smokers, and 82 and 65 smokers in the healthy controls and lung cancer patients, respectively. This can be controlled for in future investigations, as well as matching the groups in age and gender. Due to the self-reported nature of smoking data and the tendency for underestimation (Connor Gorber et al., 2009), large cohort numbers would also be important.
3 Other factors
Many other variables have been investigated in smaller individual studies. No effect on cirDNA has been noted in studies examining height (Breitbach et al., 2014a), spring versus autumn season (Çayir et al., 2018), number of blood volunteering times (Zhong et al., 2007), history of betel nut chewing (Hsieh et al., 2016) or haematocrit or cannula placement pain (Brodbeck et al., 2020).
There is evidence that meal-derived DNA is present in the circulation. This DNA is mostly intact (>10 kbp) (Spisák et al., 2013). However, whether this impacts measurably on the cirDNA concentration remains unclear. Only a single study, which found no relationship between cirDNA and time since last food intake, has been published (Meddeb et al., 2019), and the effect of specific foods has not been examined.
4. Study methodology
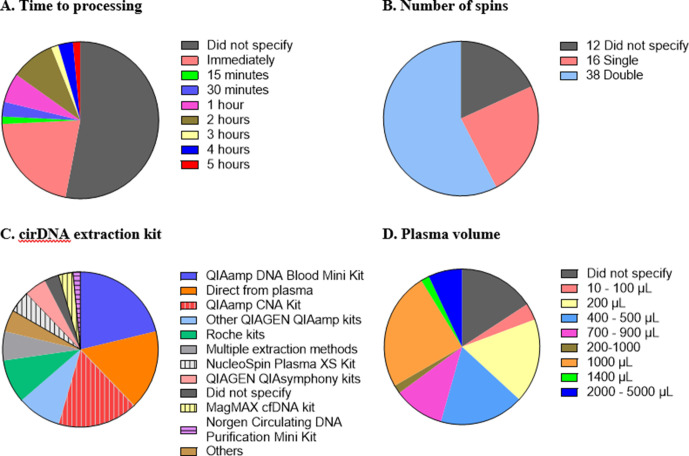
While there is general agreement that standardised methodology and complete reporting of experimental parameters is desirable, consensus for a standardised set of protocols for cirDNA analysis has not been developed. There are numerous steps in cirDNA analysis, starting from blood collection all the way through to quantification, and variation at each step creates difficulty in comparing studies and a hindrance in translating biomarkers to the clinic. Here, we highlight some of the differences in the technical aspects of the 66 publications reviewed (Figure 1).
Figure 1. Technical aspects and protocol reporting in the 66 publications summarised in this review.
(A) Interval time between blood collection and processing. (B) Number of centrifugations performed to obtain plasma samples from whole blood. (C) cirDNA extraction methods (specialised cirDNA kits are denoted by stripes). (D) Input volume of plasma into extraction (D).
Blood collection tube
A range of tubes for blood collection and plasma separation are available, including tubes stabilised to avoid leukocyte lysis. Most studies used EDTA tubes; however, 3 studies used heparin-based additives (Atamaniuk et al., 2010; Korzeneva et al., 2015; Sozzi et al., 2001), 15 studies did not specify the tube type (Supplementary file 1) and 2 were ambiguous (Czamanski-Cohen et al., 2013; Korabecna et al., 2011). The study by Meddeb et al., 2019 used Streck tubes when measuring the effect of circadian rhythm, and included a direct comparison to EDTA tubes, with no consistent differences observed.
Time to blood processing
It is important that the time between blood collection and plasma processing is considered and reported as prolonged blood storage allows leukocytes to lyse and hence create genomic DNA contamination (Trigg et al., 2018; Warton et al., 2014). Different studies have used different ‘cutoff’ times such as 1 (Ohlsson et al., 2020; van der Drift et al., 2010), two (Brodbeck et al., 2020; Spindler et al., 2014) or 5 (Bu et al., 2020) hr. Out of the 66 studies, 35 (53%) did not provide any information regarding the duration between blood collection and processing. Of the 31 studies that do specify the time to processing, all fall within a reasonable time, with a maximum of 5 hr between blood collection and plasma separation (Figure 1A).
Number of spins
A key step in blood processing for cirDNA extraction is centrifugation to separate the plasma from the red blood cells and leukocytes. Thirty-eight out of 66 studies (58%) centrifuged the blood samples twice, 16 studies (24%) did so once and 12 studies (18%) did not specify (Figure 1B). The role of the second spin is to minimise the potential for leukocyte contamination (Trigg et al., 2018), especially in case of inaccurate pipetting.
cirDNA extraction
Sixty-four studies used a single extraction method while three utilised multiple methods to analyse the same cohort, including quantifying the cirDNA directly from plasma. In total, there are 11 studies that omitted the extraction step and quantitated cirDNA directly (Figure 1C).
Most studies used commercial kits to purify cirDNA. There are several kits available to specifically extract cirDNA such as QIAamp Circulating Nucleic Acid (CNA) Kit, NucleoSpin Plasma XS Kit, MagMAX Cell-free DNA Isolation Kit and Circulating DNA Purification Mini Kit. Only 37% of the 46 studies that involved a DNA extraction step used a kit specifically formulated for cirDNA. Using non-specialised kits results in substantially reduced cirDNA yields (Devonshire et al., 2014; Warton et al., 2018). For example, a comparison of the QIAamp CNA kit and the QIAamp DNA Blood Mini kit showed that the latter extracted less than one third of the DNA extracted by QIAamp CNA kit, with a bias towards high-molecular-weight DNA (Warton et al., 2018).
Out of these studies that did not use a dedicated kit, nearly half used QIAGEN kits (mostly QIAamp DNA Blood Mini Kit) and the remaining used a variety of other kits such as MagNA Pure LC DNA Isolation Kit-Large Volume. Some studies used various non-kit methods such as phenol-chloroform-based extraction (Jylhävä et al., 2011; Korzeneva et al., 2015; Tug et al., 2015) and in-house protocols (Tamkovich et al., 2005). Only two studies did not specify any information about DNA extraction method, nor if they did so.
Volume of plasma used for extraction/quantitation
Both more (Alborelli et al., 2019) and less (Devonshire et al., 2014) efficient extraction of cirDNA has been reported with increasing plasma volume. About 40% of the studies used volumes below 1 mL for cirDNA extraction, down to as low as 50 µL (Tug et al., 2015; Figure 1D). Some of the low starting amounts are likely due to kit configuration, for example, the QIAamp DNA Blood Mini Kit specifies 1–200 µL of sample input. This again highlights the importance of using the appropriate kit to extract cirDNA.
Quantitation method
The quantitation methods were predominantly qPCR, which remains the ‘gold standard’ for cirDNA quantitation (just over 50% of studies), followed by Qubit. Other means of quantitation were PicoGreen, cell death detection ELISA, SYBR nucleic acid gel stain, DNA DipStick TM Kit and GB genetic human DNA assay.
It is apparent in this analysis of 66 studies that there remain major inconsistences in the methods used to extract and analyse cirDNA. This not only raises questions about the validity of individual results but makes comparing studies and evaluating results difficult.
Conclusion
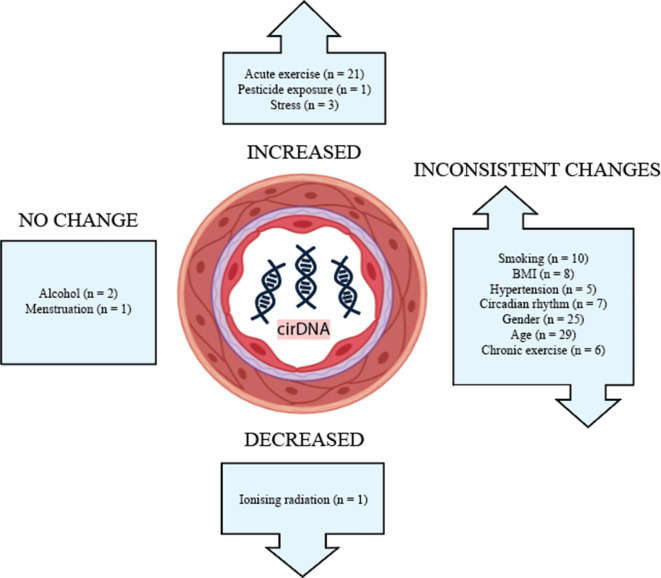
The effects of lifestyle and biological factors on cirDNA are summarised in Figure 2. Despite technical and methodological variation between studies, acute exercise has consistently been shown to produce a robust but transient increase in cirDNA. The effect of exercise is very pronounced, with increases in cirDNA concentration that dwarf the rises reported in some disease states. In most exercise regimes, cirDNA returns to baseline level within a short amount of time (30–60 min); however, rigorous exercise induces a slower decline, with a measurable increase persisting at 48 hr (Margeli et al., 2005). Furthermore, the lowest level of exercise required for a measurable increase in cirDNA is not known, thus we propose limiting physical activity prior to a blood draw as a strategy to decrease baseline variation and improve capacity to detect differences between study groups. In line with this, study methods should report whether participant physical activity was controlled for.
Figure 2. The effect of biological and lifestyle factors on blood plasma cirDNA concentration in healthy individuals and patients with various diseases and treatments.
Alcohol use and menstruation appear to have a negligible effect on cirDNA levels; however, the number of studies is small. Most other biological and lifestyle factors have been reported to both increase and decrease cirDNA levels. Better-designed and disaggregated studies are required to confidently rule in or out their effect.
Addressing each of these factors to accurately answer how they impact cirDNA level would require a very large study with a substantial number of participants and multidiscipline expertise to ensure that each factor is investigated and controlled properly. If this type of study was to be conducted, the best practice should be applied. Blood should be collected in a single-tube type, with short and consistent time between blood collection and centrifugation. Double centrifugation and specialised cirDNA kit for extraction should also be used.
A step towards obtaining more reliable data is choosing methods appropriate for cirDNA analysis, as well as careful sample handling and detailed reporting of protocols. Transparency in disclosing the way samples are processed and analysed may be aided by the development of reporting guidelines analogous to the Minimum Information for Publication of Quantitative Real-Time PCR Experiments (MIQE) guidelines (Bustin et al., 2009).
There remain large knowledge gaps in how common biological and lifestyle factors impact cirDNA. An understanding of cirDNA dynamics outside of a disease context is important for establishing accurate baseline levels and developing sensitive clinical tests that minimise the confounding effect of healthy variation.
Acknowledgements
NY was supported by the Australian Government Research Training Program (RTP) Stipend through The University of New South Wales, Beth Yarrow Memorial Award in Medical Science and Translational Cancer Research Network PhD Scholarship Top Up Award, via the Cancer Institute NSW. KW was supported by Ovarian Cancer Research Foundation (GA-2018-14) and CAMILLA AND MARC. The funders had no role in the decision to publish or preparation of the manuscript. The authors also acknowledge The University of New South Wales (Lowy Cancer Research Centre) for providing support for carrying out the review.
Funding Statement
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Contributor Information
Caroline Elizabeth Ford, Email: caroline.ford@unsw.edu.au.
Y M Dennis Lo, The Chinese University of Hong Kong, Hong Kong.
Y M Dennis Lo, The Chinese University of Hong Kong, Hong Kong.
Funding Information
This paper was supported by the following grants:
CAMILLA AND MARC to Kristina Warton.
Australian Research Training Program to Nicole Laurencia Yuwono.
Translational Cancer Research Network to Nicole Laurencia Yuwono.
Beth Yarrow Memorial Fund to Nicole Laurencia Yuwono.
Ovarian Cancer Research Foundation GA-2018-14 to Kristina Warton.
Additional information
Competing interests
No competing interests declared.
holds stock in Guardant Health, Exact Sciences and Epigenomics AG.
Author contributions
Conceptualization, Project administration, Writing – original draft, Writing – review and editing.
Conceptualization, Funding acquisition, Project administration, Supervision, Writing – review and editing.
Conceptualization, Funding acquisition, Project administration, Supervision, Writing – review and editing.
Additional files
References
- A. Gentles J, G. Hornsby W, S. Gray H, A. Miller J, R. Dotterweich A, A. Stuart C, H. Stone M. Changes in cell free DNA during a college soccer season. Journal of Trainology. 2015;4:25–31. doi: 10.17338/trainology.4.1_25. [DOI] [Google Scholar]
- Ackermann K, Revell VL, Lao O, Rombouts EJ, Skene DJ, Kayser M. Diurnal Rhythms in Blood Cell Populations and the Effect of Acute Sleep Deprivation in Healthy Young Men. Sleep. 2012;35:933–940. doi: 10.5665/sleep.1954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Goblan AS, Al-Alfi MA, Khan MZ. Mechanism linking diabetes mellitus and obesity. Diabetes, Metabolic Syndrome and Obesity. 2014;7:587–591. doi: 10.2147/DMSO.S67400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alborelli I, Generali D, Jermann P, Cappelletti MR, Ferrero G, Scaggiante B, Bortul M, Zanconati F, Nicolet S, Haegele J, Bubendorf L, Aceto N, Scaltriti M, Mucci G, Quagliata L, Novelli G. Cell-free DNA analysis in healthy individuals by next-generation sequencing: a proof of concept and technical validation study. Cell Death & Disease. 2019;10:534. doi: 10.1038/s41419-019-1770-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alghofaili L, Almubarak H, Gassem K, Islam SS, Coskun S, Kaya N, Karakas B. Cell-free DNA levels of twins and sibling pairs indicate individuality and possible use as a personalized biomarker. PLOS ONE. 2019;14:e0223470. doi: 10.1371/journal.pone.0223470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerlaan W, Betsou F. Biospecimen Science of Blood for cfDNA Genetic Analyses. Current Pathobiology Reports. 2019;7:9–15. doi: 10.1007/s40139-019-00193-7. [DOI] [Google Scholar]
- Armstrong GM, Maybin JA, Murray AA, Nicol M, Walker C, Saunders PTK, Rossi AG, Critchley HOD. Endometrial apoptosis and neutrophil infiltration during menstruation exhibits spatial and temporal dynamics that are recapitulated in a mouse model. Scientific Reports. 2017;7:17416. doi: 10.1038/s41598-017-17565-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atamaniuk J, Vidotto C, Tschan H, Bachl N, Stuhlmeier KM, Müller MM. Increased concentrations of cell-free plasma DNA after exhaustive exercise. Clinical Chemistry. 2004;50:1668–1670. doi: 10.1373/clinchem.2004.034553. [DOI] [PubMed] [Google Scholar]
- Atamaniuk J, Stuhlmeier KM, Vidotto C, Tschan H, Dossenbach-Glaninger A, Mueller MM. Effects of ultra-marathon on circulating DNA and mRNA expression of pro- and anti-apoptotic genes in mononuclear cells. European Journal of Applied Physiology. 2008;104:711–717. doi: 10.1007/s00421-008-0827-2. [DOI] [PubMed] [Google Scholar]
- Atamaniuk J, Vidotto C, Kinzlbauer M, Bachl N, Tiran B, Tschan H. Cell-free plasma DNA and purine nucleotide degradation markers following weightlifting exercise. European Journal of Applied Physiology. 2010;110:695–701. doi: 10.1007/s00421-010-1532-5. [DOI] [PubMed] [Google Scholar]
- Beiter T, Fragasso A, Hudemann J, Niess AM, Simon P. Short-term treadmill running as a model for studying cell-free DNA kinetics in vivo. Clinical Chemistry. 2011;57:633–636. doi: 10.1373/clinchem.2010.158030. [DOI] [PubMed] [Google Scholar]
- Beiter T, Fragasso A, Hudemann J, Schild M, Steinacker J, Mooren FC, Niess AM. Neutrophils release extracellular DNA traps in response to exercise. Journal of Applied Physiology. 2014;117:325–333. doi: 10.1152/japplphysiol.00173.2014. [DOI] [PubMed] [Google Scholar]
- Beranek M, Fiala Z, Kremlacek J, Andrys C, Krejsek J, Hamakova K, Chmelarova M, Palicka V, Borska L. Changes in circulating cell-free DNA and nucleosomes in patients with exacerbated psoriasis. Archives of Dermatological Research. 2017;309:815–821. doi: 10.1007/s00403-017-1785-5. [DOI] [PubMed] [Google Scholar]
- Bhowmik B, Afsana F, Ahmed T, Akhter S, Choudhury HA, Rahman A, Ahmed T, Mahtab H, Azad Khan AK. Obesity and associated type 2 diabetes and hypertension in factory workers of Bangladesh. BMC Research Notes. 2015;8:460. doi: 10.1186/s13104-015-1377-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boniface S, Kneale J, Shelton N. Drinking pattern is more strongly associated with under-reporting of alcohol consumption than socio-demographic factors: evidence from a mixed-methods study. BMC Public Health. 2014;14:1297. doi: 10.1186/1471-2458-14-1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitbach S, Tug S, Simon P. Circulating Cell-Free DNA. Sports Medicine. 2012;42:565–586. doi: 10.2165/11631380-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Breitbach S, Sterzing B, Magallanes C, Tug S, Simon P. Direct measurement of cell-free DNA from serially collected capillary plasma during incremental exercise. Journal of Applied Physiology. 2014a;117:119–130. doi: 10.1152/japplphysiol.00002.2014. [DOI] [PubMed] [Google Scholar]
- Breitbach S, Tug S, Helmig S, Zahn D, Kubiak T, Michal M, Gori T, Ehlert T, Beiter T, Simon P. Direct quantification of cell-free, circulating DNA from unpurified plasma. PLOS ONE. 2014b;9:e87838. doi: 10.1371/journal.pone.0087838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodbeck K, Schick S, Bayer B, Anslinger K, Krüger K, Mayer Z, Holdenrieder S, Peldschus S. Biological variability of cell-free DNA in healthy females at rest within a short time course. Ternational Journal of Legal Medicine. 2020;134:911–919. doi: 10.1007/s00414-019-02240-9. [DOI] [PubMed] [Google Scholar]
- Brooks PJ, Theruvathu JA. DNA adducts from acetaldehyde: implications for alcohol-related carcinogenesis. Alcohol. 2005;35:187–193. doi: 10.1016/j.alcohol.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Bryk AH, Prior SM, Plens K, Konieczynska M, Hohendorff J, Malecki MT, Butenas S, Undas A. Predictors of neutrophil extracellular traps markers in type 2 diabetes mellitus: associations with a prothrombotic state and hypofibrinolysis. Cardiovascular Diabetology. 2019;18:49. doi: 10.1186/s12933-019-0850-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bu J, Lee TH, Jeong W-J, Poellmann MJ, Mudd K, Eun HS, Liu EW, Hong S, Hyun SH. Enhanced detection of cell-free DNA (cfDNA) enables its use as a reliable biomarker for diagnosis and prognosis of gastric cancer. PLOS ONE. 2020;15:e0242145. doi: 10.1371/journal.pone.0242145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bustin SA, Benes V, Garson JA, Hellemans J, Huggett J, Kubista M, Mueller R, Nolan T, Pfaffl MW, Shipley GL, Vandesompele J, Wittwer CT. The MIQE Guidelines: Minimum Information for Publication of Quantitative Real-Time PCR Experiments. Clinical Chemistry. 2009;55:611–622. doi: 10.1373/clinchem.2008.112797. [DOI] [PubMed] [Google Scholar]
- Butkevich A, Abraham C, Phillips RA. Hormone replacement therapy and 24-hour blood pressure profile of postmenopausal women. American Journal of Hypertension. 2000;13:1039–1041. doi: 10.1016/S0895-7061(00)00284-3. [DOI] [PubMed] [Google Scholar]
- Caglar O, Cilgin B, Eroglu M, Cayir A. Evaluation of circulating cell free DNA in plasma as a biomarker of different thyroid diseases. Brazilian Journal of Otorhinolaryngology. 2020;86:321–326. doi: 10.1016/j.bjorl.2018.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catarino R, Coelho A, Araújo A, Gomes M, Nogueira A, Lopes C, Medeiros R. Circulating DNA: Diagnostic Tool and Predictive Marker for Overall Survival of NSCLC Patients. PLOS ONE. 2012;7:e38559. doi: 10.1371/journal.pone.0038559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Çayir A, Coskun M, Coskun M, Cobanoglu H. DNA damage and circulating cell free DNA in greenhouse workers exposed to pesticides. Environmental and Molecular Mutagenesis. 2018;59:161–169. doi: 10.1002/em.22148. [DOI] [PubMed] [Google Scholar]
- Chen K-Z, Lou F, Yang F, Zhang J-B, Ye H, Chen W, Guan T, Zhao M-Y, Su X-X, Shi R, Jones L, Huang XF, Chen S-Y, Wang J. Circulating Tumor DNA Detection in Early-Stage Non-Small Cell Lung Cancer Patients by Targeted Sequencing. Scientific Reports. 2016;6:31985. doi: 10.1038/srep31985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherpitel CJ, Ye Y, Stockwell T, Vallance K, Chow C. Recall bias across 7 days in self-reported alcohol consumption prior to injury among emergency department patients. Drug and Alcohol Review. 2018;37:382–388. doi: 10.1111/dar.12558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor Gorber S, Schofield-Hurwitz S, Hardt J, Levasseur G, Tremblay M. The accuracy of self-reported smoking: a systematic review of the relationship between self-reported and cotinine-assessed smoking status. Nicotine & Tobacco Research. 2009;11:12–24. doi: 10.1093/ntr/ntn010. [DOI] [PubMed] [Google Scholar]
- Coulet F, Blons H, Cabelguenne A, Lecomte T, Lacourreye O, Brasnu D, Beaune P, Zucman J, Laurent-Puig P. Detection of Plasma Tumor DNA in Head and Neck Squamous Cell Carcinoma by Microsatellite Typing and p53 Mutation Analysis. Cancer Research. 2000;60:707–711. [PubMed] [Google Scholar]
- Cristina SJL, Marta CM, Mercedes GS, Almudena PM, Álvaro HM, Luis VSJ, Tesifón PC. Characterization and evaluation of liver fibrosis grade in patients with chronic hepatitis B virus infection and normal transaminases. Clinical and Molecular Hepatology. 2018;24:384–391. doi: 10.3350/cmh.2018.0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czamanski-Cohen J, Sarid O, Cwikel J, Lunenfeld E, Douvdevani A, Levitas E, Har-Vardi I. Increased plasma cell-free DNA is associated with low pregnancy rates among women undergoing IVF-embryo transfer. Reproductive BioMedicine Online. 2013;26:36–41. doi: 10.1016/j.rbmo.2012.09.018. [DOI] [PubMed] [Google Scholar]
- Czamanski-Cohen J, Sarid O, Cwikel J, Levitas E, Lunenfeld E, Douvdevani A, Har-Vardi I. Decrease in cell free DNA levels following participation in stress reduction techniques among women undergoing infertility treatment. Archives of Women’s Mental Health. 2014;17:251–253. doi: 10.1007/s00737-013-0407-2. [DOI] [PubMed] [Google Scholar]
- Czeisler CA, Buxton OM. In: Principles and Practice of Sleep Medicine. Kryger MH, Roth T, Dement WC, editors. W.B. Saunders; 2011. Chapter 35 - The Human Circadian Timing System and Sleep–Wake Regulation; pp. 402–419. [Google Scholar]
- de Sousa MV, Madsen K, Fukui R, Santos A, da Silva MER. Carbohydrate supplementation delays DNA damage in elite runners during intensive microcycle training. European Journal of Applied Physiology. 2012;112:493–500. doi: 10.1007/s00421-011-2000-6. [DOI] [PubMed] [Google Scholar]
- Demir R, Yaba A, Huppertz B. Vasculogenesis and angiogenesis in the endometrium during menstrual cycle and implantation. Acta Histochemica. 2010;112:203–214. doi: 10.1016/j.acthis.2009.04.004. [DOI] [PubMed] [Google Scholar]
- Devonshire AS, Whale AS, Gutteridge A, Jones G, Cowen S, Foy CA, Huggett JF. Towards standardisation of cell-free DNA measurement in plasma: controls for extraction efficiency, fragment size bias and quantification. Analytical and Bioanalytical Chemistry. 2014;406:6499–6512. doi: 10.1007/s00216-014-7835-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatouros IG, Destouni A, Margonis K, Jamurtas AZ, Vrettou C, Kouretas D, Mastorakos G, Mitrakou A, Taxildaris K, Kanavakis E, Papassotiriou I. Cell-free plasma DNA as a novel marker of aseptic inflammation severity related to exercise overtraining. Clinical Chemistry. 2006;52:1820–1824. doi: 10.1373/clinchem.2006.070417. [DOI] [PubMed] [Google Scholar]
- Fatouros IG, Jamurtas AZ, Nikolaidis MG, Destouni A, Michailidis Y, Vrettou C, Douroudos II, Avloniti A, Chatzinikolaou A, Taxildaris K, Kanavakis E, Papassotiriou I, Kouretas D. Time of sampling is crucial for measurement of cell-free plasma DNA following acute aseptic inflammation induced by exercise. Clinical Biochemistry. 2010;43:1368–1370. doi: 10.1016/j.clinbiochem.2010.08.020. [DOI] [PubMed] [Google Scholar]
- Fein G, Torres J, Price LJ, Di Sclafani V. Cognitive performance in long-term abstinent alcoholic individuals. Alcoholism, Clinical and Experimental Research. 2006;30:1538–1544. doi: 10.1111/j.1530-0277.2006.00185.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fellmann N. Hormonal and plasma volume alterations following endurance exercise. A brief review. Sports Medicine. 1992;13:37–49. doi: 10.2165/00007256-199213010-00004. [DOI] [PubMed] [Google Scholar]
- Ferrandi PJ, Fico BG, Whitehurst M, Zourdos MC, Bao F, Dodge KM, Rodriguez AL, Pena G, Huang C-J. Acute high-intensity interval exercise induces comparable levels of circulating cell-free DNA and Interleukin-6 in obese and normal-weight individuals. Life Sciences. 2018;202:161–166. doi: 10.1016/j.lfs.2018.04.007. [DOI] [PubMed] [Google Scholar]
- Frank MO. Circulating Cell-Free DNA Differentiates Severity of Inflammation. Biological Research For Nursing. 2016;18:477–488. doi: 10.1177/1099800416642571. [DOI] [PubMed] [Google Scholar]
- Frühbeis C, Helmig S, Tug S, Simon P, Krämer-Albers E-M. Physical exercise induces rapid release of small extracellular vesicles into the circulation. Journal of Extracellular Vesicles. 2015;4:28239. doi: 10.3402/jev.v4.28239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaddameedhi S, Selby CP, Kemp MG, Ye R, Sancar A. The Circadian Clock Controls Sunburn Apoptosis and Erythema in Mouse Skin. The Journal of Investigative Dermatology. 2015;135:1119–1127. doi: 10.1038/jid.2014.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentles JA, Hornsby WG, Coniglio CL, Dotterweich AR, Miller JA, Stuart CA, Stone MH. Cell free DNA as a marker of training status in weightlifters. Biology of Sport. 2017;3:287–294. doi: 10.5114/biolsport.2017.67855. [DOI] [Google Scholar]
- Greystoke A, Harris G, Jenkins M, Goonetilleke D, Moore D, Lancashire M, Ranson M, Hughes A, Clack G, Dive C. Assessment of diurnal changes and confounding factors that affect circulating cell death biomarker levels: a short communication. Journal of Pharmaceutical and Biomedical Analysis. 2013;84:184–188. doi: 10.1016/j.jpba.2013.06.010. [DOI] [PubMed] [Google Scholar]
- Hagstrom AD, Yuwono N, Warton K, Ford CE. Sex Bias in Cohorts Included in Sports Medicine Research. Sports Medicine. 2021;51:1799–1804. doi: 10.1007/s40279-020-01405-6. [DOI] [PubMed] [Google Scholar]
- Haller N, Tug S, Breitbach S, Jörgensen A, Simon P. Increases in Circulating Cell-Free DNA During Aerobic Running Depend on Intensity and Duration. Ternational Journal of Sports Physiology and Performance. 2017;12:455–462. doi: 10.1123/ijspp.2015-0540. [DOI] [PubMed] [Google Scholar]
- Haller N, Helmig S, Taenny P, Petry J, Schmidt S, Simon P. Circulating, cell-free DNA as a marker for exercise load in intermittent sports. PLOS ONE. 2018;13:e0191915. doi: 10.1371/journal.pone.0191915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helmig S, Frühbeis C, Krämer-Albers EM, Simon P, Tug S. Release of bulk cell free DNA during physical exercise occurs independent of extracellular vesicles. European Journal of Applied Physiology. 2015;115:2271–2280. doi: 10.1007/s00421-015-3207-8. [DOI] [PubMed] [Google Scholar]
- Hsieh CC, Hsu HS, Chang SC, Chen YJ. Circulating Cell-Free DNA Levels Could Predict Oncological Outcomes of Patients Undergoing Esophagectomy for Esophageal Squamous Cell Carcinoma. Ternational Journal of Molecular Sciences. 2016;17:2131. doi: 10.3390/ijms17122131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummel EM, Hessas E, Müller S, Beiter T, Fisch M, Eibl A, Wolf OT, Giebel B, Platen P, Kumsta R, Moser DA. Cell-free DNA release under psychosocial and physical stress conditions. Translational Psychiatry. 2018;8:236. doi: 10.1038/s41398-018-0264-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahr S, Hentze H, Englisch S, Hardt D, Fackelmayer FO, Hesch RD, Knippers R. DNA fragments in the blood plasma of cancer patients: quantitations and evidence for their origin from apoptotic and necrotic cells. Cancer Research. 2001;61:1659–1665. [PubMed] [Google Scholar]
- Jenkins FJ, Van Houten B, Bovbjerg DH. Effects on DNA Damage and/or Repair Processes as Biological Mechanisms Linking Psychological Stress to Cancer Risk. Journal of Applied Biobehavioral Research. 2014;19:3–23. doi: 10.1111/jabr.12019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong DW, Moon J-Y, Choi Y-W, Moon H, Kim K, Lee Y-H, Kim S-Y, Kim Y-G, Jeong K-H, Lee S-H. Effect of blood pressure and glycemic control on the plasma cell-free DNA in hemodialysis patients. Kidney Research and Clinical Practice. 2015;34:201–206. doi: 10.1016/j.krcp.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang P, Lo YMD. The Long and Short of Circulating Cell-Free DNA and the Ins and Outs of Molecular Diagnostics. Trends in Genetics. 2016;32:360–371. doi: 10.1016/j.tig.2016.03.009. [DOI] [PubMed] [Google Scholar]
- Jiang J, Chen X, Sun L, Qing Y, Yang X, Hu X, Yang C, Xu T, Wang J, Wang P, He L, Dong C, Wan C. Analysis of the concentrations and size distributions of cell-free DNA in schizophrenia using fluorescence correlation spectroscopy. Translational Psychiatry. 2018;8:104. doi: 10.1038/s41398-018-0153-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jylhävä J, Kotipelto T, Raitala A, Jylhä M, Hervonen A, Hurme M. Aging is associated with quantitative and qualitative changes in circulating cell-free DNA: the Vitality 90+ study. Mechanisms of Ageing and Development. 2011;132:20–26. doi: 10.1016/j.mad.2010.11.001. [DOI] [PubMed] [Google Scholar]
- Jylhävä J, Jylhä M, Lehtimäki T, Hervonen A, Hurme M. Circulating cell-free DNA is associated with mortality and inflammatory markers in nonagenarians: the Vitality 90+ Study. Experimental Gerontology. 2012;47:372–378. doi: 10.1016/j.exger.2012.02.011. [DOI] [PubMed] [Google Scholar]
- Jylhävä J, Nevalainen T, Marttila S, Jylhä M, Hervonen A, Hurme M. Characterization of the role of distinct plasma cell-free DNA species in age-associated inflammation and frailty. Aging Cell. 2013;12:388–397. doi: 10.1111/acel.12058. [DOI] [PubMed] [Google Scholar]
- Jylhävä J, Lehtimäki T, Jula A, Moilanen L, Kesäniemi YA, Nieminen MS, Kähönen M, Hurme M. Circulating cell-free DNA is associated with cardiometabolic risk factors: The Health 2000 Survey. Atherosclerosis. 2014;233:268–271. doi: 10.1016/j.atherosclerosis.2013.12.022. [DOI] [PubMed] [Google Scholar]
- Karlas T, Weise L, Kuhn S, Krenzien F, Mehdorn M, Petroff D, Linder N, Schaudinn A, Busse H, Keim V, Pratschke J, Wiegand J, Splith K, Schmelzle M. Correlation of cell-free DNA plasma concentration with severity of non-alcoholic fatty liver disease. Journal of Translational Medicine. 2017;15:106. doi: 10.1186/s12967-017-1208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawabata T, Suzuki T, Miyagawa T. Effect of blood volume on plasma volume shift during exercise. Journal of Thermal Biology. 2004;29:775–778. doi: 10.1016/j.jtherbio.2004.08.054. [DOI] [Google Scholar]
- Kim K, Shin DG, Park MK, Baik SH, Kim TH, Kim S, Lee S. Circulating cell-free DNA as a promising biomarker in patients with gastric cancer: diagnostic validity and significant reduction of cfDNA after surgical resection. Annals of Surgical Treatment and Research. 2014;86:136–142. doi: 10.4174/astr.2014.86.3.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kokawa K, Shikone T, Nakano R. Apoptosis in the human uterine endometrium during the menstrual cycle. The Journal of Clinical Endocrinology & Metabolism. 1996;81:4144–4147. doi: 10.1210/jcem.81.11.8923873. [DOI] [PubMed] [Google Scholar]
- Korabecna M, Horinek A, Bila N, Opatrna S. In: Circulating Nucleic Acids in Plasma and Serum. Gahan P, editor. Springer; 2011. Circadian Rhythmicity and Clearance of Cell-Free DNA in Human Plasma; pp. 195–198. [DOI] [Google Scholar]
- Korzeneva IB, Kostuyk SV, Ershova LS, Osipov AN, Zhuravleva VF, Pankratova GV, Porokhovnik LN, Veiko NN. Human circulating plasma DNA significantly decreases while lymphocyte DNA damage increases under chronic occupational exposure to low-dose gamma-neutron and tritium β-radiation. Mutation Research. 2015;779:1–15. doi: 10.1016/j.mrfmmm.2015.05.004. [DOI] [PubMed] [Google Scholar]
- Krüger K, Mooren FC. Exercise-induced leukocyte apoptosis. Exercise Immunology Review. 2014;20:117–134. [PubMed] [Google Scholar]
- Lam WKJ, Gai W, Sun K, Wong RSM, Chan RWY, Jiang P, Chan NPH, Hui WWI, Chan AWH, Szeto C-C, Ng SC, Law M-F, Chan KCA, Chiu RWK, Lo YMD. DNA of Erythroid Origin is Present in Human Plasma and Informs the Types of Anemia. Clinical Chemistry. 2017;63:1614–1623. doi: 10.1373/clinchem.2017.272401. [DOI] [PubMed] [Google Scholar]
- Lastra G, Syed S, Kurukulasuriya LR, Manrique C, Sowers JR. Type 2 diabetes mellitus and hypertension: an update. Endocrinology and Metabolism Clinics of North America. 2014;43:103–122. doi: 10.1016/j.ecl.2013.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee YJ, Yoon K-A, Han J-Y, Kim HT, Yun T, Lee GK, Kim HY, Lee JS. Circulating cell-free DNA in plasma of never smokers with advanced lung adenocarcinoma receiving gefitinib or standard chemotherapy as first-line therapy. Clinical Cancer Research. 2011;17:5179–5187. doi: 10.1158/1078-0432.ccr-11-0400. [DOI] [PubMed] [Google Scholar]
- Li M, Jia Y, Xu J, Cheng X, Xu C. Assessment of the circulating cell-free DNA marker association with diagnosis and prognostic prediction in patients with lymphoma: a single-center experience. Annals of Hematology. 2017;96:1343–1351. doi: 10.1007/s00277-017-3043-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu YZ, Wang YX, Jiang CL. Inflammation: The Common Pathway of Stress-Related Diseases. Frontiers in Human Neuroscience. 2017;11:316. doi: 10.3389/fnhum.2017.00316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lui YYN, Chik KW, Chiu RWK, Ho CY, Lam CWK, Lo YMD. Predominant hematopoietic origin of cell-free DNA in plasma and serum after sex-mismatched bone marrow transplantation. Clinical Chemistry. 2002;48:421–427. [PubMed] [Google Scholar]
- Madsen AT, Hojbjerg JA, Sorensen BS, Winther-Larsen A. Day-to-day and within-day biological variation of cell-free DNA. EBioMedicine. 2019;49:284–290. doi: 10.1016/j.ebiom.2019.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margeli A, Skenderi K, Tsironi M, Hantzi E, Matalas A-L, Vrettou C, Kanavakis E, Chrousos G, Papassotiriou I. Dramatic elevations of interleukin-6 and acute-phase reactants in athletes participating in the ultradistance foot race spartathlon: severe systemic inflammation and lipid and lipoprotein changes in protracted exercise. The Journal of Clinical Endocrinology and Metabolism. 2005;90:3914–3918. doi: 10.1210/jc.2004-2346. [DOI] [PubMed] [Google Scholar]
- Mavropalias G, Calapre L, Morici M, Koeda T, Poon WCK, Barley OR, Gray E, Blazevich AJ, Nosaka K. Changes in plasma hydroxyproline and plasma cell-free DNA concentrations after higher- versus lower-intensity eccentric cycling. European Journal of Applied Physiology. 2021;121:1087–1097. doi: 10.1007/s00421-020-04593-1. [DOI] [PubMed] [Google Scholar]
- Maybin JA, Critchley HOD. Menstrual physiology: implications for endometrial pathology and beyond. Human Reproduction Update. 2015;21:748–761. doi: 10.1093/humupd/dmv038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCubbin JA, Helfer SG, Price TM. Blood pressure control and hormone replacement therapy in postmenopausal women at risk for coronary heart disease. American Heart Journal. 2002;143:711–717. doi: 10.1067/mhj.2002.121262. [DOI] [PubMed] [Google Scholar]
- Meddeb R, Dache ZAA, Thezenas S, Otandault A, Tanos R, Pastor B, Sanchez C, Azzi J, Tousch G, Azan S, Mollevi C, Adenis A, El Messaoudi S, Blache P, Thierry AR. Quantifying circulating cell-free DNA in humans. Scientific Reports. 2019;9:5220. doi: 10.1038/s41598-019-41593-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss J, Magenheim J, Neiman D, Zemmour H, Loyfer N, Korach A, Samet Y, Maoz M, Druid H, Arner P, Fu K-Y, Kiss E, Spalding KL, Landesberg G, Zick A, Grinshpun A, Shapiro AMJ, Grompe M, Wittenberg AD, Glaser B, Shemer R, Kaplan T, Dor Y. Comprehensive human cell-type methylation atlas reveals origins of circulating cell-free DNA in health and disease. Nature Communications. 2018;9:5068. doi: 10.1038/s41467-018-07466-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nédélec M, McCall A, Carling C, Legall F, Berthoin S, Dupont G. Recovery in soccer: part I - post-match fatigue and time course of recovery. Sports Medicine. 2012;42:997–1015. doi: 10.2165/11635270-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Nishimoto S, Fukuda D, Higashikuni Y, Tanaka K, Hirata Y, Murata C, Kim-Kaneyama J-R, Sato F, Bando M, Yagi S, Soeki T, Hayashi T, Imoto I, Sakaue H, Shimabukuro M, Sata M. Obesity-induced DNA released from adipocytes stimulates chronic adipose tissue inflammation and insulin resistance. Science Advances. 2016;2:e1501332. doi: 10.1126/sciadv.1501332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuttall FQ. Body Mass Index: Obesity, BMI, and Health: A Critical Review. Nutrition Today. 2015;50:117–128. doi: 10.1097/nt.0000000000000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohlsson L, Hall A, Lindahl H, Danielsson R, Gustafsson A, Lavant E, Ljunggren L. Increased level of circulating cell-free mitochondrial DNA due to a single bout of strenuous physical exercise. European Journal of Applied Physiology. 2020;120:897–905. doi: 10.1007/s00421-020-04330-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parent MÉ, El-Zein M, Rousseau MC, Pintos J, Siemiatycki J. Night Work and the Risk of Cancer Among Men. American Journal of Epidemiology. 2012;176:751–759. doi: 10.1093/aje/kws318. [DOI] [PubMed] [Google Scholar]
- Pfeifer GP, Denissenko MF, Olivier M, Tretyakova N, Hecht SS, Hainaut P. Tobacco smoke carcinogens, DNA damage and p53 mutations in smoking-associated cancers. Oncogene. 2002;21:7435–7451. doi: 10.1038/sj.onc.1205803. [DOI] [PubMed] [Google Scholar]
- Pritchett D, Reddy AB. Circadian Clocks in the Hematologic System. Journal of Biological Rhythms. 2015;30:374–388. doi: 10.1177/0748730415592729. [DOI] [PubMed] [Google Scholar]
- Rabinovich-Nikitin I, Lieberman B, Martino TA, Kirshenbaum LA. Circadian-Regulated Cell Death in Cardiovascular Diseases. Circulation. 2019;139:965–980. doi: 10.1161/CIRCULATIONAHA.118.036550. [DOI] [PubMed] [Google Scholar]
- Ranchoux B, Meloche J, Paulin R, Boucherat O, Provencher S, Bonnet S. DNA Damage and Pulmonary Hypertension. Ternational Journal of Molecular Sciences. 2016;17:E990. doi: 10.3390/ijms17060990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratna A, Mandrekar P. Alcohol and Cancer: Mechanisms and Therapies. Biomolecules. 2017;7:E61. doi: 10.3390/biom7030061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silver R, Schwartz WJ. In: Methods in Enzymology. Young MW, editor. Academic Press; 2005. The Suprachiasmatic Nucleus is a Functionally Heterogeneous Timekeeping Organ; pp. 451–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder MW, Kircher M, Hill AJ, Daza RM, Shendure J. Cell-free DNA Comprises an In Vivo Nucleosome Footprint that Informs Its Tissues-Of-Origin. Cell. 2016;164:57–68. doi: 10.1016/j.cell.2015.11.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sozzi G, Conte D, Mariani L, Lo Vullo S, Roz L, Lombardo C, Pierotti MA, Tavecchio L. Analysis of Circulating Tumor DNA in Plasma at Diagnosis and during Follow-Up of Lung Cancer Patients. Cancer Research. 2001;61:4675–4678. [PubMed] [Google Scholar]
- Sozzi G, Conte D, Leon M, Ciricione R, Roz L, Ratcliffe C, Roz E, Cirenei N, Bellomi M, Pelosi G, Pierotti MA, Pastorino U. Quantification of free circulating DNA as a diagnostic marker in lung cancer. Journal of Clinical Oncology. 2003;21:3902–3908. doi: 10.1200/jco.2003.02.006. [DOI] [PubMed] [Google Scholar]
- Spindler K-LG, Appelt AL, Pallisgaard N, Andersen RF, Brandslund I, Jakobsen A. Cell-free DNA in healthy individuals, noncancerous disease and strong prognostic value in colorectal cancer. Ternational Journal of Cancer. 2014;135:2984–2991. doi: 10.1002/ijc.28946. [DOI] [PubMed] [Google Scholar]
- Spindler KLG, Pallisgaard N, Andersen RF, Brandslund I, Jakobsen A. Circulating free DNA as biomarker and source for mutation detection in metastatic colorectal cancer. PLOS ONE. 2015;10:e0108247. doi: 10.1371/journal.pone.0108247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spisák S, Solymosi N, Ittzés P, Bodor A, Kondor D, Vattay G, Barták BK, Sipos F, Galamb O, Tulassay Z, Szállási Z, Rasmussen S, Sicheritz-Ponten T, Brunak S, Molnár B, Csabai I. Complete Genes May Pass from Food to Human Blood. PLOS ONE. 2013;8:e69805. doi: 10.1371/journal.pone.0069805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stawski R, Walczak K, Kosielski P, Meissner P, Budlewski T, Padula G, Nowak D. Repeated bouts of exhaustive exercise increase circulating cell free nuclear and mitochondrial DNA without development of tolerance in healthy men. PLOS ONE. 2017;12:e0178216. doi: 10.1371/journal.pone.0178216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan E, Harris RA, Pfefferbaum A. Alcohol’s effects on brain and behavior. Alcohol Research & Health. 2010;33:127–143. [PMC free article] [PubMed] [Google Scholar]
- Sun K, Jiang P, Chan KCA, Wong J, Cheng YKY, Liang RHS, Chan W, Ma ESK, Chan SL, Cheng SH, Chan RWY, Tong YK, Ng SSM, Wong RSM, Hui DSC, Leung TN, Leung TY, Lai PBS, Chiu RWK, Lo YMD. Plasma DNA tissue mapping by genome-wide methylation sequencing for noninvasive prenatal, cancer, and transplantation assessments. PNAS. 2015;112:E5503–E5512. doi: 10.1073/pnas.1508736112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun K, Jiang P, Cheng SH, Cheng THT, Wong J, Wong VWS, Ng SSM, Ma BBY, Leung TY, Chan SL, Mok TSK, Lai PBS, Chan HLY, Sun H, Chan KCA, Chiu RWK, Lo YMD. Orientation-aware plasma cell-free DNA fragmentation analysis in open chromatin regions informs tissue of origin. Genome Research. 2019;29:418–427. doi: 10.1101/gr.242719.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabibzadeh S. The signals and molecular pathways involved in human menstruation, a unique process of tissue destruction and remodelling. Molecular Human Reproduction. 1996;2:77–92. doi: 10.1093/molehr/2.2.77. [DOI] [PubMed] [Google Scholar]
- Tamkovich SN, Bryzgunova OE, Rykova EY, Permyakova VI, Vlassov VV, Laktionov PP. Circulating nucleic acids in blood of healthy male and female donors. Clinical Chemistry. 2005;51:1317–1319. doi: 10.1373/clinchem.2004.045062. [DOI] [PubMed] [Google Scholar]
- Teo YV, Capri M, Morsiani C, Pizza G, Faria AMC, Franceschi C, Neretti N. Cell-free DNA as a biomarker of aging. Aging Cell. 2019;18:e12890. doi: 10.1111/acel.12890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thierry AR, El Messaoudi S, Gahan PB, Anker P, Stroun M. Origins, structures, and functions of circulating DNA in oncology. Cancer Metastasis Reviews. 2016;35:347–376. doi: 10.1007/s10555-016-9629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpe R, Sunderland C. Muscle damage, endocrine, and immune marker response to a soccer match. Journal of Strength and Conditioning Research. 2012;26:2783–2790. doi: 10.1519/JSC.0b013e318241e174. [DOI] [PubMed] [Google Scholar]
- Tosevska A, Franzke B, Hofmann M, Vierheilig I, Schober-Halper B, Oesen S, Neubauer O, Wessner B, Wagner K-H. Circulating cell-free DNA, telomere length and bilirubin in the Vienna Active Ageing Study: exploratory analysis of a randomized, controlled trial. Scientific Reports. 2016;6:38084. doi: 10.1038/srep38084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tóth K, Patai ÁV, Kalmár A, Barták BK, Nagy ZB, Galamb O, Wichmann B, Tulassay Z, Molnár B. Circadian Rhythm of Methylated Septin 9, Cell-Free DNA Amount and Tumor Markers in Colorectal Cancer Patients. Pathology Oncology Research. 2017;23:699–706. doi: 10.1007/s12253-016-0174-2. [DOI] [PubMed] [Google Scholar]
- Trigg RM, Martinson LJ, Parpart-Li S, Shaw JA. Factors that influence quality and yield of circulating-free DNA: A systematic review of the methodology literature. Heliyon. 2018;4:e00699. doi: 10.1016/j.heliyon.2018.e00699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuda H, Ito YM, Todo Y, Iba T, Tasaka K, Sutou Y, Hirai K, Dozono K, Dobashi Y, Manabe M, Sakamoto T, Yamamoto R, Ueda K, Akatsuka M, Kiyozuka Y, Nagai N, Imai M, Kobiki K, Fujita H, Itamochi H, Oshita T, Kawarada T, Hatae M, Yokoyama Y. Measurement of endometrial thickness in premenopausal women in office gynecology. Reproductive Medicine and Biology. 2018;17:29–35. doi: 10.1002/rmb2.12062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tug S, Helmig S, Deichmann ER, Schmeier-Jürchott A, Wagner E, Zimmermann T, Radsak M, Giacca M, Simon P. Exercise-induced increases in cell free DNA in human plasma originate predominantly from cells of the haematopoietic lineage. Exercise Immunology Review. 2015;21:164–173. [PubMed] [Google Scholar]
- Tug S, Mehdorn M, Helmig S, Breitbach S, Ehlert T, Simon P. Exploring the Potential of Cell-Free-DNA Measurements After an Exhaustive Cycle-Ergometer Test as a Marker for Performance-Related Parameters. Ternational Journal of Sports Physiology and Performance. 2017a;12:597–604. doi: 10.1123/ijspp.2016-0157. [DOI] [PubMed] [Google Scholar]
- Tug S, Tross A-K, Hegen P, Neuberger EWI, Helmig S, Schöllhorn W, Simon P. Acute effects of strength exercises and effects of regular strength training on cell free DNA concentrations in blood plasma. PLOS ONE. 2017b;12:e0184668. doi: 10.1371/journal.pone.0184668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Drift MA, Hol BEA, Klaassen CHW, Prinsen CFM, van Aarssen YAWG, Donders R, van der Stappen JWJ, Dekhuijzen PNR, van der Heijden HFM, Thunnissen FBJM. Circulating DNA is a non-invasive prognostic factor for survival in non-small cell lung cancer. Lung Cancer. 2010;68:283–287. doi: 10.1016/j.lungcan.2009.06.021. [DOI] [PubMed] [Google Scholar]
- Vittori LN, Tarozzi A, Latessa PM. In: Cell-Free DNA as Diagnostic Markers: Methods and Protocols. Casadio V, Salvi S, editors. New York, NY: Springer; 2019. Circulating Cell-Free DNA in Physical Activities; pp. 183–197. [DOI] [PubMed] [Google Scholar]
- Wagner JT, Kim HJ, Johnson-Camacho KC, Kelley T, Newell LF, Spellman PT, Ngo TTM. Diurnal stability of cell-free DNA and cell-free RNA in human plasma samples. Scientific Reports. 2020;10:16456. doi: 10.1038/s41598-020-73350-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F, Li C, Chen L. The Circadian Gene Clock Plays an Important Role in Cell Apoptosis and the DNA Damage Response In Vitro. Technology in Cancer Research & Treatment. 2015;15:480–486. doi: 10.1177/1533034615585433. [DOI] [PubMed] [Google Scholar]
- Warton K, Lin V, Navin T, Armstrong NJ, Kaplan W, Ying K, Gloss B, Mangs H, Nair SS, Hacker NF, Sutherland RL, Clark SJ, Samimi G. Methylation-capture and Next-Generation Sequencing of free circulating DNA from human plasma. BMC Genomics. 2014;15:476. doi: 10.1186/1471-2164-15-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warton K, Graham LJ, Yuwono N, Samimi G. Comparison of 4 commercial kits for the extraction of circulating DNA from plasma. Cancer Genetics. 2018;228–229:143–150. doi: 10.1016/j.cancergen.2018.02.004. [DOI] [PubMed] [Google Scholar]
- Wendeu-Foyet MG, Bayon V, Cénée S, Trétarre B, Rébillard X, Cancel-Tassin G, Cussenot O, Lamy P-J, Faraut B, Ben Khedher S, Léger D, Menegaux F. Night work and prostate cancer risk: results from the EPICAP Study. Occupational and Environmental Medicine. 2018;75:573–581. doi: 10.1136/oemed-2018-105009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weng M-W, Lee H-W, Park S-H, Hu Y, Wang H-T, Chen L-C, Rom WN, Huang WC, Lepor H, Wu X-R, Yang CS, Tang M-S. Aldehydes are the predominant forces inducing DNA damage and inhibiting DNA repair in tobacco smoke carcinogenesis. PNAS. 2018;115:E6152–E6161. doi: 10.1073/pnas.1804869115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong FCK, Sun K, Jiang P, Cheng YKY, Chan KCA, Leung TY, Chiu RWK, Lo YMD. Cell-free DNA in maternal plasma and serum: A comparison of quantity, quality and tissue origin using genomic and epigenomic approaches. Clinical Biochemistry. 2016;49:1379–1386. doi: 10.1016/j.clinbiochem.2016.09.009. [DOI] [PubMed] [Google Scholar]
- Wu J, Tang W, Huang L, Hou N, Wu J, Cheng X, Ma D, Qian P, Shen Q, Guo W, Peng W, Liu Y, Jiang C, Feng J. The analysis of cell-free DNA concentrations and integrity in serum of initial and treated of lymphoma patients. Clinical Biochemistry. 2019;63:59–65. doi: 10.1016/j.clinbiochem.2018.10.002. [DOI] [PubMed] [Google Scholar]
- Yan L, Chen Y, Zhou J, Zhao H, Zhang H, Wang G. Diagnostic value of circulating cell-free DNA levels for hepatocellular carcinoma. International Journal of Infectious Diseases. 2018;67:92–97. doi: 10.1016/j.ijid.2017.12.002. [DOI] [PubMed] [Google Scholar]
- Yoon KA, Park S, Lee SH, Kim JH, Lee JS. Comparison of circulating plasma DNA levels between lung cancer patients and healthy controls. The Journal of Molecular Diagnostics. 2009;11:182–185. doi: 10.2353/jmoldx.2009.080098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuwono NL, Henry CE, Ford CE, Warton K. Total and endothelial cell-derived cell-free DNA in blood plasma does not change during menstruation. PLOS ONE. 2021;16:e0250561. doi: 10.1371/journal.pone.0250561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao H, Albino AP, Jorgensen E, Traganos F, Darzynkiewicz Z. DNA damage response induced by tobacco smoke in normal human bronchial epithelial and A549 pulmonary adenocarcinoma cells assessed by laser scanning cytometry. Cytometry. Part A. 2009;75:840–847. doi: 10.1002/cyto.a.20778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng YWL, Chan KCA, Sun H, Jiang P, Su X, Chen EZ, Lun FMF, Hung ECW, Lee V, Wong J, Lai PBS, Li C-K, Chiu RWK, Lo YMD. Nonhematopoietically derived DNA is shorter than hematopoietically derived DNA in plasma: a transplantation model. Clinical Chemistry. 2012;58:549–558. doi: 10.1373/clinchem.2011.169318. [DOI] [PubMed] [Google Scholar]
- Zhong XY, Hahn S, Kiefer V, Holzgreve W. Is the quantity of circulatory cell-free DNA in human plasma and serum samples associated with gender, age and frequency of blood donations? Annals of Hematology. 2007;86:139–143. doi: 10.1007/s00277-006-0182-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.