Abstract
Subacute thyroiditis following vaccination is an uncommon presentation of thyrotoxicosis. As the world undertakes its largest immunisation campaign to date in an attempt to protect the population from COVID-19 infections, an increasing number of rare post vaccine side effects are being observed. We report a case of a middle-aged woman who presented with painful thyroid swelling following the second dose of the COVID-19 mRNA vaccine BNT162b2 (Pfizer–BioNTech) with clinical, biochemical and imaging features consistent with destructive thyrotoxicosis. Symptomatic management only was required for the self-limiting episode. Thyroiditis typically has a mild and self-limiting course and thus this observation should not deter people from vaccination, as COVID-19 infection has a far greater morbidity and mortality risk than thyroiditis.
Keywords: endocrine system, immunological products and vaccines, thyroid disease
Background
Subacute thyroiditis (SAT) post vaccination is an uncommon presentation of thyrotoxicosis. With the largest vaccination drive ongoing globally, rarer side effects are being noted. Here, we report an interesting case of thyrotoxicosis following COVID-19 vaccination, its clinical course, diagnostic challenge and management.
Case presentation
A middle-aged woman presented with a history of rapid onset painful swelling of the thyroid gland and symptoms of thyrotoxicosis, including poor sleep, worsening night sweats, hyper defaecation and weight loss. The onset of symptoms was 2 weeks following her second dose of the COVID-19 mRNA vaccine BNT162b2 (Pfizer–BioNTech). There was no significant medical history and the patient was not on any regular prescribed medications. There was no history of prior use of lithium, amiodarone or interferon (which could potentially precipitate thyrotoxicosis).
Investigations
Initial biochemical investigations were consistent with thyrotoxicosis, with normal anti-thyroid peroxidase (TPO) and thyroid stimulating hormone (TSH) receptor antibody levels (TRAb; table 1). Technetium (Tc-99m) pertechnetate thyroid scintigraphy performed during the thyrotoxic phase demonstrated minimal isotope uptake, consistent with destructive thyroiditis (figure 1). She had no treatment other than a short course of a non-steroidal anti-inflammatory drug and her symptoms resolved over 6 weeks; her thyroid function normalised within 8 weeks (table 1).
Table 1.
Laboratory results
| Parameters | Trend in the results | Reference range | |
| Thyrotoxic phase | Euthyroid phase | ||
| TSH | <0.010 | 0.63 | 0.2–4.5 (mU/L) |
| Free T4 | 27 | 10 | 9–21 (pmol/L) |
| Total T3 | 3.3 | – | 0.9–2.4 (nmol/L) |
| Anti-TPO | 79.5 | – | 0–100 (IU/mL) |
| TRAb | <1.2 | – | 0-2-1 (IU/L) |
| Haemoglobin | 124 | 130 | 115–165 (g/L) |
| White cell count | 5.6 | 5.1 | 4.0–11.0 (109/L) |
| Lymphocyte count | 1.40 | 1.38 | 1.5–4.0 (109/L) |
| Platelet count | 313 | 267 | 150–400 (109/L) |
| C reactive protein | 23 | <1 | 0–5 (mg/L) |
TPO, thyroid peroxidase; TRAb, TSH receptor antibody; TSH, thyroid stimulating hormone.
Figure 1.
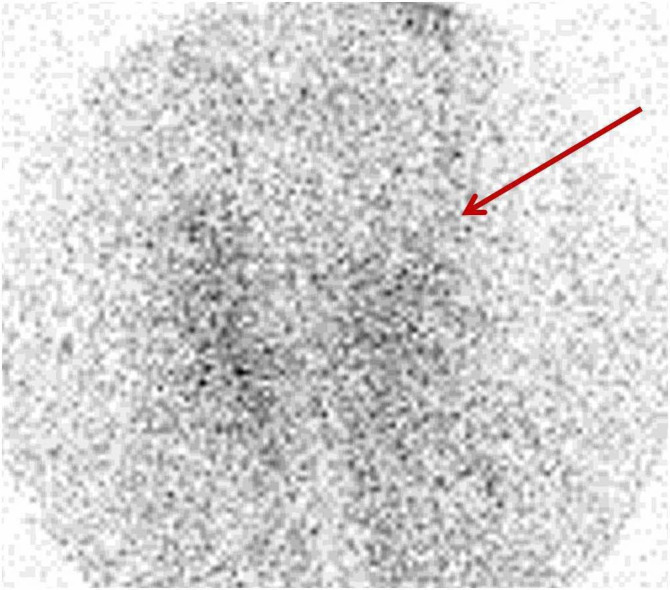
Technetium (Tc-99m) pertechnetate uptake scan showing only minimal uptake (indicating by red arrow) suggestive of destructive thyroiditis.
Differential diagnosis
While Graves’ disease can present with transient hyperthyroidism, the clinical picture, normal thyroid autoantibodies and scintigraphy findings were indicative of subacute destructive thyroiditis
Outcome and follow-up
Our patient was managed conservatively with a course of Non-steroidal anti-inflammatory drugs (NSAIDs) for her pain relief. As her thyrotoxicosis symptoms rapidly resolved, she did not require any antithyroid medication or beta-blocker. At her follow up review at 3 months, she continued to remain clinically and biochemically euthyroid.
Discussion
SAT, also identified by various other names, is well recognised to cause follicular destruction and the rapid release of preformed thyroid hormones.1 If a likely precipitating event can be identified, this is most commonly a viral upper respiratory tract infection during the 2–3 weeks preceding the onset of thyroid symptoms.2 However, there have also been documented cases of SAT occurring shortly after influenza vaccination.3 The exact pathogenesis underlying vaccination-associated SAT is unclear. Some authors have attributed it to the adjuvant causing autoimmune/inflammatory syndrome induced by adjuvants (ASIA) but others have suggested that the vaccine core component might cause either direct injury or share the same epitope, inducing antibody cross-reaction between the antigen in the vaccine and thyroid follicular cells.3 4 Biopsy studies in these patients have demonstrated infiltration predominantly with multinuclear giant cell granulomas.5
SARS-CoV-2 virus gains entry into multiple endocrine tissues, including thyroid follicular cells, due to the abundance of angiotensin-converting enzyme-2 receptors expressed on their surface.6 Studies with human IgG1 monoclonal antibody against SAR-CoV-2 spike protein have shown cross-reactivity with TPO, thyroglobulin and other cellular components of the follicle.7 Some form of thyroid dysfunction is seen in nearly one-third of all COVID-19 infections in whom thyroid function has been measured.8 However, studies during the development of vaccines against the SARS-CoV-2 virus have not reported a significant incidence of thyroid complications. This may be due to patient numbers in these studies being too small to enable the identification of rare side effects.9 To our knowledge, there have been just two other similar reports of post-vaccination thyrotoxicosis so far, one following the Pfizer/BioNTech mRNA vaccine and the other following CoronaVac, which is an inactivated whole-cell vaccine.10 11 At this stage, it is very difficult to be certain whether it is the antigen component or the adjuvant which predominantly causes the immune/inflammatory response.
The diagnosis is essentially clinical, with elevated thyroid hormone and suppressed TSH concentrations. Low isotope uptake on thyroid scintigraphy and normal TPO and TSH receptor antibody levels are useful in excluding other common causes of hyperthyroidism. Where there is limited access to these investigations, a lower ratio of T3 to T4 favours destructive thyroiditis in comparison with Graves’ thyrotoxicosis.12 The treatment is symptomatic, with non-steroidal anti-inflammatory drugs and beta-blockers during the inflammatory thyrotoxic phase and subsequently levothyroxine if the patient goes on to develop symptomatic hypothyroidism, as with any form of SAT. Corticosteroids may be considered for the patient presenting with moderate-to-severe pain with or without thyrotoxicosis or who failed to respond to initial treatment with NSAIDs.
Vaccination on such a global scale will inevitably be associated with rare side effects, which were not evident in vaccine trials. However, SAT is generally relatively mild and transient, so it should not deter people from getting vaccinated, particularly given the much greater risks from contracting COVID-19 infection.
Patient’s perspective.
I had my second dose of the Pfizer COVID-19 vaccine early this year. For the next 36 hours I felt very unwell—like I had a bad influenza with headaches, muscle and joint pain and was feeling shivery and exhausted. After 36 hours I felt completely well again.
Two weeks later I had noticed that my neck was painful. I was reading and found my neck hurt when I bent my head down. I could also feel a lump at the front of my neck which was tender to touch. When I looked in the mirror there was a visible lump. This was more noticeable when I swallowed and my husband could also see it. I did not have a sore throat and had no difficulty swallowing or speaking. I did not feel particularly unwell. I did think that it was my thyroid that was swollen and not my throat or larynx.
I saw my GP and she could feel a lump and took some bloods. She asked if there was any history of thyroid problems in my family. My mother had thyroid cancer when she was young and her sister and her sister’s son have Hashimoto’s thyroiditis. The doctor also asked if I had lost any weight, I had not really paid any attention to my weight but when I weighed myself at home, I had lost weight and my clothes felt looser. I lost my appetite initially—I usually snack between meals but I was not feeling like eating much. I was going to the toilet very frequently and had a marked increase in night sweats and was finding it very difficult to get any sleep. I was also having sweats during the day, was very intolerant of heat and felt very anxious. My weight was continuing to drop even when my appetite returned. I lost 10 lbs in total.
I had a thyroid scan 2 weeks after the swelling onset and at this time the lump had decreased in size and was not very noticeable. By the start of May, I was feeling better; my bowels had returned to normal, I was no longer anxious and my night sweats had settled. I was also gaining weight again.
Learning points.
Subacute thyroiditis following COVID-19 vaccination is a rare complication.
Taking a comprehensive history, including recent COVID-19 vaccination and/or infection, can help to identify rare vaccine-related complications.
Thyroiditis is usually a mild self-limiting illness and the possible association with prior vaccination should not deter people from COVID-19 vaccination.
Acknowledgments
The authors are grateful to the patient for her thoughtful review of the manuscript and permission to share her story.
Footnotes
Contributors: MSJ and ARD were involved in the primary evaluation and management of the patient and conception and drafting of the case report. FG and AWP were involved in reviewing the existing literature and revising the report. ARD is the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Volpé R. Thyroiditis: current views of pathogenesis. Med Clin North Am 1975;59:1163–75. 10.1016/S0025-7125(16)31965-4 [DOI] [PubMed] [Google Scholar]
- 2.Desailloud R, Hober D. Viruses and thyroiditis: an update. Virol J 2009;6:5. 10.1186/1743-422X-6-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Passah A, Arora S, Damle NA, et al. Occurrence of subacute thyroiditis following influenza vaccination. Indian J Endocrinol Metab 2018;22:713–4. 10.4103/ijem.IJEM_237_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Watad A, David P, Brown S, et al. Autoimmune/Inflammatory syndrome induced by adjuvants and thyroid autoimmunity. Front Endocrinol 2016;7:150. 10.3389/fendo.2016.00150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trivedi DP, Bhagat R, Nakanishi Y, et al. Granulomatous thyroiditis: a case report and literature review. Ann Clin Lab Sci 2017;47:620–4. [PubMed] [Google Scholar]
- 6.Lundholm MD, Poku C, Emanuele N, et al. SARS-CoV-2 (COVID-19) and the endocrine system. J Endocr Soc 2020;4:bvaa144. 10.1210/jendso/bvaa144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vojdani A, Vojdani E, Kharrazian D. Reaction of human monoclonal antibodies to SARS-CoV-2 proteins with tissue antigens: implications for autoimmune diseases. Front Immunol 2020;11:617089. 10.3389/fimmu.2020.617089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lania A, Sandri MT, Cellini M, et al. Thyrotoxicosis in patients with COVID-19: the THYRCOV study. Eur J Endocrinol 2020;183:381–7. 10.1530/EJE-20-0335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med 2020;383:2603–15. 10.1056/NEJMoa2034577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.İremli BG, Şendur SN, Ünlütürk U. Three cases of subacute thyroiditis following SARS-CoV-2 vaccine: postvaccination Asia syndrome. J Clin Endocrinol Metab 2021;106:2600-2605. 10.1210/clinem/dgab373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Franquemont S, Galvez J. Subacute thyroiditis after mRNA vaccine for Covid-19. J Endocr Soc 2021;5:A956–7. 10.1210/jendso/bvab048.1954 [DOI] [Google Scholar]
- 12.Baral S, Shrestha PK, Pant V. Serum Free T3 to Free T4 Ratio as a Useful Indicator for Differentiating Destruction Induced Thyrotoxicosis from Graves' Disease. J Clin Diagn Res 2017;11:OC12–14. 10.7860/JCDR/2017/28293.10180 [DOI] [PMC free article] [PubMed] [Google Scholar]


