Abstract
Chronic pain and post-traumatic stress disorder (PTSD) frequently co-occur, and research suggests that these 2 conditions exacerbate one another producing greater impact on normal functioning in combination than separately. The influence of traumatic experiences on both pain and PTSD has been shown, but the nature of this interplay remains unclear. Although Criterion A trauma is required for the diagnosis of PTSD, whether the association between PTSD and chronic pain is dependent on Criterion A is underexplored. In this observational cohort study, we examined the association between pain and PTSD-like symptoms in the context of Criterion A trauma in 5,791 men from the Vietnam Era Twin Registry. Correlations and mixed-effects regression models were used to evaluate the relationship between PTSD Checklist-Civilian Version symptoms and multiple indicators of pain from the Short Form McGill Pain Questionnaire across trauma history and chronic pain conditions. 53.21% of the participants experienced trauma consistent with DSM-IV Criterion A for PTSD. The associations between pain indicators and PTSD-like symptoms was stronger for individuals with a history of trauma but remained robust for individuals without trauma history. Small but significant interactions between past trauma and pain indicators and PTSD-like symptoms were observed. Findings were similar in a subsample of participants with history of chronic pain conditions. The relationship between PTSD-like symptoms and indicators of pain were largely independent of trauma consistent with Criterion A, highlighting the need to better understand and address stressful life events in chronic pain patients and pain concerns in individuals reporting trauma.
Keywords: Pain intensity, Post-traumatic stress disorder, Trauma, Stressful life events, Veterans
Pain is one of the most commonly reported health concerns of patients with post-traumatic stress disorder (PTSD), a mental health diagnosis that may occur after exposure to a traumatic event and is characterized by a constellation of symptoms including intrusive thoughts, dreams or memories, psychological distress including avoidance of reminders, and alterations in cognition, mood, and heightened arousal and reactivity.5 A growing number of studies have shown that PTSD symptoms tend to be elevated in patients with chronic pain conditions.9 With an estimated 1 in 5 adults suffering from chronic pain, it presents an immense public health problem.22 In fact, chronic pain is reported in 20 to 80% of individuals with a history of trauma, and 10 to 50% of individuals with PTSD report chronic pain.48 Patients with chronic pain and a history of trauma have worse functional status, report greater distress, and demonstrate worse response to medical intervention.43 Similarly, the presence of chronic pain and PTSD increases symptom severity in both conditions.43
The high rate of comorbidity and considerable symptom overlap—including hyperarousal, avoidance, anxiety, emotional lability, somatic focus—between chronic pain and PTSD suggests that the disorders may share an underlying etiology.7,10,18,43 Recent work by our group confirmed overlap in both genetic and nonshared environmental factors contributing to PTSD and chronic overlapping pain conditions (COPCs) including migraine headache, temporomandibular disorder, and chronic back pain.20 The significant nonshared environmental correlations revealed an overlap in environmental factors that contribute to both PTSD and COPCs. However, these findings did not consider specific types of environmental experiences, nor characterize the role of trauma. Although the contribution of common environmental influences to the development of both chronic pain conditions and PTSD symptoms and is supported, and while a diagnosis of PTSD is conditional on the presence of trauma, it is unclear whether the association between pain symptoms and PTSD symptoms is contingent on or is largely independent of trauma history.
Trauma exposure meeting a specific standard, known as Criterion A in the Diagnostic and Statistical Manual of Mental Disorders (DSM) is central to a diagnosis of PTSD but defining exactly what constitutes trauma has been difficult and some have challenged the construct validity of this “diagnostic gate keeper.”25,38,47 Though the definition of Criterion A has broadened across DSM editions—from the stringent DSM-III2 standard of events being considered traumatic only if they were “outside the realm of normal human experience,” to the events that are direct or indirect, threatened, or actual in the DSM-IV3, to the more inclusive definition of actual or threatened death, serious injury, or sexual violence as well as indirect and repeated exposure to details of trauma in the DSM-55—trauma above a certain threshold remains a diagnostic requirement. Criterion A trauma is necessary but not sufficient for a PTSD diagnosis. While 50 to 85% of people experience a Criterion A event in their life-time,24 individuals vary in their vulnerability to trauma; most do not go on to develop PTSD symptoms and the lifetime civilian prevalence of PTSD is around 7%.30 Challenges to the predictive validity of Criterion A have shown that PTSD symptoms may emerge in the context of stressful life events rather than Criterion A and that the absence of Criterion A does little to affect overall prevalence rates of a PTSD diagnosis.19,25,32
The above puts into question the role of trauma on the relationship between chronic pain and PTSD. If trauma does contribute to the relationship between chronic pain and PTSD, it is unclear whether the nature of the trauma experience needs be consistent with PTSD criterion A or whether less severe experiences, such as stressful life events (eg, divorce, job loss, illness, or medical treatment)–which have been associated with both pain phenotypes31,50,52 and PTSD severity33–may also contribute to the co-occurrence of chronic pain and PTSD symptoms. In other words, is the association between chronic pain and PTSD contingent on an experience of severe trauma above the threshold set by the DSM or does it extend beyond it to include stressful life events?
Few investigations into the role of trauma on the relationship between pain phenotypes and PTSD have been carried out. To our knowledge, no studies have examined the role of Criterion A trauma and stressful life events in the relationship of chronic pain and PTSD symptoms. The link between chronic pain and PTSD may be confounded by the occurrence of specific types of traumatic events that can cause personal physical injury that then precipitate chronic pain and PTSD.9 Thus, only a small handful of studies have examined the relationship between trauma, chronic pain, and PTSD and those have primarily focused on injury-related trauma and none on stressful life events. Previous limited research suggests that the relationship between chronic pain and PTSD may be independent of type of trauma exposure.1,36,37 Given the dearth of research in this area, the main aim of this study was to investigate the role of Criterion A trauma versus stressful life events on the relationship between several indicators of pain and PTSD-like symptoms in a sample of Veterans. We hypothesized that the relationship between indicators of pain and PTSD-like symptoms would be maintained independent of reported Criterion A trauma history, indicating both that PTSD-like symptoms may be present in the absence of Criterion A trauma and that these symptoms would maintain their association with pain. Because the relationship between pain indicators and PTSD-like symptoms could be contingent on the presence or absence of chronic pain, we further examined these associations in in a subsample of individuals with one or more COPCs. We hypothesized that restricting the sample to individuals with chronic pain conditions would reduce the association between pain indicators and PTSD-like symptoms.
Methods
Participants
Data used for this study were collected as part of an ongoing registry of veterans who are twins. Participants were recruited from the Vietnam Era Twin (VET) Registry, a community-based sample of male twins born between 1939 and 1957, and who both served in the U. S. military at some point between 1965 and 1975.23 With approximately 7,500 twin pairs, the VET Registry is one of the largest twin registries in the United States with participants in all 50 states. Initial contact of registry members occurred in 1987 when basic demographic information, health assessment, and zygosity evaluation took place. The Registry has been described in detail previously.49
Procedures
Between 2010 and 2012, participants were contacted regarding Veterans Administration (VA) Cooperative Study #569—“The course and consequences of post-traumatic stress disorder in Vietnam-era veteran twins.” A mailed questionnaire evaluated a wide range of physical and mental health issues, including pain intensity and PTSD symptoms. A subset of participants available for participation was contacted by telephone for an interview which included the evaluation of DSM, Fourth Edition (DSM-IV)3 Criterion A trauma history as part of the structured Composite International Diagnostic Interview (CIDI).29 Data collection was done under contract by Abt SRBI, Inc. The VA Central Institutional Review Board and the Research and Development Committee at VA San Diego Healthcare System approved the study. All participants provided written informed consent.
Measures
Pain Indicators.
Clinical pain intensity was measured using the Short Form McGill Pain Questionnaire (MPQ).40 The MPQ is designed to assess multiple components of pain including sensory and affective experiences.39 Participants rated 15 descriptors (11 sensory; 4 affective) on an intensity scale form 0 = “none”, 1 = “mild”, 2 = “moderate” or 3 = “severe” regarding pain in the past week. Sensory items include descriptors or pain such as “throbbing” or “stabbing”, while the affective items include descriptors such as “punishing-cruel” and “tiring-exhausting.” In addition to a total score (range 0 to 45), scores for Sensory (MPQ-S; range 0 to 33), and Affective (MPQ-A; range 0 to 12) descriptors were calculated. The Short Form MPQ also includes a rating of pain intensity over the past week adapted from a visual analogue scale to a rating of 0 = “no pain” to 10 = “worst pain possible” (MPQ-VAS) and a Present Pain Intensity (MPQ-PPI) rating of current pain on a scale of 0 = “no pain” to 5 = “excruciating pain.” Higher scores indicate greater sensory or affective components to pain severity. This instrument has shown good reliability and validity for a wide variety of acute and chronic pain populations.41
PTSD-Like Symptoms.
The PTSD Checklist-Civilian Version (PCL),53 a self-report questionnaire of PTSD symptoms, was used to assess PTSD symptom burden over the previous 4 weeks. Because veterans were discharged from the military decades prior, the civilian, rather than the military, version of the PCL was used54 to also capture nonmilitary related potentially traumatic experiences. The PCL consists of 17 items corresponding to DSM, Fourth Edition (DSM-IV)4 symptom criteria with each item scored on a 5-point scale from 1 = “not at all” to 5 = “extremely”. PTSD symptom clusters corresponding to the DSM-IV criteria were derived from PCL items. Cluster “B” re-experiencing symptoms from PCL questions 1 to 5, cluster “C” Avoidance symptoms from PCL questions 6 to 12, and cluster “D” Arousal symptoms from PCL questions 13 to 17 were calculated. Because PTSD criterion A is not required, the PCL assesses PTSD symptom burden in the context of stressful life events, rather than specific previous Criterion A trauma. Total scores range from 17 to 85. The PCL has strong agreement with the Clinician Administered PTSD Scale55 as well as the CIDI PTSD module.34
Trauma history.
Trauma history was assessed as part of the telephone administration of the CIDI29 according to the DSM-IV. The CIDI is a structured instrument intended for administration by trained nonclinical interviewers. Training for the CIDI was done by certified trainers at the start of the study and continuously monitored during the fieldwork. Standard CIDI administration was followed in which symptom questions for up to 2 separate Criterion A traumatic events named by the respondent were asked. Consistent with DSM-IV criteria,4 trauma events constituted experiences that were life-threatening and were accompanied by a reaction of fear, helplessness, or horror. Trauma history assessed was not limited to military experiences, but could reflect any traumatic experience, before, during, or after military service. If more than 2 events were reported by the participant and if one event involved theater combat exposure, follow-up questions were asked about the combat exposure event. Based on this PTSD assessment, respondents were classified as having reported the presence or absence of lifetime Criterion A trauma.
Chronic pain conditions.
Including fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, temporomandibular disorder, migraine headache, tension headache, chronic prostatitis, chronic joint pain, and chronic back pain, known as COPCs were assessed with a questionnaire. COPCs represent a group of complex chronic pain conditions that lack a clear etiology and are characterized by disability, poor health outcomes, health care overutilization, and lower quality of life.35 Participants were asked, “Have you ever been told by a doctor or other health professional that you had …” followed by a list of conditions. Individuals who endorsed a history of one or more of these chronic pain conditions were included in the chronic pain subsample.
Statistical Analyses
T-tests were used to evaluate differences between individuals with and without trauma in the full sample and the chronic pain subsample. Further analyses were conducted using correlations and mixed-effects regression models in R,45 lme4 package,11 in order to account for the correlated structure of the twin data. Each twin was identified by a unique ID and a twin-pair specific number, known as a family ID, which was entered as a random effect in the models. Analyses were conducted in the full sample, and in the chronic pain subsample. Models controlled for the effects of age, and when significantly skewed, data were natural log transformed to approximate normality. To evaluate the role of Criterion A trauma on the relationship between pain intensity and PTSD-like symptoms, we tested for the significance of interactions between PCL-Total and trauma as well as MPQ-Total and trauma. We tested for the interaction of trauma on the associations between PCL and MPQ-T and the 4 MPQ subscales. Similarly, we evaluated the significance of the coefficient for the interaction terms indicating whether the association between pain intensity and PTSD-like symptoms differed in the trauma and the no-trauma groups. Plots for interactions significant at P < .05 were used to ease interpretation.
Results
Out of 7,568 participants, 5,975 (77.6%) were asked to and completed the phone interview assessing Criterion A traumatic experiences; of these, 272 individuals had missing survey data, resulting in an analytic data set of 5,703. Of these, 3,086 were monozygotic, 2,126 dizygotic, and 491with undetermined zygosity. Consistent with the VET Registry sample, participants were middleaged (mean = 61.1 years, range 53–73), mostly White (93.3%), and non-Hispanic (96.9%). Most were married or widowed (79.9%) and most (71.3%) had completed at least some college education.
Of the full sample of 5,703 Veterans, 2,553 (44.8%) individuals reported at least one COPC, making up the chronic pain subsample (Table 1). 3,015 (52.9%) individuals of the full sample, and 1,581 (61.9%) of the chronic pain subsample respectively, reported experiencing at least one traumatic event consistent with PTSD criterion A of the DSM-IV.4 Within the full sample and the chronic pain subsample, individuals with a history of Criterion A trauma reported significantly higher levels of symptoms across all PCL and MPQ scales compared to individuals without a reported history of Criterion A trauma (t-test P’s < .001). Cohen’s d effect size values (Table 1) ranged from d = .43 for PPI to d = .70 for PPI-total, in the chronic pain subsample, suggesting a small to moderate level of practical significance, with most comparisons in the small effect size range.15 Highest levels of symptoms were reported by individuals with a history of trauma and at least one COPC. However, individuals without a reported history of Criterion A trauma also reported symptoms across nearly the entire range of PCL scores (Fig 1) (range = 17–83) though with less variability.
Table 1.
PTSD-Like Symptoms (PCL) and Pain Indicators (MPQ) Across Level of Trauma
|
Full Sample
|
Chronic Pain Subsample
*
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Missing | All N = 5,703 Mean (SD) | Trauma Yes, n = 3,015 Mean (SD) | Trauma No, n = 2,688 Mean (SD) | P | D | All N = 2,553 Mean (SD) |
Trauma Yes, n = 1,581
Mean (SD) |
Trauma No, n = 972
Mean (SD) |
P | d | |
| PCL-Total | 25 | 26.91 (13.34) | 30.78 (15.36) | 22.56 (8.80) | <.001 | .66 | 31.81 (15.67) | 35.60 (16.84) | 25.66 (11.10) | <.001 | .70 |
| Re-experiencing | 19 | 7.23 (3.94) | 8.30 (4.63) | 6.03 (2.49) | <.001 | .61 | 8.48 (4.79) | 9.57 (5.24) | 6.70 (3.23) | <.001 | .66 |
| Avoidance | 16 | 10.88 (5.77) | 12.47 (6.64) | 9.10 (3.90) | <.001 | .62 | 12.87 (6.79) | 14.41 (7.29) | 10.36 (4.94) | <.001 | .65 |
| Arousal | 18 | 8.82 (4.48) | 10.05 (5.03) | 7.44 (3.26) | <.001 | .62 | 10.49 (5.08) | 11.64 (5.37) | 8.62 (3.91) | <.001 | .64 |
| MPQ-Total | 229 | 5.77 (7.84) | 7.57 (8.89) | 3.80 (5.89) | <.001 | .50 | 9.78 (9.34) | 11.42 (9.86) | 7.14 (7.77) | <.001 | .48 |
| Sensory | 225 | 4.67 (6.11) | 6.04 (6.85) | 3.16 (4.74) | <.001 | .49 | 7.83 (7.15) | 9.06 (7.48) | 5.86 (6.10) | <.001 | .47 |
| Affective | 228 | 1.11 (2.09) | 1.53 (2.44) | .65 (1.50) | <.001 | .44 | 1.95 (2.66) | 2.37 (2.87) | 1.28 (2.13) | <.001 | .43 |
| VAS | 115 | 2.80 (2.70) | 3.41 (2.83) | 2.12 (2.36) | <.001 | .50 | 4.28 (2.75) | 4.72 (2.72) | 3.56 (2.64) | <.001 | .43 |
| PPI | 98 | 1.29 (1.12) | 1.54 (1.17) | 1.01 (.99) | <.001 | .48 | 1.88 (1.13) | 2.06 (1.14) | 1.59 (1.06) | <.001 | .43 |
Abbreviations: PCL-Total, PTSD Checklist total score; MPQ-Total, Short Form McGill Pain Questionnaire total score; VAS, MPQ Visual Analogue Scale; PPI, MPQ Present Pain Intensity; SD, standard deviation; P, probability value; d, Cohen’s d, (M1 - M2)/SD; small effect d, .20, medium effect d, .50, large effect d = .80. Mean levels compared using Welch 2 sample t-tests.
History of chronic pain defined by the endorsement of one or more chronic overlapping pain conditions evaluated.
Figure 1.
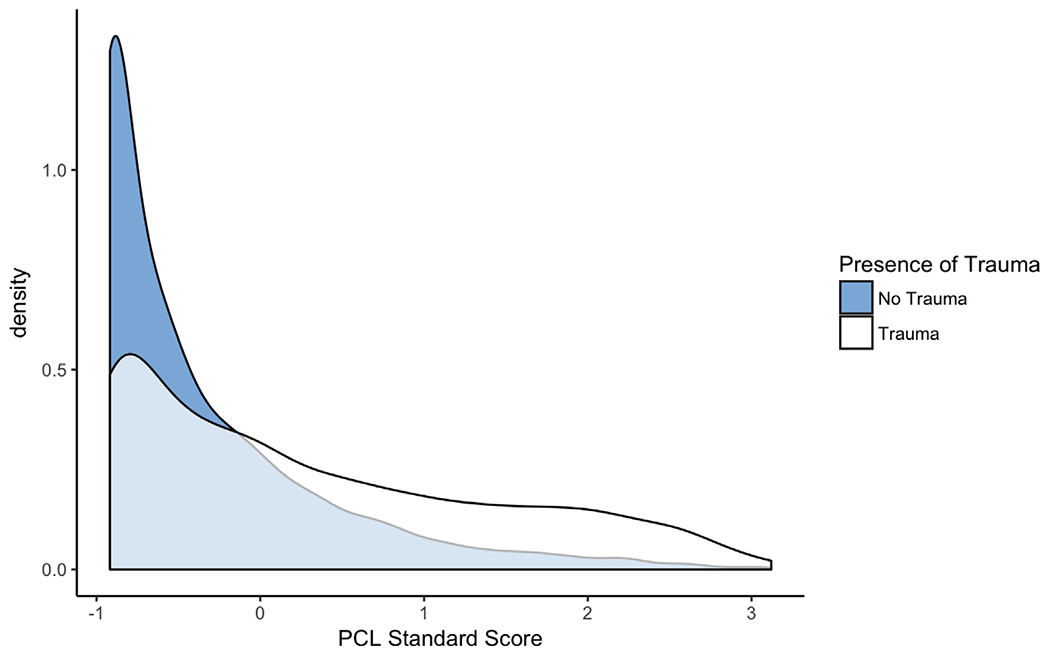
Density plot of log-transformed PTSD Checklist (PCL) standard scores for individuals with and without trauma in the full sample.
Correlations between PCL total score and MPQ total and subscales across trauma status are presented in Table 2 for the full sample and the chronic pain subsample. The correlations for the full sample (r’s = .48–.62, P < .001), as well as for individuals within the full sample with a history of trauma (r’s = .48–0.62, P < .001) were strong and positive. In those without a history of trauma the correlations were slightly lower yet remained significant (r’s = .39–.54, P < .001). While the correlations differed between the trauma and no trauma group of the full sample, this decrease was small and not meaningful suggesting that a history of Criterion A trauma had little influence on the association between PCL total score and MPQ scores. The correlations for the chronic pain subsample (r’s = .41–.60, P < .001), as well as for individuals with chronic pain and a history of trauma (r’s = .42–.59, P < .001) were strong and positive, but slightly lower than in the full sample. The correlations were more modest yet remained significant (r’s = .30–.54, P < .001) in individuals with chronic pain but without a history of trauma. Similarly, the decrease in correlations was small and trauma history made little contribution to the association between PCL and MPQ scores.
Table 2.
Correlations Between PCL Total Score and MPQ and Significance of Interaction Between Trauma and PCL Symptoms, Controlling for Age
|
All (N = 5,703)
|
Trauma (N = 3,015)
|
No Trauma (N =2,688)
|
Interaction of PCL-T and Trauma History
|
|||||
|---|---|---|---|---|---|---|---|---|
| R | P | R | P | R | P | β | P | |
| Full sample | ||||||||
| MPQ-Total | .60 | <.001 | .60 | <.001 | .50 | <.001 | −.05 | <.05 |
| Sensory | .56 | <.001 | .57 | <.001 | .46 | <.001 | −.04 | .16 |
| Affective | .62 | <.001 | .62 | <.001 | .54 | <.001 | .04 | .07 |
| VAS | .49 | <.001 | .49 | <.001 | .40 | <.001 | −.08 | <.01 |
| PPI | .48 | <.001 | .48 | <.001 | .39 | <.001 | −.07 | <.01 |
|
| ||||||||
| Chronic pain subsample | ||||||||
| MPQ-Total | .56 | <.001 | .56 | <.001 | .45 | <.001 | −.02 | .68 |
| Sensory | .51 | <.001 | .52 | <.001 | .40 | <.001 | .00 | .99 |
| Affective | .60 | <.001 | .59 | <.001 | .54 | <.001 | .00 | .93 |
| VAS | .41 | <.001 | .42 | <.001 | .32 | <.001 | −.02 | .65 |
| PPI | .42 | <.001 | .42 | <.001 | .30 | <.001 | .02 | .68 |
Abbreviations: PCL-T, PTSD Checklist total score; MPQ-Total, Short Form McGill Pain Questionnaire total score; VAS, MPQ Visual Analogue Scale; PPI, MPQ Present Pain Intensity; r, Pearson product moment correlation coefficient; β, standardized regression coefficient (beta weight); P, probability value.
Using mixed-effects regression models, we evaluated the interaction of trauma with PCL total score for each of the MPQ scales. There was no significant interaction between trauma and MPQ total score (Fig 2A). Interactions were significant for VAS (P < .01), and PPI (P = .01), suggesting that the relationship between PCL and the MPQ visual analog scale and Present Pain Intensity scales varied across presence of trauma (see Fig 2B and C) though these differences were exceedingly small. Participants with a reported history of trauma endorsed more VAS and PPI symptoms at lower levels of the PCL but the difference in reported pain between individuals with and without a reported history of trauma was no longer present at higher levels of PCL symptoms. None of the interactions of trauma with PCL total score for the MPQ scales were significant in the chronic pain subsample, suggesting that in individuals with chronic pain conditions, the association between PCL and MPQ scales does not vary across history of trauma.
Figure 2.
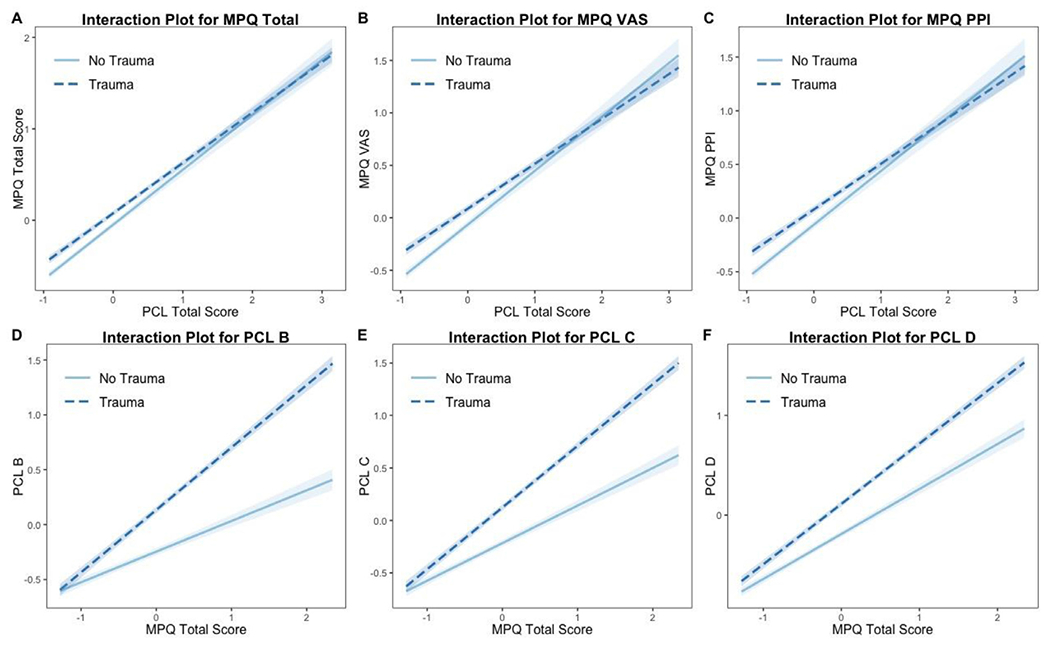
Interaction plots and 95% confidence intervals for full sample. Models controlled for age and correlated nature of the twin data. Presented for significant interaction only (P ≤ .05). MPQ-Total, Short Form McGill Pain Questionnaire total score; MPQ VAS, MPQ Visual Analogue Scale; MPQ PPI, MPQ Present Pain Intensity; PCL-Total, PTSD checklist total score; PCL-B, PTSD re-experiencing; PCL-C, PTSD avoidance; PCL-D, PTSD arousal.
Correlations between MPQ Total score and PCL symptom clusters across trauma status are presented in Table 3 for the full sample and the chronic pain subsample. Within the full sample, the largest association was between MPQ Total score and PCL Arousal symptoms (r = .60, P < .001) and the smallest was between MPQ Total score and PCL re-experiencing symptoms (r = .51, P < .001). The correlations for those with and without trauma also were significant (P’s < .001) with a similar pattern such that the strongest associations were between MPQ Total score and Arousal symptoms, and the smallest for MPQ Total score and re-experiencing symptoms. All correlations were significantly different (<.001) between the trauma and no trauma group of the full sample. Similarly, within the chronic pain subsample, the largest association was between MPQ Total score and Arousal symptoms (r = .55, P < .001) and the smallest was between MPQ Total score and re-experiencing symptoms (r = .48, P < .001). Overall, these correlations were slightly lower than in the full sample. The correlations for those with and without trauma also were significant (P’s < .001) and followed a similar pattern, with strongest associations between MPQ Total score and Arousal symptoms, and the smallest for MPQ Total score and re-experiencing symptoms. All correlations were significantly different (<.001) between the trauma and no trauma group of the chronic pain sample.
Table 3.
Correlation Between MPQ Total Score and PCL Symptom Clusters Across Presence of Trauma, and Significance of Interaction Between Trauma and MPQ Total Score, Controlling for Age
|
All (N = 5,703)
|
Trauma (N = 3,015)
|
No Trauma (N = 2,688)
|
Interaction of PCL-T and Trauma History
|
|||||
|---|---|---|---|---|---|---|---|---|
| r | P | r | P | r | P | β | P | |
| Full sample | ||||||||
| Re-experiencing | .51 | <.001 | .53 | <.001 | .37 | <.001 | .29 | <.001 |
| Avoidance | .56 | <.001 | .57 | <.001 | .45 | <.001 | .23 | <.001 |
| Arousal | .60 | <.001 | .60 | <.001 | .51 | <.001 | .16 | <.001 |
|
| ||||||||
| Chronic pain subsample | ||||||||
| Re-experiencing | .48 | <.001 | .50 | <.001 | .33 | <.001 | .29 | <.001 |
| Avoidance | .52 | <.001 | .53 | <.001 | .42 | <.001 | .21 | <.001 |
| Arousal | .55 | <.001 | .55 | <.001 | .46 | <.001 | .14 | <.001 |
Abbreviations: MPQ-T, Short Form McGill Pain Questionnaire total score; PCL, PTSD Checklist; Re-experiencing, PCL re-experiencing symptom cluster, Avoidance, PCL Avoidance symptom cluster; Arousal, PCL Arousal symptom cluster; r, Pearson product moment correlation coefficient; β, standardized regression coefficient (beta weight); P, probability value.
All interactions between MPQ Total score and trauma history in the full sample were significant, suggesting that the relationship between MPQ and PCL symptom clusters varied across presence of trauma. Participants with a reported history of trauma reported more PCL re-experiencing (Fig 2D), Avoidance (Fig 2E), and Arousal (Fig 2F) symptoms and the association of these symptoms with pain intensity were greater in participants with trauma. As in the full sample, in the chronic pain subsample, all interactions between MPQ Total score and trauma history were significant, suggesting that the relationship between MPQ and PCL symptom clusters varied across presence of reported trauma.
Discussion
We evaluated the relationship between multiple pain indicators and PTSD-like symptoms across reported history of trauma and history of COPCs. As expected, individuals with a reported history of Criterion A trauma reported more PTSD-like symptoms and a higher level of pain symptoms, with the highest level of symptoms reported by those with a history of trauma and COPCs. Interaction analyses showed that some aspects of the relationship between pain intensity and PTSD-like symptoms varied across history of trauma in the full sample, and the chronic pain subsample. In line with previous research,6,18 our results revealed a robust association between multiple indicators of pain and PTSD-like symptoms. While attenuated, the relationship between pain indicators and PTSD-like symptoms remained strong and significant for individuals with no reported Criterion A trauma history within the full sample and the chronic pain subsample, suggesting that the relationship between pain indicators and PTSD-like symptoms may not exclusively depend on a history of traumatic experiences. Similarly, the association between overall pain intensity and PTSD-like symptom clusters remained significant even in the absence of reported Criterion A trauma in both, the full and the chronic pain subsample, suggesting that while both conditions may be initiated or exacerbated by traumatic events, these seem neither necessary nor sufficient to the development of pain or the PTSD-like symptoms and may be triggered by stressful life events.
As hypothesized, we found that the pain and PTSD-like symptoms relationship was maintained independent of reported Criterion A trauma history. Our results are in line with previous studies including a cross-sectional study showing that combat injury and PTSD were independent predictors of headache in 308 Iraq and Afghanistan Veterans,1 as well as a more recent cross-sectional study of 202 chronic pain patients showing that PTSD symptoms partially mediated the relationship between trauma exposure and multiple indicators of pain severity.37 Another recent study found that physical symptoms including pain were prospectively related to PTSD symptoms in Veterans returning from deployment, even without a traumatic physical injury.36 Together, these findings suggest that the association between pain indicators and PTSD-like symptoms is not contingent on Criterion A exposure. It is also important to note that the attenuation of associations across trauma status may be due to the reduced variability of PTSD-like symptoms in the trauma group, which is likely to decrease the strength of associations with pain indicators in these individuals. This reduction in variability may be the sole source of differences between the trauma and no-trauma groups in our results and lends further support that the relationship between PTSD-like symptoms and pain is likely independent of Criterion A history. Given the experience of trauma is subjective, a variety of stressful life events may be perceived as traumatic and potentially serve as triggers for the development of both sets of symptoms in someone with other existing vulnerability.31,33,50,52 Therefore, it is possible that the pain and PTSD-like symptoms may occur after stressful life events and not just criterion A trauma.
Our results also showed that some of the interplay between pain intensity and PTSD-like symptoms varied across history of trauma in the full sample, and the chronic pain subsample, but that these differences were small. The interaction between PTSD-like symptoms and trauma history were significant but small for the MPQ total score and the current pain ratings and not for the affective or the sensory symptoms, which evaluated the specific aspects of the pain experience. Within the chronic pain subsample, none of the interaction terms between PTSD-like symptoms and trauma history were significant, suggesting that in those with chronic pain conditions, the relationship between pain intensity and PTSD-like symptoms did not vary across history of trauma. This attenuation in the chronic pain sample could be due to the decreased range of pain intensity scores and PTSD-like symptom scores in individuals with chronic pain. Evaluation of the interaction of trauma and pain intensity total scores however, revealed that the relationship between the total pain intensity scores and PTSD-like symptom clusters (B, C, D) did vary across trauma exposure in the full sample as well as in the chronic pain subsample. Taken together, these results show that the effect of PTSD-like symptoms on pain intensity scales does not vary in a meaningful way across trauma and that relationship between pain intensity and PTSD-like symptoms is largely independent of trauma history as defined by Criterion A.
The finding that trauma did not moderate the relationship between PTSD-like symptoms and some of the pain intensity symptoms may also reflect the fact that Veterans in the trauma group reported trauma consistent with Criterion A, while Veterans in the nontrauma group most likely experienced a significant stressful life event that results in PTSD-like symptoms. As a result, our findings suggest that the relationship between PTSD-like symptoms and pain is maintained both in the context of trauma or events that are sufficiently stressful to cause PTSD-like symptoms, in the absence of Criterion A traumatic events. Because the trauma evaluated in this study could have occurred at any time (pre, during, or post deployment) we are not able to directly evaluate the trajectory of the trauma-pain relationship. It is worth noting, however, that the current relationship between PTSD-like symptoms and pain intensity symptoms may have endured because of trauma occurring many decades prior in combat. Even though the association between PTSD-like symptoms and pain intensity was maintained in the absence of trauma, trauma does appear to make some contribution to the overall relationship between PTSD-like symptoms and measures of pain intensity. Future research should continue to examine the different qualities of the pain experience and its association with psychopathology, and the role of traumatic experiences on this relationship.
Our results also demonstrate that endorsement of PTSD-like symptoms can occur in the absence of Criterion A trauma history required for a diagnosis of PTSD. Furthermore, symptoms comprising the 3 PTSD symptom clusters, including re-experiencing and avoidance symptoms, were present in individuals with and without Criterion A, and the association between these PTSD-like symptoms and pain indicators was robust and maintained across all 3 clusters. The PCL assesses PTSD symptom information from a potentially wide range of stressful life experiences. Thus, re-experiencing symptoms (eg, intrusive memories, feelings) of PTSD are presented in the context of “stressful experiences” rather than Criterion A trauma as are several of the PCL items targeting PTSD avoidance symptoms (eg, avoiding thinking or talking about stressful experience or specific activities). The remaining avoidance items (eg, emotional numbing, social isolation), and arousal items (eg, irritability, jumpiness) of the PCL are presented without reference to stressful experiences and may represent a measure of general distress including sleep difficulty, anger, irritability, difficulty concentrating, alertness, and jumpiness. While hyperarousal and avoidance symptoms are shared by other anxiety disorders, re-experiencing symptoms are unique to PTSD. Our finding suggests that the association between pain indicators and PTSD-like symptoms is likely not limited only to symptoms characterized by general distress, such as social isolation or irritability, but may instead reflect the emergence of key PTSD-like symptoms in response to stressful life events and less-severe traumatic experiences.
Ours is not the first study to report such findings47 and our results are consistent with Franklin et al who recently reported no difference in PCL symptom severity or clinically-indicated level of PTSD in a sample of outpatient Veterans with and without Criterion A trauma.19 Presence of PTSD symptoms without Criterion A has also been documented in civilians who reported greater symptom severity subsequent to stressful life events such as the death or illness of a loved one rather than a Criterion A trauma21 as well as a sample of women Veterans in which stressful life events were associated with both pain phenotypes and PTSD symptoms.33
What, then, are PTSD-like symptoms without trauma? What does it mean for someone to endorse items on the PCL at a level predictive of a PTSD diagnosis, without meeting Criterion A? Several possibilities emerge. First, these PTSD-like symptoms may reflect general distress independent of trauma, consistent with overall demoralization and general vulnerability to psychopathology. Additionally, it is possible that the relationship between pain intensity and PTSD-like symptoms may not result from the trauma itself, but rather reflect an association with the psychological distress characteristic of PTSD and as well as other internalizing psychopathology, such as anxiety or depression disorders. Given the fact that over half of the symptoms on the PCL make a specific reference to “stressful experiences” it is unlikely, however, that all individuals endorsing PTSD-like symptoms in the clinical range are reporting general distress. This is further supported by the presence of re-experiencing items in individuals with no Criterion A trauma suggesting that symptoms specific to PTSD were also present without life-time Criterion A trauma. Alternatively, PTSD-like symptoms in the absence of Criterion A may be symptoms consistent with a post-traumatic reaction but present in response to events that failed to meet the threshold set by Criterion A. If the latter is true, this may suggest that Criterion A is not necessary for the emergence of PTSD-like symptoms and that various stressful life events may elicit similar lasting response, as is consistent with a growing body of research.19,25,32 This does not suggest that stressful life events that do not provoke feelings of fear or threat contribute to the emergence of PTSD-like symptoms, but that individuals who react with fear, threat to survival, or horror to events below the Criterion A threshold may develop PTSD-like symptoms.
While broadening the definition of trauma further stands to erode the integrity of the diagnosis and the ability to identify posttraumatic mechanisms that differentiate PTSD from other psychopathology46,47, our current findings suggest that closer attention to the role of stressful life events in the context of both PTSD-like symptoms as well as chronic pain is warranted in both the research and clinical context. Specifically, a better understanding of whether PTSD symptoms in the absence of Criterion A trauma are conceptually distinct from PTSD symptoms in the presence of Criterion A trauma is important to clarify the relationship between trauma and PTSD-like symptoms. Research has shown that despite similar overall PTSD symptom severity, individuals with Criterion A endorse more PTSD-specific items, than those without.19 Replicating these findings in nonclinical or civilian samples would help to identify symptoms with high discriminant validity. Further research into whether individuals with PTSD symptoms with and without Criterion A trauma differ in their course, prognosis, treatment response, or outcomes and how these potential trajectories relate to the development and maintenance of chronic pain are important targets for future studies in both Veteran and civilian samples of men and women.
Our results suggest that the relationship between pain and PTSD-like symptoms extends well beyond the clinical threshold represented by a DSM PTSD diagnosis, and should be the focus of ongoing research and clinical efforts. Because psychological responses to traumatic experiences can take many forms, future studies on the association between pain and trauma should consider this relationship both in the context of general emotional disturbance and across a wider range of psychopathology, in addition to PTSD, including other mood and anxiety disorders. Given the subjective nature of trauma, a variety of stressful life events such as divorce, illness, moving, unemployment, poverty may serve as triggers for the development of both pain and PTSD-like symptoms in someone with existing vulnerability. Even without a PTSD diagnosis, these PTSD-like symptoms may make a clinically meaningful impact and assessing and treating PTSD-like symptoms among chronic pain patients, regardless of Criterion A history may encourage integrative treatments and lead to better treatment outcomes. Because individual differences may affect the individual severity of trauma sufficient for a traumatic response, future research into individual differences such as anxiety sensitivity8 as a predisposing factor contributing to the development of both chronic pain and PTSD is encouraged.
Chronic pain and PTSD share many physiological, cognitive, and behavioral characteristics. For example, both chronic pain and PTSD are characterized by biases in attention toward threatening stimuli, appraisal tendencies, heightened startle reaction, trait fear,44 hypervigilance, emotional numbing, avoidance,51 and stress response dysregulation8 suggesting that the 2 conditions share similar features. Negative affect and anxiety vulnerability have also been linked to chronic pain conditions and PTSD,16,27,44 suggesting that differences in personality features that predispose individuals to chronic pain and PTSD symptoms may be partially responsible for their comorbidity.12 The role of acute central sensitization, a heightened response in neurons and circuits in nociceptive pathways, has also been proposed as mediating links between pain and PTSD.42 Furthermore, findings from imaging studies have independently established connections between chronic pain and PTSD with activity in the hypothalamic-pituitary-adrenal axis, the amygdala,17,26 as well as structural and functional alterations in the anterior cingulate cortex, a brain region involved in attention and emotion.13,28,56
This study had several limitations. The use of self-report data for pain intensity and PTSD-like symptom burden assessment may have led to underreporting of symptoms. Despite this, overall prevalence and correlations are consistent with previous studies suggesting that our data are representative.14 Additionally, our results are based on symptoms measures and self-reported physician diagnosis of COPCs which may not adequately capture their chronicity, or the length of time someone has had the condition. Research involving the history and duration of chronic pain may be beneficial. While the total sample and the chronic pain subsample did overlap, constructing our groups in this way allowed us to evaluate the impact of COPCs on the relationship between PCL and MPQ. Future research should examine these associations in participants meeting the diagnostic criteria for chronic pain conditions and PTSD and fully examine the potential confounding role of other internalizing disorders such as major depression. Given that we were specifically interested in any history of trauma, we did not examine the impact of multiple traumatic events or types of trauma exposure. It is worth noting that the restricted variability of PCL scores in individuals without a history of Criterion A trauma may account for the reductions in the correlations we report between PCL and MPQ scores rather than any meaningful contribution of trauma history to the relationship. Additional research to examine the potential impact of types and quantity of traumatic and stressful life events on the relationship between pain and PTSD could further our understanding of the pain-PTSD interplay.
Our sample consisted of male Veteran participants, and future research should expand these findings to women, evaluate these relationships in female combat Veterans, as well as representative community samples. Although chronic pain and PTSD are more prevalent in women, they are nonetheless highly prevalent and problematic in men, making the current evaluation important in improving our understanding of their relationship. Our overall sample contained individuals with chronic pain conditions and allowed our results to remain more generalizable than a chronic pain-free sample. The current study does not account for predisposing factors that may contribute to the development of either chronic pain or PTSD and prospective studies evaluating participants prior to trauma exposure may further elucidate the pain, trauma, and PTSD symptom interplay. Studies evaluating predeployment health in Veterans, for example, would be well-equipped to address this important question. Despite these limitations, this study substantially extends the work to date by specifically examining the role of trauma on the association between pain and PTSD-like symptoms.
Future research incorporating both chronic pain and PTSD together would be of great benefit. Using several of these measures collectively may represent an endophenotype for vulnerability for maladaptive stress response which may be expressed in either a physical chronic pain or anxiety and stress-related disorders such as PTSD. Similarly, the role of diverse types of traumatic and stressful experiences (for example, with and without physical injury) may further clarify the relationship between chronic pain, trauma, and PTSD. Finally, exploring these experiences in longitudinal samples to investigate temporal progression of these conditions and establish the chronicity of pain, is important to understanding of their interplay across the lifespan.
In summary, our findings suggest that while a reported history of Criterion A trauma may increase the presentation of both pain indicators and PTSD symptoms, the association between pain and PTSD-like symptoms is largely independent of Criterion A trauma. Future research should evaluate the relationship between pain and trauma across a wider range of psychopathology, including, but not limited to PTSD. Because of the complicated interplay between pain, psychopathology, and trauma, clinical intervention aimed at evaluating and addressing both physical and emotional distress in chronic pain patients is important in improving patient outcomes.
Perspective:
This article demonstrates that the relationship between PTSD-like symptoms and indicators of pain is largely independent of trauma consistent with Criterion A. This finding highlights the need to better understand and address stressful life events in chronic pain patients and pain concerns in individuals reporting trauma.
Acknowledgments
Funding for the MAPP Research Network was obtained under a cooperative agreement from National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institutes of Health (NIH) (U01 DK082325). The Cooperative Studies Program of the Office of Research and Development, Clinical Science Research and Development, of the United States Department of Veterans Affairs provided financial support for Cooperative Study #569 and the development and maintenance of the Vietnam Era Twin (VET) Registry. Dr. Gasperi is funded by VA Career Development Award #1IK2CX002107 from the U.S. Department of Veterans Affairs Clinical Science Research and Development Service. Dr. Panizzon was supported in part by National Institute on Aging K08 AG047903 and R01 AG05064. Dr. Suri is a Staff Physician at the VA Puget Sound Health Care System in Seattle, Washington. The participation of Dr. Suri in this study was funded by VA Puget Sound Health Care System. Dr. Suri is funded by VA Career Development Award # 1IK2RX001515 from the U.S. Department of Veterans Affairs Rehabilitation Research and Development Service. The authors gratefully acknowledge the continued cooperation and participation of the members of the VET Registry; without their contribution, this research would not have been possible. The authors would like to thank the reviewers for their advice and comments. The views expressed in this paper are those of the authors and do not reflect the official policy or position of NIDDK, Department of Veterans Affairs, the United States Government, or any institution with which the authors are affiliated.
Footnotes
The authors have no conflict of interest to declare.
References
- 1.Afari N, Harder LH, Madra NJ, Heppner PS, Moeller-Bertram T, King C, Baker DG: PTSD, combat injury, and headache in veterans returning from Iraq/Afghanistan. Headache J Head Face Pain 49:1267–1276, 2009 [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 3rd ed. Washington, DC, Author, 1987 [Google Scholar]
- 3.American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, Author, 1994 [Google Scholar]
- 4.American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, Author, 2000 [Google Scholar]
- 5.American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Washington, DC, Author, 2013 [Google Scholar]
- 6.Arguelles LM, Afari N, Buchwald DS, Clauw DJ, Furner S, Goldberg J: A twin study of posttraumatic stress disorder symptoms and chronic widespread pain. Pain 124:150–157, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Asmundson GJ: The emotional and physical pains of trauma: Contemporary and innovative approaches for treating co-occurring PTSD and chronic pain. Depress Anxiety. 31:717–720, 2014 [DOI] [PubMed] [Google Scholar]
- 8.Asmundson GJ, Coons MJ, Taylor S, Katz J: PTSD and the experience of pain: Research and clinical implications of shared vulnerability and mutual maintenance models. Can J Psychiatry 47:930–937, 2002 [DOI] [PubMed] [Google Scholar]
- 9.Asmundson GJ, Katz J: Understanding the co-occurrence of anxiety disorders and chronic pain: State-of-the-art. Depress Anxiety. 26:888–901, 2009 [DOI] [PubMed] [Google Scholar]
- 10.Ballantyne JC, Sullivan MD: Intensity of chronic pain—the wrong metric? N Engl J Med. 373:2098–2099, 2015 [DOI] [PubMed] [Google Scholar]
- 11.Bates D, Mächler M, Bolker B, Walker S: Fitting linear mixed-effects models using lme4. J Stat Softw. 67:1–48, 2015 [Google Scholar]
- 12.Beckham JC, Crawford AL, Feldman ME, Kirby AC, Hertzberg MA, Davidson J, Moore SD: Chronic posttraumatic stress disorder and chronic pain in Vietnam combat veterans. J Psychosom Res. 43:379–389, 1997 [DOI] [PubMed] [Google Scholar]
- 13.Bliss TV, Collingridge GL, Kaang B-K, Zhuo M: Synaptic plasticity in the anterior cingulate cortex in acute and chronic pain. Nat Rev Neurosci. 17:485–496, 2016 [DOI] [PubMed] [Google Scholar]
- 14.Brennstuhl MJ, Tarquinio C, Montel S: Chronic pain and PTSD: Evolving views on their comorbidity. Perspect Psychiatr Care 51:295–304, 2015 [DOI] [PubMed] [Google Scholar]
- 15.Cohen J: Statistical Power Analysis for the Behavioral Sciences, 2nd ed. Hillside, NJ, Lawrence Erlbaum Associates, 1988 [Google Scholar]
- 16.Cottam WJ, Condon L, Alshuft H, Reckziegel D, Auer DP: Associations of limbic-affective brain activity and severity of ongoing chronic arthritis pain are explained by trait anxiety. NeuroImage: Clin 12:269–276, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Etkin A, Wager TD: Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry. 164:1476–1488, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fishbain DA, Pulikal A, Lewis JE, Gao J: Chronic pain types differ in their reported prevalence of post-traumatic stress disorder (PTSD) and there is consistent evidence that chronic pain is associated with PTSD: An evidence-based structured systematic review. Pain Med 18:711–735, 2017 [DOI] [PubMed] [Google Scholar]
- 19.Franklin CL, Raines AM, Hurlocker MC: No trauma, no problem: Symptoms of posttraumatic stress in the absence of a criterion a stressor. J Psychopathol Behav Assess. 41:107–111, 2019 [Google Scholar]
- 20.Gasperi M, Panizzon M, Goldberg J, Buchwald D, Afari N: Posttraumatic stress disorder and chronic pain conditions in men: A Twin Study. Psychosom Med. 83:109–117, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gold SD, Marx BP, Soler-Baillo JM, Sloan DM: Is life stress more traumatic than traumatic stress? J Anxiety Disord. 19:687–698, 2005 [DOI] [PubMed] [Google Scholar]
- 22.Goldberg DS, McGee SJ: Pain as a global public health priority. BMC Public Health 11:770–774, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goldberg J, Curran B, Vitek ME, Henderson WG, Boyko EJ: The Vietnam era twin registry. Twin Res 5:476–481, 2002 [DOI] [PubMed] [Google Scholar]
- 24.Goldstein RB, Smith SM, Chou SP, Saha TD, Jung J, Zhang H, Pickering RP, Ruan WJ, Huang B, Grant BF: The epidemiology of DSM-5 posttraumatic stress disorder in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Soc Psychiatry Psychiatr Epidemiol. 51:1137–1148, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hyland P, Karatzias T, Shevlin M, McElroy E, Ben-Ezra M, Cloitre M, Brewin CR: Does requiring trauma exposure affect rates of ICD-11 PTSD and complex PTSD? Implications for DSM-5. Psychological Trauma: Theory, Research, Practice, and Policy ; 13:133–141, 2021 [DOI] [PubMed] [Google Scholar]
- 26.Jiang Y, Oathes D, Hush J, Darnall B, Charvat M, Mackey S, Etkin A: Perturbed connectivity of the amygdala and its subregions with the central executive and default mode networks in chronic pain. Pain 157:1970–1978, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kain ZN, Mayes LC, Caldwell-Andrews AA, Karas DE, McClain BC: Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing surgery. Pediatrics 118:651–658, 2006 [DOI] [PubMed] [Google Scholar]
- 28.Kennis M, Rademaker AR, van Rooij SJ, Kahn RS, Geuze E: Resting state functional connectivity of the anterior cingulate cortex in veterans with and without post-traumatic stress disorder. Hum Brain Mapp. 36:99–109, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kessler RC, Üstün TB: The world mental health (WMH) survey initiative version of the world health organization (WHO) composite international diagnostic interview (CIDI). Int J Methods Psychiatr Res. 13:93–121, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kessler RC, Wang PS: The descriptive epidemiology of commonly occurring mental disorders in the United States. Annu Rev Public Health. 29:115–129, 2008 [DOI] [PubMed] [Google Scholar]
- 31.Lampe A, Doering S, Rumpold G, Sölder E, Krismer M, Kantner-Rumplmair W, Schubert C, Söllner W: Chronic pain syndromes and their relation to childhood abuse and stressful life events. J Psychosom Res. 54:361–367, 2003 [DOI] [PubMed] [Google Scholar]
- 32.Larsen SE, Berenbaum H: Did the DSM-5 improve the traumatic stressor criterion?: Association of DSM-IV and DSM-5 criterion a with posttraumatic stress disorder symptoms. Psychopathology 50:373–378, 2017 [DOI] [PubMed] [Google Scholar]
- 33.Lehavot K, Goldberg SB, Chen JA, Katon JG, Glass JE, Fortney JC, Simpson TL, Schnurr PP: Do trauma type, stressful life events, and social support explain women veterans’ high prevalence of PTSD? Soc Psychiatry Psychiatr Epidemiol. 53:943–953, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Magruder K, Yeager D, Goldberg J, Forsberg C, Litz B, Vaccarino V, Friedman M, Gleason T, Huang G, Smith N: Diagnostic performance of the PTSD checklist and the Vietnam Era Twin Registry PTSD scale. Epidemiol Psychiatr Sci. 24:415–422, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maixner W, Fillingim RB, Williams DA, Smith SB, Slade GD: Overlapping chronic pain conditions: implications for diagnosis and classification. J Pain. 17:T93–T107, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McAndrew LM, Lu S-E, Phillips LA, Maestro K, Quigley KS: Mutual maintenance of PTSD and physical symptoms for Veterans returning from deployment. Eur J Psychotraumatol. 10:1608717, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McKernan LC, Johnson BN, Reynolds WS, Williams DA, Cheavens JS, Dmochowski RR, Crofford LJ: Posttraumatic stress disorder in interstitial cystitis/bladder pain syndrome: Relationship to patient phenotype and clinical practice implications. Neurourol Urodyn. 38:353–362, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McNally RJ: Progress and controversy in the study of posttraumatic stress disorder. Annu Rev Psychol. 54:229–252, 2003 [DOI] [PubMed] [Google Scholar]
- 39.Melzack R: The McGill Pain Questionnaire: major properties and scoring methods. Pain 1:277–299, 1975 [DOI] [PubMed] [Google Scholar]
- 40.Melzack R: The short-form McGill pain questionnaire. Pain 30:191–197, 1987 [DOI] [PubMed] [Google Scholar]
- 41.Melzack R, Katz J, Turk DC: The McGill Pain Questionnaire: Appraisal and Current Status, Handbook of Pain Assessment. 2nd New York, NY, Guilford Press, 2001, pp 35–52 [Google Scholar]
- 42.Moeller-Bertram T, Strigo IA, Simmons AN, Schilling JM, Patel P, Baker DG: Evidence for acute central sensitization to prolonged experimental pain in posttraumatic stress disorder. Pain Med 15:762–771, 2014 [DOI] [PubMed] [Google Scholar]
- 43.Otis JD, Keane TM, Kerns RD: An examination of the relationship between chronic pain and post-traumatic stress disorder. J Rehabil Res Dev. 40:397–406, 2003 [DOI] [PubMed] [Google Scholar]
- 44.Ploghaus A, Narain C, Beckmann CF, Clare S, Bantick S, Wise R, Matthews PM, Rawlins JNP, Tracey I: Exacerbation of pain by anxiety is associated with activity in a hippocampal network. J Neurosci. 21:9896–9903, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.R Core Team: R: A Language and Environment for Statistical Computing. Vienna, Austria, R Foundation for Statistical Computing, 2018 [Google Scholar]
- 46.Rosen GM: Traumatic events, criterion creep, and the creation of pretraumatic stress disorder. Sci Rev Mental Health Pract 3:39–42, 2004 [Google Scholar]
- 47.Rosen GM, Lilienfeld SO: Posttraumatic stress disorder: An empirical evaluation of core assumptions. Clin Psychol Rev. 28:837–868, 2008 [DOI] [PubMed] [Google Scholar]
- 48.Sharp TJ, Harvey AG: Chronic pain and posttraumatic stress disorder: Mutual maintenance? Clin Psychol Rev. 21:857–877, 2001 [DOI] [PubMed] [Google Scholar]
- 49.Tsai M, Mori AM, Forsberg CW, Waiss N, Sporleder JL, Smith NL, Goldberg J: The Vietnam Era Twin Registry: a quarter century of progress. Twin Res Hum Genet 16:429–436, 2013 [DOI] [PubMed] [Google Scholar]
- 50.Vilela FC, Vieira JS, Giusti-Paiva A, da Silva ML: Experiencing early life maternal separation increases pain sensitivity in adult offspring. Int J Dev Neurosci. 62:8–14, 2017 [DOI] [PubMed] [Google Scholar]
- 51.Vlaeyen JW, Linton SJ: Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain 85:317–332, 2000 [DOI] [PubMed] [Google Scholar]
- 52.Wager J, Brehmer H, Hirschfeld G, Zernikow B: Psychological distress and stressful life events in pediatric complex regional pain syndrome. Pain Res Manage. 20:189–194, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Weathers F, Litz B, Herman D, Huska J, Keane T: The PTSD Checklist: Reliability, validity and diagnostic utility. in Paper Presented at the Annual Meeting of the International Society for Traumatic Stress Studies, San Antonio, TX; 1993 [Google Scholar]
- 54.Weathers FW, Ford J: Psychometric properties of the PTSD Checklist (PCL-C, PCL-S, PCL-M, PCL-PR). Meas Stress Trauma Adapt 34:250–252, 1996 [Google Scholar]
- 55.Yeager DE, Magruder KM, Knapp RG, Nicholas JS, Frueh BC: Performance characteristics of the posttraumatic stress disorder checklist and SPAN in Veterans Affairs primary care settings. Gen Hosp Psychiatry. 29:294–301, 2007 [DOI] [PubMed] [Google Scholar]
- 56.Yoshino A, Okamoto Y, Onoda K, Yoshimura S, Kunisato Y, Demoto Y, Okada G, Yamawaki S: Sadness enhances the experience of pain via neural activation in the anterior cingulate cortex and amygdala: An fMRI study. Neuroimage 50:1194–1201, 2010 [DOI] [PubMed] [Google Scholar]


