Abstract
Although posttraumatic stress disorder (PTSD) is associated with negative family outcomes, including parenting challenges, little is known about the biological and emotional processes that might underlie this association. The present project addressed this gap by examining associations between maternal PTSD and parenting behaviors in a lab setting. We expected that PTSD would be associated with more ineffective parenting behaviors, and that negative emotion and cortisol reactivity would mediate this relation. A total of 78 mothers and their toddler-aged children completed a task designed to elicit parental responses to typical instances of child misbehavior. Salivary cortisol was collected from mothers prior and subsequent to the lab paradigm and mothers provided ratings of their experienced emotion while viewing a video of the interaction. Contrary to hypotheses, cortisol reactivity did not mediate associations between PTSD and parenting. However, findings suggest that PTSD is associated with greater permissive parenting behaviors, and mothers with even subthreshold symptoms of PTSD may experience more negative emotion during challenging parent-child interactions that ultimately interferes with parenting. Mothers with PTSD may benefit from interventions that focus on modifying the intensity of their negative emotions in the context of child misbehavior to more effectively set limits in everyday discipline encounters.
Keywords: Posttraumatic Stress Disorder, parenting, emotional reactivity, cortisol reactivity, observational
Psychopathology of various types has been linked to increases in parental negativity and ineffective parenting behaviors (see Berg-Nielsen et al., 2002 for a review). Within the broader realm of psychopathology, posttraumatic stress disorder (PTSD) might pose particularly unique challenges to parenting (see Christie et al., 2019 for a review). PTSD is characterized by a persistent sense of current threat that results in experiential, emotional, and behavioral avoidance patterns as individuals attempt to limit their exposure to evocative cues (American Psychiatric Association [APA], 2013). However, interactions with young children often involve challenging encounters that require parents to manage their own reactions in service of their child’s wellbeing. In such situations, trauma symptoms characterized by alterations in arousal and reactivity (i.e., hyperarousal) may impinge upon a parent’s ability to use sensitivity when interacting with their children, resulting in more frequent outbursts of negative emotion (i.e., harsh/overreactive parenting). In line with this possibility, research demonstrates that PTSD severity among parents is positively associated with observed harsh/overreactive interactions with young children (e.g., Ammerman et al., 2012; van Ee et al., 2012). Alternatively, symptoms reflecting emotional avoidance and numbing (characteristic of negative alterations in cognitions and moods associated with PTSD) may influence a parent who is easily overwhelmed by a child’s misbehavior to respond by “giving in” to the child’s demand to avoid conflict (i.e., lax/permissive parenting). In support of this proposition, a history of childhood maltreatment has been linked with permissive parenting styles among parents of young children and adolescents (DiLillo & Damshek, 2003; Jaffe et al., 2012), though conflicting findings exist (Schwerdtfeger et al., 2013). Yet we are aware of no published study using observational methods to examine whether PTSD is associated with lax/permissive behaviors among parents of young children. This is a notable gap given that the discrepancy between self-report and observational measures of negative parenting may be wider among parents reporting higher distress (Herbers et al., 2017). Additionally, if PTSD has the potential to interfere with effective parenting behaviors, then an important next step is to examine factors that may account for this association. Understanding biological and emotional processes facilitating this association may reveal important processes that can be targeted through interventions to improve parenting behaviors of trauma-exposed mothers.
Models of Stress Reactivity
The stress response system (SRS) – comprised of the parasympathetic and sympathetic system, as well as the hypothalamic pituitary adrenal (HPA) axis – is responsible for helping individuals maintain physiological and behavioral homeostasis in the context of challenge, and may be altered by experiences of trauma and adversity (Boyce & Ellis, 2005). Changes in this system brought on by PTSD may increase risk for maladaptive parenting behaviors, particularly during challenging parent-child interactions. According to the Adaptive Calibration Model (ACM; Del Giudice et al., 2011), two patterns of stress responsivity typically occur following exposure to trauma and adversity: (a) vigilant, which is marked by heightened stress reactivity and heightened negative mood, and (b) unemotional, which is marked by low physiological stress and lack of affective responsivity to psychosocial stressors. The ACM emphasizes that whether a given individual displays vigilant or unemotional stress response patterns depends in part on the adaptability of the responses to a given interaction. For example, in the context of true danger, vigilant responses, characterized by emotional reactivity and swift activation of the fight or flight system, are likely adaptive for coping with uncontrollable threats. Unemotional responses may also be adaptive in that lower emotionality may reduce vulnerability and promote strength in the context of more unforgiving environments.
Although parent-child discipline encounters typically lack the possibility of true danger, they nonetheless require that parents manage largely uncontrollable and potentially aversive child noncompliance. Applying the ACM model to the case of trauma, we propose that parents with PTSD may be more likely to perceive discipline encounters as challenging, resulting in activation of the SRS. Indeed, a robust literature demonstrates that attentional biases toward threat-related information is a primary feature of PTSD (e.g., Vythilingam et al., 2007). Further, in a recent extension of the Cognitive-Behavioral Interpersonal Theory of PTSD (Dekel & Monson, 2012), Creech and Misca (2017) theorize that attentional biases toward threat may stimulate more biased cognitions among parents, as well as negative emotions related to parenting, which in turn has cascading effects on parent-child interaction. Thus, supported by ample evidence that both emotional and physiological factors have a major effect on parental behaviors more broadly (e.g., Dix, 1991; Gonzales et al., 2012), here, we examine two biological and emotional processes —in vivo emotional and physiological reactivity—through which PTSD may negatively impact parenting behaviors.
Experienced Emotion
During interactions with young children, particularly toddlers, mothers attempting to manage child misbehavior that is out of their control may experience intense negative emotions (Dix, 1991). Frequency and intensity of these emotions, in turn, may potentiate or inhibit certain parenting behaviors in an attempt to maintain or change toddler behavior (Dix, 1991; Lorber & O’Leary, 2005). Research consistently supports broad linkages between negative emotions and hostile parenting across child development (Rueger et al., 2011), and observations of mother-child interactions reveal that mothers who experience greater negative emotion are more likely to engage in harsh/overreactive (Arnold & O’Leary, 1995) and lax/permissive discipline behaviors with their toddler-aged children (Lorber, 2007).
A separate but related literature also suggests that maternal PTSD may lead to strong negative emotional responses during challenging parent-child interactions. PTSD is associated with higher trait negative affect (Finucane et al., 2012), as well as more intense subjective reactions to emotionally evocative situations (Orsillo et al., 2004). Because discipline encounters can generate negative emotions (Dix, 1991), the redirection of attention toward the management of one’s own emotional distress among individuals with PTSD may contribute to maladaptive parenting behaviors. Specifically, mothers with PTSD may engage with children in a more hostile manner in an attempt to suppress emotionally aversive child behavior quickly, or “give in” to their child in an attempt to spare themselves of the experience of negative emotion.
Cortisol Reactivity
Physiological responses of mothers during discipline encounters represent a second pathway through which PTSD may affect parenting behaviors. In particular, abundant research demonstrates that individuals with PTSD do not experience the usual habituation of cortisol response in the face of stress (see Morris et al., 2012 for a review). Specifically, whereas cortisol release usually terminates once a stressor has passed, frequent perceptions of threat are associated with prolonged activation of the cortisol stress response and greater cortisol release among trauma survivors. Over time, however, trauma-induced elevations in cortisol appear to downregulate HPA functioning, resulting in lower cortisol release to protect brain structures from adverse effects associated with prolonged exposure to cortisol (Yehuda, 2002). Accordingly, a large number of studies support linkages between exposure to adversity and autonomic hyperreactivity, while a similarly sized body of research supports associations between exposure to trauma and hyporeactivity (see Del Giudice et al., 2011). The majority of research to date has examined alterations in daily cortisol levels among trauma-exposed samples (Morris et al., 2012); however, there is also evidence to suggest that trauma-exposed samples demonstrate, on a moment-to-moment basis, both cortisol hyperactivity (e.g., Elzinga et al., 2003) as well as hyporeactivity (e.g., Cordero et al., 2017).
Reflecting a U-shaped function between cortisol and behavioral risk, previous research has similarly linked both high and low cortisol levels to negative parenting outcomes (e.g., Mills-Koonce et al., 2009; Juul et al., 2015). That is, mothers with both high and low cortisol levels have been found to engage in overreactive parenting and withdrawal behaviors toward infants and toddlers in the context of diverse parent-child interactions (e.g., separation stress, naturalistic interactions; Cordero et al., 2017; Juul et al., 2015; Mills-Koonce et al. 2009). For example, Mills-Koonce et al. (2009) found that higher baseline salivary cortisol among mothers was associated with more negative-intrusive caregiving behaviors during a free play interaction task. In contrast, Juul et al. (2015) found that mothers with a history of child trauma exhibited blunted cortisol reactivity, which was associated with reduced affective expression during an infant stressor paradigm. Taken together, HPA axis abnormalities have been repeatedly associated with diminished parenting quality, suggesting that cortisol dysregulation (in the form of either elevated or suppressed responding) may be associated with increases in both harsh and lax parenting among mothers with PTSD.
Does Subthreshold PTSD Matter for Parenting?
If negative emotion and cortisol dysregulation mediate relations between PTSD and parenting difficulties, a related question is whether these processes are specific to individuals meeting full DSM-5 criteria for PTSD or whether similar associations exist among parents experiencing significant but subthreshold symptoms of PTSD. Subthreshold PTSD refers to symptoms that fall short of meeting criteria for the full syndrome, yet often still result in clinically significant distress (Carlier & Gersons, 1995). Like those diagnosed with PTSD, individuals experiencing subthreshold symptoms often report psychosocial impairment in a variety of domains, including interpersonal functioning (e.g., Zlotnick et al., 2002). Such findings raise the possibility that both full and subthreshold PTSD might be associated with parenting problems via emotional reactivity and cortisol dysregulation. Though a number of approaches to categorization of subthreshold symptoms have been used (see Franklin et al., 2018), here we examine this question with a community sample of mothers identified through diagnostic interviewing as meeting criteria for full PTSD, subthreshold PTSD (i.e., two or three of the required four symptom clusters), or few to no symptoms of PTSD (i.e., one or zero of the required four symptom clusters). The empirical basis for our groupings comes from McLaughlin and colleagues (2015), who surveyed 23,936 respondents across 13 countries. Results showed that the highest distress-impairment was observed among the respondents who met full DSM-5 PTSD criteria, but that respondents meeting two or three of the DSM-5 criteria (i.e., subthreshold PTSD) also had significantly elevated scores for most adverse outcomes. This subthreshold group, in turn showed greater impairment than participants meeting only one of four DSM-5 criteria.
The Present Study
Theory and research suggest that trauma-related psychopathology may intensify emotional and biological reactions during challenging parent-child interactions, which in turn may play distinct roles in shaping in vivo parenting behaviors. Drawing on this work, our aims in the present study were to (1) investigate associations between maternal PTSD and parenting behaviors (laxness and overreactivity) during a challenging parent-child interaction, and (2) examine the role of mothers’ emotional reactivity and cortisol dysregulation (i.e., hyperreactive or hyporeactive responses) in mediating these associations. We also examined whether these associations exist for mothers with significant but subthreshold PTSD symptoms, as well as diagnosable PTSD, compared to those with few to no symptoms of PTSD. We hypothesized that, compared to mothers without diagnosable PTSD, those meeting full criteria for PTSD would demonstrate less effective parenting behaviors, as well as greater negative emotion and cortisol dysregulation. We also hypothesized that, compared to mothers with few to no PTSD symptoms, those experiencing significant but subthreshold symptoms of PTSD (or higher) would demonstrate less effective parenting behaviors, as well as greater negative emotion and cortisol dysregulation. Finally, in light of consistent findings that socioeconomic status is an important predictor of parental disciplinary styles (e.g., Bornstein & Bradley, 2014), we also investigated the potential role of income on our models.
We focus on parents of toddler-aged children in the present study because the toddler years are an important developmental period during which child noncompliance is common and associated with other problematic outcomes. For example, longitudinal research demonstrates that noncompliance during toddlerhood is relatively stable over time and predicts aggression and externalizing problems later in life (see Kalb & Loeber, 2003 for a review). Notably parental discipline, which affects child noncompliance, can be altered by parent training programs (Maughan et al., 2005), highlighting the need for additional research focused on increasing understanding of parenting behaviors among mothers of toddler-aged children (18–36 months).
Method
Participants
Participants were 78 mothers and their 18- to 36-month-old children. Mothers ranged in age from 21 to 45 (M = 32.9; SD = 5.3) and children ranged in age from 18–36 months (M = 30 months; SD = 0.3). The majority of mothers identified as White (n = 71, 91%) and non-Hispanic/Latino (n = 72; 92%); among the 78 participants, 15% (n = 12) identified with at least one racial or ethnic minority group. The modal level of education achieved was a Bachelor’s degree, and the modal combined family income was over $100,000, but variability was evident, with approximately 48% of the sample earning below the state median household income of $60,000. Additional sample demographics are located in Table 1.
Table 1.
Descriptive Statistics for Demographic Variables (N = 78)
| Variable | N or M | SD or % |
|---|---|---|
|
| ||
| Mom Age | 33.0 | 5.3 |
| Mom Race | ||
| White | 71 | 91.03% |
| Asian | 2 | 2.56% |
| Multiracial | 5 | 6.41% |
| Mom Ethnicity | ||
| Not Hispanic/Latino | 72 | 92.31% |
| Hispanic/Latino | 3 | 3.85% |
| Multiethnic | 2 | 2.56% |
| Missing | 1 | 1.28% |
| Mom Marital Status (Married) | 61 | 78.21% |
| Mom not in romantic relationship | 7 | 8.97% |
| Mom Currently Employed | 60 | 76.92% |
| Mom Highest Education | ||
| Less than High School | 1 | 1.28% |
| High School/GED | 4 | 5.13% |
| Some college | 16 | 20.51% |
| Associate’s | 7 | 8.97% |
| Bachelor’s | 37 | 47.45% |
| Master’s | 10 | 12.82% |
| Professional/Doctorate | 3 | 3.85% |
| Average Yearly Household Income | ||
| $0-$20,000 | 10 | 12.82% |
| $20,000-$40,000 | 13 | 16.67% |
| $40,000-$60,000 | 14 | 17.95% |
| $60,000-$80,000 | 13 | 16.67% |
| $80,000-$100,000 | 9 | 11.54% |
| Over $100,000 | 18 | 23.08% |
| Missing | 1 | 1.28% |
| Child Age | 30 months | 0.3 |
| Child Sex (Female) | 28 | 35.90% |
| Child Race | ||
| White | 66 | 84.62% |
| Asian | 2 | 2.56% |
| Multiracial | 10 | 12.82% |
| Child Ethnicity | ||
| Not Hispanic/Latino | 66 | 84.62% |
| Hispanic/Latino | 10 | 12.82% |
| Multiethnic | 1 | 1.28% |
| Missing | 1 | 1.28% |
Recruitment
The majority of mother-child dyads (n = 52) were recruited through publicly available birth announcements; letters were sent to mothers with children in the proposed age range. The remaining participants were recruited via flyers throughout the community (n = 16), word of mouth, (n = 4), university websites and listservs (n = 3), and Craigslist advertisements (n = 3). Exclusion criteria included the presence of Addison’s or Cushing’s disease or current pregnancy due to changes in cortisol hormones that occur under these circumstances. Mothers received $10 compensation for completing the initial online survey and $15 per hour during the lab portion for a total of up to $55. Children received a toy from a prize box.
Procedures
Prior to enrollment, all participants were screened online to assess eligibility and then followed up with by phone for scheduling. During the screening, participants completed an abridged version of the Life Events Checklist for DSM-5 (LEC-5) followed by the PTSD Checklist for DSM-5 (PCL-5; Weathers et al., 2013a) to enable oversampling for trauma exposure and PTSD. Following screening procedures, interested participants were invited to complete a 30-minute online questionnaire from home, during which they received informed consent and were then scheduled to attend a single lab visit. Participants were scheduled no earlier than 1:00PM, to limit the influence of diurnal fluctuations in cortisol levels. Upon arrival, informed consent was reviewed, and participants provided the first sample of salivary cortisol to acclimate participants to cortisol procedures; this sample was not used in data analyses. Mothers who endorsed a Criterion A event then received the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5; Weathers et al., 2013b) interview. Because responding to the CAPS-5 could potentially increase cortisol reactivity, over the next 20 minutes, mothers completed a demographics questionnaire, including items assessing possible confounders of cortisol data, and a series of self-report measures assessing parental efficacy, romantic relationship quality, emotion regulation, and alcohol use, to allow cortisol to return to baseline. Next, just prior to the parent-child interaction task, a second saliva sample was taken. Participants then completed two standardized discipline encounter tasks (Arnold & O’Leary, 1995) while being video-recorded in a room containing the appropriate set-up for the parent-child interaction. Cortisol was collected for a third time immediately following the parent-child interaction and again 20 minutes later. Finally, using procedures developed by Slep and O’Leary (1998), mothers provided emotion ratings while watching a video of their interactions with their child. Prior to leaving, all participants underwent a full debriefing about the study. The university’s Institutional Review Board approved all procedures.
Measures
Trauma exposure and PTSD diagnosis.
A trained, master’s-level clinician (the first author) administered the CAPS-5 interview to mothers who had experienced a Criterion A trauma. The CAPS-5 has demonstrated strong interrater reliability (κs ranging from .78 to 1.00), good test-retest reliability (ICC = .78), and strong convergent validity (Weathers et al., 2018). In the present study, Cronbach’s alpha across items was high (α = .92). First, the CAPS-5 was used for the classification of participants into no PTSD, subthreshold PTSD, or full PTSD groups. Mothers who did not endorse a Criterion A event, as well as those who reported a Criterion A event but met criteria for no or only one symptom cluster (intrusive memories, avoidance, negative alterations in cognitions and moods, alterations in arousal and reactivity), were coded into the no PTSD group. Consistent with prior work (e.g., McLaughlin et al., 2015), subthreshold PTSD was defined as meeting criteria on any two or three of the four symptom clusters.
To test our hypotheses that problematic parenting might exist even among mothers meeting subthreshold symptoms of PTSD, we used the above classifications to code mothers into two groups: (1) mothers with no PTSD compared to those with subthreshold or full PTSD (subthreshold cut-point), and (2) mothers with no PTSD or subthreshold PTSD compared to those with full PTSD (full PTSD cut-point). By using two cut-points, we were able to investigate whether even subthreshold PTSD is associated with impairments that warrant closer empirical and clinical attention.
Parenting behavior.
To obtain an observational measure of maternal overreactive and lax discipline, mothers-child dyads completed a standardized discipline encounter protocol developed by Arnold and O’Leary (1995). This protocol has been used in several prior studies (e.g., Lorber & O’Leary, 2005; Slep & O’Leary, 1998) and consists of two 10-minute tasks that are video recorded. During each task, mothers were asked to instruct their children not to touch an assortment of visually appealing objects (e.g., a jar of candy) placed on low tables throughout the room. In the first task, mothers gave their child a set of unattractive toys (e.g., toy fruit) and asked the child to play independently while she was on the phone with the experimenter. In the second task, mothers placed a mat and book on the floor and asked the child to rest while she completed questionnaires. Throughout these tasks the experimenter cued the mother to proceed but provided no advice on how to manage the child.
A team of three coders blinded to participant trauma history and PTSD diagnosis viewed the video interactions of mothers during the parent-child discipline encounter and coded global ratings on 7-point scales (1 = good or effective to 7 = bad or ineffective) of two maternal parenting behaviors: harshness and laxness. Harshness reflects the degree and frequency of reacting to child misbehavior in a hostile way either verbally (e.g., yelling) or behaviorally (e.g., grabbing an arm), while laxness reflects the degree and frequency of mothers’ permissive responses to child misbehavior (e.g., giving in). A global score was given for each of the two separate tasks (i.e., phone task, quiet time task) and scores from each task were subsequently averaged. Research indicates convergent validity between discipline behaviors observed during this protocol and self-report measures of overreactive (r = .61) and lax parenting behaviors (r = .65; Arnold et al., 1993), as well as high interrater reliability (Arnold & O’Leary, 1995). Research assistants attended weekly trainings until achieving ICCs of at least .70 prior to coding videos. A random sample of 25% of videos was double-coded and indicated strong inter-coder agreement (Laxness = .91, Overreactivity = .77), based on established guidelines (Cicchetti, 1994).
Experienced emotion.
Following these tasks, using procedures developed by Slep and O’Leary (1998), mothers viewed the video of their interactions with their child and made continuous ratings of the intensity of their emotional experience using a joystick. The joystick is divided into three parts, with increasing negative scores as the joystick is lowered, increasing positive scores as the joystick is raised, and neutral scores when the joystick is centered (ratings range from −500 to +500). For each 5-second interval, the average position of the dial for the time it was in the negative and positive regions, as well as the number of seconds the dial was in the negative, neutral, and positive regions, were recorded. Next, affect scores were calculated by subtracting (a) the number of seconds the dial was in the positive region multiplied by the average dial position during that time from (b) the number of seconds the dial was in the negative region multiplied by the average dial position during that time. The joystick apparatus and scoring procedure has been used in previous research assessing self-ratings of emotion (e.g., Lorber & O’Leary, 2005) and has demonstrated good construct validity (Lorber, 2007).
Cortisol reactivity.
Following procedures used by Granger and colleagues (2012), salivary cortisol samples were obtained from mothers at four time points during the lab visit, three of which are utilized in subsequent analyses. Statistical analyses were run using area under the curve with respect to the increase (AUCI; Pruessner et al., 2003), which is calculated with reference to the baseline measurement, thus emphasizing change over time. Saliva was collected via passive drool in a 2 mL polypropylene crovial (SalivaBio, Carlsbad, CA, USA), with participants providing enough saliva (at least 200 uL) for assaying of cortisol. Samples were immediately placed on ice in a cooler, transported to a −20°C freezer immediately after the study session, and later transferred to a −80°C freezer for long-term storage. Saliva samples were analyzed using a commercially available immunoassay without modification to the manufacturer’s recommended protocol (Salimetrics, State College, PA, USA). All samples were assayed in duplicate, with the average used in subsequent data analyses (intra-assay CV = 4.46%, inter-assay CV = 4.71%) in μg/dL.
Data Analysis
Statistical power for testing the proposed models was estimated a priori using a Monte Carlo simulation (Muthén & Muthén, 1998–2017; Thoemmes et al., 2010). Results indicated that 75 participants would be acceptable for testing the proposed models, assuming medium effect sizes and power > .80. We determined this sample would be sufficiently powered to analyze lax and overreactive parenting in separate models, consistent with prior research using this same paradigm (e.g., Slep & O’Leary, 1998). The data were carefully screened for accuracy, missingness, and outliers. Data on participants’ current mood and level of anxiety, general physical activity level, overall health, food and water intake, dental hygiene (e.g., oral disease, open mouth sores), oral contraceptive use, as well as sleep, alcohol, nicotine, caffeine, and medication use, were collected to screen for potential confounding influences on cortisol samples (see Granger et al., 2012), but no statistically significant relations emerged (rs ranging from .00 to .20, ps ranging from .08 to .99). However, two participants’ cortisol data were identified as possible outliers; one participant’s data was removed because cortisol levels were too high for the samples to be diluted within range of the assay. Consistent with recommendations (Pollet & van der Meij, 2017), the other participant’s data was addressed using a nonparametric procedure (bias-corrected bootstrapping) in analyses to ensure that it did not bias results. Two participants were missing data on the video-rated parenting behaviors due to technical malfunction of the video recording software. As a result, these participants were also missing data on the emotion ratings task, and an additional participant opted out of the emotion ratings task due to time constraints (n = 3). After cleaning the data and examining descriptive statistics, bivariate correlations were conducted to examine differences in the patterns of associations across PTSD groups.
To examine the specific aims of our study, we used Mplus (Muthén & Muthén, 1998–2017) to test direct and indirect effects of PTSD on parenting behaviors (i.e., laxness and overreactivity) as mediated through negative emotion and cortisol dysregulation. We used Hayes’ (2017) approach to mediation which specifies that indirect effects be estimated based on whether the product of paths a and b is significantly different than zero. Thus, statistical significance of both a and b separately are not requirements of mediation (Hayes, 2017, p. 116). We used a nonparametric resampling method (bias-corrected bootstrap) with 5,000 resamples to derive the 95% CIs. This approach performs well in small samples by maximizing power while minimizing Type 1 error rate and is optimal for the proposed design because it accounts for non-normal distributions of indirect effects. Data were missing for < 5% of the sample and were addressed using full information maximum likelihood.
We conducted four separate path analyses to investigate the point (i.e., subthreshold or full PTSD) at which mothers’ lax and overreactive parenting is affected. Specifically, two of these path analyses compared mothers with no PTSD or subthreshold PTSD (grouped together) to mothers with full PTSD on each parenting outcome (i.e., laxness and overreactivity). The other two path analyses compared mothers with subthreshold or full PTSD (grouped together) to mothers with no PTSD on each parenting outcome (i.e., laxness and overreactivity). Significant findings for the first two path models (comparing no PTSD to subthreshold+full PTSD) would suggest that problematic parenting exists among mothers with subthreshold or greater symptoms of PTSD. By contrast, significant findings for only the second set of analyses (comparing no PTSD+subthreshold to full PTSD) would suggest that parenting difficulties emerge at the level of full diagnostic criteria.
Results
Descriptive Statistics and Bivariate Correlations
Across the sample, 19 mothers met criteria for full PTSD, 24 met criteria for subthreshold PTSD (i.e., 2 or 3 symptoms clusters) but did not reach full diagnostic criteria, and 35 evidenced no significant PTSD pathology. Participants in the subthreshold and full PTSD groups reported a range of traumas on the LEC-5. Across these 43 participants, the most commonly identified “worst” index trauma consisted of physical/sexual domestic violence (n = 7; 16%), sexual assault by a non-partner (n = 6; 14%), physical/sexual child abuse (n = 4; 9%), witnessing a life-threatening illness/injury (n = 4; 9%), and witnessing a sudden accidental death (n = 4; 9%). The average PTSD symptom count and severity across participants with subthreshold PTSD was 5.2 (SD = 1.9), and 14.4 (SD = 4.4), respectively. The average PTSD symptom count and severity across participants with full PTSD was 12.7 (SD = 3.1), and 31.9 (SD = 8.9), respectively.
Descriptive statistics and bivariate correlations are displayed in Supplementary Table 1. Across the sample, mothers displayed moderate lax parenting behaviors and low levels of overreactive parenting. While watching the videos of their interactions, mothers’ emotion ratings reflected mildly positive mood on average, although significant variability is evident. Mothers’ cortisol reactivity scores reflected, on average, a sharp decrease in cortisol between samples 1 and 2, and a smaller decrease in cortisol during the recovery between samples 2 and 3. Mothers meeting criteria for full PTSD demonstrated greater laxness and greater overreactivity (relative to subthreshold or no PTSD). Additionally, mothers indicating more negative emotion during the tasks demonstrated greater lax parenting during the tasks (see Supplementary Table 1 for all test statistics and p-values). Lower income was correlated with greater parental overreactivity (r = −.25, p = .03), but not laxness (r = −.16, p = .17); however, to be conservative, we adjusted for income across both overreactivity and laxness models.
Path Analyses
Lax parenting.
As shown in Figure 1, consistent with hypotheses, mothers meeting full criteria for PTSD (relative to subthreshold or no PTSD) utilized more lax parenting behaviors during the discipline encounter (unstandardized direct effect: b = 0.921, 95% CI [0.211, 1.721]; standardized direct effect: β = 0.347, 95% CI [0.065, 0.597]), and greater negative emotion was significant associated with greater lax parenting (b = −0.004., 95% CI [−0.007, −0.002]; β = −0.317, 95% CI [−0.546, −0.140]). No indirect effects emerged in this model (negative emotion: b = −0.043, 95% CI [−0.248, 0.096]; β = −0.016, 95% CI [−0.094, 0.035]; cortisol reactivity: b = −0.022, 95% CI [−0.316, 0.078]; β = −0.008, 95% CI [−0.114, 0.030). The model accounted for 3.9% of the variance in cortisol reactivity, 9.3% of the variance in negative emotion, and 20.8% of the variance in lax parenting. In contrast, when comparing mothers meeting at least subthreshold PTSD (relative to no PTSD), greater negative emotion significantly mediated the association between PTSD status and lax parenting (indirect effect: b = 0.111, 95% CI [0.004, 0.364], β = 0.048, 95% CI [0.001, 0.142]). Cortisol reactivity did not significantly mediate associations between PTSD status and lax parenting (indirect effect: b = −0.037, 95% CI [−0.210, 0.031]; β = −0.016, 95% CI [−0.090, 0.015]). The model accounted for 6.0% of the variance in cortisol reactivity, 11.7% of the variance in negative emotion, and 12.4% of the variance in lax parenting behaviors.
Figure 1.
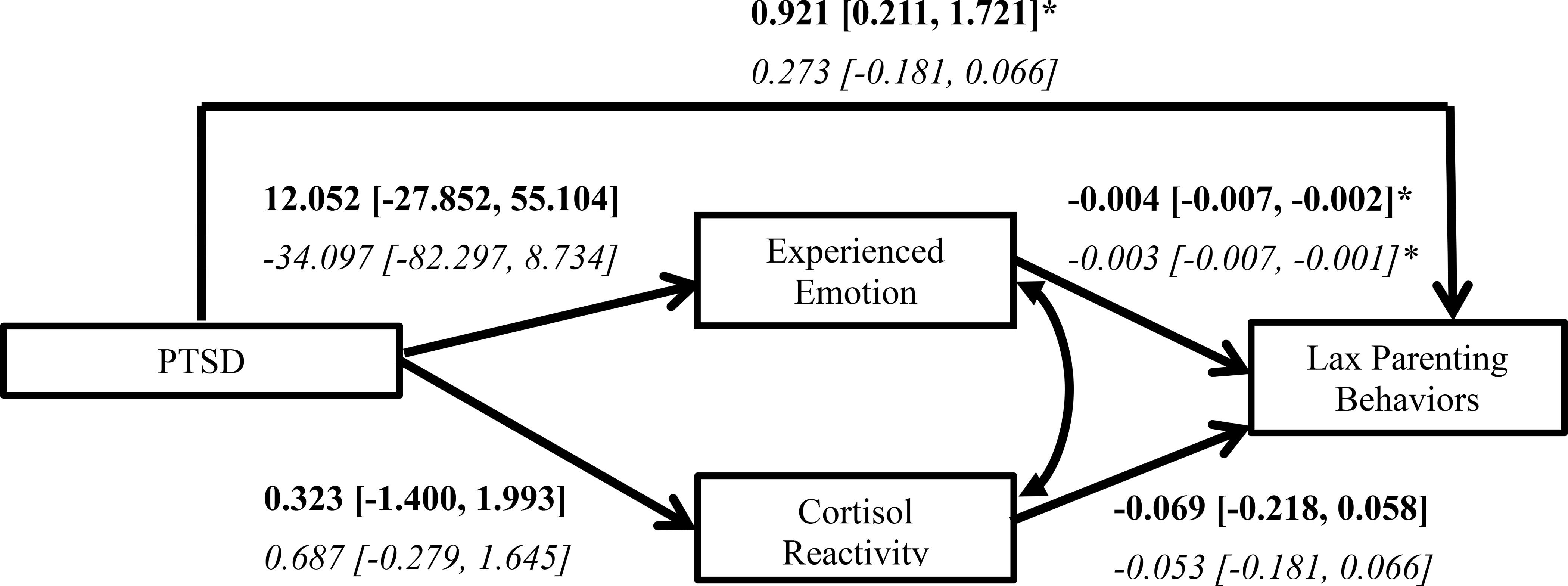
Path model for associations between PTSD status and lax parenting through experienced emotion and cortisol reactivity, controlling for income. Bolded estimates are from the model with PTSD representing the contrast between mothers who met criteria for PTSD relative to subthreshold or no PTSD; italicized estimates are from the model with PTSD representing the contrast between mothers who met at least subthreshold PTSD relative to no PTSD. We report bias-corrected confidence intervals based on 5,000 bootstrap draws.
* 95% CI does not contain zero
Overreactive parenting.
In contrast to hypotheses, mothers meeting criteria for PTSD (relative to subthreshold or no PTSD) were not more likely to use overreactive parenting during the discipline encounter (unstandardized direct effect: b = 0.673, 95% CI [−0.018, 1.405]; standardized direct effect: B = 0.296, 95% CI [−0.020, 0.566]). No indirect effects emerged in this model (negative emotion: b = −0.021, 95% CI [−0.218, 0.018]; β = −0.009, 95% CI [−0.088 0.008]; cortisol reactivity: b = −0.014, 95% CI [−0.206, 0.066]; β = −0.006, 95% CI [−0.090, 0.029]). The model accounted for 3.9% of the variance in cortisol reactivity, 8.9% of the variance in negative emotion, and 14.6% of the variance in overreactive parenting behaviors. Additionally, when comparing mothers meeting at least subthreshold PTSD (relative to no PTSD), there was no significant association between PTSD status and overreactive parenting (direct effect: b = 0.158, 95% CI [−0.352, 0.611]; β = 0.081, 95% CI [−0.190, 0.300]). No indirect effects emerged in this model (negative emotion: b = 0.025, 95% CI [−0.029, 0.183]; β = 0.013, 95% CI [−0.016, 0.089]; cortisol reactivity: b = −0.018, 95% CI [−0.139, 0.038]; β = −0.009, 95% CI [−0.073, 0.020). The model accounted for 5.9% of the variance in cortisol reactivity, 10.8% of the variance in negative emotion, and 7.8% of the variance in overreactive parenting behaviors.
Supplemental analyses.
Though the focus of the present study was to distinguish whether clinically meaningful thresholds (i.e., subthreshold versus full PTSD) are differentially associated with parenting, we conducted supplementary analyses that modeled PTSD symptoms as a continuous variable to examine associations among key constructs in a dimensional capacity (see Supplementary Figure). These results largely replicated main analyses; for each one unit increase in PTSD severity, there was a significant increase in lax parenting. Similarly, for each one unit increase in negative emotion, there was a significant increase in lax parenting. However, when examining PTSD symptoms in a dimensional capacity, greater negative emotion did not significantly mediate the association between PTSD status and lax parenting.
Discussion
The present study investigated the association between PTSD and maternal parenting and examined experienced emotion and cortisol reactivity as potential mediators of this association. We did not find support for the hypothesized model in its entirety; however, there was evidence of significant direct and indirect effects among particular paths within the model. Specifically, on average, mothers meeting full criteria for PTSD, compared to those with subthreshold or few to no symptoms of PTSD, used greater lax parenting behaviors. Further, on average, mothers experiencing at least subthreshold PTSD engaged in greater lax parenting by way of increased negative emotion. PTSD status was unrelated to overreactive parenting, and cortisol reactivity did not mediate associations between PTSD and either form of maladaptive parenting behavior.
To our knowledge, this is the first study to use observational methods to demonstrate that PTSD is associated with lax/permissive behaviors among parents of young children. The finding that mothers with PTSD more often engaged in lax parenting behaviors is unique, but parallels other findings demonstrating links between PTSD and related constructs, such as parental distress avoidance behaviors (e.g., rapid soothing, Brockman et al., 2016). The associations found here suggest that PTSD symptoms might be associated with increased avoidance of effortful attempts to manage child behaviors during situations that elicit rule-breaking. It is possible that mothers with PTSD may withdraw from parenting situations they perceive as overwhelming in response to trauma-related symptoms such as emotional numbing and experiential avoidance. Findings also align with the notion that trauma is associated with increased use of permissive parenting behaviors due to diminished emotional resources for enforcing discipline (see DiLillo & Damashek, 2003). Indeed, PTSD is characterized by strong negative emotions, including fear, anger, guilt, and shame; mothers who experience these emotions more intensely may struggle to effectively enforce rules.
In support of the latter possibility, the present results indicate that greater negative emotion mediated relations between PTSD status and lax parenting. To our knowledge, this is the first study to specifically examine reports of in vivo emotional experiences in the context of parenting among mothers with PTSD. Findings support theory suggesting that PTSD is associated with increased negative affect during emotionally evocative situations (Orsillo et al., 2004), and that greater intensity of negative emotions is associated with more ineffective parenting behaviors (Rueger et al., 2011). Strong negative emotions may interfere with parental appraisals, undermine emotion regulation, and instigate behaviors to lessen negative emotions that conflict with sensitivity to children’s needs (Dix, 1991; Lorber & O’Leary, 2005). The present work also aligns with evidence that PTSD does not need to rise to DSM-5 threshold criteria to significantly influence interpersonal functioning (e.g., Zlotnick et al., 2002). That is, trauma-related symptoms have the potential to intensify emotional reactivity and influence parenting behaviors even at comparatively milder levels. Further, results of supplemental analyses indicated that the indirect effect of negative emotion was no longer present when examining PTSD symptoms continuously. This suggests that considering discrete thresholds of severity might reveal important mechanisms that would otherwise be overlooked when examining PTSD in a dimensional capacity.
PTSD status was not associated with overreactive parenting behaviors in the present study. These findings contrast with theory suggesting that trauma symptoms are associated with greater irritability and anger reactions, including hostile parenting behaviors (e.g., Leen-Feldner et al., 2011). One reason why the link between PTSD and overreactive parenting did not emerge may stem from the relatively low rates of overreactive parenting observed across the entire study sample. Although the analytic technique used here accounted for non-normal data, there may have been a floor effect for maternal overreactivity, which in turn limited the ability to predict higher levels across the sample. Alternatively, there is evidence from prior work that trauma-exposed mothers who are resilient may compensate for potential consequences of trauma by increasing attentiveness and sensitivity to their children (Letourneau et al., 2007). A similar process may have occurred among mothers in the present study, enabling them to more easily regulate their responses to child misbehavior.
Results did not support our hypothesis that greater negative emotion mediates the association between PTSD and overreactive parenting, suggesting that other variables such as parenting attitudes, physiological arousal (e.g., heart rate variability), and skills deficits may play a bigger role in influencing harsh parenting (Lorber & O’Leary, 2005; Pinderhughes et al., 2000). Results also did not support our hypothesis that cortisol dysregulation mediates relations between PTSD and either lax or overreactive parenting. Comprehensive reviews on the link between PTSD and cortisol reactivity paint a complicated picture where differences exist among: (1) comorbidly depressed individuals with PTSD versus individuals with PTSD-only, (2) those exposed to single versus multi-event traumas, and (3) those exposed to recent trauma versus exposure occurring during childhood (e.g., Morris et al., 2012). Future research using larger samples would allow for examination of moderators and therefore provide a better understanding of the potential role of cortisol in impacting parenting behaviors among trauma-exposed mothers.
Limitations and Future Directions
The present study included mothers with diverse trauma histories recruited from the community. This is especially important given that prior studies of PTSD and parenting typically sample from discrete populations (e.g., military service members exposed to combat). Still, it is possible that specific types of trauma (e.g., exposure to child abuse) uniquely influence parenting and warrant future study. Relatedly, it is possible that populations exposed to more complex trauma experiencing more severe psychopathology may face greater challenges with parenting. For example, a sizable literature suggests that depressed mothers with histories of child maltreatment demonstrate high levels of parenting impairment (e.g., Muzik et al., 2017), suggesting a need for researchers to account for varying types of trauma-related psychopathology. Next, the majority of participants in the current study were White and highly-educated, and approximately half reported household incomes above the state median. The link between PTSD and difficulties with parenting may be more robust among mothers from disadvantaged backgrounds, given reduced access to resources and increased exposure to daily stressors (Hatch & Dohwenrend, 2007). Fathers are also deserving of future study; though associations between PTSD and parenting among male military service members has been well-studied (see Creech & Misca, 2017 for a review), less attention has been devoted to understanding how civilian PTSD might affect parenting.
Lab-based observational methods are useful for studying how families navigate stressful parent-child interactions, in part, because they enable examination of biological, emotional, and behavioral processes as they naturally unfold. Despite the advantages of this approach, the present study relied on cross-sectional data for testing mediation hypotheses, which precludes evidence of directionality among our key constructs of interest. Though existing theory supports the proposed directionality, the simultaneous measurement of our mediators and outcome variables may have resulted in inflated associations. Further, because the standardized lab task used here was designed to elicit parental responses to typical instances of child misbehavior, it is possible that it did not entirely replicate the intensity of a discipline encounter that would more predictably elicit strong physiological and emotional reactivity in some mothers. For example, on average, mothers did not endorse predominantly negative emotion across the tasks. To enhance ecological validity, future research could utilize a more stressful parent-child interaction task—perhaps in the context of the home environment—to elicit these kinds of reactions.
Next, although we collected data on mothers’ moment-to-moment emotional experiences, a summary score was ultimately used in the present analyses. This summary score was obtained using a semantic differential scale (i.e., polar adjectives at extremes of the scale) ranging from negative to position emotion, as opposed to reflecting negative emotion only. Future research could explore more proximal links between negative emotion and specific parenting behaviors by investigating whether moment-to-moment positive or negative emotion ratings precede specific instances of overreactivity and laxness. Additionally, given evidence suggesting that different kinds of negative emotions (e.g., anger, fear, sadness) may result in different motivation orientations and action tendencies in the context of parenting (Dix, 1991), future research should investigate how different emotions may differentially predict harsh and lax parenting among PTSD-affected parents. Finally, additional mechanisms beyond cortisol reactivity and experienced emotion should be examined as mediators within the context of PTSD and parenting behaviors. Undoubtedly, there are numerous affective (e.g., experiential avoidance), cognitive (e.g., attributional biases), and biological (e.g., parasympathetic influences, epigenetic factors) correlates of PTSD with effects on parenting.
Clinical Implications
Findings suggest a number of possible avenues for intervention. In addition to providing trauma-exposed mothers with empirically supported treatments for PTSD, parenting-focused interventions centered on helping mothers modify the intensity and frequency of their negative emotions in response to child behavior are also likely to be useful for mothers with PTSD. For example, if mothers with PTSD symptoms struggle to manage negative emotions arising in the context of aversive child behavior, they may have difficulty setting limits on child misbehavior. These mothers may benefit from training in distress tolerance to strengthen their resolve around sticking to established rules. Further, if PTSD symptoms increase parents’ attention to negatively biased cognitions (e.g., related to parental inefficacy around rule-setting), they might benefit from interventions focused on challenging these cognitions in order to better regulate negative emotions. Indeed, a number of interventions that aim to improve parenting by addressing trauma-related distress have already been developed, including Mom Power (Gewirtz et al., 2017) and the After Deployment Adaptive Parenting Tools Program (Muzik et al., 2015). However, though parent training programs often emphasize reducing harsh and inconsistent parenting (O’Connell et al., 2009), our findings suggest that permissive parenting may be of particular concern and warrant addressing among mothers with significant PTSD symptoms. Efforts to reduce permissiveness could be aided by research that identifies the moment-to-moment precipitants of lax parenting among those with PTSD symptoms. Finally, our findings in combination with a growing body of research uncovering a range of clinically significant impairments among those with subthreshold symptoms (e.g., Zlotnick et al., 2002) suggest the importance of addressing emotion regulation and parenting behaviors across a wider spectrum of trauma-exposed populations.
Supplementary Material
Acknowledgments
This research was supported by a Ruth L. Kirschstein National Research Service Award (F31HD089687) from the National Institute of Child Health and Human Development (NICHD), an American Psychological Association (APA) Dissertation Research Award, and an internal funding mechanism Social and Behavioral Sciences Research Consortium at the University of Nebraska-Lincoln awarded to Dr. Molly R. Franz, under the supervision of Dr. David DiLillo.
Although data from this sample have been published elsewhere (i.e., Kumar, Franz, Brock, & DiLillo, 2019), this is the first article in which salivary cortisol reactivity and in-themoment ratings of experienced emotion were examined as predictors of observed parenting behaviors. Portions of this article were presented at the Association for Behavioral and Cognitive Therapies Convention, November 2018, Washington D.C.
We thank the mothers and children who participated in this research, Drs. Amy Smith Slep and Douglas Granger who served as consultants, and the team of research assistants who contributed to various stages of the study. In particular, we thank Elizabeth Alexander, Laurel Bailey, Madeline Contreras, Anika Eisenbraun, Kristina Riemer, Naomi Samuel, Abbie Sanders, Tanner Smith, and Autumn Urbigkit for project coordination.
Contributor Information
Molly R. Franz, University of Maryland, Baltimore County
Shaina A. Kumar, University of Nebraska-Lincoln
Rebecca L. Brock, University of Nebraska-Lincoln
Jessica L. Calvi, University of Nebraska-Lincoln
David DiLillo, University of Nebraska-Lincoln.
References
- Ammerman RT, Putnam FW, Chard KM, Stevens J, & Van Ginkel JB (2012). PTSD in depressed mothers in home visitation. Psychological Trauma: Theory, Research, Practice, and Policy, 4, 186–195. doi: 10.1037/a0023062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Trauma and stressor-related disorders. In Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Arnold EH & O’Leary SG (1995). The effect of child negative affect on maternal discipline behavior. Journal of Abnormal Child Psychology, 23, 585–595. doi: 10.1007/BF01447663 [DOI] [PubMed] [Google Scholar]
- Arnold DS, O’Leary SG, Wolff LS, & Acker MM (1993). The Parenting Scale: a measure of dysfunctional parenting in discipline situations. Psychological Assessment, 5, 137–144. doi: 10.1037/1040-3590.5.2.137 [DOI] [Google Scholar]
- Berg-Nielsen T, Vikan A, & Dahl AA (2002). Parenting related to child and parental psychopathology: A descriptive review of the literature. Clinical Child Psychology and Psychiatry, 7, 529–552. doi: 10.1177/1359104502007004006 [DOI] [Google Scholar]
- Bornstein MH, & Bradley RH (2014). Socioeconomic status, parenting, and child development. Abingdon, UK: Routledge. [Google Scholar]
- Boyce WT, & Ellis BJ (2005). Biological sensitivity to context: I. An evolutionary–developmental theory of the origins and functions of stress reactivity. Development and Psychopathology, 17, 271–301. doi:10.10170S0954579405050145 [DOI] [PubMed] [Google Scholar]
- Brockman C, Snyder J, Gewirtz A, Gird SR, Quattlebaum J, Schmidt N, … Zettle R (2016). Relationship of service members’ deployment trauma, PTSD symptoms, and experiential avoidance to postdeployment family reengagement. Journal of Family Psychology, 30, 52–62. doi: 10.1037/fam0000152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlier IV, & Gersons BP (1995). Partial posttraumatic stress disorder (PTSD): The issue of psychological scars and the occurrence of PTSD symptoms. Journal of Nervous and Mental Disease, 183, 107–109. doi: 10.1097/00005053-199502000-00008 [DOI] [PubMed] [Google Scholar]
- Christie H, Hamilton-Giachritsis C, Alves-Costa F, Tomlinson M, & Halligan SL (2019). The impact of parental posttraumatic stress disorder on parenting: A systematic review. European Journal of Psychotraumatology, 10, 1550345. doi: 10.1080/20008198.2018.1550345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti DV (1994). Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment, 6, 284–290. doi: 10.1037/1040-3590.6.4.284 [DOI] [Google Scholar]
- Cordero MI, Moser DA, Manini A, Suardi F, Sancho-Rossignol A, Torrisi R, … & Schechter DS (2017). Effects of interpersonal violence-related post-traumatic stress disorder (PTSD) on mother and child diurnal cortisol rhythm and cortisol reactivity to a laboratory stressor involving separation. Hormones and Behavior, 90, 15–24. doi: 10.1016/j.yhbeh.2017.02.007 [DOI] [PubMed] [Google Scholar]
- Creech SK, & Misca G (2017). Parenting with PTSD: A review of research on the influence of PTSD on parent-child functioning in military and veteran families. Frontiers in Psychology, 8, 1101–1108. 10.3389/fpsyg.2017.01101/full [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dekel R, & Monson CM (2010). Military-related post-traumatic stress disorder and family relations: Current knowledge and future directions. Aggression and Violent Behavior, 15, 303–309. doi: 10.1016/j.avb.2010.03.001 [DOI] [Google Scholar]
- Del Guidice M, Ellis BJ, & Shirtcliff EA (2011). The adaptive calibration model of stress responsivity. Neuroscience and Biobehavioral Reviews, 35, 1562–1592. doi: 10.1016/j.neubiorev.2010.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiLillo D, & Damashek A (2003). Parenting characteristics of women reporting a history of childhood sexual abuse. Child Maltreatment, 8, 319–333.doi: 10.1177/1077559503257104 [DOI] [PubMed] [Google Scholar]
- Dix T (1991). The affective organization of parenting: Adaptive and maladaptative processes. Psychological Bulletin, 110, 3–25. doi: 10.1037/0033-2909.110.1.3 [DOI] [PubMed] [Google Scholar]
- Elzinga BM, Schmahl CG, Vermetten E, van Dyck R, & Bremner JD (2003). Higher cortisol levels following exposure to traumatic reminders in abuse-related PTSD. Neuropsychopharmacology, 28, 1656–1665. doi: 10.1038/sj.npp.1300226 [DOI] [PubMed] [Google Scholar]
- Finucane AM, Dima A, Ferreira N, & Halvorsen M (2012). Basic emotion profiles in healthy, chronic pain, depressed and PTSD individuals. Clinical Psychology & Psychotherapy, 19, 14–24. doi: 10.1002/cpp.733 [DOI] [PubMed] [Google Scholar]
- Franklin CL, Raines AM, Chambliss JL, Walton JL, & Maieritsch KP (2018). Examining various subthreshold definitions of PTSD using the Clinician Administered PTSD Scale for DSM-5. Journal of Affective Disorders, 234, 256–260. doi: 10.1016/j.jad.2018.03.001 [DOI] [PubMed] [Google Scholar]
- Gewirtz AH, DeGarmo DS, & Zamir O (2017). After deployment, adaptive parenting tools: 1-year outcomes of an evidence-based parenting program for military families following deployment. Prevention Science, 19, 589–599. doi: 10.1007/s11121-017-0839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez A, Jenkins JM, Steiner M, & Fleming AS (2012). Maternal early life experiences and parenting: The mediating role of cortisol and executive function. Journal of the American Academy of Child & Adolescent Psychiatry, 51, 673–682. doi: 10.1016/j.jaac.2012.04.003 [DOI] [PubMed] [Google Scholar]
- Granger DA, Johnson SB, Szanton SL, Out D, & Schumann LL (2012). Incorporating salivary biomarkers into nursing research: An overview and review of best practices. Biological Research for Nursing, 14, 347–356. doi: 10.1177/1099800412443892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatch SL, & Dohrenwend BP (2007). Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: A review of the research. American Journal of Community Psychology, 40, 313–332. doi: 10.1007/s10464-007-9134-z [DOI] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (2nd ed.). New York, NY: Guilford Press. [Google Scholar]
- Herbers JE, Garcia EB, & Obradović J (2017). Parenting assessed by observation versus parent-report: Moderation by parent distress and family socioeconomic status. Journal of Child and Family Studies, 26, 3339–3350. doi: 10.1007/s10826-017-0848-8 [DOI] [Google Scholar]
- Jaffe AE, Cranston CC, & Shadlow JO (2012). Parenting in females exposed to intimate partner violence and childhood sexual abuse. Journal of Child Sexual Abuse, 21, 684–700. doi: 10.1080/10538712.2012.726698 [DOI] [PubMed] [Google Scholar]
- Juul SH, Hendrix C, Robinson B, Stowe ZN, Newport DJ, Brennan PA, & Johnson KC (2015). Maternal early-life trauma and affective parenting style: The mediating role of HPA-axis function. Archives of Women’s Mental Health, 1, 1–7. doi: 10.1007/s00737-015-0528-x [DOI] [PubMed] [Google Scholar]
- Kalb LM, & Loeber R (2003). Child disobedience and noncompliance: A review. Pediatrics, 111, 641–652. doi: 10.1542/peds.111.3.641 [DOI] [PubMed] [Google Scholar]
- Kumar SA, Franz MR, Brock RL, & DiLillo D (2019). Posttraumatic stress and parenting behaviors: The mediating role of emotion regulation. Journal of Family Violence. doi: 10.1007/s10896-019-00124-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letourneau NL, Fedick CB, & Willms JD (2007). Mothering and domestic violence: A longitudinal analysis. Journal of Family Violence, 22, 649–659. doi: 10.1007/s10896-007-9099-6 [DOI] [Google Scholar]
- Lorber MF (2007). Validity of video-mediated recall procedures for mothers’ emotion and child ratings. Journal of Family Psychology, 21, 520–528. doi: 10.1037/0893-3200.21.3.520 [DOI] [PubMed] [Google Scholar]
- Lorber MF, & O’Leary SG (2005). Mediated paths to overreactive discipline: Mothers’ experienced emotion, appraisals, and physiological responses. Journal of Consulting and Clinical Psychology, 73, 972–981. doi: 10.1037/0022-006X.73.5.972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Koenen KC, Friedman MJ, Ruscio AM, Karam EG, Shahly V, … Andrade LH (2015). Subthreshold posttraumatic stress disorder in the world health organization world mental health surveys. Biological Psychiatry, 77, 375–384. doi: 10.1016/j.biopsych.2014.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maughan DR, Christiansen E, Jenson WR, Olympia D, & Clark E (2005). Behavioral parent training as a treatment for externalizing behaviors and disruptive behavior disorders: A meta-analysis. School Psychology Review, 34, 267–286. doi: 10.1080/02796015.2005.12086287 [DOI] [Google Scholar]
- Mills-Koonce WR, Propper C, Gariepy JL, Barnett M, Moore GA, Calkins S, & Cox MJ (2009). Psychophysiological correlates of parenting behavior in mothers of young children. Developmental Psychobiology, 51, 650–661. doi: 10.1002/dev.20400 [DOI] [PubMed] [Google Scholar]
- Morris MC, Compas BE, & Garber J (2012). Relations among posttraumatic stress disorder, comorbid major depression, and HPA function: A systematic review and meta-analysis. Clinical Psychology Review, 32, 301–315. doi: 10.1016/j.cpr.2012.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO (1998–2017). Mplus User’s Guide. Eighth Edition. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Muzik M, Rosenblum KL, Alfafara EA, Schuster MM, Miller NM, Waddell RM, & Kohler ES (2015). Mom Power: Preliminary outcomes of a group intervention to improve mental health and parenting among high-risk mothers. Archives of Women’s Mental Health, 18, 507–521. doi: 10.1007/s00737-014-0490-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzik M, Morelen D, Hruschak J, Rosenblum KL, Bocknek E, & Beeghly M (2017). Psychopathology and parenting: An examination of perceived and observed parenting in mothers with depression and PTSD. Journal of Affective Disorders, 207, 242–250. doi: 10.1016/j.jad.2016.08.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connell ME, Boat T, & Warner KE (2009). Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities (Vol. 7). Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Orsillo SM, Batten SV, Plumb JC, Luterek JA, & Roessner BM (2004). An experimental study of emotional responding in women with posttraumatic stress disorder related to interpersonal violence. Journal of Traumatic Stress, 17, 241–248. doi: 10.1023/B:JOTS.0000029267.61240.94 [DOI] [PubMed] [Google Scholar]
- Pinderhughes EE, Dodge KA, Bates JE, Pettit GS, & Zelli A (2000). Discipline responses: Influences of parents’ socioeconomic status, ethnicity, beliefs about parenting, stress, and cognitive-emotional processes. Journal of Family Psychology, 14, 380–400. doi: 10.1037/0893-3200.14.3.380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollet TV, & van der Meij L (2017). To remove or not to remove: the impact of outlier handling on significance testing in testosterone data. Adaptive Human Behavior and Physiology, 3, 43–60. doi: 10.1007/s40750-016-0050-z [DOI] [Google Scholar]
- Pruessner JC, Kirschbaum C, Meinlschmid G, & Hellhammer DH (2003). Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology, 28, 916–931. doi: 10.1016/S0306-4530(02)00108-7 [DOI] [PubMed] [Google Scholar]
- Rueger SY, Katz RL, Risser HJ, & Lovejoy MC (2011). Relations between parental affect and parenting behaviors: A meta-analytic review. Parenting: Science and Practice, 11, 1–33. doi: 10.1080/15295192.2011.539503 [DOI] [Google Scholar]
- Schwerdtfeger KL, Larzelere RE, Werner D, Peters C, & Oliver M (2013). Intergenerational transmission of trauma: The mediating role of parenting styles on toddlers’ DSM-related symptoms. Journal of Aggression, Maltreatment & Trauma, 22, 211–229. doi: 10.1080/10926771.2013.743941 [DOI] [Google Scholar]
- Slep AMS, & O’Leary SG (1998). The effects of maternal attributions on parenting: An experimental analysis. Journal of Family Psychology, 12, 234–243. doi: 10.1037/0893-3200.12.2.234 [DOI] [Google Scholar]
- Thoemmes F, MacKinnon DP, & Reiser MR (2010). Power analysis for complex mediational designs using Monte Carlo methods. Structural Equation Modeling, 17, 510–534. doi: 10.1080/10705511.2010.489379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Ee E, Kleber RJ, & Mooren T (2012). War trauma lingers on: Associations between maternal posttraumatic stress disorder, parent–child interaction, and child development. Infant Mental Health Journal, 33, 459–468. doi: 10.1002/imhj.21324 [DOI] [PubMed] [Google Scholar]
- Vythilingam M, Blair KS, McCaffrey D, Scaramozza M, Jones M, Nakic M, … & Pine DS (2007). Biased emotional attention in post-traumatic stress disorder: A help as well as a hindrance? Psychological Medicine, 37, 1445–1455. doi: 10.1017/S003329170700092X [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013a). The PTSD Checklist for DSM-5 (PCL-5) – LEC-5 and Extended Criterion A Instrument available from http://www.ptsd.va.gov
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013b). The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5). Interview available from the National Center for PTSD; at www.ptsd.va.gov. [Google Scholar]
- Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, … & Marx BP (2018). The Clinician-Administered PTSD Scale for DSM–5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychological Assessment, 30, 383–395. doi: 10.1037/pas0000486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehuda R (2002). Current status of cortisol findings in post-traumatic stress disorder. Psychiatric Clinics of North America, 25, 341–368. doi: 10.1016/S0193-953X(02)00002-3 [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Franklin CL, & Zimmerman M (2002). Does “subthreshold” posttraumatic stress disorder have any clinical relevance? Comprehensive Psychiatry, 43, 413–419. doi: 10.1053/comp.2002.35900 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


