Abstract
Purpose
The purpose of this study is to evaluate the short-term results of lateral closing wedge osteotomy with medial hemiplateau elevation for the management of severe infantile Blount's disease.
Materials and methods
In this prospective study, 11 cases of severe Blount's disease (Langenskiold stages five and six) were managed in the period between January 2017 and January 2020. Double osteotomy technique was applied, namely a metaphyseal closing wedge and a medial hemiplateau elevation, through a single midline incision. Fixation was achieved by a medial anatomical locked plate. Patients were evaluated clinically according to a modified version of paediatric outcomes data collection Instrument (PODCI) and radiologically by measuring the angle between the tibial and the femoral shaft, the mechanical axis deviation (MAD) and the angle of the medial tibial plateau (MTP) depression.
Results
The average follow-up period was 2 years. Healing of the osteotomies was achieved in all cases after the index operation within an average of 3 months. Based on our modification of the PODCI score, five cases had an excellent outcome, five were good, and one case ended with a fair outcome. No major complications were encountered in this study.
Conclusion
The management of severe Blount's disease by acute correction using the aforementioned technique has been proven to achieve acceptable clinical and radiological outcomes without significant complications.
Level of evidence
Level IV case series study.
How to cite this article
Nada AA, Hammad ME, Eltanahy AF, et al. Acute Correction and Plate Fixation for the Management of Severe Infantile Blount's Disease: Short-term Results. Strategies Trauma Limb Reconstr 2021;16(2):78–85.
Keywords: Blount's disease, Closing wedge osteotomy, Double osteotomy, Hemiplateau elevation, Tibia vara
Introduction
Blount's disease represents a pathological angular deformity of the upper tibial epiphysis as a result of disordered endochondral ossification, which leads to a complex three-dimensional deformity; varus, procurvatum and internal tibial torsion.1,2
Blount's disease may occur at an early onset (<3 years) or late-onset tibia vara, which includes juvenile group (4–10 years) and adolescent group (11 years and older), with no history of trauma, infection or other known causes for physeal arrest. Recurrence after treatment is not uncommon, and the incidence can reach up to 50%. Recurrence results in a more complex condition as it involves elements of the original deformity and those resulting from previous surgeries.2–4
Patients with Blount's disease usually present with an asymptomatic deformity, frequently with an evident lateral thrust. In symptomatic patients, medial or anteromedial knee pain is usually encountered, particularly with exercise. Tenderness may coexist.3,5
In Blount's patients, according to Hueter-Volkmann principal, excessive loading on the medial part of the proximal tibial physis causes mechanical growth retardation, especially in obese children, which aggravates the varus deformity.2 Thus, theoretically, mechanical realignment with osteotomy unloads the suppressed physis and corrects the mechanical problem. However, significant depression of medial plateau in severe cases would also require medial plateau elevation for the correction of the existing knee joint incongruity.2,3
Many options are proposed for surgical management, including hemiepiphysiodesis, tibial osteotomy and correction using internal fixation by plates or stables or external fixation using Ilizarov or Taylor spatial frame (TSF), allowing acute or gradual controlled correction.2,3,5
The concept of double osteotomy, including medial hemiplateau elevation in severe cases, has been studied and modified since its first proposition.6 Most authors use graft to support the hemiplateau elevation and then fixation using K-wires and cast, Ilizarov frame, or plates. The procedure may be performed in single or in a staged surgery.7
Materials and Methods
This prospective study included 11 out of 20 cases of severe Blount's disease (stages V and VI), who have a true limb length discrepancy (LLD) less than 4 cm, with ipsilateral knee joint laxity. All patients with severe Blount's disease (Langenskiold stages V and VI) treated between 20XX and 20XX were screened for inclusion in this study. Exclusion criteria were patients with no joint laxity and those with a true LLD of more than 4 cm. Of the 20 potential cases, 9 were excluded, leaving 11 eligible patients.
The parents of all included cases reported the presence of bilateral or unilateral knee deformity before the age of 3 years, which, in addition to the severity of the presenting deformity, was strongly suggestive that such cases were infantile Blount's disease. Of the 11 cases included, 7 were stage V and 4 were stage VI (according to Langenskiold and Riska classification)8 at the time of presentation. Cases were managed and followed up in the period from January 2017 to January 2020, with a minimum follow-up period of 18 months, as an inclusion criterion.
The age of the patients ranged from 11.5 to 15 years (average, 13.5 years). There were six males and five females (Table 1).
Table 1.
Distribution of the studied cases according to different parameters (n = 11)
| Number (%) | |
|---|---|
| Age at the time of presentation (years) | |
| Mean ± SD | 13.5 ± 1.1 |
| Median (min.–max.) | 13.8 (11.4–15) |
| Sex | |
| Male | 6 (54.5) |
| Female | 5 (45.5) |
| Presentation | |
| First | 5 (45.5) |
| Recurrent | 6 (54.5) |
| Side | |
| Right | 5 (45.5) |
| Left | 6 (54.5) |
| Stage | |
| IV | 4 (36.4) |
| V | 7 (63.6) |
| Follow-up (years) | |
| Mean ± SD | 2.2 ± 0.5 |
| Median (min.–max.) | 2 (1.5–3) |
Five of the included cases did not receive any previous surgical treatment, while the other six cases were recurrent. The first surgery in the recurrent group was an osteotomy and fixation either by K-wires or plates. The average time from the first surgery to presentation was 5.5 years (range from 4 to 6 years).
Preoperatively, all children complained of knee pain, varus deformity and a varus thrust during walking. Patients were evaluated clinically, according to a modified version of an adolescent paediatric outcomes data collection (PODCI)9 (Table 2). In our modification, we focused on the questions that are related to the lower limb function, appearance, satisfaction and pain. Questions related to the upper limb function, and those lacking applicability to the targeted population, were excluded from the original PODCI score. For each question, the patient is asked to select the most accurate response from four options, ranging from “excellent” to “poor.” The average preoperative modified PODCI score was 51.
Table 2.
Modified PODCI score
| Item | Very happy | Somewhat happy | Not sure | Somewhat unhappy | Very unhappy | |
|---|---|---|---|---|---|---|
| 1 | How happy is the child with how he/she looks? | 1 | 2 | 3 | 4 | 5 |
| 2 | How happy is the child with clothes his/her can wear? | 1 | 2 | 3 | 4 | 5 |
| 3 | How happy is the child with his/her ability to do the same things his/her friends do? | 1 | 2 | 3 | 4 | 5 |
| 4 | How happy is the child with his/her health in general? | 1 | 2 | 3 | 4 | 5 |
| Easy | A little hard | Very hard | Cannot do at all | |||
| 5 | Can the child stand while washing his/her hand and face at the sink? | 1 | 2 | 3 | 4 | |
| 6 | Can the child sit in a regular chair without holding on? | 1 | 2 | 3 | 4 | |
| 7 | Can the child get in and out the toilet? | 1 | 2 | 3 | 4 | |
| 8 | Can the child get on and off the bus? | 1 | 2 | 3 | 4 | |
| 9 | Can the child bend over from standing position and pick up something off the floor? | 1 | 2 | 3 | 4 | |
| 10 | Can the child walk the required distance? | 1 | 2 | 3 | 4 | |
| 11 | Can the child run short distance? | 1 | 2 | 3 | 4 | |
| 12 | Can the child use the bicycle or tricycle? | 1 | 2 | 3 | 4 | |
| 13 | Can the child climb three flights of stairs? | 1 | 2 | 3 | 4 | |
| 14 | Can the child participate in competitive level sports with other children the same age? | 1 | 2 | 3 | 4 | |
| 15 | How much pain has your child had during the last week? | None 1 | Very Mild 2 | Mild 3 | Moderate 4 | Severe 5 |
| 16 | During the last week, how much did pain interfere with your child's normal activities (at home, outside and school)? | Never 1 | Sometimes 2 | Half the time 3 | Often 4 | Extremely 5 |
| 17 | How often does your child need help from another person for sitting and standing? | Never 1 | Sometimes 2 | Half the time 3 | Often 4 | All the time 5 |
| 18 | How often does his/her need help from another person walking or climbing? | Never 1 | Sometimes 2 | Half the time 3 | Often 4 | All the time 5 |
| 19 | How would you feel if your child had to spend the rest of his/her life with his/her bone and muscle condition as it is right now? | Very satisfied 1 | Somewhat satisfied 2 | Neutral 3 | Somewhat dissatisfied 4 | Very dissatisfied 5 |
Score range: Best score, 19; Worst score, 85; Excellent, 19–36; Good, 37–52; Fair, 53–69; Poor, 70–85
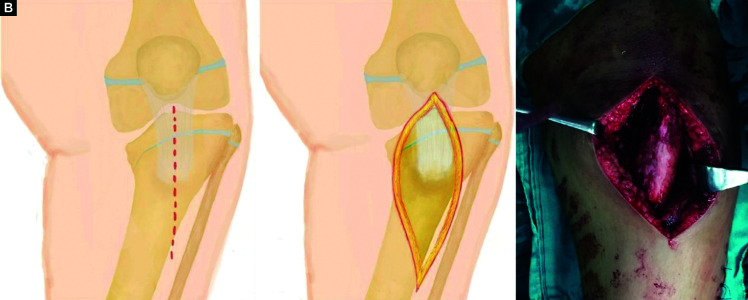
Radiological evaluation was based on standing anteroposterior (AP) and lateral views of both lower limbs, with the patella facing forward, and was obtained preoperatively. The angle between the tibial and the femoral shaft, the mechanical axis deviation (MAD) and the angle of the medial tibial plateau (MTP) depression were measured and recorded (Fig. 1). Computed tomography scans were obtained in all cases to confirm the stage of the disease, the presence of the physeal bar and for preoperative planning.
Fig. 1.
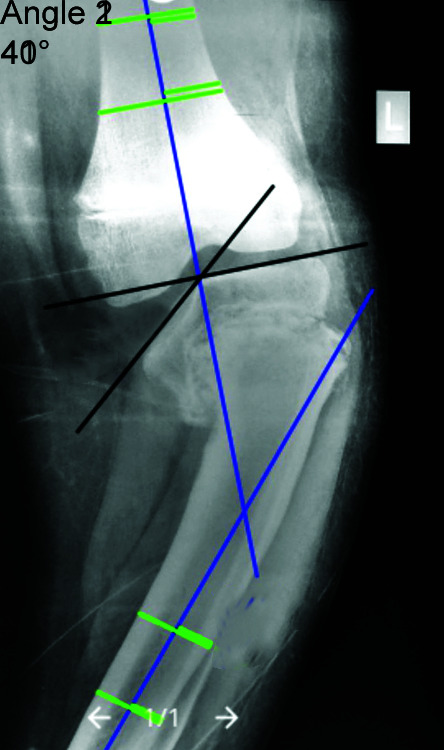
Preoperative measurement of the angle between the tibial and the femoral shaft (angle 1), and the angle of the MTP depression (angle 2)
A broad-spectrum antibiotic was given perioperatively. The patient was positioned supine on a standard radiolucent orthopaedic table. The image intensifier is placed on the opposite side and rotated for AP and lateral views.
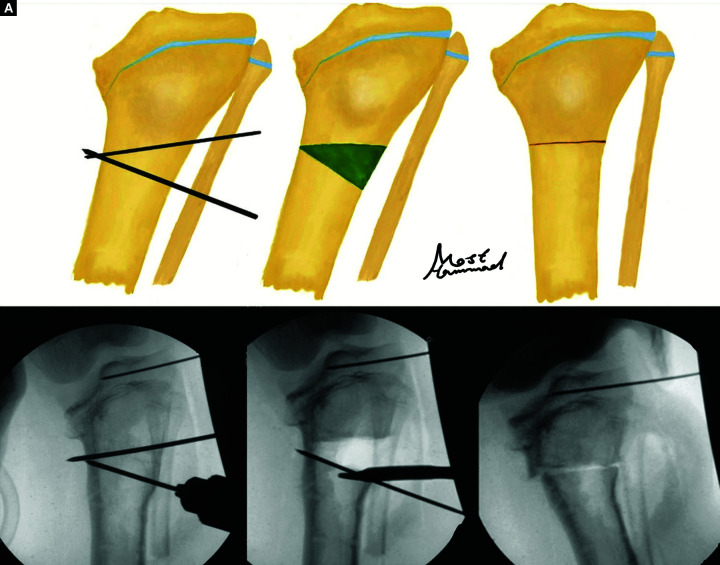
Through a lateral incision, a mid-fibular osteotomy, with excision of 2 to 3 cm of the fibula, was performed. Two tibial osteotomies were performed; one for the medial plateau elevation combined with the insertion of the bone graft and one for the correction of tibial deformity, both through a single midline incision (Fig. 2).
Figs 2A to C.
A single midline incision is used to perform both tibial osteotomies
Two K-wires were inserted to plan the lateral proximal tibial closing wedge osteotomy, as planned preoperatively. This wedge-shaped osteotomy was performed about 5 cm distal to the joint line, below the tibial tuberosity (Fig. 3). A bony wedge was removed for the correction of the varus deformity. The internal tibial torsion was addressed and corrected with this step. The degree of correction of the torsion was determined mainly clinically. Preliminary fixation by K-wires was done.
Figs 3A and B.
Lateral closing wedge osteotomy was performed about 5 cm distal to the joint line, below the tibial tuberosity, to correct the metaphyseal component of the deformity
Another two K-wires were inserted parallel to the medial plateau, starting from just below the beak of the depressed plateau, to guide the second osteotomy. Another wire was inserted from anterior to posterior parallel to the upper tibial slope, to guide the correction of the posterior slope simultaneously.
Two K-wires were inserted from lateral to medial, reaching past the intercondylar point where the planned medial osteotomy would stop, and this prevented the extension of the medial elevating osteotomy to the articular surface (Fig. 4A). Another method was to drill a small hole in the intercondylar area to prevent inadvertent extension of the medial elevation osteotomy to the joint surface (a stopper), and this method was used in four cases.
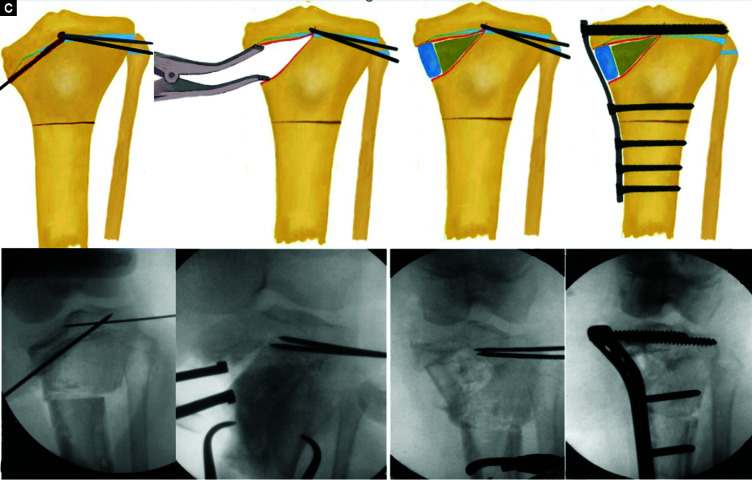
Figs 4A to D.
Steps of performing the medial hemiplateau elevation osteotomy, bone graft insertion and fixation
A wide chisel, guided by two K-wires, was used to target the intercondylar area without crossing the articular cartilage; then, the osteotomy site was opened using a lamina spreader (Fig. 4B). The knee was kept in flexion for minimising the risk of neurovascular damage. Subsequently, the bony wedge from the first tibial osteotomy was inserted deeply at the osteotomy site, and the fibular bony part was inserted peripherally to support the new position and maintain the correction (Fig. 4C).
An anatomically contoured proximal tibia locking plate was applied, and at least two screws were inserted into the epiphysis and at least three bicortical screws distal to the tibial osteotomy (Fig. 4D). The cable test using a diathermy cable was used to assess the mechanical axis correction in all cases before the closure.9
The surgical wounds were closed in layers, and care was taken to avoid the tight closure of the fascia to prevent compartment syndrome. A long leg cast (plaster of paris) was applied for 2 weeks. Plain supine AP and lateral X-rays were obtained on the next day after surgery.
The rehabilitation protocol consisted of mobilising the patients in a hinged, non-weight-bearing knee brace after cast removal and wound healing. Strengthening exercises for the quadriceps and hamstrings were performed. The brace was removed after 6 weeks and partially assisted weight–bearing was allowed as tolerated. Full weight-bearing was initiated after 10–12 weeks, when signs of the radiological union were obtained (Figs 5 and 6).
Figs 5A to C.

(A) Preoperative standing clinical photograph of both lower limbs; the left side shows an evident varus deformity; (B) Postoperative correction of the deformity is evident clinically; (C) Good flexion range of the operated side is maintained
Figs 6A and B.

Pre- and postoperative standing X-ray scanogram of both lower limbs showing correction of the mechanical axis; also there is a partial compensation of the LLD after the surgery due to the correction of the deformity
During the follow-up visits, standing AP and lateral view of both lower limbs, with the patella facing forward, were requested, every 6 months and at the last follow-up. The radiographic angles were measured and recorded. At the 18-month follow-up visit, functional re-evaluation of the patients was done using the modified PODCI score.
The obtained clinical and radiological data were and analysed using IBM SPSS software package version 20.0. (Armonk, New York: IBM Corp). The Kolmogorov-Smirnov test was used to verify the normality of the distribution of variables. Comparisons between groups for categorical variables were assessed using paired t-test, and it was assessed for the comparison between different periods for normally distributed quantitative variables. Mann-Whitney test was used to compare between two groups for not normally distributed quantitative variables. Spearman's coefficient was used to correlate between quantitative variables. The significance of the obtained results was judged at the 5% level.
Results
Out of 20 potentially eligible patients, 11 cases fulfilled the inclusion criteria and were included, and 9 patients were excluded; 6 of them were excluded due to the presence of true LLD more than 4 cm, and 3 had no ipsilateral knee joint laxity. All the 11 included patients were followed up for at least 18 months and thus were eligible for the analysis. The follow-up period ranged from 1.5 to 3 years, with an average of 2 years. The age of the analysed patients ranged from 11.5 to 15 years, with a mean age of 13.8 years. There were six males and five females.
According to the modified PODCI score, five cases were graded excellent, five were good, and one case had a fair outcome. Cosmetic appearance, comfort, stability during long-distance walking and short-distance running were the main improvements that impacted patients’ satisfaction. The mean postoperative modified PODCI score was 38.8 ± 10.7. There was a significant improvement compared to the preoperative score (p <0.001).
Six of the included cases underwent previous corrective surgeries; however, this had no statistically significant influence on the final functional outcome (modified PODCI score), as compared to the cases who had no previous ipsilateral corrective surgeries. LLD was >1.5 cm in all cases preoperatively (ranging from 1.7 to 3 cm). The corrective osteotomy added a true length to the affected limb that ranged from 1 to 1.8 cm (mean, 1.3 ± 0.3), with all cases having less than 1.4 cm LLD postoperatively (mean, 0.9 ± 0.3).
Based on Langenskiold classification, seven were stage V and four were stage VI. The MTP depression angle ranged from 30° to 55° with a mean of 40.9° ± 8° preoperatively. Postoperatively, the mean was 6° ± 5.6° (ranging from 0° to 18°). Both Langenskiold stage and MTP angle had no statistically significant influence on the final functional outcome.
The preoperative tibiofemoral angle ranged from 28° to 44° with a mean of 36.6° ± 5.1°. Our aim was to correct to a neutral or to a slight valgus angle; 0° degree was attained in two cases; valgus in five cases (ranging from −3° to −10°), while residual varus was present in four cases (up to 8°), and this variation in the postoperative tibiofemoral angle (−10° to +8°) did not have a significant influence on the functional outcome.
Preoperative MAD ranged from 44 to 72 mm (with an average of 56.8 mm and a standard deviation of 9.9 mm). Postoperative MAD ranged from −8° to +7°. Both pre- and postoperative MAD did not have a statistically significant impact on the final functional outcome (Table 3).
Table 3.
Comparison between the pre- and postoperative measurements (n = 11)
| Preoperative | Postoperative | p-value | |
|---|---|---|---|
| LLD (cm) | |||
| Mean ± SD | 2.2 ± 0.4 | 0.9 ± 0.3 | <0.001* |
| Decrease (95% CI) | 1.3 ± 0.2 | ||
| Tibiofemoral angle | |||
| Mean ± SD | 36.6 ± 5.1 | −0.5 ± 6.2 | <0.001* |
| Decrease (95% CI) | 37.2 ± 5 | ||
| MAD | |||
| Mean ± SD | 56.8 ± 9.9 | −1.2 ± 5.3 | <0.001* |
| Decrease (95% CI) | 58 ± 9 | ||
| Depression angle | |||
| Mean ± SD | 40.9 ± 8 | 6 ± 5.6 | <0.001* |
| Decrease (95% CI) | 34.9 ± 8.2 | ||
| Modified PODCI score | |||
| Mean ± SD | 50.6 ± 9.7 | 38.8 ± 10.7 | <0.001* |
| Decrease (95% CI) | 11.8 ± 2.1 | ||
LLD, limb length discrepancy; PODCI, paediatric outcomes data collection instrument; p, p value for comparing between pre and post;
statistically significant at p ≤0.05; CI, confidence interval
Both osteotomies healed completely at an average of 3 months postoperatively in all patients. Range of knee motion was maintained as all patients were able to achieve full extension and flexion. Two cases had erythema at wound edges observed within the first week postoperatively; however, both cases healed uneventfully after a short course of broad-spectrum antibiotics and repeated dressings.
Discussion
Management of severe Blount's disease is usually complex. Correction is needed to prevent further increase in varus deformity and early development of osteoarthritis, also to correct the gait abnormality.7,11,12 Correction of such cases using only valgus osteotomy results in a high rate of recurrence and the need for reoperation. Additional elevation of the medial plateau to correct the joint incongruity is an essential step in severe cases with increased medial plateau obliquity, to reach the aim of a joint line that is parallel to the ground, preferably in one setting.6,13,14
Based on the modified PODCI score, out of 11 cases, 5 cases achieved excellent results, good outcome was obtained in 5 cases, and 1 case showed a fair result (satisfactory results in 90.9%).
Cosmetic appearance, comfort and stability during long-distance walks and short-distance running seemed to be the main improvements that impacted patients’ satisfaction, conforming with the findings of Gkiokas and Brilakis,2 who reported satisfactory results in all their patients. Abraham et al.15 had 18 out of the 19 patients subjected to a similar questionnaire, in which they achieved satisfactory results. Both used a similar technique of single-stage double osteotomy with hemiplateau elevation.
Lateral closing wedge osteotomy caused additional limb shortening; however, such shortening was not a concern, as none of the included cases required additional lengthening in a second stage. This could be explained by the fact that part of the LLD was caused by the deformity, which was eventually corrected. Furthermore, most of the included patients were approaching skeletal maturity. However, cases who had marked LLD (more than 4 cm) would require Ilizarov lengthening and thus were excluded from this study. Gkiokas and Brilakis2 used a similar technique on eight cases and reported that only one case needed a second-stage lengthening and stated that a 3-cm discrepancy in this case was existent preoperatively.
Several advantages were gained using closing wedge osteotomy, as it does not require iliac crest bone graft in contrast to opening wedge5 and provides a strong bony block to support the medial plateau elevation securely, as originally described by Gregosiewicz et al.6 An iliac bone graft was used by Gkiokas and Brilakis2 and Abraham et al.;14 however, this was not needed in any of the studied cases. Another advantage of closing wedge osteotomy is being relatively simple, compared to dome, oblique or bamboo osteotomy, which are more technically demanding.15–17 In addition, it has a reduced risk of non-union compared to opening wedge and allows an earlier range of motion.18,19
In general, gradual correction with Ilizarov or TSF has yielded good results for the management of severe Blount's disease. Using circular frames allowed for early weight-bearing and accurate deformity correction by frame adjustment later after surgery.20–22 However, several drawbacks have been observed. Jones et al.4 reported a period of 4 months till the removal of the fixator in cases who did not require lengthening and up to 8 months in cases who required lengthening. Also, a period of 5.5 months till removal of the frame was reported by Fitoussi et al.7 Thus, considering the added burden of the daily care of the fixator, the high risk of pin tract infection and the complexity of the construct, the option of internal fixation and acute correction in one sitting seems to be more appealing.2,22–24
Some authors report that concomitant epiphysiodesis of the lateral part of the proximal tibial physis should be performed to avoid recurrence of the deformity.8,25,26 In the current study, long screws were advanced through the plate, crossing from the medial to the lateral part of the proximal tibial epiphysis. Theoretically, they tether the physis, producing the epiphysiodesis effect, for both medial and lateral parts of the physis, which is needed to prevent the recurrence of the deformity. However, the exact effect cannot be accurately estimated, as the included patients were adolescents, and the anticipated remaining growth in most of the included cases might not be enough to confirm such effects.
In this study, one K-wire was inserted from anterior to posterior parallel to the posterior tibial slope of the MTP; it was used to guide the slope correction, which was done by elevating the plateau more posteriorly than anteriorly. Jones et al.4 commented on the importance of correcting the posterior tibial slope, stating that varus thrust was seen in patients whose posterior slope was excessive.
In this series, the mean preoperative value of MTP depression angle was 40.9°, ranging from 30° to 55°. According to Schoenecker et al.,26 MTP depression should be corrected when the slope exceeds 30°.
In all studied cases in this series, there was a significant joint laxity, which is also an ideal indication for MTP elevation. If there is no laxity, it can be due to relative joint congruence, hindering MTP elevation, as its elevation in this case can increase the pressure on the joint cartilage.
In this study, a neutral mechanical axis correction was the aim, because the risk of recurrence was not high, as all the included patients were adolescents. Overcorrection to about 10° is recommended by many authors.6,27 However, some advocate normalization of the mechanical axis.8 Considering that most of the patients are obese, overcorrection can result in poor cosmetic appearance and an awkward gait. In general, there is no consensus in the literature regarding the ideal alignment of the lower extremity.
The study has some limitations, as it includes a relatively small series of cases. However, this corresponds to those in the literature, as such severe cases are uncommon. The relatively short–term follow-up is another limitation of this study, as longer follow-up is required to evaluate some possible complications, such as recurrence, MTP re-depression and cartilage degeneration. Also, the intraoperative cable to test that was used to assess the correction intraoperatively is not a very accurate method.28,29 In addition, the modified score that was used for functional evaluation in this study is not validated. The reliability, relevance and responsiveness of the adopted modified score for paediatric lower limb function need to be evaluated on a larger scale in future studies.
Conclusion
Based on the final clinical and radiographic outcomes of this study, it is concluded that severe degrees of infantile Blount's disease can be safely managed by acute correction using a single–stage double osteotomy with an elevation of the medial hemiplateau. This single-stage double osteotomy technique has been shown to be successful for this sample of patients and yielded acceptable clinical and radiological outcomes, without significant major complications. Furthermore, it required a relatively short postoperative rehabilitation period.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments.
Consent
A written, informed consent was obtained from all the patients authorising the treatment, radiological and photographic documentation. All the patients have approved that the data would be submitted for publication.
Authors’ Contribution
Abdullah A Nada contributed to study design, drafting, data collection, analysis, interpretation, revision and critical appraisal. Mostafa E Hammad contributed to study design, drafting, data collection, analysis, interpretation, revision, critical appraisal and drawing the diagrams. Ahmed F ELTANAHY contributed to data collection, drafting and critical revision. Ahmed A Gazar contributed to study design, drafting and critical revision. Ahmed M KHALIFA contributed to data interpretation, drafting and critical revision. Mohamed H El-Sayed contributed to study design, drafting and critical revision. All authors approve the final version of the paper provided.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Phedy P, Siregar PU. Osteotomy for deformities in blount disease: A systematic review. J Orthop. 2016;13(3):207. doi: 10.1016/j.jor.2015.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gkiokas A, Brilakis E. Management of neglected Blount disease using double corrective tibia osteotomy and medial plateau elevation. J Child Orthop. 2012;6(5):4118. doi: 10.1007/s11832-012-0443-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnston CE, Young M. Tachdjians Pediatric Orthopaedics, Fifth Edit. 5/e. Elsevier Inc.; 2017. Tachdjians Pediatric Orthopaedics, Disorders of the Leg. pp. 713–760.e5. [Google Scholar]
- 4.Jones S, Hosalkar HS, Hill RA, Hartley J. Relapsed infantile Blounts disease treated by hemiplateau elevation using the Ilizarov frame. J Bone Joint Surg Br. 2003;85(4):565–571. doi: 10.1302/0301-620x.85b4.13602. [DOI] [PubMed] [Google Scholar]
- 5.Griswold B, Gilbert S, Khoury J. Opening Wedge Osteotomy for the Correction of Adolescent Tibia Vara. Iowa Orthop J. 2018;38:1416. [PMC free article] [PubMed] [Google Scholar]
- 6.Gregosiewicz A, Wośko I, Kandzierski G, Drabik Z. Double-elevating osteotomy of tibiae in the treatment of severe cases of Blounts disease. J Pediatr Orthop. 1989;9(2):178–181. [PubMed] [Google Scholar]
- 7.Fitoussi F, Ilharreborde B, Lefevre Y, Souchet P, Presedo A, Mazda K, et al. Fixator-assisted medial tibial plateau elevation to treat severe Blount's disease: Outcomes at maturity. 2011:1728. doi: 10.1016/j.otsr.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 8.Langenskiöld A, Riska EB. Tibia vara (osteochondrosis deformans tibiae): a survey of seventy–one cases. JBJS. 1964;46(7):140520. [PubMed] [Google Scholar]
- 9.Daltroy LH, Liang MH, Fossel AH, Goldberg MJ. The POSNA pediatric musculoskeletal functional health questionnaire: report on reliability, validity, and sensitivity to change. J Pediatr Orthop. 1998;18(5):56171. doi: 10.1097/00004694-199809000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Krettek C, Miclau T, Gru O, Schandelmaier P, Tscherne H. Intraoperative control of axes, rotation and length in femoral and tibial fractures technical note. Injury. 1998;29:29–39. doi: 10.1016/s0020-1383(98)95006-9. [DOI] [PubMed] [Google Scholar]
- 11.Oto M, Yilmaz G, Bowen JR, Thacker M, Kruse R. Adolescent Blount disease in obese children treated by eight-plate hemiepiphysiodesis. Eklem Hast ve Cerrahisi. 2012;23(1):20–24. [PubMed] [Google Scholar]
- 12.Rahman A, Amer AL, Khanpour AA. Evaluation of treatment of late-onset tibia vara using gradual angulation translation high tibial osteotomy. Acta Orthop Belg. 2010;76(3):360–366. [PubMed] [Google Scholar]
- 13.van Huyssteen AL, Hastings CJ, Olesak M, Hoffman EB. Double-elevating osteotomy for late-presenting infantile Blounts disease. The importance of concomitant lateral epiphysiodesis. J Bone Jt Surg - Ser B. 2005;87(5):710–715. doi: 10.1302/0301620X.87B5.15473. [DOI] [PubMed] [Google Scholar]
- 14.Hofmann A, Jones RE, Herring JA. Blounts disease after skeletal maturity. J Bone Joint Surg Am. 1982;64(7):1004–1009. [PubMed] [Google Scholar]
- 15.Abraham E, Toby D, Welborn MC, Helder CW, Murphy A. New Single-stage Double Osteotomy for Late-presenting Infantile Tibia Vara: A Comprehensive Approach. J Pediatr Orthop. 2019;39(5):247–256. doi: 10.1097/BPO.0000000000000926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Siregar P. Bamboo Osteotomy for Blounts Disease. Malaysian Orthop J. 2010;4(1):56–59. doi: 10.5704/MOJ.1003.013. [DOI] [Google Scholar]
- 17.Rab GT. Oblique tibial osteotomy for Blounts disease (tibia vara). J Pediatr Orthop. 1988;8(6):715–720. doi: 10.1097/01241398-198811000-00018. [DOI] [PubMed] [Google Scholar]
- 18.Debarge R, Trouillet F, Demey G, Magnussen RA. High tibial osteotomy. Surg Knee. 2014;24(2):149–161. doi: 10.1007/978-1-4471-5631-4_16. [DOI] [Google Scholar]
- 19.Van Houten AH, Heesterbeek PJC, Van Heerwaarden RJ, Van Tienen TG, Wymenga AB. Medial open wedge high tibial osteotomy: Can delayed or nonunion be predicted? Clin Orthop Relat Res. 2014;472(4):1217–1223. doi: 10.1007/s11999-013-3383-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wright J, Calder P. Severe infantile blounts disease: Hemiplateau elevation and metaphyseal correction with use of the taylor spatial frame. J Limb Lengthening Reconstr. 2018;4(2):76. doi: 10.4103/jllr.jllr_2_18. [DOI] [Google Scholar]
- 21.Feldman DS, Madan SS, Ruchelsman DE, Sala DA, Lehman WB. Accuracy of correction of tibia vara: acute versus gradual correction. J Pediatr Orthop. 2006;26(6):794–798. doi: 10.1097/01.bpo.0000242375.64854.3d. [DOI] [PubMed] [Google Scholar]
- 22.Hefny H, Shalaby H, El-kawy S. A New Double Elevating Osteotomy in Management of Severe Neglected Infantile Tibia Vara using the Ilizarov Technique. 2006;26(2):233–237. doi: 10.1097/01.bpo.0000218530.59233.ab. [DOI] [PubMed] [Google Scholar]
- 23.Edwards TA, Hughes R, Monsell F. The challenges of a comprehensive surgical approach to Blounts disease. J Child Orthop. 2017;11(6):479–487. doi: 10.1302/18632548.11.170082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sachs O, Katzman A, Abu-johar E, Eidelman M. Treatment of Adolescent Blount Disease Using Taylor Spatial Frame With and Without Fibular Osteotomy: Is there any difference? 2015;35(5):501–506. doi: 10.1097/BPO.0000000000000317. [DOI] [PubMed] [Google Scholar]
- 25.Sasaki T, Yagi T, Monji J, Yasuda K, Kanno Y. Transepiphyseal plate osteotomy for severe tibia vara in children: follow-up study of four cases. J Pediatr Orthop. 1986;6(1):61–65. [PubMed] [Google Scholar]
- 26.Schoenecker PL, Johnston R, Rich MM, Capelli AM. Elevation of the medical plateau of the tibia in the treatment of Blount disease. J Bone Joint Surg Am. 1992;74(3):351–358. [PubMed] [Google Scholar]
- 27.Chotigavanichaya C, Salinas G, Green T, Moseley CF, Otsuka NY. Recurrence of varus deformity after proximal tibial osteotomy in Blount disease: long-term follow-up. J Pediatr Orthop. 2002;22(5):638–641. [PubMed] [Google Scholar]
- 28.Lützner J, Gross AF, Günther KP, Kirschner S. Reliability of limb alignment measurement for high tibial osteotomy with a navigation system. Eur J Med Res. 2009;14(10):447–450. doi: 10.1186/2047-783x-14-10-447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yoon S-D, Zhang G, Kim H-J, Lee B-J, Kyung H-S. Comparison of cable method and miniaci method using picture archiving and communication system in preoperative planning for open wedge high tibial osteotomy. Knee Surg Relat Res. 2016;28(4):283. doi: 10.5792/ksrr.16.052. [DOI] [PMC free article] [PubMed] [Google Scholar]