Diabetes-related foot ulcers (DFUs) affect around 20 million people annually and are a leading cause of the global disability burden (1). DFUs are complex to treat, take months to heal, result in poorer quality of life, and place patients at high risk of hospitalization and amputation. Thus, understanding the influence that different factors have on healing of DFUs is vital.
Various demographic, comorbidity, limb, ulcer, and treatment-related factors associated with healing of DFUs have been identified from cohorts attending mostly metropolitan tertiary centers (2–4). However, very few studies have prospectively investigated the influence that these and other factors have on healing in more real-world DFU cohorts attending geographically diverse secondary and tertiary centers. Therefore, we aimed to investigate the influence of 34 factors on healing in a large real-world DFU cohort.
We prospectively examined 4,832 consecutive patients with DFU(s) that presented for their first visit to 1 of 65 secondary or tertiary diabetic foot services, across 15 of 17 regions in Queensland (Australia), between July 2011 and December 2017. A DFU was defined as a full-thickness wound below the ankle on a person with diabetes. For DFU clinical and research purposes, foot-related health professionals using the Queensland High Risk Foot Form (QHRFF) directly examined each patient clinically at their first (and subsequent) visit for 4 demographic, 9 comorbidity, 6 limb, 3 ulcer, and 12 treatment factors (5). For those with multiple DFUs, we used the most severe score for each factor and the combined ulcer size from all DFUs (5). Factors from the first visit were used as the baseline. Subsequent visit examinations determined if the DFU(s) healed, defined as complete epithelialization of all DFUs without amputation, death, or recurrence within 1 month. The QHRFF is valid and reliable for the direct capture of these factors by the foot-related health professionals that were trained with a QHRFF manual (5).
DFUs healed within 3 and 12 months were the primary outcomes, as different factors have been reported to influence short- and longer-term healing (2–4). All factors were analyzed at a univariable level, with those achieving P < 0.1 entered into multivariable logistic regression models to examine factors independently associated with each outcome. Before analysis, we excluded 123 patients lost to follow-up after baseline visit, excluded factors with >25% missing data, and used multiple imputation for factors with <25% missing data. All analyses were performed using Stata/SE version 16.1 (StataCorp, TX, USA).
Of 4,709 included patients (median age 63 years [interquartile range 54–72], 69.5% male, 91.0% with type 2 diabetes, 10.5% Indigenous Australians), 1,956 (41.5%) healed within 3 months and 3,012 (64.0%) within 12 months. After entering 18 factors into the multivariable models (Fig. 1), 7 were negatively associated with DFU healing within both 3 and 12 months, including younger age (<50 years), geographical remoteness, smoking, peripheral arterial disease, large ulcer sizes, deep ulcers, and infection, while receiving knee-high offloading treatment at baseline was positively associated with healing (all P ≤ 0.05). Other factors negatively associated with healing within 3 months were neuropathy, and those for healing within 12 months were previous amputation and recent surgical and medical specialist treatment (at baseline or the prior week).
Figure 1.
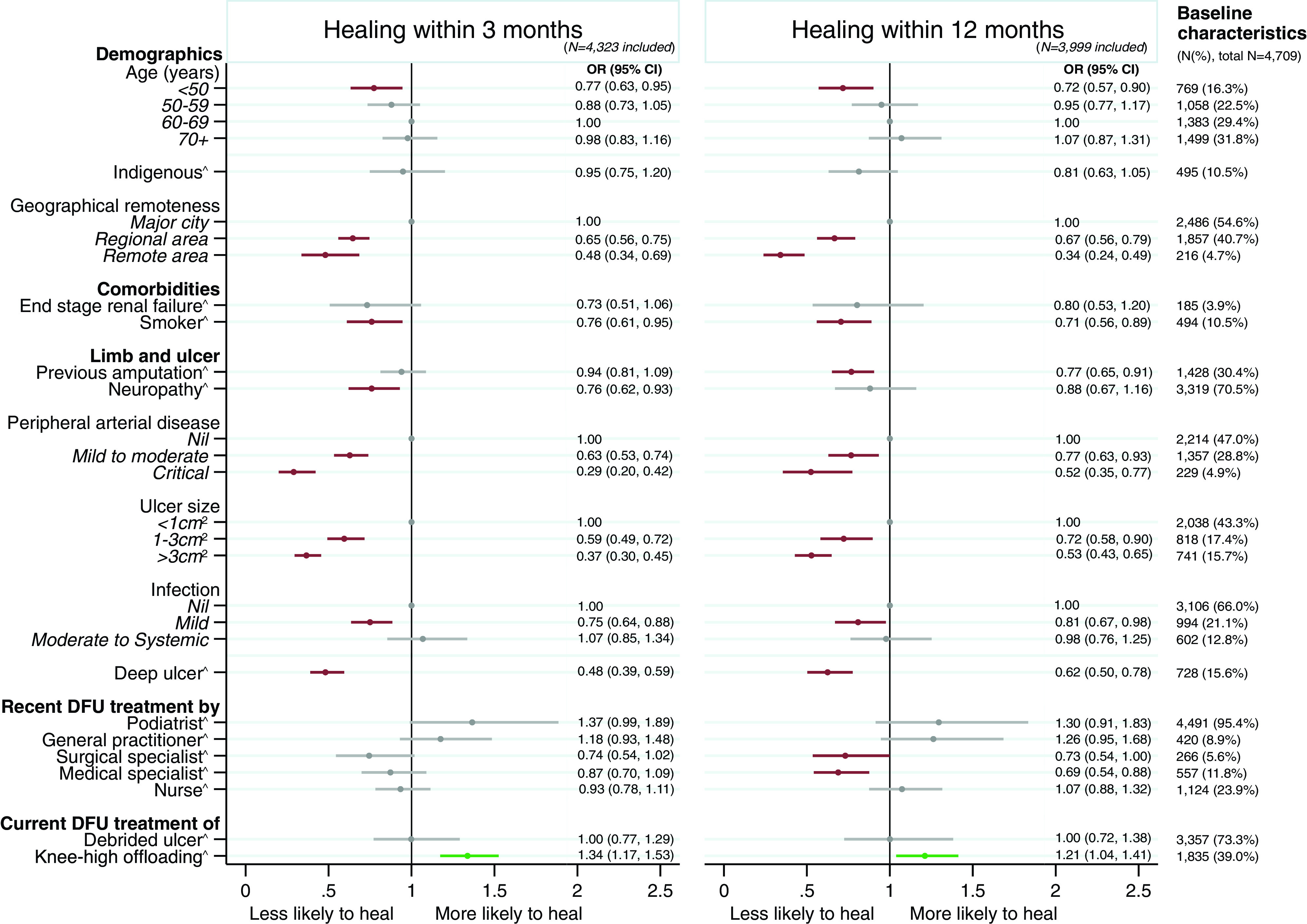
Multivariable analysis of factors associated with healing of DFUs within 3 months and 12 months. All included variables are those with P < 0.10 on the univariable analysis. Statistically significant (P < 0.05) factors associated with lower likelihood to heal are highlighted in red, statistically significant factors associated with higher likelihood to heal are in green, and variables not found to be significant (P > 0.05) are in gray. Multiple imputation was used to impute variables with <25% missing data, including geographical remoteness, previous amputation, neuropathy, peripheral arterial disease, ulcer size, infection, deep ulcer, debrided ulcer, and knee-high offloading. The multivariable logistic model for healing at 3 months was built including patients with at least a 3-month follow-up (n = 4,323). The multivariable logistic model for healing at 12 months was built including patients with at least a 12-month follow-up (n = 3,999). OR, odds ratios. ^The results of the category “Yes” are presented, with the category “No” used as the reference group for this variable.
This prospective study of a large, diverse, real-world DFU cohort (equivalent to ∼50% of ∼9,000 people with DFU each year in Queensland [1]) first confirms previously reported limb and ulcer-related factors that negatively influence healing of DFU in cohorts attending mostly metropolitan tertiary centers, including neuropathy, peripheral arterial disease, previous amputation, larger ulcer size, deep ulcers, and infection (2–4). Second, it confirms the previously reported harmful effect of smoking on DFU healing from smaller tertiary center cohorts. Third, and perhaps most importantly, we seemed to identify new factors positively (current knee-high offloading treatment) and negatively (younger age, geographical remoteness, and recent specialist treatment) influencing healing of DFU.
Concerning these new findings, we suggest the negative influence of younger age to potentially be a surrogate for younger-onset type 2 diabetes, emerging as a more severe phenotype for (foot) complications. Geographical remoteness and recent specialist treatment are likely surrogates for delayed access and/or more severe presentation to specialist diabetic foot services, reinforcing the impact of early access to these services on DFU healing. Knee-high offloading treatment confirms trial findings and might be a surrogate for the positive influence of guideline-recommended treatment on DFU healing. Interestingly, we did not find Indigenous status, after controlling for geographical remoteness, to be associated with DFU healing.
Overall, these new findings confirm and extend our understanding of the influence that severity of DFU presentation, early access to diabetic foot services, and enacting guideline-recommended treatment have on healing DFUs.
Article Information
Acknowledgments. This research was conducted using the QHRFF Database resource. The authors are most grateful to the Diabetic Foot Working Group, Queensland Statewide Diabetes Clinical Network (Australia), and to the individual centers that provided the data.
Funding. Funding sources for this work include the Chinese Scholarship Council and Australian National Health and Medical Research Council (grant numbers 1143435 and 1161138).
The funding sources had no role in study design, data analysis, interpretation, or decision to submit for publication.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. Y.Z. contributed to conception and design of the study; contributed to data acquisition, analysis, and interpretation; and drafted and critically reviewed the manuscript for intellectual content. S.C. contributed to conception and design of the study and to data analysis and interpretation and drafted and critically reviewed the manuscript for intellectual content. S.M.M. contributed to conception and design of the study and data interpretation and critically reviewed the manuscript for intellectual content. R.P. contributed to conception and design of the study and data acquisition and critically reviewed the manuscript for intellectual content. J.J.v.N. and Q.C. contributed to data analysis and interpretation and critically reviewed the manuscript for intellectual content. P.H.D. and E.M.K. contributed to conception and design of the study and data acquisition and critically reviewed the manuscript for intellectual content. P.A.L. contributed to conception and design of the study; contributed to data acquisition, analysis, and interpretation; and drafted and critically reviewed the manuscript for intellectual content. All authors reviewed and approved the final version of the manuscript. Y.Z. had full access to all the data and final responsibility for publication submission. Y.Z. and P.A.L. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Appendix
Diabetic Foot Working Group, Queensland Statewide Diabetes Clinical Network (Australia): Kimberley Canning, Danielle Charles, Patrick Derhy, Pankaj Jha, Achamma Joseph, Ewan Kinnear (chair), Amy Langley, Shireen Lazaro, Peter Lazzarini, Rebecca Mann, Helen Martin, Sharon O’Rourke, and Helen Sheahan.
Footnotes
A complete list of the members of the Diabetic Foot Working Group, Queensland Statewide Diabetes Clinical Network (Australia), is provided in the Appendix.
References
- 1. Zhang Y, Lazzarini PA, McPhail SM, van Netten JJ, Armstrong DG, Pacella RE. Global disability burdens of diabetes-related lower-extremity complications in 1990 and 2016. Diabetes Care 2020;43:964–974 [DOI] [PubMed] [Google Scholar]
- 2. Prompers L, Schaper N, Apelqvist J, et al. Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE Study. Diabetologia 2008;51:747–755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Margolis DJ, Allen-Taylor L, Hoffstad O, Berlin JA. Diabetic neuropathic foot ulcers: the association of wound size, wound duration, and wound grade on healing. Diabetes Care 2002;25:1835–1839 [DOI] [PubMed] [Google Scholar]
- 4. National Diabetes Foot Care Audit . National Diabetes Foot Care Audit fourth annual report; 9 May 2019. Accessed 28 May 2020. Available from https://www.hqip.org.uk/wp-content/uploads/2019/05/National-Diabetes-Foot-Care-Audit-fourth-annual-report-FINAL.pdf
- 5. Jia L, Parker CN, Parker TJ, et al.; Diabetic Foot Working Group, Queensland Statewide Diabetes Clinical Network (Australia) . Incidence and risk factors for developing infection in patients presenting with uninfected diabetic foot ulcers. PLoS One 2017;12:e0177916. [DOI] [PMC free article] [PubMed] [Google Scholar]


