Abstract
Objective
Scores to predict sepsis or define sepsis severity could improve care for very low birth weight (VLBW) infants. The heart rate characteristics (HRC) index (HeRO score) was developed as an early warning system for late-onset sepsis (LOS), and also rises before necrotizing enterocolitis (NEC). The neonatal sequential organ failure assessment (nSOFA) was developed to predict sepsis-associated mortality using respiratory, hemodynamic, and hematologic data. The aim of this study was to analyze the HRC index and nSOFA near blood cultures in VLBW infants relative to diagnosis and sepsis-associated mortality.
Study Design
Retrospective, single-center study of VLBW infants from 2011 to 2019. We analyzed HRC index and nSOFA around blood cultures diagnosed as LOS/NEC. In a subgroup of the cohort, we analyzed HRC and nSOFA near the first sepsis-like illness (SLI) or sepsis ruled-out (SRO) compared with LOS/NEC. We compared scores by diagnosis and mortality during treatment.
Results
We analyzed 179 LOS/NEC, 93 SLI, and 96 SRO blood culture events. In LOS/NEC, the HRC index increased before the blood culture, while nSOFA increased at the time of culture. Both scores were higher in nonsurvivors compared with survivors and in LOS/NEC compared with SRO. The nSOFA 12 hours after the time of blood culture predicted mortality during treatment better than any other time point analyzed (area under the curve 0.91).
Conclusion
The HRC index provides earlier warning of imminent sepsis, whereas nSOFA after blood culture provides better prediction of mortality.
Keywords: prematurity, predictive analytics, necrotizing enterocolitis, neonatal sepsis
Sudden deterioration due to inflammatory illnesses such as late-onset sepsis (LOS) and necrotizing enterocolitis (NEC) can have lifelong or life-limiting consequences for premature infants in the neonatal intensive care unit (NICU). Rates of LOS and NEC have decreased over time, but morbidity and mortality remain high, particularly for very low birth weight (VLBW, <1,500 g) infants.1 Survivors have a high risk of permanent neurodevelopmental impairment, attributed to the damaging effects of inflammation on the developing brain.2,3 Early detection of the systemic inflammatory response to infection could lead to earlier treatment and improved outcomes.
Heart rate characteristics (HRC) monitoring was developed to detect signatures of illness from the NICU bedside monitor electrocardiogram, and was validated in multicenter VLBW cohorts to predict the fold-increased risk of imminent deterioration from sepsis as the HRC index (HeRO score).4,5 For example, an HRC index of 2.0 indicates a twofold increase in sepsis risk within the next 24 hours. Display of the HRC index reduced sepsis-associated mortality by 40% in a large randomized clinical trial, presumably because of earlier diagnosis and treatment.6,7 This continuous risk score detects abnormal patterns in the HR of decreased variability and transient decelerations caused by the systemic inflammatory response to infection.8,9 The HRC index was designed to predict sepsis, but can be altered by medications or conditions other than sepsis, including surgery, postnatal steroids, and significant respiratory deterioration.10–12 A high average HRC index is associated with an increased risk of mortality,13,14 but the score is not well calibrated for illness severity.
The lack of a scoring system correlated with the severity of neonatal sepsis remains a critical barrier to research and quality improvement.15 For adults, a sequential organ failure assessment (SOFA) tool was developed decades ago16 to predict mortality or identify the need for ICU transfer. A threshold SOFA score of two or more serves as the operational definition of life-threatening organ dysfunction and defines sepsis among adults with suspected infection.17 Recently, a similar tool was developed for NICU patients to predict the risk of death during sepsis treatment.18,19 The neonatal SOFA (nSOFA) score estimates mortality risk by assigning points for respiratory deterioration, hemodynamic compromise, and hematologic dysfunction.
The score was derived from observational data on progressive organ failure in cases of fatal LOS,20 and then validated for sepsis mortality prediction in a separate, single-center cohort.19 Recently, a large multicenter study validated the score for predicting mortality in preterm infants with LOS and demonstrated similar performance at multiple NICUs.21 The nSOFA score has not previously been evaluated in patients diagnosed with culture-negative sepsis or infections with a focus other than blood or spinal fluid, which we call sepsis-like illness (SLI).
In this study, we aimed to analyze both HRC index values and nSOFA scores near blood culture events and assess the changes in the two risk markers relative to the diagnosis and relative to mortality during treatment of LOS or NEC. We speculated that nSOFA and HRC monitoring would provide complementary information to guide the care of the septic neonate, with the HRC index pointing the clinician to the patient at high risk of imminent deterioration due to sepsis and the nSOFA score grading the severity of the episode by estimating the risk of death during treatment.
Materials and Methods
Subjects and Definitions
The University of Virginia Institutional Review Board (UVA IRB) approved this retrospective cohort study with a waiver of consent. For VLBW infants <33 weeks’ gestational age admitted from 2011 to 2019, we reviewed all cases of bacteremia diagnosed as LOS and all events diagnosed as NEC with or without bacteremia. We defined LOS as sepsis with a positive blood culture obtained after 3 days of age and treated with at least 5 days of antibiotics. Blood culture events positive for Coagulase-negative Staphylococcus (CONS) were excluded if the clinical team called the result a contaminant or treated the infant with antibiotics for <5 days. NEC cases were identified from a unit-specific database for event tracking and only cases of confirmed modified Bell’s stage II or greater were included in the analysis. We used the time of the earliest blood culture associated with the NEC event as the time of diagnosis. The actual time of diagnosis based on exam or radiological findings may differ, but typically not by more than a few hours. We analyzed more than one event per infant if the two LOS/NEC events were separated by at least 10 days without antibiotics. The primary outcome was death during the treatment of confirmed infection as defined by death prior to the cessation of antibiotics. As a secondary outcome, we analyzed death at any time after LOS or NEC.
In a subset of the cohort (2012–2017), we reviewed the first negative blood culture obtained after 3 days of age to determine the diagnosis. Infants with LOS or NEC as well as a distinct negative blood culture event were included in both analyses. Negative blood culture events were defined as follows:
SLI—negative blood culture treated at least 5 days with empiric antibiotics for clinical sepsis or focal infection, including urinary tract infection (UTI), pneumonia, or spontaneous intestinal perforation;
Sepsis ruled-out (SRO)—negative blood culture and treated for <5 days with empiric antibiotics.
Events with either nSOFA or HRC index data missing were excluded from both analyses, which eliminated events that occurred within 48 hours of admission for infants admitted after 3 days of age.
nSOFA Score Calculation
The components used to calculate nSOFA scores were automatically extracted from the electronic health record and validated by chart review. The score assigns points according to the following criteria19:
Respiratory: 0 points if no need for mechanical ventilation or intubated with oxygen saturation/fraction of inspired oxygen (SpO2/FiO2) ratio ≥ 300; 2 points if intubated with SpO2/FiO2 <300, 4 points for <200, 6 points for <150, or 8 points for <100);
Cardiovascular: 1 point for systemic steroid use, 2 points for inotrope use, 3 points for one inotrope plus systemic steroids or additional inotropes, and 4 points for two or more inotropes and systemic steroids;
Hematologic: 0 points for platelet count ≥ 150 × 103, 1 point for platelet count 100–149 × 103, 2 points for platelets 50–99 × 103, or 3 points for platelets < 50 × 103.
A new nSOFA score was calculated every time new data points were available from the flowsheets. nSOFA scores were analyzed at nine time points: the time of blood culture (time 0) and 6, 12, 24, and 48 hours before and after the blood culture.
HRC Index Data Collection
All infants were monitored using the HeRO system (Medical Predictive Science Corporation, Charlottesville, VA) during the study period. The HRC monitoring algorithm uses measurements of HR variability, asymmetry, and entropy to capture abnormal patterns of decreased HR variability and repetitive HR decelerations. The HRC index is calculated from the previous 12 hours of electrocardiogram data, updated hourly, and represents the fold-increased risk of clinical deterioration with confirmed or suspected sepsis in the subsequent 24 hours. Central and bedside monitors display the continuous HRC index for all NICU patients, and nurses file scores hourly in the electronic medical record.
Data Analysis
At nine time-points surrounding the time of blood culture, we compared the HRC index and nSOFA for infants with LOS/NEC who died during treatment to those who survived the infection using Wilcoxon rank-sum tests. Scores at each time point were also compared between events diagnosed as LOS/NEC, SLI, and SRO using Wilcoxon tests. We analyzed the change from baseline in HRC index and nSOFA by comparing the score at 48 hours before culture to the values at all subsequent times (24, 12, and 6 hours prior to the event, the time of the event, and 6, 12, 24, 48 hours after the event) using Wilcoxon signed-rank tests. We used logistic regression to predict death during treatment of LOS or NEC with the HRC index, total nSOFA, and component nSOFA scores and calculate the area under the receiver operator characteristic curves (AUC).
Results
Clinical Characteristics of Patients and Events
Among 956 VLBW infants <33 weeks’ gestational age admitted from 2011 to 2019, we identified 207 cases of LOS/NEC (166 LOS in 150 infants [16%], 41 NEC in 41 infants [4%]). This overall prevalence aligns with published multicenter LOS and NEC rates.22–25 Six LOS and nine NEC events did not meet our definition of a distinct event or had missing data, so a total of 192 LOS/NEC events in 179 patients were included in the analysis. Table 1 compares the characteristics of infants analyzed with LOS or NEC to those of the full cohort. Infants with LOS or NEC had lower gestational age and birth weight, more comorbidities, and were more likely to be male (p < 0.05). In the subgroup of infants admitted during 2012 to 2017, 313 of 612 infants (51%) had at least one blood culture obtained to evaluate for LOS. Of these, we analyzed the first distinct event with a negative blood culture in 188 infants with data available; 92 were diagnosed as SLI (42 clinical sepsis, 50 focal infections without bacteremia) and 96 were diagnosed as SRO. Age at blood culture was higher for events diagnosed as LOS or NEC, but this is only comparing the age at the first negative blood culture and most infants had more than one. Table 2 shows the frequency of organisms isolated in LOS events, with CONS identified in 59%.
Table 1.
Clinical characteristics of VLBW infants <33 weeks’ gestational age with LOS or NEC during the study period compared with all infants
| With LOS or NEC | All VLBW infants | |
|---|---|---|
| n (%) | 179 (19%) | 956 |
| Gestational age, weeks (mean, SD) | 25.7 (2.31)a | 27.2 (2.62) |
| Birth weight, grams (mean, SD) | 816 (230)a | 978 (295) |
| Female, n (%) | 76 (42.5%)a | 465 (48.6%) |
| Died before NICU discharge, n (%) | 20 (10.1%) | 90 (9.4%) |
Abbreviations: LOS, late-onset sepsis; NEC, necrotizing enterocolitis; NICU, neonatal intensive care unit; SD, standard deviation; VLBW, very low birth weight.
p < 0.05.
Table 2.
Organisms isolated in positive blood cultures and classification of cases diagnosed as necrotizing enterocolitis (NEC)
| Organism | n (%) |
|---|---|
| Total | 158 |
| Coagulase negative staphylococcal sp. | 110 (69) |
| Staphylococcus aureus | 12 (8) |
| Escherichia coli | 10 (6) |
| Klebsiella pneumoniae | 6 (4) |
| Enterobacter cloacae | 4 (2) |
| Serratia marcescens | 4 (2) |
| Enterococcus faecalis | 3 (2) |
| Group B. Streptococcus | 3 (2) |
| Pseudomonas Aeruginosa | 2 (1) |
| NEC with bacteremia | 9 |
| NEC without bacteremia | 25 |
| Stage 2 | 15 |
| Stage 3 | 10 |
Mortality during treatment in the LOS/NEC cases occurred in 10 infants (8 LOS, 2 NEC) at median 4 days from culture (range: 0–15). Of the eight infants who died during LOS, three had gram-negative and five had gram-positive bacteremia. Twenty (11%) infants with LOS or NEC died at any time following the event and 90 (9%) died overall. Of the 10 infants who survived the LOS/NEC episode but died before discharge, the median days from the event to death were 51 days (range: 20–148).
HRC Index and nSOFA Scores in LOS/NEC Survivors versus Nonsurvivors
Figs. 1 and 2 show the distribution of nSOFA using boxplots at each of the nine time points analyzed and show the continuous HRC index using a loess curve to fit the group means at each time point analyzed. For infants with LOS/NEC, both the HRC index and nSOFA were higher near the time of blood culture for infants who died during the event than for those who survived (Fig. 1A, B). The difference in survivors and nonsurvivors was apparent for nSOFA earlier than the HRC index (earliest comparison with p < 0.05 at 48 hours before culture for nSOFA versus time 0 for HRC index). Mortality occurred in 19% of events with nSOFA >4 at 6 hours after culture, and the mean HRC index was higher in these events compared with events with nSOFA 0–4 (mean [standard deviation] vs. at 6 hours after culture, p < 0.05) (Fig. 3). Table 3 shows the AUC and 95% confidence interval (CI) predicted by nSOFA and HRC at the time of blood culture and the maximum score of the nine time points, both for mortality during LOS or NEC and at any time after.
Fig. 1.
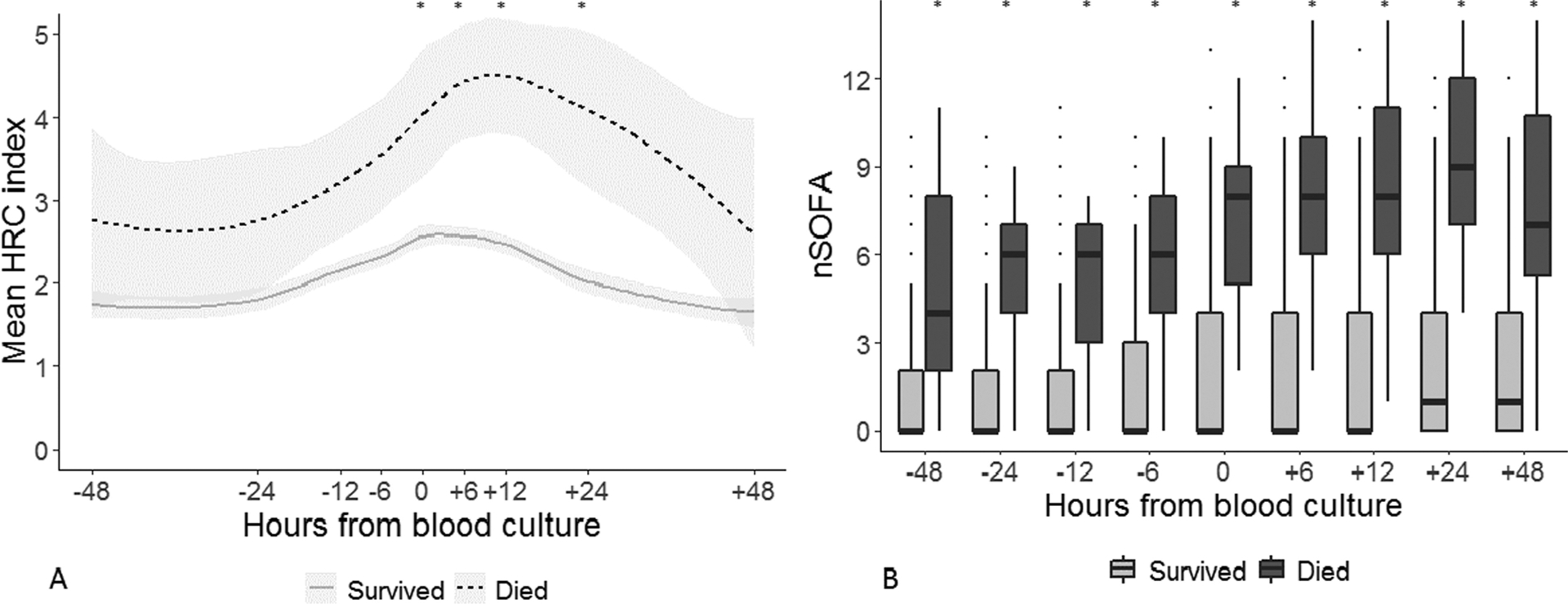
Heart rate characteristics (HRC) index and neonatal sequential organ failure assessment (nSOFA) scores at nine time points surrounding the time of blood culture (time 0) in events diagnosed as late-onset sepsis (LOS) or necrotizing enterocolitis (NEC) for patients who died during the episode compared with those who survived. (A) The HRC index was higher for infants who died during LOS or NEC from the time of blood culture to 24 hours after (*p < 0.05). (B) nSOFA was higher for infants who died during LOS or NEC at all time points analyzed (*p < 0.01).
Fig. 2.
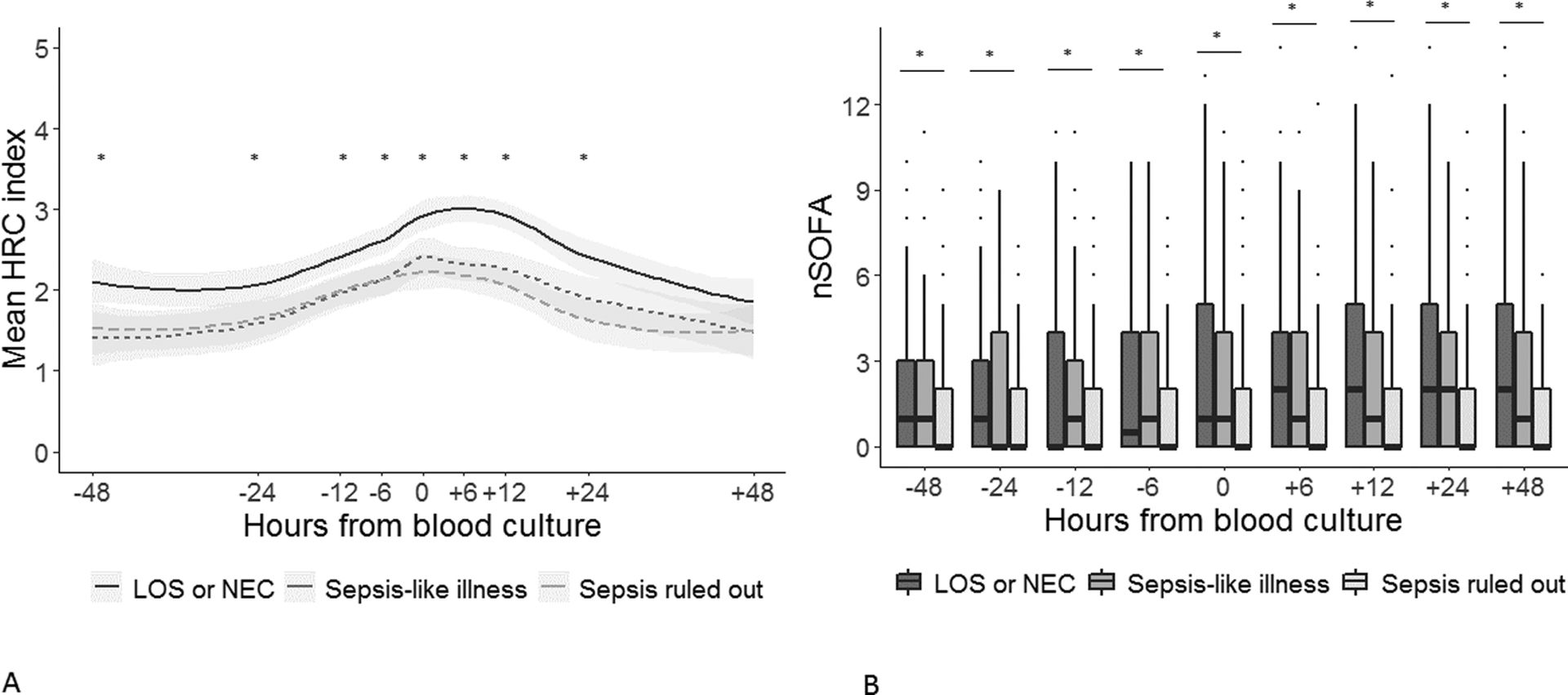
The heart rate characteristics (HRC) index and neonatal sequential organ failure assessment (nSOFA) scores for cases diagnosed as late-onset sepsis with bacteremia or necrotizing enterocolitis (NEC), sepsis-like illnesses, and sepsis ruled out. (A) Mean HRC index was higher from 48 hours before to 24 hours after blood culture for cases of late-onset sepsis (LOS) or NEC compared with events diagnosed as sepsis-like illness or sepsis ruled-out (*p < 0.05). (B) nSOFA scores were higher for events diagnosed as LOS or NEC than those where sepsis was ruled out (*p < 0.05 at all-time points), but were not different from sepsis-like illnesses.
Fig. 3.
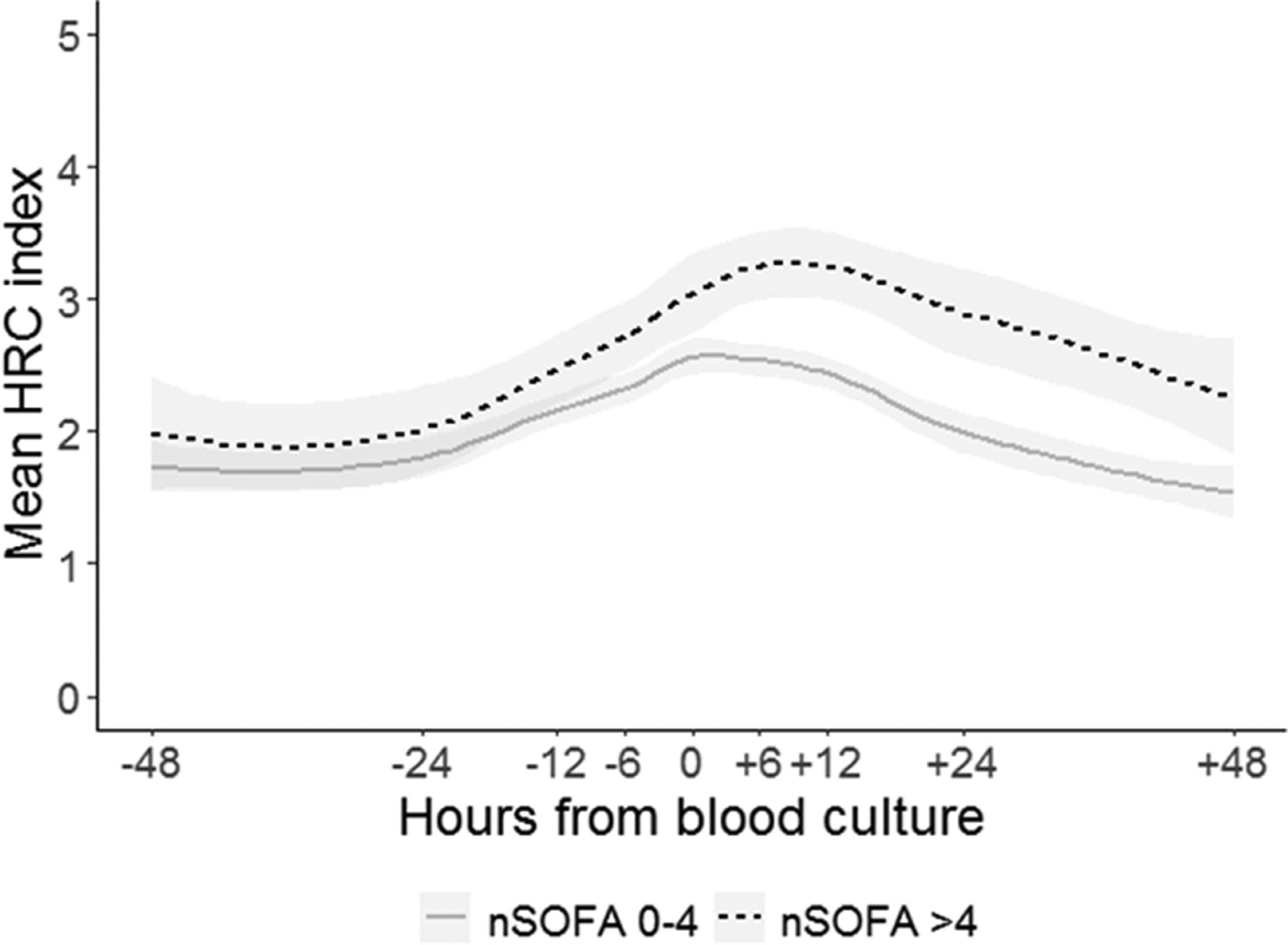
The heart rate characteristics (HRC) index was higher at the time of blood culture and every time point after for events with neonatal sequential organ failure assessment (nSOFA) >4 compared with events with nSOFA 0–4.
Table 3.
Predictive performance of nSOFA and HRC index for death during treatment of sepsis or NEC (n = 10) and death any time after sepsis or NEC (n = 20)
| Mortality during LOS or NEC AUC (95% CI) | Mortality any time after LOS or NEC AUC (95% CI) | |
|---|---|---|
| nSOFA time 0 | 0.859 (0.766–0.952) | 0.831 (0.746–0.916) |
| HRCi time 0 | 0.644 (0.508–0.780) | 0.548 (0.440–0.656) |
| nSOFAMax | 0.938 (0.880–0.996) | 0.888 (0.825–0.951) |
| HRCiMax | 0.677 (0.524–0.829) | 0.568 (0.456–0.679) |
| nSOFAMax + HRCiMax | 0.944 (0.889–0.999) | 0.890 (0.827–0.952) |
Abbreviations: AUC, area under the curve; CI, confidence interval; HRC, heart rate characteristics; LOS, late-onset sepsis; NEC, necrotizing enterocolitis; nSOFA, neonatal sequential organ failure assessment.
Components of nSOFA in Survivors versus Nonsurvivors of LOS/NEC
Points given for respiratory dysfunction (mechanical ventilation and SpO2/FiO2 ratio) were the most predictive component at all time points analyzed (Fig. 4). The cardiovascular component AUC increased from the time points before culture to after (12 hours before culture = 0.558 [95% CI: 0.430–0.687]; time 0 = 0.615 [95% CI: 0.456–0.773]; 12 hours after culture = 0.793 [95% CI: 0.629–0.958]), while the hematologic component remained a poor individual predictor by AUC at every time point (AUC: 0.552–0.561). By 12 hours after blood culture, the total nSOFA score predicted mortality during LOS or NEC with AUC 0.912 (95% CI: 0.841–0.987) (Fig. 4B).
Fig. 4.
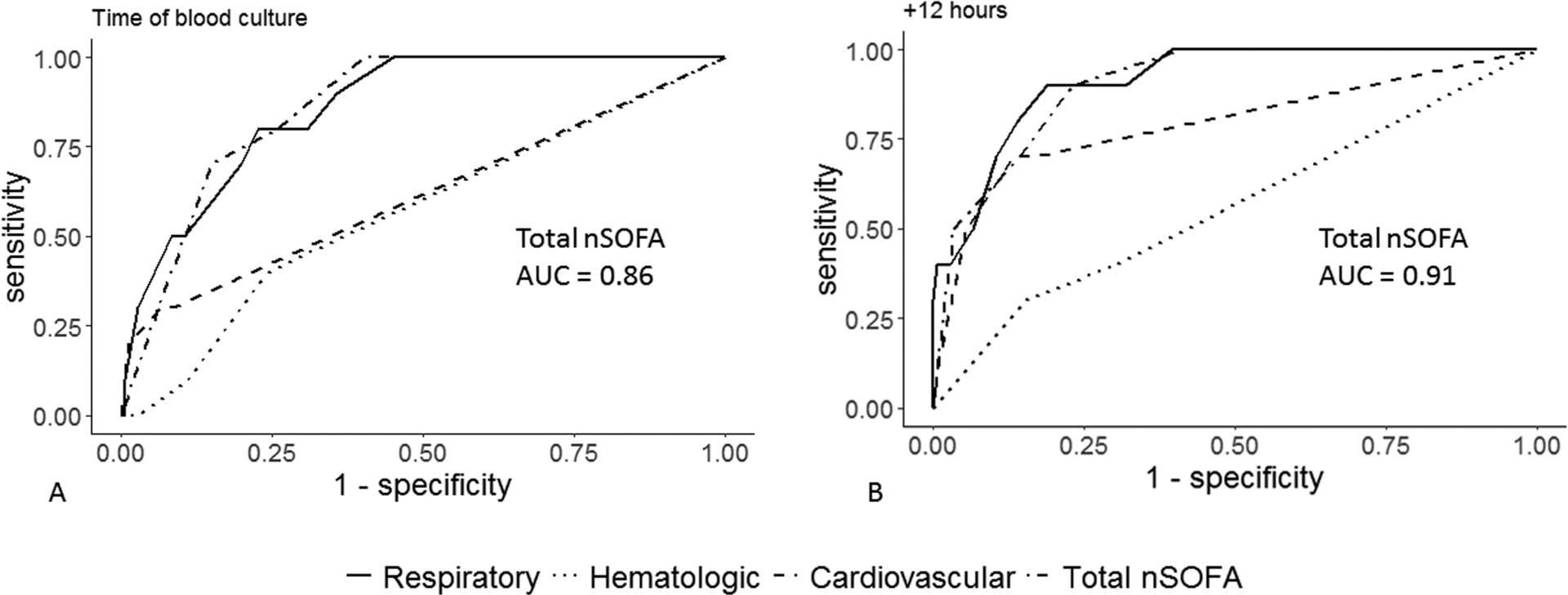
Receiver operator characteristic curves for the total neonatal sequential organ failure assessment (nSOFA) and component scores at the time of positive blood culture and 12 hours after culture. Points given for respiratory dysfunction (mechanical ventilation and oxygen saturation/fraction of inspired oxygen ratio) were the most predictive component at all time points analyzed. The cardiovascular component area under the curve (AUC) increased from time points before culture to after, while the hematologic component remained a poor individual predictor by AUC at every time point. By 12 hours after blood culture, performance of the total nSOFA score to predict mortality during the episode reached an AUC of 0.91.
HRC Index and nSOFA in LOS or NEC versus SLI and SRO
In the subset of the cohort with negative blood culture events abstracted, the mean HRC index was higher near the time of blood culture for LOS or NEC compared with SLI and SRO (Fig. 2A). nSOFA was higher at all time points in events diagnosed as LOS or NEC than those diagnosed as SRO (p < 0.05), but was not different from SLI events (Fig. 2B).
In an analysis of repeated measures of the HRC index in all cases of LOS or NEC, the increase from baseline for each infant occurred, on average, 6 hours before the time of blood culture (p < 0.01 for the value 48 hours before culture compared with the value 6 hours before culture and every subsequent time point). nSOFA also rose near the time of positive blood culture or NEC, with a significant change from 48 hours before culture to the time of blood culture for all events (p < 0.01, Fig. 5).
Fig. 5.
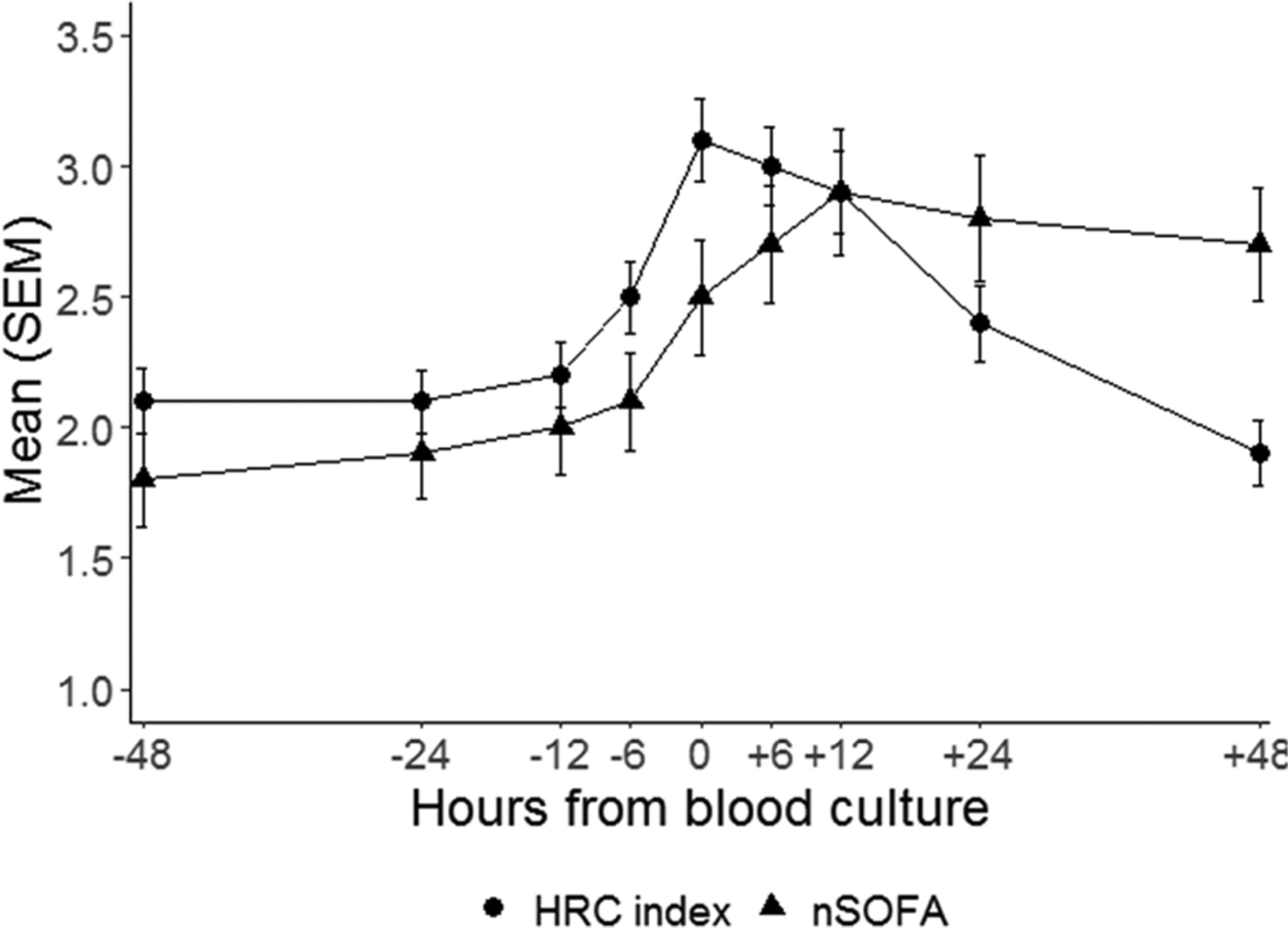
In cases of late-onset sepsis or necrotizing enterocolitis, the heart rate characteristics (HRC) index increased from baseline (48 hours before culture) by 6 hours before blood culture, while neonatal sequential organ failure assessment (nSOFA) increased compared with baseline at the time of culture.
Discussion
In this study of VLBW infants with proven and suspected sepsis, we describe both the HRC index, developed as an early warning system for sepsis,26 and the nSOFA score, developed to gauge sepsis severity and predict mortality.19 We found that both scores were elevated in confirmed infections compared with negative sepsis evaluations and that both scores were higher in infants who died during treatment of the infection. Furthermore, in cases of LOS or NEC, the rise in the HRC index occurred before the blood culture, while the rise in nSOFA occurred shortly after. nSOFA demonstrated high predictive performance for mortality during the sepsis treatment, which serves as an important marker of the severity of the event. Our results demonstrate how a predictive monitoring score and an illness severity score might be useful when combined in clinical practice. An increase in the HRC index brings the attention of the clinical team to the infant with imminent clinical deterioration, while nSOFA communicates the severity of illness and predicts risk of mortality.
The HRC index was developed at UVA and tested in a nine-NICU randomized trial that showed reduced all-cause and sepsis-related mortality for infants randomized to have their HRC index displayed.6,7 Previous studies have shown an increase in the hours to days preceding clinical diagnosis, which our results in an independent cohort confirm.27–29 While prior studies have shown HRC to be similar for events diagnosed as clinical sepsis or UTI and sepsis with bacteremia,29,30 our cohort shows a higher HRC index for LOS and NEC events compared with SLIs, which includes clinical, or culture-negative, sepsis and focal infections. We grouped these events because their numbers were too small to analyze individually and because of their clinical similarities. In these cases, infection might not be confirmed or uniformly defined, but the medical team decides that the illness warrants empiric treatment for infection with a course of antibiotics.
The HRC index algorithm continuously monitors for abnormal HR patterns caused by systemic inflammation8 and bacterial toxin effect.9 While some infants with an exaggerated inflammatory response to infection may have a higher HRC index, abnormal HR patterns alone do not define the severity of the event. Instead, illness severity has been estimated by developing nSOFA, an empirical score based on organ dysfunction as it presents in neonates.19,20 HRC monitoring is well calibrated to predict imminent infection,26 but can be altered by medications or conditions other than sepsis. For example, postnatal steroids increase HR variability,11 while atropine decreases it by blocking parasympathetic control of the heart. Surgeries performed with general anesthesia increase the HRC index, likely due to the combined effect of anesthesia and inflammation on HR control. Finally, pain and pain medications may transiently affect HRC31 but have not been shown to cause an abrupt increase in the HRC index. A retrospective review of “spikes” in the HRC index from patients where the score was not displayed showed that half of these events were associated with blood culture for suspected infection, a third correlated with a respiratory deterioration, and in another third, there was no clear clinical event associated with the spike.10 We were unable to account for all variables that may cause a false increase in the HRC index, a limitation of the retrospective analysis.
nSOFA and HRC monitoring are likely to be synergistic both in clinical care and research. In clinical care, abnormal HRC points to the infant needing careful assessment for signs of infection. Once sepsis is diagnosed, nSOFA is highly predictive of mortality and provides the first objective tool of its kind to define sepsis severity.19 Our results show that these two validated scores can provide complementary information to the clinical team. In research, predictive monitoring algorithms such as HRC have been modeled on sepsis using the only currently available definitions: either positive blood culture or antibiotic duration or both. With nSOFA to classify sepsis severity, predictive algorithms can be modeled using more clinically relevant outcomes, which might improve performance.32 In this study, events with an elevated nSOFA shortly after diagnosis had a higher HRC index during the event.
Infants who died during sepsis treatment in this study had a higher average HRC index and nSOFA than those who survived, as early as 2 days before blood culture. We did not calculate nSOFA more than 48 hours from the blood culture but hypothesize that the baseline scores for infants who die of sepsis are higher than the average for survivors, possibly as early as birth. Prospective studies of nSOFA are needed to evaluate the score longitudinally for baseline and episodic differences. A study of early HRC by Sullivan et al found that the average HRC index in the first 24 hours and 7 days after birth was higher in infants who died or developed sepsis weeks later.14 Other studies of abnormal HRC demonstrate a higher baseline in infants who ultimately develop sepsis compared with those who have relatively stable NICU courses.4,27
In adult medicine, the operational definition of sepsis recently changed from using systemic inflammatory response syndrome (SIRS) criteria to organ failure criteria,17,33 as defined by the adult SOFA score.16 SIRS criteria have also failed to accurately define sepsis in neonates.34,35 Neonatal sepsis is typically defined by blood culture results and antibiotic duration, criteria that have been recognized as problematic due to the potential for false negative and false positive blood culture results as well as variability in antibiotic use.36,37 nSOFA was developed as an operational definition for sepsis using empirical points for quantification of neonatal organ dysfunction in the categories of respiratory, cardiovascular, and hematologic systems.19 In our cohort, the respiratory component was the most predictive component at all time points, but the predictive performance of the hematologic and cardiac components improved after the event. This is not surprising, as hypotension and thrombocytopenia often prompt a sepsis evaluation and therefore points for the hematologic and cardiovascular components follow the time of diagnosis. However, respiratory distress is not specific to sepsis in the NICU and therefore might not trigger a sepsis evaluation. Furthermore, this component uses physiological monitoring data, as does HRC monitoring, and adding measures of respiratory dysfunction to continuous HRC might also improve early warning of sepsis.12,38 We analyzed the HRC index and nSOFA models as they were developed and validated in previous studies, but adding mortality and sepsis risk factors such as gestational age or birth weight could further improve risk prediction. Nonsurvivors had lower gestational age and birth weight in our cohort and previous studies have shown the added value of combining physiologic and demographic variables for models predicting sepsis.27,38
The retrospective design and low number of infants with the primary outcome limit the validity of our results. While the overall cohort and number of LOS/NEC events were large, relatively few infants died during treatment of the event. Still, our results align with a multicenter analysis of nSOFA,21 providing some assurance in their generalizability despite the small numbers. We chose this primary outcome to be consistent with previous studies published on nSOFA for the sake of comparison and because death due to sepsis is an objective measure of the episode’s severity. Using death at any time after the event, results were similar. We did not analyze the cause of death for infants who died after completing treatment for sepsis or NEC. The analysis of negative blood culture events was also limited by the study design. Most VLBW infants with at least one blood culture have more than one blood culture,39 but we did not annotate every blood culture. Instead, we analyzed the first negative blood culture, which assumes that the trends of nSOFA and HRC are similar for the first sepsis rule out or clinical sepsis event and subsequent ones. Further studies are needed to analyze trends longitudinally for every episode and to analyze continuous sepsis risk prediction stratified by illness severity.
Prospective studies are needed to further demonstrate the utility of combined predictive monitoring for sepsis using a continuous early warning score such as the HRC index and a periodic mortality risk score based on organ failure criteria such as nSOFA. Furthermore, model development using events defined by illness severity could improve performance of predictive analytics for early sepsis detection.
Conclusion
In VLBW infants with confirmed late-onset infection, the HRC index increased before the time of blood culture and the nSOFA was higher in nonsurvivors compared with survivors. Both scores were higher in events diagnosed as LOS or NEC compared with those diagnosed as SRO. SLIs had HRC index values similar to events with no infection but nSOFA values similar to confirmed infections. This study demonstrates the strengths of each score and the potential utility of their combined use in clinical care and research.
Key Points.
The HRC index and nSOFA provide complementary information on sepsis risk and sepsis-related mortality risk.
This study adds to existing literature evaluating these risk scores independently by analyzing them together and in cases of not only proven but also suspected infections.
The impact of combining risk models could be improved outcomes for premature infants.
Funding
B.A.S. (K23HD097254), K.D.F. (R01HD072071), and J.L.W. (R01GM128452; R01HD089939, R01HD097081) received support from the National Institutes of Health.
Footnotes
Conflict of Interest
J.L.W. has served as a paid consultant for Evolve Biosystems. The other authors declare no conflict of interest.
References
- 1.Greenberg RG, Kandefer S, Do BT, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Late-onset sepsis in extremely premature infants: 2000–2011. Pediatr Infect Dis J 2017;36(08): 774–779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stoll BJ, Hansen NI, Adams-Chapman I, et al. ; National Institute of Child Health and Human Development Neonatal Research Network. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA 2004;292(19):2357–2365 [DOI] [PubMed] [Google Scholar]
- 3.Bright HR, Babata K, Allred EN, et al. ; ELGAN Study Investigators. Neurocognitive outcomes at 10 years of age in extremely preterm newborns with late-onset bacteremia. J Pediatr 2017;187:43–49. e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Griffin MP, Moorman JR. Toward the early diagnosis of neonatal sepsis and sepsis-like illness using novel heart rate analysis. Pediatrics 2001;107(01):97–104 [DOI] [PubMed] [Google Scholar]
- 5.Fairchild KD, O’Shea TM. Heart rate characteristics: physiomarkers for detection of late-onset neonatal sepsis. Clin Perinatol 2010;37(03):581–598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moorman JR, Carlo WA, Kattwinkel J, et al. Mortality reduction by heart rate characteristic monitoring in very low birth weight neonates: a randomized trial. J Pediatr 2011;159(06):900–6.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fairchild KD, Schelonka RL, Kaufman DA, et al. Septicemia mortality reduction in neonates in a heart rate characteristics monitoring trial. Pediatr Res 2013;74(05):570–575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fairchild KD, Srinivasan V, Moorman JR, Gaykema RPA, Goehler LE. Pathogen-induced heart rate changes associated with cholinergic nervous system activation. Am J Physiol Regul Integr Comp Physiol 2011;300(02):R330–R339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fairchild KD, Saucerman JJ, Raynor LL, et al. Endotoxin depresses heart rate variability in mice: cytokine and steroid effects. Am J Physiol Regul Integr Comp Physiol 2009;297(04):R1019–R1027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sullivan BA, Grice SM, Lake DE, Moorman JR, Fairchild KD. Infection and other clinical correlates of abnormal heart rate characteristics in preterm infants. J Pediatr 2014;164(04): 775–780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alonzo CJ, Fairchild KD. Dexamethasone effect on heart rate variability in preterm infants on mechanical ventilation. J Neonatal Perinatal Med 2017;10(04):425–430 [DOI] [PubMed] [Google Scholar]
- 12.Sullivan BA, Fairchild KD. Predictive monitoring for sepsis and necrotizing enterocolitis to prevent shock. Semin Fetal Neonatal Med 2015;20(04):255–261 [DOI] [PubMed] [Google Scholar]
- 13.Griffin MP, O’Shea TM, Bissonette EA, Harrell FE Jr, Lake DE, Moorman JR. Abnormal heart rate characteristics are associated with neonatal mortality. Pediatr Res 2004;55(05):782–788 [DOI] [PubMed] [Google Scholar]
- 14.Sullivan BA, McClure C, Hicks J, Lake DE, Moorman JR, Fairchild KD. Early heart rate characteristics predict death and morbidities in preterm infants. J Pediatr 2016;174:57–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wynn JL, Polin RA. Progress in the management of neonatal sepsis: the importance of a consensus definition. Pediatr Res 2018;83(1–1):13–15 [DOI] [PubMed] [Google Scholar]
- 16.Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 1996;22(07):707–710 [DOI] [PubMed] [Google Scholar]
- 17.Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016;315(08):801–810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sweeney TE, Wynn JL, Cernada M, et al. Validation of the sepsis metascore for diagnosis of neonatal sepsis. J Pediatric Infect Dis Soc 2018;7(02):129–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wynn JL, Polin RA. A neonatal sequential organ failure assessment score predicts mortality to late-onset sepsis in preterm very low birth weight infants. Pediatr Res 2020;88(01):85–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wynn JL, Kelly MS, Benjamin DK, et al. Timing of multiorgan dysfunction among hospitalized infants with fatal fulminant sepsis. Am J Perinatol 2017;34(07):633–639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fleiss N, Coggins SA, Lewis AN, et al. Evaluation of the neonatal sequential organ failure assessment and mortality risk in preterm infants with late-onset infection. JAMA Netw Open 2021;4(02): e2036518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patel AL, Panagos PG, Silvestri JM. Reducing incidence of necrotizing enterocolitis. Clin Perinatol 2017;44(03):683–700 [DOI] [PubMed] [Google Scholar]
- 23.Boghossian NS, Page GP, Bell EF, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Late-onset sepsis in very low birth weight infants from singleton and multiple-gestation births. J Pediatr 2013;162(06):1120–1124, 1124.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zozaya C, García González I, Avila-Alvarez A, et al. Incidence, treatment, and outcome trends of necrotizing enterocolitis in preterm infants: a multicenter cohort study. Front Pediatr 2020; 8:188. Doi: 10.3389/fped.2020.00188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Horbar JD, Carpenter JH, Badger GJ, et al. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics 2012;129(06):1019–1026 [DOI] [PubMed] [Google Scholar]
- 26.Griffin MP, Lake DE, Bissonette EA, Harrell FE Jr, O’Shea TM, Moorman JR. Heart rate characteristics: novel physiomarkers to predict neonatal infection and death. Pediatrics 2005;116(05): 1070–1074 [DOI] [PubMed] [Google Scholar]
- 27.Lake DE, Fairchild KD, Moorman JR. Complex signals bioinformatics: evaluation of heart rate characteristics monitoring as a novel risk marker for neonatal sepsis. J Clin Monit Comput 2014;28(04): 329–339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stone ML, Tatum PM, Weitkamp JH, et al. Abnormal heart rate characteristics before clinical diagnosis of necrotizing enterocolitis. J Perinatol 2013;33(11):847–850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Griffin MP, O’Shea TM, Bissonette EA, Harrell FE Jr, Lake DE, Moorman JR. Abnormal heart rate characteristics preceding neonatal sepsis and sepsis-like illness. Pediatr Res 2003;53(06): 920–926 [DOI] [PubMed] [Google Scholar]
- 30.Aviles-Otero N, Ransom M, Weitkamp J, et al. Urinary tract infections in very low birthweight infants: a two-center analysis of microbiology, imaging and heart rate characteristics. J Neonatal Perinatal Med 2020(x):1–8 [DOI] [PubMed] [Google Scholar]
- 31.Weissman A, Zimmer EZ, Aranovitch M, Blazer S. Heart rate dynamics during acute pain in newborns. Pflugers Arch 2012; 464(06):593–599 [DOI] [PubMed] [Google Scholar]
- 32.Coggins SA, Weitkamp J-H, Grunwald L, et al. Heart rate characteristic index monitoring for bloodstream infection in an NICU: a 3-year experience. Arch Dis Child Fetal Neonatal Ed 2016;101 (04):F329–F332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of clinical criteria for sepsis: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016;315(08): 762–774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coggins S, Harris MC, Grundmeier R, Kalb E, Nawab U, Srinivasan L. Performance of pediatric systemic inflammatory response syndrome and organ dysfunction criteria in late-onset sepsis in a quaternary neonatal intensive care unit: a case-control study. J Pediatr 2020;219:133–139.e1 [DOI] [PubMed] [Google Scholar]
- 35.Hofer N, Zacharias E, Müller W, Resch B. Performance of the definitions of the systemic inflammatory response syndrome and sepsis in neonates. J Perinat Med 2012;40(05):587–590 [DOI] [PubMed] [Google Scholar]
- 36.Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Lancet 2017;390 (10104):1770–1780 [DOI] [PubMed] [Google Scholar]
- 37.Mukhopadhyay S, Puopolo KM. Antibiotic use and mortality among premature infants without confirmed infection-perpetrator or innocent bystander? JAMA Pediatr 2016;170(12): 1144–1146 [DOI] [PubMed] [Google Scholar]
- 38.Sullivan BA, Nagraj VP, Berry KL, et al. Clinical and vital sign changes associated with late-onset sepsis in very low birth weight infants at 3 NICUs. J Neonatal Perinatal Med 2021(x):1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stoll BJ, Hansen N, Fanaroff AA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics 2002;110(2 Pt 1):285–291 [DOI] [PubMed] [Google Scholar]


