Abstract
Primary pulmonary angiosarcoma is a rare type of malignant vascular tumour with poor prognosis. Diagnosis is often late due to non-specific symptoms and low clinical suspicion for angiosarcoma. A 72-year-old man presented to hospital with a 6-month history of mild progressive dyspnoea, with associated cough, episodes of presyncope and weight loss. CT pulmonary angiogram (CTPA) was reported as a large saddle pulmonary embolism extending into both the right and left pulmonary arteries. Further Multidisciplinary team meeting (MDM) discussion, and review of CTPA and subsequent investigations revealed a large primary pulmonary artery sarcoma which was later confirmed histology. The patient was referred to the cardiothoracic surgeons and underwent left radical pneumonectomy.
Keywords: lung cancer (oncology), respiratory cancer, pulmonary embolism
Background
Angiosarcoma is a malignant epithelial cell neoplasm of vascular or lymphatic origin. A primary lung tumour is extremely rare, with only a several cases reported. The incidence of primary pulmonary angiosarcoma is about 0.001% to 0.030%. The key features of behaviour of these tumours include insidious growth, extensive local invasion and haematogenous metastasis. It mainly occurs in middle-aged men. The postoperative survival time is only about 12 months.1
Case presentation
We describe a case of a patient with primary pulmonary angiosarcoma. A 72-year-old man presented to hospital with a 6-month history of mild progressive dyspnoea, with associated cough, episodes of presyncope and weight loss. He had a medical history of hypertension and psoriasis.
Physical examination demonstrated no significant abnormal findings. Investigations were significant for a raised D-dimer (1.66 µg/mL) and raised NT-pro Brain natriuretic peptide (BNP) (8767 pg/mL). Other blood reports including full blood count, C reactive protein, fibrinogen, liver function test and renal functions test were normal.
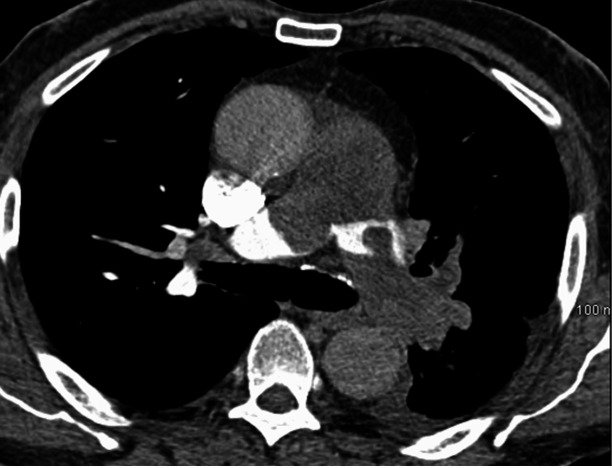
CT pulmonary angiogram (CTPA) demonstrated large occluding and saddle embolus in the main pulmonary trunk extending into both right and left main pulmonary arteries. There was marked obstruction on the left with no contrast seen within any of the left pulmonary artery branches within the left hemithorax (figure 1).
Figure 1.
CT pulmonary angiogram. CT PA:Filling defect in main PA and right and left PA. Obstruction of Left PA with no visible contrast.
This case was initially diagnosed as pulmonary embolism and commenced on treatment with anticoagulation. Echocardiogram demonstrated right ventricular dysfunction with Right ventricular systolic pressure (RSVP) of above 60 mm Hg.
This case was further discussed and CTPA was reviewed in multidisciplinary team meeting attended by respiratory physician, chest radiologist and cardiothoracic surgeon with the possible diagnosis of pulmonary angiosarcoma and positron emission tomography (PET CT) was performed after MDM.
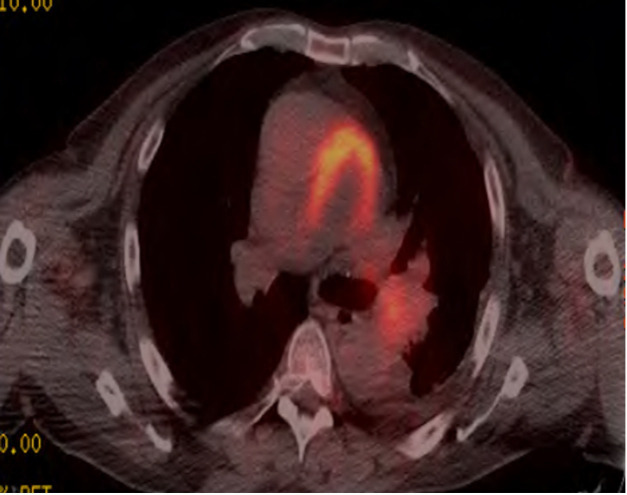
PET CT demonstrated distention of pulmonary trunk and proximal pulmonary arteries with evidence of occluding Fluorodeoxyglucose (FDG) avid soft tissue SUV max of 7.4, extending into proximal aspect of right pulmonary artery and lobar branches on left side. Further extension distally in the left pulmonary artery with SUV max of 5.1 was demonstrated. No FDG positive disease was identified outside the pulmonary arterial system (figure 2).
Figure 2.
PET CT. PET CT : FDG avid soft tissue in main PA and Left PA.
Fluoroscopy guided percutaneous biopsy was attempted but it was difficult to biopsy due to hard nature of mass, therefore it was a presumed diagnosis of pulmonary artery sarcoma due FDG avid soft tissue mass on PET CT. Management options were to do nothing at all with average survival of only few months or treat with chemotherapy and radiotherapy, which has no huge response found in literature. Other options were either a palliative pulmonary thrombo-endarterectomy with an average survival of about 6 months, or curative type surgical resection with average survival of 3–4 years.
Treatment
The patient was referred to the cardiothoracic surgeons and he underwent radical left pneumonectomy with resection of pulmonary valve, main PA into proximal RPA and coronary artery bypass grafts × two for left main coronary stenosis. Histology later confirmed high grade primary pulmonary atrial sarcoma. The tumour was 150 mm in length extended down into left branch pulmonary arteries. There was a lot of pleomorphic spindle cell tumour cells and mixed atypical cells with extensive necrosis, fibrosis and occasional mitosis. Immunohistochemistry revealed positive staining of neoplastic cells for vimentin, actin, desmin and CD31. Immunostains for cytokeratins, Epithelial membrane atigen (EMA) and S100 were negative.
Outcome and follow-up
He made good postoperative recovery after few weeks of surgery and started walking independently with mild shortness of breath. Follow-up CT thorax 2 months after discharge showed no evidence of recurrence.
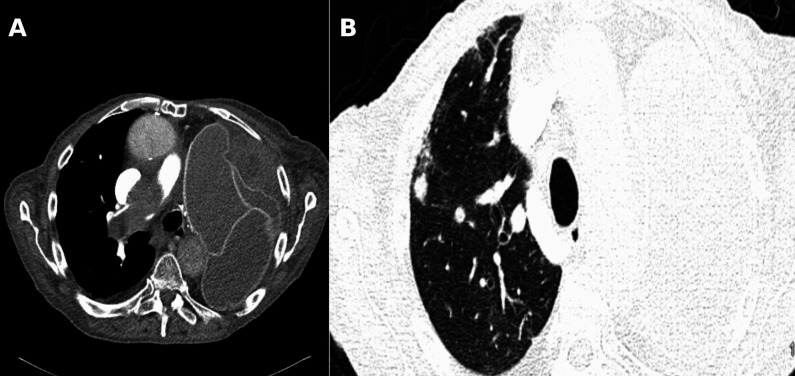
Ten months postsurgery, the patient was reviewed in the clinic, and he complained of severe dyspnoea. Repeating CT thorax demonstrated recurrence of pulmonary angiosarcoma with extensive filling defect with in right main pulmonary artery extending down in Right lower lobe (RLL) pulmonary arteries and multiple right lung nodules (figure 3A, B).
Figure 3.
(A, B) CT Thorax,10 months postsurgery. CT Thorax: extensive filling defect within right main PA extending down in RLL pulmonary artery and multiple right lung nodule.
Patient was referred for palliative radiotherapy but he was too frail to receive radiotherapy treatment, and he died within 1 month of diagnosis of recurrence of pulmonary angiosarcoma.
Discussion
Primary pulmonary angiosarcoma is a difficult disease to diagnose clinically with non-specific respiratory symptoms. Patients present with non-specific respiratory symptoms which include hemoptysis, dyspnoea, cough, chest pain and weight loss. Early diagnosis is uncommon, because of its rarity and low index of suspicion. The average age of diagnosis of the disease according to the data given in the literature is 55.9 years and men are found to be more often affected than women.2 3
The key features of behaviour of these tumours include insidious growth, extensive local invasion and haematogenous metastasis. Definitive diagnosis is made by biopsy and immunohistochemical analysis. Pulmonary angiosarcoma is characterised by the proliferation of tumour cells with endothelial features. Features include variably sized vascular channels with irregular branching, epithelioid like endothelial lining of vascular spaces, abundant cytoplasm with pleomorphic nuclei and prominent nucleoli. Endothelial markers are typically expressed in angiosarcoma. These markers include CD 31, CD 34 and factor VIII related antigen. Of these markers, CD 31 is relatively specific and extremely sensitive, being detected in approximately 90% of cases.4
No standard treatment regimen has been established for pulmonary angiosarcoma. Radiation therapy, chemotherapy, surgical resection and immunotherapy have been attempted. For patients with localised disease, surgery has been shown to be the most effective Most patients with primary pulmonary angiosarcoma have poor prognosis after surgery excision. The report of longest survival period was 3 years.5
Learning points.
Primary pulmonary angiosarcoma is an extremely rare tumour.
Due to its non-specific clinical manifestations and radiological features, pulmonary angiosarcoma is often misdiagnosed with pulmonary embolism.
Primary pulmonary angiosarcoma should be considered in patients with atypical symptoms and inadequate response to thrombolytic therapy.
High risk of recurrence.
After surgery, the patient should have regular follow-up.
Acknowledgments
Department Of Respiratory MedicineUniversity Hospital Limerick, Ireland.
Footnotes
Contributors: Dr KR was the lead author of this case report and actively involved in the management of patient.Dr OR was actively involved in the management of patient and contributed in collection of data and drafting of manuscript.Dr AO’B was the consultant involved in the management of patient and finalised the manuscript of case report for submission.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained from next of kin.
References
- 1.Levy E, Korach A, Amir G, et al. Undifferentiated sarcoma of the pulmonary artery mimicking pulmonary thromboembolic disease. Heart Lung Circ 2006;15:62–3. 10.1016/j.hlc.2005.06.009 [DOI] [PubMed] [Google Scholar]
- 2.Patsios D, de Perrot M, Tsao M-S, et al. Epithelioid angiosarcoma of the lung: a rare late complication of Lucite plombage. Br J Radiol 2006;79:e36–9. 10.1259/bjr/12749434 [DOI] [PubMed] [Google Scholar]
- 3.Wilson R, Glaros S, Brown RKJ, et al. Complete radiographic response of primary pulmonary angiosarcomas following gemcitabine and taxotere. Lung Cancer 2008;61:131–6. 10.1016/j.lungcan.2007.12.006 [DOI] [PubMed] [Google Scholar]
- 4.Travis WD, Brambilla E, Muller-Hermelink HK, et al. World Health organization classification of tumours. pathology and genetics of tumours of the lung, pleura, thymus and heart. IARC Press: Lyon, 2004. [Google Scholar]
- 5.Ozcelik C, Onat S, Yaldiz M, et al. Primary epithelioid angiosarcoma of the lung presenting as pulmonary hemorrhage. Asian Cardiovasc Thorac Ann 2006;14:69–71. 10.1177/021849230601400118 [DOI] [PubMed] [Google Scholar]