Abstract
BACKGROUND:
At the end of life, children with neurological conditions have complex health care needs that can be met by providing care of their life-limiting conditions concurrently with hospice care (i.e. concurrent care). Given the limited literature on concurrent care for children with neurologic conditions, this investigation aimed to identify patterns of non-hospice, health care service needs and to assess characteristics of children within each group.
METHODS:
A nationally representative sample children with neurological conditions enrolled in concurrent hospice care was used. Latent class analysis (LCA) and descriptive statistics were calculated to identify patterns of health care needs and characteristics of children within the groups. A subgroup analysis of infants was conducted.
RESULTS:
Among the 1,601 children, the most common types of services were inpatient hospitals, durable medical equipment, and home health. Two classes of service needs were identified: moderate-intensity (58%) and high-intensity (42%). Children in the moderate-intensity group were predominantly between 1 to 5-years of age, male, Caucasian, and non-Hispanic. The most common neurological condition was CNS degeneration. They also had significant comorbidities, mental/behavioral health conditions, and technology dependence. They commonly resided in urban areas in the South. Children in the high-intensity group had a wide range of neurological conditions and high acuity. The subgroup analysis of infants indicated a different neurological profile.
CONCLUSIONS:
Two distinct classes of non-hospice, health care services needs emerged among children with neurological conditions at end of life. The groups had unique demographic profiles.
Introduction
Children with neurological conditions at the end of life have unique and complex care needs. Many pediatric patients with life-limiting conditions such as brain/spinal cord malformation, central nervous system (CNS) disease, and infantile cerebral palsy have experienced poor health their entire, short lives. They often suffer with a wide range of nervous system symptoms including developmental delays, lack of coordination, changes in mood, seizures, muscle wasting, swallowing difficulties, and slurred speech. Consequently, their health care service needs can be significant, especially at the end of life. The enactment of the 2010 Affordable Care Act (ACA, Section 2302) allows children and their families to continue health care services for the child’s life-limiting condition while enrolled in hospice care. Concurrent hospice care changed the hospice eligibility rules for children in Medicaid or Children’s Health Insurance Program.1
Background
Although there is increasing evidence about pediatric concurrent hospice care,2-4 the health care service needs of children with neurological conditions during concurrent care has not received sufficient attention. In a series of case reports, Miller and colleagues5 identified the health care service needs of a pediatric patients in concurrent hospice care with degenerative neurologic disorders, progressive inflammatory polyneuropathy, and Huntington’s disease with intractable seizure. They found special feedings, medications, ventilators, and private duty nursing were the most common health care services used among these children. No other studies were identified that included this population at the end of life.
Given the limited literature on health care service needs in concurrent hospice care for children with neurological conditions, the current investigation had two aims. The first aim was to apply Latent Class Analysis (LCA) to identify patterns of non-hospice, health care service needs among children with neurological conditions. The second aim of the study was to assess the characteristics of latent class membership.
Methods
Data for this retrospective cohort designed study were from the Center for Medicare & Medicaid Services (CMS) Medicaid files, 2011-2013. The Medicaid files are national claims data collected annually by CMS. Although the intent of the claims data is to document payment to health care providers for services rendered to Medicaid beneficiaries, CMS provides data files for health care research upon approval of study protocols, data management plans, and data use agreement.6 Data are from all 50 states and the District of Columbia. For each Medicaid beneficiary, person-level research files are created by CMS and include Personal Summary (e.g., demographics), Inpatient (e.g., hospital admissions and procedures), Prescription Drugs (e.g., medications and dates) and Other Services (e.g., hospice, durable medical equipment, dental) records.7 Medicaid data are one of the only national sources of information on children enrolled in hospice care.
The sampling frame for this study was limited to children in hospice care, which was 21,383 children in the Medicaid data. The sample was restricted to children who received pediatric concurrent hospice care, which is defined as the receipt of hospice and non-hospice, health care services simultaneously during hospice enrollment. Pediatric concurrent hospice care is federally mandated for all state Medicaid programs by the Affordable Care Act, Section 2302.1 Children with life-limiting, neurological conditions [i.e., brain/spinal cord malformation, mental retardation disability, central nervous system (CNS) disease, infantile cerebral palsy, epilepsy, other neurological conditions (i.e., occlusion of cerebral arteries, muscular dystrophies, myopathies, movement disease)] as classified by Feudtner and colleagues8 were also included. Because pediatric concurrent hospice care is only available for children under 21 years, children over 21 years were excluded. Additionally, if dates of birth or death were missing, children were excluded from the study. The final sample was 1,601 children with neurological conditions, who received pediatric concurrent hospice care. The Institutional Review Board of the University of Tennessee, Knoxville reviewed and approved the study.
Measures
Health Care Service Needs.
Several steps were used to create the measures of non-hospice, health care service needs from the Medicaid data. First, non-hospice health care services were identified in the Inpatient, Other Services, and Prescriptions records. Using a date algorithm, the services dates were matched with hospice care dates and retained.9,10 Next, the health care service needs were coded using CMS-assigned service labels. Twenty labels were used including inpatient hospital, durable health equipment, home health, medications, labs & x-rays, other services, targeted case management, physician services, outpatient hospital, personal care, private duty nursing, transportation, rehabilitation, physical therapy/occupational therapy/speech therapy, clinic, other practitioners, psychiatric services, dental services, residential care, and nurse practitioner services. Individual measures were created for each category and dichotomized as “yes” or “no.”
Demographics.
A set of demographic variables was created for this study. Age group was operationalized as <1 yr, 1-5 years, 6-14 years, and 15-20 years. Gender was dichotomized as female or male. Caucasian, Black, and other races were the categories for race, while ethnicity was either Hispanic or non-Hispanic. Comorbidities were defined as the presence of multiple complex chronic conditions.11 Mental/behavioral health conditions and technology dependence were dichotomized variables.8,12 Measures of the child’s residence were rural/urban and region (Midwest, Northeast, South, and West). 13
Data Analysis
The primary goal of this study was to apply the Latent Class Analysis (LCA) to identify unobserved latent subgroups of children with neurological conditions in concurrent hospice care with respect to their non-hospice health care service needs.14 The second goal was to assess the demographic characteristics of latent class membership. A series of LCA models with an increasing number of latent classes were created from the health care service needs and used to determine the optimal number of latent classes.
To approximate the optimal number of latent classes, the number of classes estimated was increased incrementally one class at a time until LCA goodness of fit measures indicated that model testing should cease. Overall fit of each model was assessed using several statistical measures including the Lo-Mendell-Rubin (LMR) likelihood ratio (detects the correct number of classes), log likelihood (detects the correct number of classes), Akaike information criterion (AIC) (evaluates the quality of a model), Bayesian information criteria (BIC) (evaluates the quality of a model), and entropy values (identifies distinctness of classes).15,16 Once the number of latent classes was identified, the prevalence rates of the latent classes and the conditional item probabilities of the individual health care service needs was calculated and values greater than 0.50 were used to define classes.20 Children were classified into an appropriate latent class based on conditional probabilities. Descriptive statistics were calculated to describe the demographic characteristics within the latent classes (i.e., frequencies). A subgroup analysis was performed among infants <1 year with neurological conditions in concurrent hospice care to examine their unique demographic profile in the latent classes. All analyses were conducted with Stata, version 15.17
Results
Table 1 displays the health care service needs of children with neurological conditions in pediatric concurrent hospice care (Supplemental Digital Content). The 1,601 children in the study generated approximately 370,000 non-hospice, health care service claims while enrolled in hospice. The most common types of service were inpatient hospital (e.g., enteral infusions, parenteral infusions, mechanical ventilation, transfusions), followed by durable medical equipment (e.g., enteral feeding supplies, oxygen equipment, suctions/pumps), home health (e.g., nursing, therapeutic exercise), and targeted case management. The least common service needs were residential care, dental, and nurse practitioner care.
Model fit indices for the different LCA models are shown in Table 2 (Supplemental Digital Content). The two-class model was considered optimal because the data fit better than the one- or three-class models. As the number of classes increased, the AIC and BIC decreased at 2 classes, which indicated improved model fit.18 Additionally, the two-class model had the highest entropy value, which also suggested best model fit.19
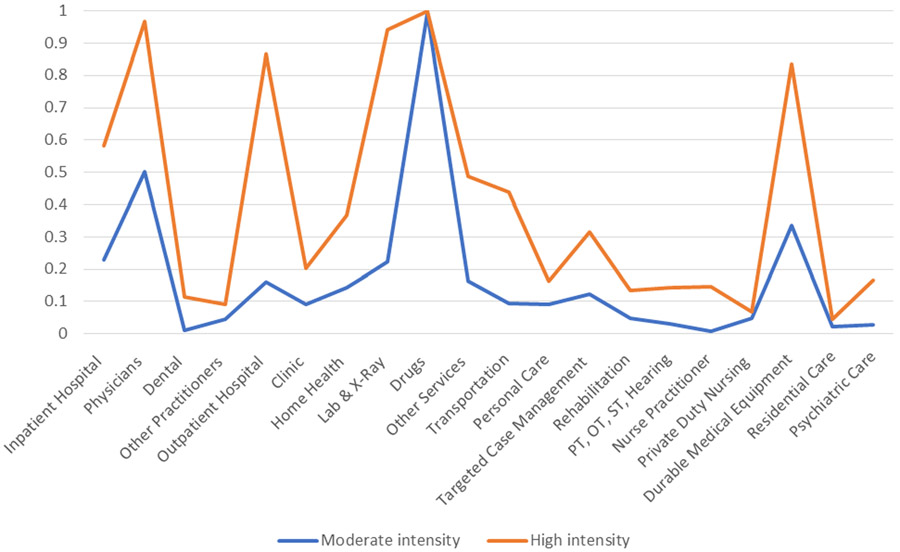
For the two-class model, conditional item probabilities are presented in Table 3 (Supplemental Digital Content). Fifty-eight percent of the sample was classified into Class 1 and 42% into Class 2. Class 1 was defined as “moderate intensity” with conditional probabilities >0.50 for use of physician services (0.502) and medications (0.992). Class 2 was defined as “high intensity” because the conditional probabilities were very high in six categories including inpatient hospital (0.582), physicians (0.968), outpatient hospital (0.866), labs & x-ray (0.940), medications (0.999), and durable medical equipment (0.834). Figure 1 displays the conditional item probabilities by class.
Figure 1.
Conditional Item Probabilities of Health Care Service Needs by Class
The demographic characteristics of latent class membership are shown in Table 4. Children in Class 1 were most frequently in the 1 to 5-year age group (36.1%), male (52.5%), Caucasian (44.9%), and non-Hispanic (77.9%). The most common neurological condition was CNS degeneration and diseases (63.8%) and the least common was intellectual dysfunction (12.5%). A majority of children in Class 1 suffered with comorbidities (77.5%), mental/behavioral health conditions (62.0%), and technology dependence (63.6%). These children frequently resided in urban areas (53.0%) in the South (34.0%). The group comprising Class 2 was most often 1 to 5 years (40.0%), male (54.6%), Other race (57.3%), and non-Hispanic (77.1%). CNS degeneration and disease were the most common neurological condition (89.0%) and intellectual dysfunction the least (14.1%). The health of Class 2 members was complicated by high comorbidities (94.9%), mental/behavioral health conditions (75.5%), and technology dependence (85.3%). A majority of children in Class 2 resided in rural areas (52.4%) in the South (52.5%).
Table 4.
Characteristics of Children with Neurological Conditions in Concurrent Hospice Care within Two-Class Model (N=1,601)
| Variables | All Children | Class 1 Moderate Intensity n = 933 |
Class 2 High Intensity n = 668 |
|---|---|---|---|
| Age Groups (%) | |||
| <1 yr | 14.1 | 10.9 | 18.4 |
| 1 to 5 yrs | 37.7 | 36.1 | 40.0 |
| 6 to 14 yrs | 31.9 | 33.2 | 30.0 |
| 15 to 20 yrs | 16.3 | 19.8 | 11.6 |
| Gender (%) | |||
| Female | 46.6 | 47.5 | 45.4 |
| Male | 53.4 | 52.5 | 54.6 |
| Race (%) | |||
| Caucasian | 38.7 | 44.9 | 30.1 |
| Black | 13.9 | 14.8 | 12.6 |
| Other Races | 47.4 | 40.3 | 57.3 |
| Ethnicity (%) | |||
| Hispanic | 22.4 | 22.1 | 22.9 |
| Non-Hispanic | 77.6 | 77.9 | 77.1 |
| Neurological Conditions a (%) | |||
| Brain and spinal cord malformations | 41.19 | 39.8 | 43.1 |
| Intellectual function | 13.14 | 12.5 | 14.1 |
| CNS degeneration and diseases | 74.28 | 63.8 | 89.0 |
| Infantile cerebral palsy | 40.13 | 36.7 | 44.9 |
| Epilepsy | 31.89 | 27.9 | 37.5 |
| Other disorders | 20.44 | 19.1 | 22.4 |
| Comorbidities (%) | 84.8 | 77.5 | 94.9 |
| Mental/Behavioral Health Conditions (%) | 67.6 | 62.0 | 75.5 |
| Technology Dependence (%) | 72.6 | 63.6 | 85.3 |
| Rural/Urban (%) | |||
| Urban | 51.1 | 53.0 | 48.5 |
| Rural | 49.5 | 47.4 | 52.4 |
| Region (%) | |||
| Midwest | 20.3 | 21.0 | 19.3 |
| Northeast | 16.3 | 25.4 | <10.0 |
| South | 41.7 | 34.0 | 52.5 |
| West | 21.7 | 19.6 | 24.6 |
Neurological conditions are not mutually exclusive; <10.0 is noted for values under 10% per Data Use Agreement; CNS = central nervous system
Analysis of infant characteristics within the two-class model are listed in Table 5 (Supplemental Digital Content). Fifty-one percent of the infants were in Class 1 and 48.8% in Class 2. Class 1 infants were characterized as predominately female (55.6%), Caucasian (44.4%), non-Hispanic (100.0%). Brain and spinal cord malformations were the most common neurological condition (77.4%), followed by CNS degeneration and diseases (73.6%) and epilepsy (32.1%). Most of Class 1 infants had comorbidities (77.8%) and technology dependence (66.7%). Infants in this class resided in urban areas (66.7%) in the Northeast (44.4%). Class 2 demographics highlighted a group of infants who were mostly male (62.5%), Other race (62.5%), and non-Hispanic (75.0%). The most common neurological conditions were brain and spinal cord malformations (78.43%), CNS degeneration and diseases (44.2%), and epilepsy (18.6%). All of the infants in this class had comorbidities and technology dependence. Their residence was frequently in urban areas (75.0%) in the South (50.0%).
Discussion
This study explored non-hospice, health care service needs among children with neurological conditions in concurrent hospice care. Two unobserved distinct latent classes were identified: Moderate intensity (Class 1); and High intensity (Class 2). Both of these classes exhibited unique patterns of needs and demographic profiles from one another. The LCA presented a novel way of understanding groups of health care service needs among children with neurological conditions that may inform tailored and targeted end-of-life care for different groups.
The group comprising the highest percentage of children with neurological conditions (58.3%) was Class 1. Their health care service needs were more likely to be focused on physician services and medications. The high intensity - Class 2 group included 41.7% of the children in the sample. This group had high health care service needs, which ranged from inpatient hospital to outpatient hospital to auxiliary services such as labs, x-rays, medications, and durable medical equipment. The analysis revealed that children in this group were more likely to reside in rural areas, compared to Class 1. This finding was unexpected. Children in rural areas at the end of life often have long distances to travel to health care services and in many cases traverse difficult terrain (e.g., mountains). The challenges of transporting a child in a personal vehicle or with transportation services are complicated by very common symptoms such as nausea and vomiting, along with transporting equipment such as oxygen. For children with siblings, parents may have additional challenges of multiple children in the car. However, in this study, rural children in Class 2 more often used health care services that normally would be located outside their community. Inpatient and outpatient services are often provided for children at end of life at a Children’s Hospital, which are almost exclusively located in urban areas. Research is needed to understand the experiences and perspectives of families in utilizing high intensity services while their child is in hospice care. Understanding the challenges and benefits of obtaining this type of care might inform the quality of delivery care for children.
The subgroup analysis among infants identified a different membership profile in the classes. Compared to the children in the study, infants had a different composition of neurological conditions. Whereas children in the overall sample primarily had CNS degeneration and diseases, infants frequently had brain and spinal cord malformation. This finding is consistent with the end-of-life literature examining the health of infants.20 While infants accounted for just 14% of the sample, it is important to note that they received high intensity healthcare services. This is consistent with how palliative care is typically delivered in the NICU: as a companion therapy to cure-oriented care.21 How an infant may fare based on their condition at birth is hard to predict and efforts are almost always initially focused on life-sustaining therapies. An infant’s condition may improve over a period of days or the infant may begin to languish over weeks or months, going on to develop complex chronic illnesses that require escalating support. During this time, while curative care continues, the provision of concurrent palliative care may provide symptom management and other supportive care to the infant and the family until such time that a decision might be made to limit, or even to withdraw, life-sustaining therapies if the burdens of technological care begin to outweigh the benefits of treatment.22 This breadth of findings suggests that programs and services be targeted by age and development in order to meet the particular demands of the condition and particular needs of families.
Strengths and Limitations
There are several limitations to note. First, this study used Medicaid data. The findings are generalizable to this group of children and might be different among children in private insurance or Tricare in receipt of concurrent hospice care. Second, pooled cross-sectional data of claims during a three-year period was used. Finally, the study used data from 2011 to 2013, which is aged. However, these data were the most current Medicaid data available and they provided the first-ever and most currently available snapshot of the national health care services used by children with neurological conditions in concurrent hospice care.
Conclusion
As one of the first latent class analysis studies of the health care service needs among children with neurological conditions during pediatric concurrent hospice care, this study provided evidence of unique groups of service needs. The results suggested that health care services cluster together in unique fashion with distinct patterns of moderate and high intensity. In addition, the demographic composition of the classes differed widely, especially among a subgroup of infants. Taken together, the results can help clinicians, researchers, and policy makers advocate for services that meet the care demands and supports of children and families in a meaningful manner with targeted support.
Supplementary Material
Table 1. Prevalence of Health Care Service Needs Among Children with Neurological Conditions in Concurrent Hospice Care
Table 2. Model Fit Indices for Latent Class Analysis
Table 3. Conditional Item Probabilities of Health Care Service Needs within Two-Class Model (N=1,601)
Table 5. Subgroup Characteristics within Two-Class Model - Infants (N=209)
Acknowledgements:
Special thanks to Ms. Jamie Butler for her assistance with the manuscript.
Funding Source:
This publication was made possible by Grant Number R01NR017848 from the National Institute of Nursing Research and National Institute of Health Office of the Director (PI: Lindley). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Nursing Research or National Institutes of Health.
Contributor Information
Lisa C. Lindley, College of Nursing, University of Tennessee, Knoxville, Knoxville, Tennessee 37996.
Radion Svynarenko, College of Nursing, University of Tennessee, Knoxville, Knoxville, Tennessee 37996.
Kim Mooney-Doyle, School of Nursing, University of Maryland, Baltimore, MD 21201.
Annette Mendola, Department of Medicine, The University of Tennessee Medical Center, Knoxville, TN 37920.
Wendy C. Naumann, Columbus, OH 43221.
Christine A. Fortney, Martha S. Pitzer Center for Women, Children and Youth, College of Nursing, The Ohio State University, Columbus, Ohio 43210.
References
- 1.Lindley LC. Health care reform and concurrent curative care for terminally ill children: a policy analysis. J Hosp Palliat Nurs. 2011;13(2):81–88. doi: 10.1097/NJH.0b013e318202e308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Keim-Malpass J, Cozad MJ, Svynarenko R, Mack JW, Lindley LC. Medical complexity and concurrent hospice care: A national study of Medicaid children from 2011 to 2013. J Spec Pediatr Nurs. Published online April 3, 2021:e12333. doi: 10.1111/jspn.12333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lindley LC, Cozad MJ, Svynarenko R, Keim-Malpass J, Mack JW. A national profile of children receiving pediatric concurrent hospice care, 2011 to 2013. J Hosp Palliat Nurs. 2021; 23(3), 214–220. doi: 10.1097/NJH.0000000000000738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lindley LC, Richar CS, Hoit T, Steinhorn DM. Cost of pediatric concurrent hospice care: an economic analysis of relevant cost components, review of the literature, and case illustration. J Palliat Med. Published online January 12, 2021. doi: 10.1089/jpm.2020.0495 [DOI] [PubMed] [Google Scholar]
- 5.Miller EG, LaRagione G, Kang TI, Feudtner C. Concurrent care for the medically complex child: lessons of implementation. J Palliat Med. 2012;15(11):1281–1283. doi: 10.1089/jpm.2011.0346 [DOI] [PubMed] [Google Scholar]
- 6.Ruttner L, Borck R, Nysenbaum J, Williams S. Guide to MAX data. Math Policy Res. 2015;21. [Google Scholar]
- 7.Wenzlow A, Bouchery E, Czajka J. Expanding Access to Medicaid Data for Research: Feasibility of MAX Sample. Medicaid Policy Brief Final Report. Washington, DC: Mathematica Policy Research; 2010. [Google Scholar]
- 8.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14(1):199. doi: 10.1186/1471-2431-14-199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mor V, Joyce NR, Coté DL, et al. The rise of concurrent care for veterans with advanced cancer at the end of life. Cancer. 2016;122(5):782–790. doi: 10.1002/cncr.29827 [DOI] [PubMed] [Google Scholar]
- 10.Mor V, Wagner TH, Levy C, et al. Association of expanded va hospice care with aggressive care and cost for veterans with advanced lung cancer. JAMA Oncol. 2019;5(6):810. doi: 10.1001/jamaoncol.2019.0081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lindley LC, Mack JW, Bruce DJ. Clusters of multiple complex chronic conditions: a latent class analysis of children at end of life. J Pain Symptom Manage. 2016;51(5):868–874. doi: 10.1016/j.jpainsymman.2015.12.310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garfield LD, Brown DS, Allaire BT, Ross RE, Nicol GE, Raghavan R. Psychotropic drug use among preschool children in the Medicaid program from 36 states. Am J Public Health. 2015;105(3):524–529. doi: 10.2105/AJPH.2014.302258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Federal Office of Rural Health Policy (FORHP). Defining Rural Population. Updated January, 2021. Accessed February 11, 2021. https://www.hrsa.gov/rural-health/about-us/definition/index.html
- 14.Muthen B Latent variable hybrids: overview of old and new models. In: Hancock GR, Samuelsen KM, eds. Advances in Latent Variable Mixture Models. The CILVR series on latent variable methodology. Information Age Pub; 2008:1–24. [Google Scholar]
- 15.Lo Y Testing the number of components in a normal mixture. Biometrika. 2001;88(3):767–778. doi: 10.1093/biomet/88.3.767 [DOI] [Google Scholar]
- 16.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equ Model. 2007;14(4):535–569. doi: 10.1080/10705510701575396 [DOI] [Google Scholar]
- 17.StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC; 2017. [Google Scholar]
- 18.Nylund-Gibson K, Choi AY. Ten frequently asked questions about latent class analysis. Transl Issues Psychol Sci. 2018;4(4):440–461. doi: 10.1037/tps0000176 [DOI] [Google Scholar]
- 19.DiStefano C, Kamphaus RW. Investigating subtypes of child development: a comparison of cluster analysis and latent class cluster analysis in typology creation. Educ Psychol Meas. 2006;66(5):778–794. doi: 10.1177/0013164405284033 [DOI] [Google Scholar]
- 20.Smith SA, Choo AL, Foster ME. Latent class analysis reveals distinct groups based on executive function and socioemotional traits, developmental conditions, and stuttering: A population study. Child Psy Human Develop. 2021, epub. doi: 10.1007/s10578-021-01160-2 [DOI] [PubMed] [Google Scholar]
- 21.Squier W, Cowan FM. The value of autopsy in determining the cause of failure to respond to resuscitation at birth. Semin Neonatol. 2004;9(4):331–345. doi: 10.1016/j.siny.2004.01.003 [DOI] [PubMed] [Google Scholar]
- 22.Carter B Pediatric palliative care in infants and neonates. Children. 2018;5(2):21. doi: 10.3390/children5020021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wool C State of the science on perinatal palliative care. J Obstet Gynecol Neonatal Nurs. 2013;42(3):372–382; quiz E54–55. doi: 10.1111/1552-6909.12034 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table 1. Prevalence of Health Care Service Needs Among Children with Neurological Conditions in Concurrent Hospice Care
Table 2. Model Fit Indices for Latent Class Analysis
Table 3. Conditional Item Probabilities of Health Care Service Needs within Two-Class Model (N=1,601)
Table 5. Subgroup Characteristics within Two-Class Model - Infants (N=209)